Back to Journals » Advances in Medical Education and Practice » Volume 13
Assessing Training Needs of Health Personnel on the Process of Selecting Blood Donors and Transfusion in the West Region of Cameroon
Authors Murhabazi Bashombwa A , Tchio-Nighie KH, Tchingué Mbianda C , Tchindebe Bouri E , Nanfak A, Buh Nkum C, Ateudjieu J
Received 13 September 2022
Accepted for publication 6 December 2022
Published 19 December 2022 Volume 2022:13 Pages 1525—1533
DOI https://doi.org/10.2147/AMEP.S388478
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Augustin Murhabazi Bashombwa,1,2 Ketina Hirma Tchio-Nighie,3 Carine Tchingué Mbianda,2 Ela Tchindebe Bouri,2 Aude Nanfak,3 Collins Buh Nkum,3 Jérôme Ateudjieu2– 4
1Faculty of Medicine, Université de Kaziba, Kaziba, Democratic Republic of Congo; 2Department of Public Health, Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Dschang, Cameroon; 3Department of Health Research, M.A. SANTE (Meilleur Accès aux Soins de Santé), Yaounde, Cameroon; 4Division of Health Operations Research, Ministry of Public Health, Yaounde, Cameroon
Correspondence: Augustin Murhabazi Bashombwa, Tel +243 808395691, Email [email protected]
Introduction: Blood transfusion is a health care procedure that can expose the donor and receiver to risks. The knowledge and practices of healthcare personnel on blood transfusion are necessary to anticipate and/or prevent the occurrence of avoidable transfusion risks. The aim of this study was to assess the training needs of health personnel on blood donor selection procedure.
Methods: We conducted a cross-sectional study targeting health personnel in health facilities that reported contributing in offering blood transfusion services in the West region of Cameroon between March and May 2022. A questionnaire administered face to face was used to collect data from the targeted health personnel exhaustively included from health facilities. Knowledge and practices were assessed by estimating the rate of correct answers. STATA software was used to analyze the data.
Results: Of the 41 health facilities that reported offering blood transfusion services, 35 (85.3%) were covered. Category 5 and 4 health facilities were respectively 23 (65.7%) and 9 (25.7%). Among the 325 health personnel involved in transfusion, 302 (92.9%) were reached among which, 201 (66.6%) were female and 127 (42.1%) were nurses. Two hundred and ten (69.5%) had already received training on blood transfusion and 268 (88.7%) expressed a need for training on blood transfusion of which 139 (51.8%) on blood donors’ selection. Sixteen (5.3%) knew how to identify blood donor and 116 (38.4) knew the minimum required tests to be performed on the donors’ blood before the transfusion. Six (2.0%) out of 302 health personnel were able to select blood donors and identify minimum tests to be performed on donors’ blood.
Conclusion: There is a real need for training of health personnel on the blood donor selection process. Health authorities should ensure that all health personnel involved in blood transfusion receive a minimum of training in blood donor selection and testing.
Keywords: training needs, health personnel, selecting, blood donors
Introduction
Blood transfusion is a life-saving fundamental procedure and requires blood to be collected, handled, stored, prescribed and monitored by trained healthcare personnel for proper patient safety.1–5 Blood transfusion has helped save many lives, but it is an activity that can constitute many risks, particularly infectious, immunological and hemodynamic.6–10 This procedure sometimes results in adverse events in the receivers, which can range from minor to serious. Studies have been conducted in different settings to assess the prevalence of adverse events after blood transfusion. Out of 100,000 transfusions, a prevalence of 220 adverse events with a predominance of immunological adverse events was found in the USA.11 In Turkey, Yeter found a prevalence of 0.09% of which 47.3% was immunological.12 In Africa, with the poor performance in the organization and coordination of national blood transfusion systems, particularly with regard to health personnel, donor selection and haemovigilance, the risks associated with blood transfusion are higher than in developed countries.13 Studies carried out in Cameroon have shown a prevalence of 2.8% with a predominance of hypotension and a seroprevalence of 10.5% in blood donations.14,15
Numerous studies present an incidence of transfusion errors ranging from 1/60,000 to 1/30,000 and estimate that the real incidence is largely underestimated. These types of errors include mainly infectious risks, immunological and volume overloads. Most of these errors are most likely associated with health personnel practices. This is supported by the fact that the training of health personnel is documented to contribute greatly to avoiding the dangers and risks associated with blood transfusion.1,4,9,16
Blood transfusion is framed by guidelines from the World Health Organization, particularly with regard to the recruitment of blood donors (guidelines on assessing donor suitability) and transfusion policy (guide for the establishment of a national haemovigilance system, management of blood transfusion services).17,18 Cameroon has complied with these guidelines through Law No. 2003/2006 of September 22, 2003, on the organization of blood transfusion and Decree No. 2019/067 of February 12, 2019, on the organization and operation of the national blood transfusion center.19,20 In Cameroon, there is a national blood transfusion program and texts that regulate its organization and functioning.20
Despite the existence of this program, there are not yet national guidelines for the implementation of these texts. The haemovigilance system is virtually absent and practices in this area are not standardized. Some health facilities have blood banks, but due to the absence of national guides and directives on blood transfusion, the services expected from each of these blood banks are not standardized. Some low referral level health facilities practice blood transfusion while some higher level health facilities do not. This situation makes it difficult to standardize staff training needs, particularly with regard to the selection of blood donors.13,15,21
Studies have shown that health personnel contribute significantly to the occurrence of transfusion risks. These include poor practices in blood donor selection, blood transfusion surveillance and other transfusion practices. An assessment of health worker training needs is required to master strategies for building staff capacity to avoid observed and documented errors.22
To the best of our knowledge, there is still no data in Cameroon on the training needs of health personnel in blood transfusion and even less on the selection of blood donors. This study aims to assess the training needs of health personnel in West Cameroon on the selection of blood donors. The results will be used to strengthen the skills of health personnel in order to reduce the risks associated with the selection of blood donors.
Methods
Study Design
This was a cross-sectional descriptive study targeting health personnel of the health facilities which had declared to offer blood transfusion services in the region of West Cameroon. Data were collected between March and May 2022 using a questionnaire administered face to face to the targeted health personnel that were exhaustively included from the included health facilities.
Study Period and Settings
Data were collected between March 2022 and May 2022. This study was conducted in health facilities of the West region of Cameroon. The West Cameroon region has 20 health Districts made up of 244 health areas, 669 integrated health center, 29 district hospitals and 1 regional hospital, 1 referral hospital, 52 district medical centers and 17 clinics.
In the Cameroonian health system, category I health facilities represent high-reference health facilities and range from descending order to category VI health facilities which represent the lowest reference level and offer the minimum package of activities.
Study Population
Were eligible, medical doctors nurses, midwives, laboratory technicians and pharmacists who worked in the blood product collection, prescription, administration and transfusion follow-up departments. Excluded were interns, staff on leave and those who refused to participate.
Sampling
The health districts were selected through random stratified sampling with regard to their urban, semi-urban and rural geographical location. These include: the health districts of Dschang, Batcham, Mifi, Penka Michel and Bandjoun. The urban district being considered as any district having more than three health areas in an urban setting; the semi-urban district with more than one health area in an urban setting and a rural district with one or less than one health area in an urban setting. All health facilities that declared to offer blood transfusion services and that were recognized by the services of the health district were exhaustively selected. All health personnel working in the transfusion collection, prescription, administration and follow-up services within selected health facilities were exhaustively targeted.
Data Collection Tool
The data was collected using a questionnaire developed by the study team and pre-tested on 3 health personnel known to be involved in blood transfusion in their health facility (Foumbot Health District Hospital). The questionnaire collected data on health facilities’ characteristics, the socio-demographic characteristics of health personnel, knowledge of health personnel on blood donors’ selection. The need for training was assessed according to the expressed needs for training on the blood donors’ selection and the rate of correct answers to the 10 questions asked on blood donors’ selection criteria (5 on the identification of blood donor and 5 on the major tests) that included knowledge on parameters of selection of blood donors and usual tests to be conducted on donors’ blood. A rate of correct answers of 100% was considered as good knowledge.
Data Management and Data Analysis
Data were extracted from hard-copies questionnaires and integrated in Microsoft Excel software. The data was checked by a second person to detect outliers. Before being analyzed, the data was checked, cleaned and validated. STATA version 13 software was used to analyze the data. Effectives and percentages were used for the string variables and means and standard deviation for the numeric variables. The need for training was assessed according to the rate of correct answers to the 10 questions asked on blood donors’ selection criteria (5 on the identification of blood donor and 5 on the major tests). A rate of correct answers of 100% was considered as good knowledge.
Ethical Considerations
The present study was conducted to assess the training needs of health personnel in West Cameroon on the recruitment of blood donors. The research protocol of the study was submitted to the Regional Ethics Committee for Human Health Research of the West Region of Cameroon and was approved under reference NO2022/06/010/CE/CRERSH-OU/VP.
Results
Description of Participants
Out of 41 health facilities claiming to offer blood transfusion services targeted, 35 (85.3%) were reached. Among the 325 health personnel found to be involved in transfusion, 302 (92.9%) consented to participate. Table 1 presents the distribution of consenting health personnel by health district, type of health facility, category of health facility, professional category and sex. Of 302 health personnel, 201 (66.6) were female, 127 (42.1%) were nurses and 131 (43.4%) were working in category V health facilities. One hundred and thirty-eight (45.7%) were between 19 and 30 years old and 139 (46.0) had professional experience between 1 and 5 years.
 |
Table 1 Distribution of Health Personnel by Health Zone, Type of Health Facility, Category of Health Facility, Department, Professional Category and Sex |
Training Needs on Blood Donors’ Selection
Expressed Needs for Training on the Selection of Blood Donors and Previous Training on Blood Transfusion
Table 2 presents the expressed need of health personnel for training in the selection of blood donors. Of the 302 responding health personnel, 210 (69.5) had completed a blood transfusion training, Of 268 (88.7) who expressed a need for training in blood transfusion, 139 (51.8%) expressed a need for training on blood donors’ selection.
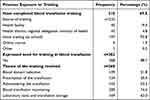 |
Table 2 Expressed Need for Training in the Selection of Blood Donors |
Objectivized Needs of Health Personnel on the Process of Blood Donors Selection
Of the 302 health personnel, 16 (5.3%) know to identify a blood donor and 116 (38.4) know to test a blood donor. Only 6 (2.0%) was able to select blood donor. Figures 1 and 2 present respectively the knowledge of health personnel on blood donors’ selection and knowledge on usual tests for blood donors’ selection. Of the 302 health personnel, 264 (87.4%) know the recommended age group of blood donors, 70 (23.2) know how to identify an ineligible blood donor. Only 162 (53.8%) health personnel knew that malaria test need to be conducted on collected blood.
 |
Figure 1 Knowledge of health personnel on blood donors’ selection. |
Distribution of Knowledge of Health Personnel on the Procedure of Blood Donor’s Selection by Category of Health Facility, Category of Health Personnel and Type of Health Facility
Table 3 presents the distribution of knowledge of health personnel on the process of blood donor selection by category of health facility, category of health personnel and type of health facility. It is noted that of 6 health personnel who know how to select blood donors, 3 (50.0%) work in a category IV health facility, 3 (50.0%) were medical doctors and 5 (83.3%) work in public health facilities.
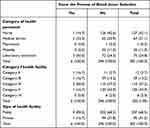 |
Table 3 Distribution of Knowledge of Health Personnel on the Procedure of Blood Donor’s Selection by Category of Health Facility, Category of Health Personnel and Type of Health Facility |
Discussion
The study shows that 210 (69.5%) health personnel had already received training on blood transfusion, 268 (88.7) expressed the need for training on blood transfusion, of which 139 (51.8%) on blood donors’ selection. Among the participants, 16 (5.3%) knew how to identify a blood donor and 116 (38.4) knew minimum required tests to be conducted on the donors’ blood before the transfusion. Only 6 (2.0%) out of 302 health personnel were able to select blood donors and identify minimum tests to be conducted on donors’ blood.
Training is a necessary prerequisite for acquiring new knowledge that can be implemented to improve the practices of health personnel. In the field of health, whether basic or continuous, knowledge is essential for the improvement of health care and the health system.23,24 In the present study, health personnel exposed to training were estimated at 69.5% among personnel involved in transfusion. This shows that some health personnel transfuse when they have not been trained and this questions the safety of patients who receive the transfusion, the recruitment and management of blood donors and the entire transfusion chain. Perhaps those who are not trained (formally) have learned by doing (experience) or from those who have been trained. Studies in Mali and DR Congo found 29.1% and 25.5% of health workers, respectively, who had previously undergone blood transfusion training.25,26 The difference between these studies and ours could be explained by the difference in training policy between the countries but also by the fact that they did not take into account initial training (that of school). By examining our results, we find that a proportion of health personnel had been exposed to theoretical and practical training on blood transfusion. Despite this, the quality of blood transfusion, the selection of blood donors and the associated risks remain to be questioned. It is essential that there is standardization of transfusion practices in the region but also to extend this study to other regions to assess and meet these needs.
It is necessary to assess the perceived needs of health personnel because it is the gateway to meeting all of their needs and objectives. Knowing the perceived needs of healthcare personnel improves their commitment and motivation. Studies have shown that taking into account the perceptions of the beneficiaries of an intervention is a key element for its success. The same is true for the perceived needs of health personnel.27–29 This is why we have, in this study, evaluated what health personnel perceive as training needs. Among our participants, 88.7% expressed a need for training on blood transfusion, mainly on donor selection and laboratory examinations in blood transfusion. To the best of our knowledge, we have only found studies that have assessed the expressed needs of healthcare personnel for training in blood transfusion. The fact that health personnel have expressed the need for training indicates that they are aware of it and are ready to be exposed to training on blood transfusion and in particular on the selection of blood donors. To objectify these perceived needs, the assessment of knowledge showed that only 5.3% of health personnel know how to identify a blood donor and 38.4% know the minimum infectious and immunological tests recommended for any blood donor. Only 2.0% know both identifying a blood donor and the minimum recommended tests. These results raise questions about the existence and standardization of guidelines, the availability and frequency of supervision, but also about the place occupied by blood transfusion in the training curricula within schools of health sciences. Studies carried out on other aspects of blood transfusion have shown results more or less similar to ours: Bediako et al in 2021 found an average level of knowledge of 29% among staff of health in Ghana.7 Mayaki et al found a level of knowledge greater than 70% among 3.3% of health workers, while Obi et al found a rate of 98% in Nigeria.3,30 The context of our study can explain these differences: knowledge was evaluated on a 100% correct response rate and we were interested in only one aspect of blood transfusion which is the selection of blood donors.
Even if they do not all have the same needs according to the different themes of blood transfusion, it is necessary to take into account the needs of each other. To meet these needs, health authorities must set up training programs that meet the expectations of health personnel. Even if the health authorities do not have all these training sources, there are even training sources available online which can cover at least 88% of the training needs of health personnel.31,32
Strength and Limitations
Our study has some limitations including the non-coverage of some health facilities (6 out of 41), but this situation does not limit the inference of these results because the 35 health facilities covered have the same characteristics as those that were not reached. The second limitation of this study is memory bias and the accuracy of information related to data collection using a questionnaire. As information on health facilities offering blood transfusion services was collected from district health services, there is a risk that some health facilities that transfuse did not report to district health services. This could underestimate the number of health facilities that offer blood transfusion services.
Conclusion and Future Directions
The Knowledge of health personnel on the selection of blood donors are insufficient and their training needs are real.
Among the health personnel, 7 out of 10 had already received training on blood transfusion. Despite this, less than 5% have the necessary knowledge on donor identification and the minimum recommended infectious and immunological tests to minimize transfusion risks. Nearly 88% of health personnel express a need for training, particularly in the selection of blood donors and the tests used in blood transfusion.
Future research should extend this study to other regions to assess and meet these needs, assess the place occupied by blood transfusion in training curricula. We recommend that health personnel be trained, in particular on online training sites. Health facilities to put in place a rigorous training and supervision program for health personnel. Health authorities to make blood transfusion guides and directives accessible and to set up a training program accessible to all health facilities.
Data Sharing Statement
Dataset used and analyzed during this study are available from the author corresponding to a reasonable request.
Ethical Approval and Consent to Participate
This study assessed the need for training of health personnel in the West region of Cameroon on the blood donor selection process and received approval from the Regional Ethics Committee for Human Health Research in West Cameroon. All participants were informed were informed about the purpose of the study. All activities were carried out according to the Declaration of Helsinki. The research protocol of the study was submitted to the Regional Ethics Committee for Human Health Research of the West Region of Cameroon and was approved under reference NO2022/06/010/CE/CRERSH-OU/VP.
Consent for Publication
All authors consent to the publication of the results of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Kaur P, Kaur G, Kaur R, Sood T. Assessment of impact of training in improving knowledge of blood transfusion among clinicians. Transfus Med Hemother. 2014;41(3):222–226. doi:10.1159/000362896
2. Masror Roudsari D, Feizi S, Maghsudlu M. Nurses’ hemovigilance knowledge and performance after teach-back, concept map, and lecture: a quasi-experimental study. Heliyon. 2021;7(1):e05982. doi:10.1016/j.heliyon.2021.e05982
3. Mayaki Z, Kabo R, Moutschen M, et al. Knowledge, attitudes and clinical practice of blood products prescribers in Niamey. Transfus Clin Biol J Soc Francaise Transfus Sang. 2016;23(2):78–85. doi:10.1016/j.tracli.2015.11.007
4. Mohd Noor NH, Saad NH, Khan M, et al. Blood transfusion knowledge among nurses in Malaysia: a university hospital experience. Int J Environ Res Public Health. 2021;18(21):11194. doi:10.3390/ijerph182111194
5. Islami Vaghar M. The impact of an educational program on blood and blood products transfusion on nurses’ level of knowledge and performance. J Med Life. 2018;11(3):238–242.
6. Aloweni F, See MTA, Ng XP, Ang SY. Employing serious game for assessing knowledge of blood transfusion procedure among nurses: a qualitative evaluation and feedback improvement study. Nurse Educ Today. 2021;101:104873. doi:10.1016/j.nedt.2021.104873
7. Bediako AA, Ofosu-Poku R, Druye AA. Safe blood transfusion practices among nurses in a major referral center in Ghana. Adv Hematol. 2021;2021:e6739329. doi:10.1155/2021/6739329
8. Ddungu H, Krantz EM, Phipps W, et al. Survey to assess knowledge and reported practices regarding blood transfusion among cancer physicians in Uganda. J Glob Oncol. 2018;4:
9. Steiner K, Baron-Stefaniak J, Hirschl AM, Barousch W, Willinger B, Baron DM. Education of medical personnel optimizes filling volume of blood culture bottles without negatively affecting microbiology testing. BMC Health Serv Res. 2020;20:1105. doi:10.1186/s12913-020-05959-z
10. Non-physician health-care workers and voluntary blood donation: an ambiguous relationship - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/28722278/.
11. Kracalik I, Mowla S, Basavaraju SV, Sapiano MRP. Transfusion-related adverse reactions: data from the national healthcare safety network hemovigilance module — United States, 2013–2018. Transfusion. 2021;61(5):1424–1434. doi:10.1111/trf.16362
12. Altayar MA, Jalal MM, Kabrah A, et al. Prevalence and association of transfusion transmitted infections with ABO and Rh blood groups among blood donors in the western region of Saudi Arabia: a 7-year retrospective analysis. Medicina. 2022;58(7):857. doi:10.3390/medicina58070857
13. Samukange WT, Kluempers V, Porwal M, et al. Implementation and performance of haemovigilance systems in 10 sub-saharan African countries is sub-optimal. BMC Health Serv Res. 2021;21. doi:10.1186/s12913-021-07235-0
14. Nchinda EC, Tagny CT, Mbanya D. Blood donor haemovigilance in Yaoundé, Cameroon. Transfus Med. 2012;22(4):257–261. doi:10.1111/j.1365-3148.2012.01161.x
15. Samje M, Fondoh VN, Nguefack-Tsague G, et al. Trends in serological markers of transfusion transmissible infections in blood donations at the Bamenda Hospital-based blood service, Cameroon. Transfus Clin Biol J Soc Francaise Transfus Sang. 2021;28(3):228–233. doi:10.1016/j.tracli.2021.05.011
16. Peedin AR. Update in transfusion medicine education. Clin Lab Med. 2021;41(4):697–711. doi:10.1016/j.cll.2021.07.010
17. Blood donation and transfusion safety. Available from: https://www.who.int/fr/news-room/fact-sheets/detail/blood-safety-and-availability.
18. World health organization. Blood donor selection: guidelines on assessing donor suitability for blood donation. Available from: https://www.who.int/publications-detail-redirect/9789241548519.
19. Republic of Cameroon. Law n°20032006 of December 22, 2003 governing blood transfusion in Cameroon. Available from: https://www.juriafrica.com/lex/decret-2019-067-12-fevrier-2019-29130.htm; 2003.
20. Republic of Cameroon. Decree no 2019067 of February 12, 2019 on the organization of blood transfusion in Cameroon. Available from: https://dpml.cm/index.php/fr/publications/normes-et-legislation/transfusion-sanguine; 2019.
21. Tagny CT, Laperche S, Murphy EL. Updated characteristics of blood services, donors and blood products in 11 French-speaking African countries. Vox Sang. 2018;113(7):647–656. doi:10.1111/vox.12702
22. Kandasamy D, Shastry S, Chenna D, Mohan G. Blood donor deferral analysis in relation to the screening process: a single-center study from Southern India with emphasis on high hemoglobin prevalence. J Blood Med. 2020;11:327–334. doi:10.2147/JBM.S265461
23. Molina-Arrebola MA, Fernández-Guerrero E, Aguirre-Ortega FJ, Avivar-Oyonarte C. Digital resources for transfusion education. J Educ Health Promot. 2020;9(1):173. doi:10.4103/jehp.jehp_81_20
24. Last K, Power NR, Dellière S, et al. Future developments in training. Clin Microbiol Infect off Publ Eur Soc Clin Microbiol Infect Dis. 2021;27(11):1595–1600. doi:10.1016/j.cmi.2021.06.032
25. Diakité M, Diawara SI, Tchiengoua Tchogang N, et al. Knowledge and attitudes of medical personnel in blood transfusion in Bamako, Mali. Transfus Clin Biol. 2012;19(2):74–77. doi:10.1016/j.tracli.2012.01.004
26. Kabinda JM, Miyanga SA, Donnen P, Ende JV, Den, Dramaix MW. Knowledge, attitudes and practices of medical and paramedical staff in blood transfusion in the Democratic Republic of Congo. Open J Prev Med. 2014;04(08):672–680. doi:10.4236/ojpm.2014.48076
27. Clark A, Anderson J, Adams E, Baker S. Assessing the knowledge, attitudes, behaviors and training needs related to infant feeding, specifically breastfeeding, of child care providers. Matern Child Health J. 2008;12(1):128–135. doi:10.1007/s10995-007-0221-4
28. Neff JL, Patterson MM, Johnson S. Meeting the training needs of those who meet the needs of victims: assessing service providers. Violence Vict. 2012;27(4):609–632. doi:10.1891/0886-6708.27.4.609
29. van Diggele C, Burgess A, Roberts C, Mellis C. Leadership in healthcare education. BMC Med Educ. 2020;20(Suppl 2):456. doi:10.1186/s12909-020-02288-x
30. Obi E, Diette-spiff C, Omunakwe H. Knowledge and practices of physicians on blood component therapy: a cross-sectional study from two tertiary hospitals in Nigeria. Afr Health Sci. 2021;21(3):1230–1236. doi:10.4314/ahs.v21i3.32
31. Blood transfusion training for health professionals nurses, caregivers. https://www.mediformation.com/pro-transfusion-module-01/formation.
32. IFRC. Education IFRC. https://www.ifrc.org/education.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

