Back to Journals » Journal of Pain Research » Volume 15
Misinterpretation of the “Overdose Crisis” Continues to Fuel Misunderstanding of the Role of Prescription Opioids
Authors Bettinger JJ, Amarquaye W, Fudin J , Schatman ME
Received 24 March 2022
Accepted for publication 29 March 2022
Published 5 April 2022 Volume 2022:15 Pages 949—958
DOI https://doi.org/10.2147/JPR.S367753
Checked for plagiarism Yes
Editor who approved publication: Dr Robert Twillman
Jeffrey J Bettinger,1 William Amarquaye,2 Jeffrey Fudin,3– 6 Michael E Schatman7– 9
1Saratoga Hospital Medical Group, Saratoga Springs, NY, USA; 2HCA Florida Brandon Hospital, Brandon, FL, USA; 3President, Remitigate Therapeutics, Delmar, NY, USA; 4Department of Pharmacy Practice, Albany College of Pharmacy & Health Sciences, Albany, NY, USA; 5Department of Pharmacy Practice, Western New England University College of Pharmacy, Springfield, MA, USA; 6Department of Pharmacy and Pain Management, Stratton VA Medical Center, Albany, NY, USA; 7Department of Anesthesiology, Perioperative Care, and Pain Medicine, NYU Grossman School of Medicine, New York, NY, USA; 8Department of Population Health – Division of Medical Ethics, NYU Grossman School of Medicine, New York, NY, USA; 9School of Social Work, North Carolina State University, Raleigh, NC, USA
Correspondence: Michael E Schatman, Department of Anesthesiology, Perioperative Care, and Pain Medicine, NYU Grossman School of Medicine, 550 1st Ave., New York, NY, 10016, USA, Tel +425-647-4880, Email [email protected]
Introduction
The United States overdose epidemic hit yet another devastating record in 2021, with drug overdose deaths surpassing 100,000 for the first time in history, representing almost a 21% increase compared to 2020.1 While undoubtedly several societal, personal, and behavioral phenomena highlighted and created by the COVID-19 pandemic have contributed to the sharp incline in overdoses our nation has witnessed over the past two years, it is imperative to recognize that all cause opioid-related overdose death rates had been rising precipitously since 2014.1 There are a variety of factors that have influenced the progressive pacing of opioid-related overdoses witnessed throughout the second decade of the 21st century. Perhaps the most significant has been the introduction and availability of illicitly manufactured synthetic opioid products (namely “fentalogues”),2,3 although additional contributors include increasing rates of polysubstance abuse,2–5 continued poor access to medication assisted treatments and behavioral health supports,6 and restrictions and reductions of legitimate opioid access when clinically indicated.7–11
Despite the multifactorial nature of the current overdose epidemic, there continues to be a disturbing and disproportionate narrative pertaining to the involvement and overall influence of opioid prescribing. A trend in misinformation has affected almost all facets of society, from politics to healthcare. Accordingly, it should not be surprising that the opioid overdose crisis has also been entangled in a messy web of a politicized revenue stream associated with lawsuits by various states and other municipalities, and the law firms and expert witnesses that frequently and repeatedly participate.12 One of the most notorious groups that continues to perpetuate false narratives regarding the prescribing of opioids is Physicians for Responsible Opioid Prescribing (PROP).13 However, they are certainly not alone in the persistent misinterpretation and misrepresentation of data and shared responsibility for adverse consequences such as increased suicidality and escalated use of non-prescription opioids, particularly those containing fentalogues that are the most frequent cause of accidental overdoses and deaths.1–3,10,11 This editorial will address several ongoing false narratives regarding opioid prescribing and its involvement in the ongoing overdose epidemic. We utilize specific quotations excerpted from a recent press release by the PROP organization that best highlight the falsehoods that too many legislators and media outlets are sadly accepting as accurate information.13
Prevention may be even more important, and decreasing new opioid prescriptions is key to ending this [overdose] epidemic... a conventional view is that the prescription opioid crisis is over. In fact, deaths due to prescription opioids have continuously increased from 1999 through 2017.13
The concept of “prevention” by means of reducing prescription and supplies of opioids as a way to end the opioid crisis (often hyperbolically identified as the “opioid epidemic”) continues to be a running narrative put forth by several organizations. It is one that is quite puzzling, particularly in the context of the above excerpt,13 as there is concomitantly an acknowledgement that approximately 99% of fentanyl-related deaths now involve illicitly synthesized fentalogues.14 It is well-accepted in scientific circles that current overdose deaths involve fentanyl-related compounds that are illicitly manufactured and not FDA approved pharmaceutical fentanyl (or its FDA approved chemical derivatives alfentanil, remifentanil, and sufentanil) used in both acute and chronic settings.2,14,15 This is a distinction that must be accurately described in order to diminish untoward apprehension in prescribing pharmaceutical fentanyl and its related compounds safely in a both monitored clinical settings and for home use.
Despite the acknowledgement that fentalogues are now involved in “almost all opioid-related overdose deaths” in the aforementioned excerpt,14 it is disingenuously claimed that the reason why “prevention” (in terms of reducing prescription opioids) is supported is the “fact” that “prescription opioid deaths have been increasing from 1999 through 2017”.13 Not only is this characterization inaccurate, but it is vastly generalized and lacking clarity. The primary shortcoming of such a statement is that the terminology of “deaths due to prescriptions opioids” is neither specifically defined nor clear. This is an important reality that is often ignored when assessing overdoses, as, perhaps most importantly, there is usually no way (or attempt) to actually verify whether patients overdosed on opioids that were prescribed to them, opioids that were prescribed to someone else that they obtained illicitly, opioids manufactured illicitly, or a combination thereof.1 Accordingly, even to label the category of overdoses involving “natural and semi-synthetic opioids” as “prescription opioids” (which it appears PROP has attempted to conjecture in their news release) is misleading and unequivocally false. However, this type of “slight of hand” is persistently used by anti-opioid factions, as the narrative is “convenient” for them, albeit false.
Adding to the lack of clarity resulting from such mislabeling of “prescription opioid deaths” is that the majority of drug overdose deaths appear to involve more than one substance.2–5,14 Drug deaths involving polysubstances propagate spurious correlations and false narratives regarding which drug or drugs contributed to the actual death. When one examines toxicology reports, multiple drugs are generally found postmortem in the deceased, particularly when an opioid is involved. In fact, there is evidence that a substantial proportion of opioid-related deaths have often involved polysubstance use over the past several decades.16 The practice of mixing opioids with psychostimulants was reported as early as the 1950s,17 with postmortem studies finding almost half of heroin overdose deaths in San Francisco involved ethanol in the 1970s,18 with multiple reports from various cities revealing that more than half of drug overdose deaths involved more than one substance throughout the 1990s.19–21 These trends in polysubstance overdose deaths have continued to persist throughout the 21st century.22–25 One of the more recent of these studies, by Hannah et al in 2017,26 determined that among death certificates examined in Marin County, California the average number of drugs identified in the toxicology screens of all 34 drug overdose deaths attributed to opioids was 6. Despite all of this evidence, the Centers for Disease Control (CDC) acknowledges that when overdose deaths involve more than one drug, a single death will be included in more than one category,1 creating greater confusion when actually attempting to label any given overdose.
In addition to such issues when considering attempts at labeling overdose deaths, there is the deficiency in the analysis by PROP of the characterization of the trajectory of “prescription opioid deaths” itself. It is stated that “prescription opioid deaths” have continuously increased from “1999 through 2017”, yet more recent data indicate that natural and semisynthetic opioid overdose deaths (to which they refer as “prescription opioid deaths”) have been stable or declining since 2015.1,2,27 Seth et al determined that longitudinal trends indicated a rapid increase in death rates involving synthetic opioids from 2013–2016 vs death rates involving natural and semisynthetic opioids, which remained relatively stable from 2009–2016, with an annual percent increase of 3.4%.27 More recently, particularly throughout the COVID-19 pandemic which has increased isolation and limited access to healthcare providers, overdose deaths have continued to increase dramatically. Freidman et al utilized provisional records from the CDC in order to determine the magnitude of the increase in monthly drug related overdose mortality during the COVID-19 pandemic.28 They determined that 9192 people died from drug overdose in May of 2020, making it the deadliest month on record and representing a 57.7% increase over May of 2019.28 These numbers have only continued to worsen, despite the annual number of opioid prescriptions drastically decreasing over the past several years (see Figure 1 below).29
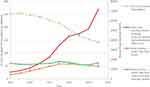 |
Figure 1 Changes in Annual Opioid Prescriptions Compared to Overdose Death Rates from Different Types of Opioids. Notes: Reproduced from CDC Drug Overdose: US Opioid Dispensing Rate Map [Internet]. CDC. Nov 2021 (accessed Feb 2022). Available from: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html.29 |
Thus, for any organization to consistently implicate prescription opioid use alone in an attempt to explain dramatic increases in drug overdose deaths continues to discount salient variables regarding other drugs that are implicated in such deaths, and how strongly the ongoing and worsening crisis correlates to each variable. Health experts have discussed the importance of capturing correct terminology when discussing opioid overdose deaths, including Peppin et al in 2020.16 Their assertion that,
this terminology is too simplistic and now woefully outdated. It understates the complexities of these deaths, and the fact that the majority of overdose deaths currently involve multiple substances 16 (pg. 3405) is holistically true and vastly salient.
After the CDC released its 2016 guideline on opioid prescribing and related state and local prescribing guidelines reduced US opioid prescribing, deaths from prescribed opioids substantially declined in 2018 and 2019 for the first time in almost two decades.13
For any organization to assess the overall “impact” of the 2016 Guideline on opioid prescribing by only evaluating trends in “deaths from prescribed opioids” in a two-year span is, again, misguided and statistically inaccurate. It also highlights the need to differentiate correlation from causation. An attempt to correlate two points without any further context, or assessment of any other variable intrinsically entwined, does not actually necessitate that one has caused the other. Further, simply isolating one year from the wider context of drug overdose death trajectories for the past ten years completely misrepresents sound science. Data published in the CDC Morbidity and Mortality Weekly Report (MMWR) in February of 2021 indicate that from 2013 through 2019, the age-adjusted rate of deaths involving synthetic opioids other than methadone increased by 1040%,30 while US annual opioid prescriptions have been drastically reduced since 2012 (again, see Figure 1).29 Therefore, if we were to utilize the same flawed practices of correlating these two data points while conflating correlation with causality, one would inaccurately conclude that reductions in opioid prescriptions result in increasing rates of overdose deaths. While there certainly may be some truth to this in regard to stable and adherent pain patients who were involuntarily tapered and compelled to turn to the streets for relief, this, in and by itself, does not fully explain a steady rise in opioid overdose deaths. It is easy to be misled by such spurious correlations. By way of example, in 2017 Raouf succinctly noted that Cost of Bananas v. Deaths Caused by Opioids, Points Scored by Losing Teams in Super Bowls v. Deaths Caused by Opioids, and Cost of 16 Ounce Bags of Potato Chips v. Deaths Caused by Opioids are all nonsensical correlations without scientific merit.31
A more thorough evaluation of the “impact” of the 2016 CDC Opioid Prescribing Guideline represents a more damning picture with unintended consequences that followed. This has been labeled as the Guideline’s “weaponization”,32 and while there have been several reviews published that have detailed the concerns associated with these unintended consequences,7,8,33 a detailed analysis is beyond the scope of this article. However, one of the most damaging aspects of the CDC Guideline was the misapplication to patient groups for whom the Guideline was not intended. Notwithstanding, patients already prescribed over a 90 milligram morphine equivalent dosage (MEDD), patients with sickle cell disease or cancer pain, patients undergoing palliative care or being treated postoperatively, have all been adversely affected.8,33 In fact, there were so many problems with unintended consequences of the Guideline that the original authors wrote a clarification in 2019 in the New England Journal of Medicine.34 One excerpt specifically states,
The panel also noted the potential for misapplication of the recommendations to populations outside the scope of the Guideline. Such misapplication has been reported for patients with pain associated with cancer, surgical procedures, or acute sickle cell crises. There have also been reports of misapplication of the Guideline’s dosage thresholds to opioid agonists for treatment of Opioid Use Disorders. Such actions are likely to result in harm to patients. (pg. 2285)34
All of this unnecessary suffering could have been prevented had the CDC followed procedures in the selection of the original panel35 and had they heeded the warning posted by several professional pain organizations that were posted on the Federal Register in response to the proposed Guideline.36
Another unfortunate consequence of the Guideline has been shifting federal and state opioid-related policies and health insurer and community pharmacy limitations on opioid prescribing, particularly among those attempting to define maximum MEDD. A study published by Duensing et al assessed such policies from 2016–2018, finding that 527 opioid related policies were approved during this time with 170 specifically imposing limits on opioid prescribing.37 Additionally, 35 of these policies specifically mentioned or integrated the CDC Opioid Prescribing Guideline to support their narratives.35 This is concerning due to the inherent problems associated with the use of “MEDD”, as there are significant gaps in absolute dose equivalents, variability between different calculators themselves, and unknowns in terms of equivalence from an adverse effect perspective.38–41 Utilizing MEDD incorrectly by many of these government entities, third party payers, and insurance stakeholders has also allowed for the development of metrics that measure outcomes in terms of reducing overall equivalent doses (by reducing prescribing) as opposed to other patient-centered outcomes. These flaws in MEDD were recognized by the US Food and Drug Administration (FDA) and several other government agencies in a 2-day seminar titled, “Morphine Milligram Equivalents: Current Applications and Knowledge Gaps, Research Opportunities, and Future Directions”.42
While reducing opioid prescribing may reduce risks and overdoses in some cases, it has quickly become used as one of the only metrics when considering decreasing risks and overdoses, which does not fully convey the clinical picture. In a study conducted by Oliva et al at the Veterans Health Administration, the authors determined that patients were at an increased risk of death from overdose or suicide after prescription opioid treatment was discontinued.10 Further, Agnoli et al in 2021 retrospectively analyzed a cohort of more than 100,000 patients previously receiving long-term opioid therapy, and determined that during the post-tapering period, tapered patients experienced an adjusted incidence rate of 9.3 overdose events per 100 person-years compared with 5.5 events per 100 person-years in the non-tapered periods [95% CI, 3.0–4.6]; alRR, 1.68 [95% CI, 1.53–1.85].11 Tapering itself was associated with significantly greater incidence rates of mental health crises, as well.11 These are some of the intrinsic risks when blanket metrics and policies that evade patient centered care and outcomes are applied, and it is imperative that we understand the absolute detriment that can be caused by misrepresentation of data.
The US uses more Rx opioids than any country in the world.13
This is a narrative that continues to be perpetuated by various pain organizations, within academic journals and media outlets, and is one that is old and, quite frankly, meaningless. These include the often quoted “statistic” that,
The United States, representing less than 5% of the world’s population, are by far the largest group of opioid users consuming 80% of the world’s supply of opioids,
as well as the insinuation that, “Americans use 99% of the hydrocodone available globally”.43–47Do these organizations, news outlets, and journal articles intend to state that the US leads the world in annual opioid prescriptions as a numerical number without accounting for number of citizens? Or, are they referring to “prescription opioids” as a “defined daily dosage” in terms of the “assumed average maintenance dose per day” for an opioid used for “its main indication in adults”? Are they differentiating between opioid prescriptions for acute and/or perioperative use versus those for chronic pain? What about palliative care/hospice/cancer related pain? Or, are they simply lumping all opioid prescriptions prescribed for any type of pain together in order to be able to make specific statements that represent intentional misinterpretations of the data?
It is scientifically and practically disturbing that these types of statements are widely made regarding opioid prescribing, considering that globally, one of the strongest indicators of pain management adequacy used by both the World Health Organization (WHO) and the International Narcotics Control Board is access to opioids.48–50 Adequate access to opioids worldwide had become of such critical importance at the end of the 20th century that in 2005, the WHO was asked to prepare a study on the medical needs for opioids and the appropriate quantities of opioids required for medical purposes.51 Thus, in 2011, Seya et al published their measure of opioid adequacy (the Adequacy of Consumption Measure (ACM)), which combines opioid consumption statistics with country-specific morbidity.52 This measure was most recently updated by Scholten et al in 2019.49 They defined their Adequacy of Opioid Consumption (AOC) Index as the per-capita consumption level for the 20 most-developed countries (with the notion that the most-developed countries on average should achieve the best public health outcomes) in 2015, where a value of 100 or greater was considered adequate consumption.49 Interestingly, and much to the chagrin of organizations like PROP, only 8% of the world’s population were found to be living in countries with adequate consumption, whereby 81% of the world live in countries with low to extremely low consumption.49 Furthermore, for 2015, Germany, Canada, and Austria had the highest AOC Indexes (304, 271, and 216, respectively) of all of the countries in the world, thus dismantling the false narrative that the US still uses “more opioid prescriptions then the rest of the world”.49 These data also make the comparison itself almost entirely irrelevant, as they are attempting to compare a country that has well established and undisputed opioid adequacy (the United States) to the rest of the world, of which the majority have low to extremely low opioid adequacy.
The claim that “Americans use 99% of the hydrocodone available globally” again neglects some very important information and is also misleading. Hydrocodone prescribing, similar to total opioid prescribing, has shown multiyear declines since 2011 in the US, with annual prescriptions decreasing by 50.9% from 2011 (144.5 million annual prescriptions) to 2018 (70.9 million annual prescriptions).53,54 These trends have continued through 2020.55 It is clear that hydrocodone consumption in the US continues to remain much higher compared to other parts of the world. However, this is not surprising, considering that there are several examples of countries having preference for other opioids that are less commonly used in the US. For the sake of comparison, in Europe and Asia it is far more common to see prescriptions for dihydrocodeine, a codeine derivative that is a less potent analgesic than hydrocodone and used for mild to moderate pain, or simply morphine itself.55 In fact, Japan, the United Kingdom, the Republic of Korea, and China accounted for 94.6% of the global dihydrocodeine consumption in 2020.55 Sweden and Belgium, in contrast, are much greater utilizers of ethylmorphine, another semi-synthetic opioid used for analgesic purposes, as those 2 nations accounted for 60.6% of its global consumption in 2020 (France, Hungary, Poland, India, and Hong Kong accounted for the remaining 39.4%).55 Even heroin, which is used to treat opiate dependency and for analgesia in other countries, is much less commonly utilized in the US comparatively, as Sweden itself made up 55% of therapeutic global heroin consumption in 2020, followed by the Netherlands (18.5%), Germany (18.2%), Canada (3.9%), the United Kingdom (2.5%), and Luxembourg (1.5%).55 It is difficult to absolutely explain hydrocodone preference in the US compared to the rest of the world; however, disingenuously continuing to cite this simple statistic in isolation without further context is another example of adding to opioid hysteria without understanding worldwide opioid preferences or trends themselves.
Amplifying this misrepresentation, it is also crucial to consider that US opioid prescribing itself has been sharply declining since 2012, with the number of annual US opioid prescriptions in 2020 having been reduced to half of what they were in 2012 (again, see Figure 1).29 Comparatively, opioid consumption rose by nearly 40% in the European Union from 2001 to 2013, and prescription opioid sales in Italy tripled throughout this period, as well.56 In France, prescription oxycodone use increased by 1950% between 2004 and 2017.57 Further, more recently, in countries such as Israel, Greece, and Portugal, prescription opioid use continued increasing by more than 50% between 2011 and 2016.58 Therefore, it is short-sighted and disingenuous for anti-opioidists to continue perpetuating nonsensical and fear-mongering rhetoric pertaining to the use of opioids in the US compared to the rest of the world, as certain parts of the world have also witnessed increasing rates of opioid prescribing.
The best evidence now shows that prescription opioids are ineffective for long-term management of common chronic pain conditions, such as osteoarthritis and low back pain.(6)13
Finally, we will comment on one of the final excerpts from PROP’s news release regarding “best evidence” as it relates to the effectiveness of opioids, and a point that is often used as justification for tapering/discontinuing established opioid regimens or to refusing prescription of opioids altogether.13 We should actually define what is meant by “long-term evidence” first, as, to date, there has not been a single, randomized, controlled trial directly assessing the effectiveness of chronic opioids in the management of chronic pain with a duration of greater than a year. This is important in that the claim often made pertains to how “opioids are not effective when used long-term”, although there is no actual empirical evidence to support such a claim. This was highlighted in a review by Furlan et al in 2011,59 which determined that of 62 trials assessing opioid efficacy for chronic noncancer pain, 51% were of one month duration or less, 39% were 5–12 weeks, and the remaining 9% were 13–24 weeks. This is not particularly surprising, considering a three-month duration clinical trial is the standard and the requirement for drug approval as outlined by the FDA.60 Accordingly, to truly analyze opioids’ potential efficacy for chronic pain, we are compelled to rely on the short-term clinical evidence that is available, as well as extension and open label trials. A more recent meta-analysis conducted by Meske et al in 2018 considered 15 RCTs assessing opioid use in chronic non-cancer pain. The authors concluded that opioids were significantly effective in reducing pain intensity and improving pain, while resulting in minor benefits in physical functioning.61 None of the trials from this meta-analysis were beyond 3 months duration, which actually is consistent with the body of evidence that supports the use of all treatments for chronic pain (non-opioid pharmacological and non-pharmacological modalities).61,62 This represents an anecdote various organizations seem to purposefully neglect in their narratives.
In addition to the body of evidence that provides support for opioid efficacy in the short term, longer term open label and extension trials (not randomized controlled) have demonstrated that opioids can provide sustained pain relief over a number of years.63–79 Opioids in varying formulations that have been studied in these types of clinical trials that demonstrate sustained analgesic effects include tapentadol,63,64 buprenorphine,65 oxycodone,66–68 oxymorphone,69 hydrocodone,70–74 hydromorphone,75,76 morphine,77 fentanyl,78 and tramadol79 in a wide range of chronic, noncancer pain conditions. Moreover, there are several one-year pivotal extension trials for various extended-release opioids that provide evidence of efficacy without a need to escalate after patients became stable.63,64,75,77 This formidable body of evidence belies the myth perpetrated by anti-opioidists that “everyone who starts on long-term opioid therapy will require progressively higher and unhealthy dosages”.
What is further disconcerting in regard to the above excerpt13 is that the cited “best evidence” is a RCT by Krebs et al published in 2018 (the SPACE trial).80 This was a 12-month randomized trial comparing pain and function efficacy of opioids versus non-opioids (oral NSAIDs, acetaminophen, etc) in 240 primarily male veteran patients with “moderate to severe” osteoarthritis-related back, knee, or hip pain.80 The study identified no significant difference in function throughout those twelve months between the two groups and found that pain level was significantly reduced in the non-opioid group, thus allegedly evidencing opioids’ non-superior efficacy.80 However, there are major and inherent flaws within the design, methodology, and execution of the study. These flaws have spawned several other reviews, editorials, and commentaries that have been published with the sole purpose of highlighting the study’s limitations and critiquing its utility from a clinical perspective.81–83 While the trial does constitute clinical trial evidence, its applicability is so constricted that it is impossible to draw any major conclusions from it.
This critique of Krebs et al is not meant to malign efforts to study opioids, non-opioids, and other pain management modalities for long-term use, particularly in comparison to each other. We strongly encourage continued research efforts in these areas to better understand all of the potential long-term efficacy and safety outcomes for all modalities used in the treatment of chronic pain. However, for this trial to continually be used as often the solitary piece of “best evidence” is not only negligent, but highlights a glaring ineptitude and likely bias of those that wield it to further their own agendas.
Conclusion
We endorse responsible prescribing and dispensing of medications of all types, including opioids; however we do not endorse propagating hysteria, deceitful use of clinical evidence or lack thereof, nor trying to influence the current pharmaceutical market for self-gain. The PROP News Release13 to which we refer throughout this analysis is fraught with gross inaccuracies, misrepresentation of data, and disregard for scientific integrity to the extent that we find it to be unconscionable. As we personally know many of the individuals responsible for this news release, we believe that at least a few of them are sufficiently adequate scientists to the extent that the picture that they have tried to paint was an intentionally inaccurate one, and that they should know better than to use deceit simply to express their misguided opinions. From an ethical perspective, we are deeply concerned that such egregious efforts are potentially damaging to vulnerable chronic pain sufferers who are already stigmatized and marginalized, thereby exacerbating their plight. Sadly, we do not believe that this analysis will serve as a catalyst for disingenuous anti-opioidists to change their ways. However, we hope that by continuing to expose the continuing falsehoods that are damaging to so many patients, the tide against opioids and those who suffer from intractable chronic pain will begin to turn in a more moderatist direction.
Disclosure
Jeffrey J Bettinger is part of the National Advisory Board for Hisamitsu America, Inc., and part of the Scientific Advisory Board for PainScript LLC., outside the submitted work. Jeffrey Fudin reports lecture, non-speakers’ bureau from Abbott Laboratories, acute perioperative pain (speakers bureau, consulting, advisory boards) from AcelRx Pharmaceuticals, collaborative publications, consulting, advisory boards from BioDelivery Sciences International, educational studio recording from Collegium Pharmaceutical, collaborative non-paid poster presentations, consulting from GlaxoSmithKline (GSK), part of advisory board for Hisamitsu America Inc and Hikma Pharmaceuticals, part of meeting registration support (ASHP 2021) for poster presentation for Lilly Pharmaceuticals, owned stocks from Modoscript, Inc, collaborative non-paid publications from Scilex Pharmaceuticals, speakers’ bureau, consultant, advisory boards from Salix Pharmaceuticals, and lecture, non-speakers’ bureau from Torrent Pharmaceuticals, during the conduct of the study. Michael E Schatman is a research consultant for Modoscript, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Centers for Disease Control and Prevention. CDC national center for health statistics: provisional drug overdose death counts [Internet]. Available from: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm#dashboard.
2. O’Donnell J, Tanz LJ, Gladden RM, et al. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70(50):1740–1746. doi:10.15585/mmwr.mm7050e3
3. Jones CM, Bekheet F, Park JN, Alexander GC. The evolving overdose epidemic: synthetic opioids and rising stimulant-related harms. Epidemiol Rev. 2020;42:154–166. doi:10.1093/epirev/mxaa011
4. Timko C, Han X, Woodhead E, Shelley A, Cucciare MA. Polysubstance use by stimulant users: health outcomes over three years. J Stud Alcohol Drugs. 2018;79:799–807. doi:10.15288/jsad.2018.79.799
5. O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital signs: characteristics of drug overdose deaths involving opioids and stimulants—24 states and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep. 2020;69:1189–1197. doi:10.15585/mmwr.mm6935a1
6. Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2020. Data on substance abuse treatment facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2021. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt35313/2020_NSSATS_FINAL.pdf.
7. Kroenke K, Alford DP, Argoff C, et al. Challenges with implementing the centers for disease control and prevention opioid guideline: a consensus panel report. Pain Med. 2019;20(4):724–735. doi:10.1093/pm/pny307
8. Darnall BD, Juurlink D, Kerns RD, et al. International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med. 2019;20(3):429–433. doi:10.1093/pm/pny228
9. Behar E, Bagnulo R, Knight K, et al. “Chasing the pain relief, not the high”: experiences managing pain after opioid reductions among patients with HIV and a history of substance use. PLoS One. 2020;15(3):e0230408. doi:10.1371/journal.pone.0230408
10. Oliva EM, Bowe T, Manhapra A, et al. Associations between stopping prescriptions for opioids, length of opioid treatment, and overdose or suicide deaths in US veterans: observational evaluation. BMJ. 2020;368:m283. doi:10.1136/bmj.m283
11. Agnoli A, Xing G, Tancredi DJ, et al. Association of dose tapering with overdose or mental health crisis among patients prescribed long-term opioids. JAMA. 2021;326(5):411–419. doi:10.1001/jama.2021.11013
12. Metzer S. Testimony of “paid expert” questioned by drugmaker [Internet]. The Journal Record; 2019. Available from: https://journalrecord.com/2019/06/17/testimony-of-paid-expert-questioned-by-drugmaker/.
13. PROP News Release. Prescription opioids continue to contribute to the rise in drug overdose deaths [Internet]. PROP; 2021. Available from: http://www.supportprop.org/opioid-news/prop-news-release-prescription-opioids-continue-to-contribute-to-the-rise-in-drug-overdose-deaths/.
14. O’Donnell J, Gladden RM, Kariisa M, Mattson CL. Using death scene and toxicology evidence to define involvement of heroin, pharmaceutical morphine, illicitly manufactured fentanyl and pharmaceutical fentanyl in opioid overdose deaths, 38 states and the District of Columbia, January 2018-December 2019. Addiction. 2021. doi:10.1111/add.15768
15. Persico AL, Wegrzyn EL, Fudin J, Schatman ME. Fentalogues. J Pain Res. 2020;13:2131–2133. doi:10.2147/JPR.S265901
16. Peppin JF, Raffa RB, Schatman ME. The polysubstance overdose-death crisis. J Pain Res. 2020;13:3405–3408. doi:10.2147/JPR.S295715
17. Piro L, Martinotti SG, Vannini R, et al. Substance screening in a sample of “clubbers”: discrepancies between self-reporting and urinalysis. Evid Based Psychiatric Care. 1954;120:10.
18. Baselt RC, Allison DJ, Wright JA, Scannell JR, Stephens BG. Acute heroin fatalities in San Francisco. Demographic and toxicologic characteristics. West J Med. 1975;122(6):455–458.
19. Taylor A, Frischer M, Goldberg D. Non-fatal overdosing is related to polydrug use in Glasgow. BMJ. 1996;313(7069):1400–1401. doi:10.1136/bmj.313.7069.1400b
20. Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98(6):739–747. doi:10.1046/j.1360-0443.2003.00376.x
21. Strang P, Griffiths P, Powis B, Fountain J, Williamson S, Gossop M. Which drugs cause overdose among opiate misusers? Study of personal and witnessed overdoses. Drug Alcohol Rev. 1999;18(3):253–261. doi:10.1080/09595239996383
22. Cone EJ, Fant RV, Rohay JM, et al. Oxycodone involvement in drug abuse deaths: a Dawn-based classification scheme applied to an oxycodone postmortem database containing over 1000 cases. J Anal Toxicol. 2003;27(2):
23. Cone EJ, Fant RV, Rohay JM, et al. Oxycodone involvement in drug abuse deaths. II. Evidence for toxic multiple drug-drug interactions. J Anal Toxicol. 2004;28(4):217–225. doi:10.1093/jat/28.4.217
24. Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2008;103(1):126–136. doi:10.1111/j.1360-0443.2007.02054.x
25. NYC Department of Health and Mental Hygiene. Illicit drug use in New York City. NYC Vital Signs. 2010;9(1):1–4.
26. Hannah HA, Arambula K, Ereman R, Harris D, Torres A, Willis M. Using local toxicology data for drug overdose mortality surveillance. Online J Public Health Inform. 2017;9(1):e143. doi:10.5210/ojphi.v9i1.7733
27. Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health. 2018;108(4):500–502. doi:10.2105/AJPH.2017.304265
28. Friedman J, Akre S. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January‒July 2020. Am J Public Health. 2021;111:1284–1291. doi:10.2105/AJPH.2021.306256
29. CDC Drug Overdose. US opioid dispensing rate map [Internet]. CDC; 2021. Available from: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html.
30. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. doi:10.15585/mmwr.mm7006a4
31. Fudin J, Raouf M. Alternative opioid facts and the new banana republic [Internet]. Paindr.com; 2017. Available from: https://paindr.com/alternative-opioid-facts-and-the-new-banana-republic/.
32. Schatman ME, Shapiro H. Damaging state legislation regarding opioids: the need to scrutinize sources of inaccurate information provided to lawmakers. J Pain Res. 2019;12:3049–3053. doi:10.2147/JPR.S235366
33. Kertesz SG, Satel SL, DeMicco J, Dart RC, Alford DP. Opioid discontinuation as an institutional mandate: questions and answers on why we wrote to the Centers for Disease Control and Prevention. Subst Abus. 2019;40(4):466–468. doi:10.1080/08897077.2019.1635973
34. Dowell D, Haegerich T, Chou R. No shortcuts to safer opioid prescribing. N Engl J Med. 2019;380(24):2285–2287. doi:10.1056/NEJMp1904190
35. Schatman ME, Ziegler SJ. Pain management, prescription opioid mortality, and the CDC: is the devil in the data? J Pain Res. 2017;10:2489–2495. doi:10.2147/JPR.S153322
36. Twillman R. AAPM CDC opioid guideline concerns [Internet letter]. American Academy of Pain Management; 2015. Available from: http://paindr.com/wp-content/uploads/2015/10/House-EC-CDC-Opioid-Guideline-Letter_AAPM-Twillman.pdf.
37. Duensing K, Twillman R, Ziegler S, et al. An examination of state and federal opioid analgesic and continuing education policies: 2016–2018. J Pain Res. 2020;13:2431–2442. doi:10.2147/JPR.S267448
38. Fudin J, Raouf M, Wegrzyn E, Schatman M. Safety concerns with centers for disease control opioid calculator. J Pain Res. 2018;11:1–4. doi:10.2147/JPR.S155444
39. Fudin J, Cleary JP, Schatman ME. The MEDD myth: the impact of pseudoscience on pain research and prescribing-guideline development. J Pain Res. 2016;9:153–156. doi:10.2147/JPR.S107794
40. Rennick A, Atkinson T, Cimino NM, et al. Variability in opioid equivalence calculations. Pain Med. 2016;17(5):892–898. doi:10.1111/pme.12920
41. Shaw K, Fudin J. Evaluation and comparison of online Equianalgesic opioid dose conversion calculators. Pract Pain Manag. 2013;13:61–66.
42. Morphine milligram equivalents. Current applications and knowledge gaps, research opportunities, and future directions [Internet]. FDA; 2021. Available from: https://www.fda.gov/drugs/news-events-human-drugs/morphine-milligram-equivalents-current-applications-and-knowledge-gaps-research-opportunities-and.
43. Minnesota Department of Health. Opioids: perception of pain [Internet]. Minnesota Department of Health; 2020. Available from: https://www.health.state.mn.us/communities/opioids/prevention/painperception.html.
44. Gusovsky D. Americans consume vast majority of the world’s opioids. CNBC; 2016. Available from: https://www.cnbc.com/2016/04/27/americans-consume-almost-all-of-the-global-opioid-supply.html.
45. International Narcotics Control Board, Narcotic Drugs. Hydrocodone is a long-acting opioid formulation used to treat severe pain for a prolonged duration, and is taken orally. Oxycodone is a synthetic analgesic drug used to treat moderate to severe pain. International Narcotics Control Board, Narcotic Drugs: estimated World Requirements for 2011, Statistics for 2009, The United Nations, Vienna, Austria; 2010. Available from: https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2010/Narcotic_drugs_publication_2010.pdf.
46. Duff JH, Tharakan SM, Davis-Castro CY, et al. Consumption of prescription opioids for pain: a comparison of opioid use in the United States and other countries [Internet]. Congressional Research Service; 2021. Available from: file:///Users/jeffreybettinger/Downloads/855318%20(1).pdf.
47. Mann B. Doctors and dentists still flooding US with opioid prescriptions [Internet]. NPR; 2020. Available from: https://www.npr.org/2020/07/17/887590699/doctors-and-dentists-still-flooding-u-s-with-opioid-prescriptions.
48. International Narcotics Control Board. Availability of internationally controlled drugs: ensuring adequate access for medical and scientific purposes [Internet]. INCB; 2015. Available from: http://www.incb.org/incb/en/publications/annual-reports/annual-report-supplement-2015.html.
49. Scholten WK, Christensen AE, Olesen AE, et al. Quantifying the adequacy of opioid analgesic consumption globally: an updated method and early findings. Am J Public Health. 2019;109(1):52–57.
50. Global atlas of palliative care at the end of life [Internet]. World Health Organization; 2014. Available from: https://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf.
51. International Narcotics Control Board. Recommendation 46. In: report of the International Narcotics Control Board for 2005. New York, NY: United Nations; 2006:97.
52. Seya MJ, Gelders SF, Achara OU, Milani B, Scholten WK. A first comparison between the consumption of and the need for opioid analgesics at country, regional, and global levels. J Pain Palliat Care Pharmacother. 2011;25(1):6–18. doi:10.3109/15360288.2010.536307
53. Rose ME. Are prescription opioids driving the opioid crisis? Assumptions vs Facts. Pain Med. 2018;19(4):793–807. doi:10.1093/pm/pnx048
54. DEA Diversion Control Division. Drug & chemical evaluation section: hydrocodone [Internet]. DEA; 2019. Available from: https://www.deadiversion.usdoj.gov/drug_chem_info/hydrocodone.pdf.
55. International Narcotics Control Board. Narcotic drugs: estimated world requirements for 2022. Statistics for 2020 [Internet]. INCB.org; 2022. Available from: https://www.incb.org/incb/en/narcotic-drugs/Technical_Reports/narcotic_drugs_reports.html.
56. Amsterdam JV, Van den Brink W. The misuse of prescription opioids: a threat for Europe? Curr Drug Abuse Rev. 2015;8(1):3–14. doi:10.2174/187447370801150611184218
57. Chenaf C, Kabore J-L, Delorme J, et al. Prescription opioid analgesic use in France: trends and impact on morbidity-mortality. Eur J Pain. 2019;23(1):124–134. doi:10.1002/ejp.1291
58. Hider-Mlynarz K, Cavalie P, Maison P. Trends in analgesic consumption in France over the last 10 years and comparison of patterns across Europe. Br J Clin Pharmacol. 2018;84(6):1324–1334. doi:10.1111/bcp.13564
59. Furlan AD, Chaparro LE, Irvin E, Mailis-Gagnon A. A comparison between enriched and nonenriched enrollment randomized withdrawal trials of opioids for chronic noncancer pain. Pain Res Manage. 2011;16:337–351. doi:10.1155/2011/465281
60. Katz N. Enriched enrollment randomized withdrawal trial designs of analgesics: focus on methodology. Clin J Pain. 2009;25(9):797–807. doi:10.1097/AJP.0b013e3181b12dec
61. Meske DS, Lawal OD, Elder H, et al. Efficacy of opioids versus placebo in chronic pain: a systematic review and meta-analysis of enriched enrollment randomized withdrawal trials. J Pain Res. 2018;11:923–934. doi:10.2147/JPR.S160255
62. Tayeb BO, Barreiro AE, Bradshaw YS, Chui KK, Carr DB. Durations of opioid, nonopioid drug, and behavioral clinical trials for chronic pain: adequate or inadequate? Pain Med. 2016;17(11):2036–2046. doi:10.1093/pm/pnw245
63. Buynak R, Rappaport SA, Rod K, et al. Long-term safety and efficacy of tapentadol extended release following up to 2 years of treatment in patients with moderate to severe, chronic pain: results from an open-label extension trial. Clin Ther. 2015;37(11):2420–2438. doi:10.1016/j.clinthera.2015.08.014
64. Wild JE, Grond S, Kuperwasser B, et al. Long-term safety and tolerability of tapentadol extended release for the management of chronic low back pain or osteoarthritis pain. Pain Pract. 2010;10(5):416–427. doi:10.1111/j.1533-2500.2010.00397.x
65. Hale M, Urdaneta V, Kirby MT, Xiang Q, Rauck R. Long-term safety and analgesic efficacy of buprenorphine buccal film in patients with moderate-to-severe chronic pain requiring around-the-clock opioids. J Pain Res. 2017;10:233–240. doi:10.2147/JPR.S120170
66. Roth SH, Fleischmann RM, Burch FX, et al. Around-the-clock, controlled-release oxycodone therapy for osteoarthritis-related pain. Arch Intern Med. 2000;160:853–860. doi:10.1001/archinte.160.6.853
67. Portenoy RK, Farrar JT, Backonja MM, et al. Long-term use of controlled-release oxycodone for noncancer pain: results of a 3-year registry study. Clin J Pain. 2007;23:287–299. doi:10.1097/AJP.0b013e31802b582f
68. Friedmann N, Klutzaritz V, Webster L. Long-term safety of Remoxy® (extended-release oxycodone) in patients with moderate to severe chronic osteoarthritis or low back pain. Pain Med. 2011;12(5):755–760. doi:10.1111/j.1526-4637.2011.01100.x
69. McIlwain H, Ahdieh H. Safety, tolerability, and effectiveness of oxymorphone extended release for moderate to severe osteoarthritis pain: a one-year study. Am J Ther. 2005;12(2):106–112. doi:10.1097/01.mjt.0000139442.65914.f9
70. Hale ME, Ma Y, Malamut R. Six-month, open-label study of hydrocodone extended release formulated with abuse-deterrence technology: safety, maintenance of analgesia, and abuse potential. J Opioid Manag. 2016;12(2):139–147. doi:10.5055/jom.2016.0326
71. Taber L, Lynch SY, He E, Ripa SR. Long-term safety and effectiveness of once-daily, single entity, extended-release hydrocodone over 76 weeks of an open-label study in patients with chronic noncancer and nonneuropathic pain. Postgrad Med. 2016;128(1):23–33. doi:10.1080/00325481.2016.1134022
72. Hale ME, Zimmerman TR, Ma Y, Malamut R. Twelve-month, open-label assessment of long-term safety and abuse potential of hydrocodone extended-release formulated with abuse-deterrence technology in patients with chronic pain. J Opioid Manag. 2015;11(5):425–434. doi:10.5055/jom.2015.0292
73. Wen W, Taber L, Lynch SY, He E, Ripa S. 12-month safety and effectiveness of once-daily hydrocodone tablets formulated with abuse-deterrent properties in patients with moderate to severe chronic pain. J Opioid Manag. 2015;11(4):339–356. doi:10.5055/jom.2015.0283
74. Nalamachu S, Rauck RL, Hale ME, Florete, Jr. OG, Robinson CY, Farr SJ. A long-term, open-label safety study of single-entity hydrocodone bitartrate extended release for the treatment of moderate to severe chronic pain. J Pain Res. 2014;7:669–678. doi:10.2147/JPR.S71536
75. Wallace M, Thipphawong J. Open-label study on the long-term efficacy, safety, and impact on quality of life of OROS hydromorphone ER in patients with chronic low back pain. Pain Med. 2010;11(10):1477–1488. doi:10.1111/j.1526-4637.2010.00956.x
76. Wallace M, Moulin DE, Rauck RL, et al. Long-term safety, tolerability, and efficacy of OROS hydromorphone in patients with chronic pain. J Opioid Manag. 2009;5(2):97–105. doi:10.5055/jom.2009.0011
77. Webster LR, Brewer R, Wang C, et al. Long-term safety and efficacy of morphine sulfate and naltrexone hydrochloride extended release capsules, a novel formulation containing morphine and sequestered naltrexone, in patients with chronic, moderate to severe pain. J Pain Symptom Manage. 2010;40(5):734–746. doi:10.1016/j.jpainsymman.2010.05.004
78. Milligan K, Lanteri-Minet M, Borchert K, et al. Evaluation of long-term efficacy and safety of transdermal fentanyl in the treatment of chronic noncancer pain. J Pain. 2001;2:197–204. doi:10.1054/jpai.2001.25352
79. Pascual ML, Fleming RR, Gana TJ, Vorsanger GJ. Open-label study of the safety and effectiveness of long-term therapy with extended-release tramadol in the management of chronic nonmaligant pain. Curr Med Res Opin. 2007;23(10):2531–2542. doi:10.1185/030079907X233179
80. Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain. The SPACE randomized clinical trial. JAMA. 2018;319:872–882. doi:10.1001/jama.2018.0899
81. Manchikanti L, Benyamin R, Hirsch JA. Comments on Space randomized clinical trial by Krebs et al. Pain Phy. 2019;22:E139–E146. doi:10.36076/ppj/2019.22.E139
82. Schneider JP, Fudin J, Gudin J. Commentary on the KREBS SPACE trial. Pract Pain Manage. 2018;1(4):e34
83. Gudin J, Kaufman AG, Datta S. Are opioids needed to treat chronic low back pain? A review of treatment options and analgesics in development. J Pain Res. 2020;13:1007–1022. doi:10.2147/JPR.S226483
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
