Back to Journals » Open Access Emergency Medicine » Volume 12
Assessing the Utility of Ultrasound and Urinalysis for Patients with Possible Epididymo-Orchitis – A Retrospective Study
Authors Zitek T , Ahmed O, Lim C , Carodine R, Martin K
Received 12 October 2019
Accepted for publication 18 February 2020
Published 13 March 2020 Volume 2020:12 Pages 47—51
DOI https://doi.org/10.2147/OAEM.S234413
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Tony Zitek,1– 3 Omar Ahmed,3 Chee Lim,4 Rianda Carodine,1,5 Kent Martin2
1Department of Emergency Medicine, University Medical Center of Southern Nevada, Las Vegas, NV, USA; 2Department of Emergency Medicine, Kendall Regional Medical Center, Miami, FL, USA; 3Department of Emergency Medicine, University of Nevada, Las Vegas School of Medicine, Las Vegas, NV, USA; 4Touro University Nevada College of Osteopathic Medicine, Henderson, NV, USA; 5University of Nevada, Las Vegas, NV, USA
Correspondence: Tony Zitek
Department of Emergency Medicine, Kendall Regional Medical Center, 11750 SW 40 th St, Miami, FL 33175, USA
Email [email protected]
Purpose: Many experts recommend ordering an ultrasound and a urinalysis on all patients with scrotal pain. While the ultrasound may help diagnose a number of potential causes of scrotal pain, the urinalysis primarily has value in assessing for epididymo-orchitis. This study sought to evaluate the utility of these diagnostic tests for patients who presented to the emergency department (ED) with acute scrotal pain and possible epididymo-orchitis.
Patients and Methods: This was a single-center chart review of patients presenting to the ED with scrotal pain. Trained research assistants reviewed charts to obtain urinalysis and ultrasound results as well as diagnoses and treatments provided. Using the final diagnosis as a gold standard, the sensitivity and specificity of ultrasound and urinalysis were calculated for the diagnosis of epididymo-orchitis. Also, through a prespecified definition of “changed management,” we estimated the percentage of cases in which a urinalysis changed management of patients with acute scrotal pain.
Results: We identified 663 adult and pediatric patients who presented with scrotal pain during 2016. All patients had an ultrasound performed, and 458 (69.1%) had a urinalysis done. The sensitivity of urinalysis for epididymo-orchitis was 58.2% (95% CI 48.9% to 67.1%), and the specificity was 85.1% (95% CI 80.8% to 88.7%). For ultrasound, the sensitivity was 78.8% (95% CI 71.4% to 85.0%) and the specificity was 98.1% (95% CI 96.4% to 99.1%). In 24 of 458 cases (5.2% [95% CI 3.4% to 7.7%]) where a urinalysis was obtained, its results may have changed management of the patient.
Conclusion: The diagnosis of patients who present to the ED with scrotal pain is primarily driven by the ultrasound results. While the urinalysis may occasionally provide some benefit in the evaluation of patients with suspected epididymo-orchitis, the reflexive ordering of a urinalysis in patients with scrotal pain may be unnecessary.
Keywords: epididymitis, urinalysis, antibiotics, ultrasound
Plain Language Summary
Many experts currently recommend that both an ultrasound and urinalysis be performed on all patients who come to the emergency department with pain of the scrotum. Ultrasound is useful for diagnosing a wide range of problems that can cause scrotal pain, while urinalysis primarily is thought to help diagnose epididymitis-orchitis (inflammation of and/or around the testicle). There is very little evidence to support the recommendation that both ultrasound and urinalysis be done on all patients with scrotal pain, so the authors sought to determine how accurate and useful these tests are for such patients.
The authors reviewed the charts of 663 patients who came to the emergency department with scrotal pain and also had an ultrasound of their scrotum performed. A number of data points were taken from the patients’ charts including the ultrasound results, urinalysis results (if any), diagnoses made, and treatments received. The authors used this data to estimate the accuracy of ultrasound and urinalysis for diagnosing epididymitis-orchitis, and to assess the overall usefulness of urinalysis for patients with scrotal pain.
Ultimately, ultrasound was found to be a more accurate test for diagnosing epididymitis-orchitis than urinalysis, and in general, urinalysis changed the treatment of only about 5% of patients with scrotal pain. Therefore, while both ultrasound and urinalysis can be useful in the assessment of patients with scrotal pain, a urinalysis may not be needed on all patients with scrotal pain.
Introduction
Ultrasound is the diagnostic test of choice to evaluate acute scrotal pain.1 In fact, the company that employs the emergency medicine physicians at the involved institution for this study mandates that its providers order a testicular ultrasound or consult a urologist on any patient with testicular pain. In addition to ultrasound, many experts2–4 recommend a urinalysis (UA) as a routine diagnostic test for patients with scrotal pain primarily because of its purported ability to help diagnose and possibly treat epididymitis.
Epididymitis is the most common cause of scrotal pain in adults in the outpatient setting5 and is often accompanied by orchitis. We therefore use the term epididymo-orchitis to represent both. The diagnosis of epididymo-orchitis has traditionally been made clinically, incorporating findings from history, physical exam, UA, and ultrasound. To help guide treatment, the Centers for Disease Control and Prevention (CDC) guidelines recommend testing for chlamydia and gonorrhea and performing UA and urine culture on all patients with suspected epididymo-orchitis.6 Since there is no gold standard test for the diagnosis of epididymo-orchitis, it has been difficult to determine the sensitivity and specificity of UA and ultrasound for this disease. Using surrogate gold standards, prior studies have estimated the sensitivity of ultrasound for epididymo-orchitis to be from 69% to 93% and the specificity to be from 86% to 92%.1,7-9 The test characteristics of UA for epididymo-orchitis are uncertain.
Thus, to obtain a better understanding of the diagnostic utility of ultrasound and UA in patients with acute scrotal pain, we performed a chart review study to estimate the sensitivity and specificity of ultrasound and UA for epididymo-orchitis. We also attempted to estimate how often a UA changes the management of patients presenting to the emergency department (ED) with acute scrotal pain.
Materials and Methods
This was a retrospective chart review of consecutive patients presenting to a single academic, county hospital’s adult and pediatric EDs with testicular/scrotal pain over a year period (2016). This study was approved by the institutional review board of the University Medical Center of Southern Nevada and was deemed exempt from full review given the retrospective nature of the review. As such, we did not require informed consent; patient data confidentiality was maintained in accordance with the Declaration of Helsinki.
In this institution, by policy, all patients with acute scrotal pain get an ultrasound. Therefore, by obtaining a list of all patients who had a testicular ultrasound ordered, we also were able to identify all patients presenting with acute scrotal pain. After identifying these patients, research assistants performed a comprehensive chart review. The physician investigators trained two student research assistants to perform chart abstraction. These abstractors were blinded to the study hypothesis. A standardized data collection form was used; there was an associated data dictionary so that all terms were defined. After the initial training of the abstractors, a sample of 50 charts from each abstractor was audited by a physician investigator to assess for accuracy. Additionally, a sample of 50 charts were reviewed by both abstractors to determine interrater reliability.
The abstractors gathered the following data from each of these charts: age, UA results (if ordered), urine culture results (if ordered), ultrasound results, final diagnosis, and antibiotics given (if any). The “final diagnosis” was defined as the diagnosis related to the patient’s scrotal pain on the last available note in the electronic medical records. For admitted patients, this was the admitting physician’s last note (generally a discharge summary). For patients discharged from the ED, the final diagnosis was that listed on the emergency physician’s note. Abstracted data were anonymized.
To determine if a UA was positive or negative, data on specific components of the UA were obtained (nitrites, leukocyte esterase, white blood cells [WBC], and bacteria). There are institutional differences in UA terminology; our institution utilizes categories as follows for WBC: 0–8, 8–25, 26–50, 50–99, and too numerous to count (TNTC). For bacteria, the categories are none, rare, few, moderate, many, and TNTC. The definition of a positive UA is inconsistent in the literature. For example, some studies define a positive urine dipstick as requiring 1+ leukocytes or positive nitrites,10,11 while other studies only require trace leukocytes or positive nitrites12,13 for a positive result. For this study, we considered a UA to be positive if leukocyte esterase was at least 1+, WBCs were at least 8–25, nitrite was positive, or bacteria were at least “few.”
Traditionally, urine cultures have been considered positive if ≥100,000 CFU/mL to differentiate contaminants and true bacteriuria.14,15 However, more recent data have suggested the cutoff may be lowered to 100 CFU/mL if a uropathogen is present.16 Therefore, our definition of a positive urine culture was any bacteria at ≥100,000 CFU/mL and ≥100 CFU/mL for uropathogens.
For all cases in which UA results were available, the research assistant determined if the UA could have changed management of the patient. A UA was considered to have potentially changed the management of the patient (namely, antibiotics or not) if either of the following were true.
- The UA was positive; the ultrasound did not show epididymo-orchitis; and the patient got antibiotics for epididymo-orchitis (presumably because of the positive UA).
- The ultrasound showed epididymo-orchitis; the UA was normal; and the provider decided NOT to give antibiotics (presumably because of the negative UA).
Data were tabulated in Microsoft Excel (Version 15, Microsoft, Redmond, WA). The data were uploaded into a statistical program called “R” for calculations. There were two objectives of this study. First, we sought to estimate the sensitivity and specificity of UA and ultrasound for the diagnosis of epididymo-orchitis using the final clinical diagnosis as the gold standard. Second, we attempted to determine the percentage of patients presenting with acute scrotal pain for whom the UA may have changed management of the patient.
Results
During the 2016 calendar year, 663 patients who presented to the adult or pediatric ED for scrotal pain were identified. All of these patients had a testicular ultrasound done. In total, 536 (80.8%) of these patients were adults, and 127 (19.2%) were pediatric. The median age was 34 years (IQR: 21.5 to 50.0 years).
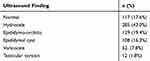
Amongst the 663 ultrasounds, 117 (17.6%) were read as normal, and 129 (19.4%) were read as showing epididymo-orchitis. Table 1 demonstrates the ultrasound findings in more detail.
Of the 663 scrotal pain patients, 458 patients (69.1%) had a urinalysis done, and 121 of those UAs (26.4%) met our criteria as positive. Only 64 urine cultures were performed, and 9 were positive (12.5%). In only two of the nine cases in which the urine culture was positive was the patient diagnosed with epididymo-orchitis.
A total of 151 of 663 patients (22.8%) were given a final discharge diagnosis of epididymo-orchitis. However, 154 patients received antibiotics to cover for epididymo-orchitis. This occurred as 15 patients who were not formally diagnosed with epididymo-orchitis were still treated with antibiotics for epididymo-orchitis. Such patients were generally diagnosed with nonspecific testicular pain or scrotal pain. At the same time, 12 patients were diagnosed with epididymo-orchitis, and did not receive antibiotics. Of note, two of these patients eloped from the department after the diagnosis was made but before antibiotics could be given. Of the remaining 10 diagnosed with epididymo-orchitis who did not receive antibiotics, seven were pediatric patients, and six of those seven pediatric patients had negative UAs.
Using the final diagnosis as the gold standard for determining whether or not the patient actually had epididymo-orchitis allowed us to calculate test characteristics for UA and ultrasound. For UA, the sensitivity was 58.2% (95% CI 48.9% to 67.1%) and the specificity was 85.1% (95% CI 80.8% to 88.7%). For ultrasound, the sensitivity was 78.8% (95% CI 71.4% to 85.0%), and the specificity was 98.1% (95% CI 96.4% to 99.1%). See Tables 2 and 3 for details regarding the calculations of the test characteristics of UA and ultrasound.
 |
Table 2 Shows a 2×2 Table for UA and Epididymitis-Orchitis. Sensitivity Is 58.2%, Specificity Is 85.1% for the Diagnosis of Epididymitis-Orchitis Using UA |
 |
Table 3 Shows a 2×2 Table for Ultrasound and Epididymitis-Orchitis. Sensitivity Is 78.8% and Specificity Is 98.1% for the Diagnosis of Epididymitis-Orchitis Using Ultrasound |
The relationship between UA results and epididymo-orchitis diagnosis differed between adult and pediatric patients. Of the 19 pediatric patients diagnosed with epididymo-orchitis, 16 had UAs, and just 2/16 were positive (both teenagers). Of the 132 adult patients diagnosed with epididymo-orchitis, 106 adults had UAs, and 69/106 (65%) had positive UAs.
In the 458 cases in which a urinalysis was obtained, the UA could have changed management in 24 cases (5.2% [95% CI 3.4% to 7.7%]). One patient (also mentioned above) had a negative UA and positive ultrasound and did not get antibiotics, possibly because he eloped from the ED before the provider had a chance to give antibiotics. As this still met our definition of “changed management,” he was counted among the 24 patients.
Finally, based on the 50 charts reviewed by both abstractors, inter-rater reliability was assessed using the datapoint of whether or not the urinalysis changed management. The kappa was found to be 0.96. Amongst 100 charts audited by the physician investigator, there was only 1 case, in which the physician investigator’s decision as to whether or not the urinalysis changed management differed from the abstractors’ decision.
Discussion
This is one of only a few studies1,7-9 that have attempted to estimate the test characteristics of ultrasound for epididymo-orchitis, and it contains a larger number of scrotal pain patients who had ultrasounds done than any of the previous studies. The sensitivity found in this study of 78.8% is in line with that reported in other studies while the specificity we found of 98.1% is a little higher than previously reported.1,7-9 While our means of calculating the sensitivity and specificity were suboptimal (as discussed further below), it is notable that ultrasound was both more sensitive and more specific for epididymo-orchitis than UA. Given that ultrasound is the primary means of diagnosing all sorts of other scrotal pathology (testicular torsion, testicular tumors, hydroceles, etc.), the role of the UA in the evaluation of patients with scrotal pain is quite narrow.
Indeed, this is the first study to attempt to assess the usefulness of the UA for patients of all ages presenting with acute scrotal pain to the ED. One prior study specifically evaluated the utility of the UA in pediatric patients with epididymitis.17 It found that pyuria and positive urine cultures were rare in pediatric epididymitis. The authors recommended that a UA and urine culture be routinely performed as antibiotics can be withheld unless there is pyuria or a positive urine culture.17 The question of whether or not to give antibiotics to pediatric patients with epididymitis is important, but this study asks an even more basic question: is UA needed at all for evaluating patients with scrotal pain (and possible epididymo-orchitis)?
A UA may sometimes change the management of a patient with acute scrotal pain (about 5% of the time based on our results), and given that it is a fairly cheap and noninvasive test, it seems reasonable to continue to consider a UA as part of the evaluation of patients with acute scrotal pain. In particular, a UA may be useful in pediatric patients with scrotal pain as a means to avoid antibiotics if the UA is negative (even in the setting of an ultrasound showing epididymitis-orchitis) as epididymitis-orchitis is less commonly of bacterial origin in prepubertal children.17–19 With that being said, despite recommendations to routinely order a UA for patients with acute scrotal pain,2–4 many physicians already forgo this test. In our study, 69% had a urinalysis done, and in a different retrospective study assessing the evaluation of acute scrotal pain, only 48% of patients had a UA performed.20 Therefore, while the data do not prove that skipping a UA is the right move, they do show that it is already commonplace not to order a UA on all scrotal pain patients. Considering this and the relatively infrequent cases in which a UA changes management of acute scrotal pain patients, recommendations that absolutely require a UA for scrotal pain are probably overstated.
When interpreting the results of this study, there are some limitations to consider. First of all, its nature as a chart review study could have resulted in unrecognized bias or confounders. In particular, our calculations of the test characteristics of UA and ultrasound were based on a false gold standard (ED diagnosis). However, there is no true gold standard test for the diagnosis of epididymo-orchitis, which is made through a combination of clinical findings and diagnostic test results. Thus, all studies attempting to calculate the sensitivity and specificity for UA and ultrasound have been limited. Next, while our institution has a policy that all patients with scrotal pain get an ultrasound, we cannot guarantee this policy was strictly followed. We may have thus obtained a biased sample of scrotal pain patients with more concerning clinical presentations than all-comers. Additionally, as discussed above, our definition of “changed management” was based upon how the UA results could have been used to change management, and our findings do not necessarily indicate that the UA actually changed the provider’s management. Finally, no clinical symptoms or examination findings were abstracted. While the inclusion of additional clinical findings would have complicated this study, such information may also have provided more context to help determine why providers managed patients in the ways they did.
Conclusion
Testicular ultrasound is more sensitive and specific than UA for epididymo-orchitis. Given this and the fact that ultrasound allows for assessment of a number of other causes of scrotal pain, including testicular torsion, ultrasound should remain the test of choice for the evaluation of acute scrotal pain. A UA may occasionally have utility for patients with possible epididymo-orchitis, but may not be needed on all patients presenting with scrotal pain. Determining which scrotal pain patients should get UAs, and which epididymo-orchitis patients should get antibiotics will require prospective evaluation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Agrawal A, Tripathi P, Shankhwar A, et al. Role of ultrasound with color doppler in acute scrotum management. J Family Med Prim Care. 2014;3(4):409–412. doi:10.4103/2249-4863.148130
2. Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol. 2015;56(1):3–11. doi:10.4111/kju.2015.56.1.3
3. Eyre R. Evaluation of the acute scrotum in adults. In H. Libman (Ed.). UpToDate. Available from: https://www.uptodate.com/contents/evaluation-of-the-acute-scrotum-in-adults.
4. Haecker F, Hauri-Hohl A, Schweinitz D. Acute epididymitis in children: a 4-year retrospective study. Eur J Pediatr Surg. 2005;15(3):180–186. doi:10.1055/s-2004-830355
5. Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583.
6. Epididymitis – 2015 STD treatment guidelines. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/std/tg2015/epididymitis.htm.
7. Wilbert DM, Schaerfe CW, Stern WD, et al. Evaluation of the acute scrotum by color-coded Doppler ultrasonography. J Urol. 1993;149:1475–1477. doi:10.1016/S0022-5347(17)36420-0
8. Ciftci AO, Senocak ME, Tanyel FC, et al. Clinical predictors for differential diagnosis of acute scrotum. Eur J Pediatr Surg. 2004;14:333–338. doi:10.1055/s-2004-821210
9. Smith RP, Tracy CR, Kavoussi PK, et al. The impact of color Doppler ultrasound on treatment patterns of epididymitis in a university-based healthcare system. Indian J Urol. 2013;29(1):22–26. doi:10.4103/0970-1591.109979
10. Frazee BW, Enriquez K, Ng V, et al. Abnormal urinalysis results are common, regardless of specimen collection technique in women without urinary tract infections. J Emerg Med. 2015;48(6):706–711. doi:10.1016/j.jemermed.2015.02.020
11. Tomas ME, Getman D, Donskey CJ, et al. Overdiagnosis of urinary tract infection and underdiagnosis of sexually transmitted infection in adult women presenting to an emergency department. J Clin Microbiol. 2015;53(8):2686–2692. doi:10.1128/JCM.00670-15
12. Blum RN, Wright RA. Detection of pyuria in symptomatic ambulatory women. J Gen Int Med. 1992;7:140–144. doi:10.1007/BF02598002
13. Shimoni Z, Glick J, Hermush V, et al. Sensitivity of the dipstick in detecting bacteremic urinary tract infections in elderly hospitalized patients. PLoS One. 2017;12(10):e0187381. doi:10.1371/journal.pone.0187381
14. Monzon OT, Ory EM, Dobson HL, et al. A comparison of bacterial counts of the urine obtained by needle aspiration of the bladder, catheterization and midstream-voided methods. N Engl J Med. 1958;259:764–767. doi:10.1056/NEJM195810162591603
15. Kass EH. Asymptomatic infections of the urinary tract. Trans Assoc Am Physicians. 1956;69:56–64.
16. Hooton T, Roberts P, Cox M, et al. Voided midstream urine culture and acute cystitis in premenopausal women. N Engl J Med. 2013;369(20):1883–1891. doi:10.1056/NEJMoa1302186
17. Joo JM, Yang SH, Kang TW, et al. Acute epididymitis in children: the role of the urine test. Korean J Urol. 2013;54(2):135–138. doi:10.4111/kju.2013.54.2.135
18. Santillanes G, Gausche-Hill M, Lewis RJ. Are antibiotics necessary for pediatric epididymitis? Pediatr Emerg Care. 2011;27:174–178. doi:10.1097/PEC.0b013e31820d647a
19. Cristoforo T. Evaluating the necessity of antibiotics in the treatment of acute epididymitis in pediatric patients. Pediatr Emerg Care. 2017. doi:10.1097/PEC.0000000000001018
20. Lorenzo L, Rogel R, Sanchez-Gonzalez J, et al. Evaluation of adult acute scrotum in the emergency room: clinical characteristics, diagnosis, management, and costs. Urology. 2016;94:36–41. doi:10.1016/j.urology.2016.05.018
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.