Back to Journals » Infection and Drug Resistance » Volume 14
Catheter-Associated Urinary Tract Infection: Incidence, Associated Factors and Drug Resistance Patterns of Bacterial Isolates in Southern Ethiopia
Authors Oumer Y, Regasa Dadi B , Seid M, Biresaw G , Manilal A
Received 15 March 2021
Accepted for publication 16 July 2021
Published 24 July 2021 Volume 2021:14 Pages 2883—2894
DOI https://doi.org/10.2147/IDR.S311229
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yisiak Oumer,1 Belayneh Regasa Dadi,1 Mohamed Seid,1 Gelila Biresaw,2 Aseer Manilal1
1Department of Medical Microbiology, Arba Minch University, Arba Minch, Ethiopia; 2Department of Hematology and Immunohematology, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Belayneh Regasa Dadi Email [email protected]
Introduction: Catheter-associated urinary tract infections (CAUTIs) are the most common nosocomial infection and a leading cause of morbidity. The aim of this study was to determine the prevalence, associated factors and antibiogram of the bacterial isolates among CAUTIs patients.
Methods: A facility-based, cross-sectional study was conducted from March to December 2019 at Arba Minch General Hospital, Southern Ethiopia. Clinical and socio-demographic data were obtained using a questionnaire. Clean catch midstream urine samples were collected and inoculated onto blood agar, MacConkey agar, and cysteine lactose electrolyte deficient agar (CLED). The inoculated culture media were incubated in an aerobic atmosphere at 37°C for 24 h. After overnight incubation, the bacterial growth on the respective media was inspected visually and graded for the presence of significant bacteriuria. A significant bacteriuria was considered, if pure culture at a concentration of ≥ 105 colony forming unit (CFU)/mL. All isolates were further identified using colony morphology and biochemical tests. Antimicrobial sensitivity was determined by modified Kirby–Bauer disc diffusion method. Data were analyzed using SPSS version 25. P-value less than 0.05 was used as statistical significance.
Results: The overall incidence of symptomatic CAUTIs was 39/231 (16.8%). Independent predictors of CAUTIs were prolonged (≥ 7 days) catheterization (AOR = 3.6, 95% CI = 1.0– 12.2), diabetes mellitus (AOR = 5.3, 95% CI = 1.4– 19.6) and insertion of catheter in surgical ward (AOR = 3.6, 95% CI = 1.08– 12.28). The most common bacterial isolates were E. coli 17/42 (40.5%), Klebsiella species 9/42 (21.4%) and Enterococcus species 5/42 (11.9%). High (> 80%) drug resistance was observed against cotrimoxazole, cefoxitin and tetracycline. Ciprofloxacin and nitrofurantoin were the most active drugs. The overall prevalence of MDR among isolates was 37/42 (88.1%). Most bacterial isolates 30/42 (71.4%) were biofilm producers.
Conclusion: High levels of drug resistance were observed to commonly used antibiotics. In our study, biofilm-producing bacterial isolates were the predominant cause of CAUTIs. Therefore, continuous surveillance of antimicrobial resistance patterns is necessary to help physicians in treatment and management of CAUTIs.
Keywords: catheter-associated urinary tract infections, uropathogens, antimicrobial susceptibility, risk factors
Introduction
Catheter-associated urinary tract infections (CAUTIs) continue to be among the most common health-care associated infections worldwide: CAUTIs account for 40% of all hospital-acquired infections and 80% of all nosocomial urinary tract infections (UTIs).1 If inadequately treated, CAUTIs may progress to complications such as cystitis, pyelonephritis, Gram-negative bacteremia, endocarditis, vertebral osteomyelitis, septic arthritis, and meningitis in all patients2 and these lead to discomfort for the patient, with an excess mortality rate of 23 deaths per 1000 inpatients and excess costs of $1000/case, i.e., additional costs per hospital acquired infection.3
It is estimated that 10–12% of hospitalized patients and 4% of patients in the community have urinary catheters in situ at any given time.4 Female sex, old age, duration of hospital stay, impaired immunity, opening a closed system, disease comorbidity and measures (i.e., diabetes mellitus, renal disease, and use of systemic antibiotics) and suboptimal aseptic techniques are risk factors of CAUTIs.5,6
Bacteria can enter the bladder during insertion of the catheter, through the catheter lumen, or from around the outside of the catheter. The most common infecting organisms are Escherichia coli, Klebsiella species, Proteus species, Enterococcus species, Pseudomonas species, Enterobacter species and Serratia species.7 Antimicrobial resistance among urinary pathogens has been an ever-increasing problem in the last few decades; there have been significant changes in the antibiogram of CAUTIs bacterial isolates and reports on spread of resistance among them.8 The combination of emerging multidrug resistant (MDR) bacteria along with the defense afforded by biofilm formation are set to make successful treatment with systemic antibiotics ever more difficult to achieve.9,10 CAUTIs are a major health concern; understanding the risk factors, incidence of bacterial isolates, biofilm formation and antimicrobial susceptibility patterns in catheterized patients is very important for proper treatment and management of CAUTIs since these data are lacking in the study area.
Methods
Study Design, Setting and Population
A facility-based cross-sectional study was conducted from March to December 2019 at Arba Minch General Hospital (AMGH), Southern Ethiopia. The study population was catheterized patients who stayed on a catheter for more than 48 h and with signs and symptoms of UTIs at AMGH during the study period. Inclusion criteria are catheterized patients who stayed on catheter for more than 48 h and with at least two of the following signs and symptoms of UTIs: fever, suprapubic tenderness, costovertebral angle pain or tenderness, urinary urgency, urinary frequency and dysuria.11 According to Centers for Disease Control and Prevention (CDC) criteria patients are said to have symptomatic CAUTI if there is significant bacteriuria (≥105 cfu/mL) with at least two signs and/or symptoms of acute UTI (from the following: fever, suprapubic tenderness, costovertebral angle pain or tenderness, urinary urgency, urinary frequency and dysuria) with an indwelling urethral catheter in place for more than 2 days. Patients were excluded if they (a) have recent history of UTI (within 6 months), (b) those who were on antimicrobial treatment of urinary tract infection or immunosuppressive drugs (within 2 weeks), (c) have a positive urine culture with significant bacterial count on the day of urinary catheter placement, (d) those who were catheterized outside the hospital, (e) those who were unconscious or had cognitive impairment, (f) those who were catheterized other than Foley catheter (g) isolation of polymicrobial growth in cultures, (h) refused to participate or were discharged or transferred to other hospitals with maintained catheter.
Data Collection and Laboratory Investigations
Socio-demographic data were collected with a pre-tested, well designed questionnaire through face to face interview. Patients’ medical data such as comorbidities, reasons for admission, admission ward, duration of hospitalization, duration of catheterization, reason for catheterization and place of catheter insertion were taken from patients’ medical records (supplemented by patient interviews). A clinical examination was performed on each participant with due emphasis on signs and symptoms compatible with UTI (which include at least two of the following signs and/or symptoms: fever, suprapubic pain or tenderness, costo-vertebral angle pain or tenderness, dysuria, urgent or frequent urination and suprapubic pain or tenderness). Catheterized patients who stayed on catheter for more than 48 hand with at least two of the following signs and/or symptoms of UTIs: fever, suprapubic tenderness, costovertebral angle pain or tenderness, urinary urgency, urinary frequency and dysuria were included in this study.
A freshly voided clean catch midstream urine sample (10–20 mL) was collected with a wide mouth sterile container with screw cap before catheter insertion. In patients with short-term (<7 days) catheterization, urine specimens were obtained by sampling through the catheter port using aseptic technique (disinfecting with 70% alcohol) or, if a port is not present, by puncturing the catheter tubing with a needle and syringe after clamping (catheter urine is taken in this case because risk of contamination is low). In patients with long-term (> 7 days) indwelling catheters, urine sample was collected after catheter was replaced from the freshly placed catheter. All collection was done immediately prior to initiating antimicrobial therapy. The urine samples were immediately transported to the Microbiology and Parasitology Laboratory of Arba Minch University for microbiological investigations.
Urine samples were inoculated simultaneously onto blood agar, MacConkey agar, and cysteine lactose electrolyte deficient agar (CLED) [Oxoid Ltd Co., Basingstoke, UK] using a sterile calibrated inoculating loop capable of transferring 0.001 mL. Inoculated culture media were incubated in aerobic atmosphere at 37°C for 24 h. After overnight incubation, the bacterial growth on the respective media was inspected visually and graded for the presence of significant bacteriuria. However, if growth was not detected, the culture plates were re-incubated for an additional 24 hbefore the culture was considered negative.
A significant bacteriuria was considered, if pure culture at a concentration of ≥105 colony forming unit (CFU)/mL and for cultures that contained two organisms we only sub-cultured the predominant organism because the organism of lower numbers is unlikely to be causing disease. If both were present at >10,000 CFU/mL, we sub-cultured both organisms. The persistence of the same organism on repeated urine cultures was considered as a pathogen even if the colony counts were low (i.e., <10,000 CFU/mL). All isolates were further identified using colony morphology and biochemical tests.12,13
Antimicrobial susceptibility testing was performed based on Kirby Bauer disc diffusion method using Clinical and Laboratory Standard Institute (CLSI) guidelines.14 A homogeneous suspension equivalent to that of 0.5 McFarland standards was prepared from an overnight pure culture of respective bacteria isolates and inoculated to Mueller Hinton agar plates. The inoculated plates were left at room temperature to dry for 3–5 min and a set of antibiotic discs were placed on the plates. The following antibiotic discs with their respective concentrations were used: penicillin (10 μg), ampicillin (10 μg), gentamicin (10 μg), ciprofloxacin (5 μg), tetracycline (30 μg), erythromycin (15 μg), vancomycin (30 μg), chloramphenicol (30 μg), norfloxacin (10 μg), nitrofurantoin (300 μg), cefoxitin (30 μg), and ceftriaxone (30 μg) for Gram-positive bacteria and ampicillin (10 μg), piperacillin (100 μg), cefoxitin (30 μg), cefepime (30 μg), ceftriaxone (5 μg), gentamicin (10 μg), ciprofloxacin (5 μg), tetracycline (30 μg), meropenem (10 μg), amikacin (30 μg), naldixic acid (30 μg), norfloxacin (10 μg), nitrofurantoin (300 μg) and ceftazidime (30 μg) for Gram-negative bacteria. The plates were then incubated at 37°C for 16–18 h. Results were interpreted as sensitive, intermediate and resistant according to the guidelines of the CLSI.14 Multidrug resistance (MDR) was determined when an organism was resistant to greater than three classes (categories) of antimicrobial agents.12,14,25
Each isolate’s in vitro biofilm-forming ability was quantified using the microtiter plate analysis. In brief, 20 µL of bacterial suspension was adjusted to a 0.5 McFarland turbidity and then 180 µL of TSB supplemented with 1% glucose were inoculated on each well in the microtiter plate to attain a final volume of 200 µL along with positive control organism and incubated at 37°C for 24 h. A sterile broth was used as a blank and negative control. After incubation, the plates were tapped and wells washed with 300 μL of phosphate buffer saline (pH 7.2) four times to remove free-floating bacteria. Biofilms that remained adhered to the walls and the bottom of the wells were fixed using methanol and stained with 0.1% crystal violet. Excess stain was washed with distilled water and the plates were left for air drying. Optical density (OD) was measured by using a microplate reader at a wavelength of 570 nm. The cut-off optical density (OD) was calculated and defined as three standard deviations above the mean OD of the negative control and accordingly the OD was found to be 0.214. Finally, the OD value of a tested strain was expressed as the average OD after subtracting the OD, 0.214 from the measured OD. Results were interpreted based on the OD value such as non-biofilm producer if OD ≤ 0.214, weak biofilm producer if the value was between 0.214 and 0.428, moderate if between 0.428 and 0.856, and strong if OD ≥ 0.856.15
Data Quality Assurance
Pre-test was conducted in Chencha Hospital (Arba Minch, Ethiopia) on 5% of study participants to assure that the data collection format was feasible in a closely related setting. Standard operational procedures were prepared and followed strictly. Cross-checking was done on a daily basis for data completeness. Control strains S. aureus ATCC 25923 and E. coli ATCC 25922 were used.
Statistical Analysis
Data were entered in to EpiData version 3.1 and exported and analyzed using SPSS software version 20 (IBM statistics, Armonk, NY). Categorical variables were analyzed by Chi-square test or Fisher’s exact test. Continuous variables were analyzed by independent t-tests or Mann–Whitney U-test. Parameters were compared using bivariate and multivariate logistic regression and chi-square tests. Variables with a p-value < 0.25 in bivariable analysis were included as candidate variables for multivariable model. The degree of association between dependent and independent variables was assessed using an adjusted odds ratio with a 95% confidence interval. All tests were 2-tailed, and a p-value of < 0.05 was taken as a cut-off point to determine the presence of a statistically significant association.
Results
Baseline Socio-demographic and Clinical Characteristics
A total of 231 hospitalized patients with urinary catheter for more than two days were enrolled in this study. Study participants were predominantly male (67.5%) in ratio of 2:1 with a mean age of 49.6 ± 15.5. Overall, study participants were catheterized for a total period of 1385 days. The mean duration of urethral catheter was 6.0 ± 2.6 days ranging between 2 and 30 days. Antibiotic prophylaxis was prescribed for 158 (68.4%) participants (Table 1).
 |
Table 1 Socio-demographic, Clinical Characteristics and Associated Factors Among Patients with Symptomatic CAUTIs |
Prevalence of CAUTIs and Associated Factors
Out of 231 patients catheterized, CAUTIs was identified in 39 patients giving an overall prevalence rate of 16.88%. The rate of incidence of symptomatic CAUTIs per 1000 catheter days was 28.15. CAUTIs was highest 25/42 (66.6%) in the age group of >60 years, in patients admitted in surgical ward 28 (71.8%), patients hospitalized for more than 10 days and patients having underlying diseases 25/42 (64.1%).
Multivariate analysis showed that factors such as insertion of catheter outside operation room, prolonged duration of catheterization (7 days) and diabetes mellitus were independent risk factors for CAUTIs. The odds of occurrence of symptomatic CAUTIs were found to be 3.18 times more in diabetes mellitus patients compared with their counterparts (p<0.001, adjusted OR = 3.18, 95 CI: 1.348–7.517). The incidence of CAUTIs was increased by more than 3-fold when the catheter was inserted out of the operation room (p<0.001, adjusted OR = 3.65, 95% CI: 1.08–12.28). Significantly higher rate of development of CAUTIs was observed among patients catheterized for seven days and above (adjusted OR = 5.36, 95 CI: 1.45–19.68) [Table 1].
Diversity of Bacteria Isolated from Patients with CAUTIs
A total of 42 bacterial isolates belonging to nine different genera were isolated from 39 patients Amongst the 42 isolates, Escherichia coli was found to be the most frequently isolated organism 17 (40.47%). Among the bacterial isolates 33/42 (78.57%) were Gram-negative bacilli and 9/42 (22.5%) were Gram-positive cocci (Figure 1).
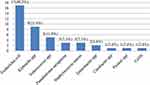 |
Figure 1 Bacterial profiles among CAUTI patients at Arba-Minch General Hospital, South Ethiopia (proportion of bacterial isolates). |
Antibiotic Susceptibility Profiles of Bacterial Isolates
The pattern of antibiotic sensitivity of the organisms causing CAUTIs was analyzed by comparing the various drug groups with different sensitivity percentages. Regardless of the isolated bacterial species, we found that among all the urinary isolates the range of resistance to ampicillin, cotrimoxazole and tetracycline were 40–100%, 75–90% and 66.7–86.6%, respectively. However nitrofurantoin was found to be effective in both Gram-positive and Gram-negative isolates with sensitivity of 40/42 (95.2%) followed by gentamicin and cefoxitin with sensitivity of 14/42 (33.4%). Resistance against the commonly prescribed fluoroquinolone group ranged from 29/42 (69%) for ciprofloxacin up to 30/42 (71.4%) for norfloxacin [Tables 2 and 3].
 |
Table 2 Antimicrobial Susceptibility Pattern of Gram-Negative Bacteria Isolated from Urine Culture of Symptomatic CAUTIs Patients |
 |
Table 3 Antimicrobial Susceptibility Pattern of Gram-Positive Bacterial Isolates from Urine Culture of Symptomatic CAUTIs Patients |
Multi-drug Resistance (MDR) Isolates of CAUTIs
Out of 42 isolates, 37 (88.1%) were found to have multi-drug resistance (MDR). All Klebsiella species showed MDR followed by 16/17 (94.1%) of E. coli [Table 4].
 |
Table 4 Percentage of the Most Common MDR Profiles Among Patients with Symptomatic CAUTIs |
Prevalence of Biofilm Formation
Out of the 42 bacteria isolated, 30 were found to be in vitro biofilm producers showing a prevalence of 71.4%. Strong biofilm formation was noted in 16/42 (53.3%) and a moderate level of biofilm formations in 10/42 (33.3%). Only a weak biofilm formation was observed in 4/42 (13.3%) cases and absolutely no such phenomenon was seen in 12/42 (28.5%). Biofilm formation was very prominent in Gram-positive bacteria 33/42 (77.8%) compared with Gram-negative isolates 29/42 (69.7%) [Table 5].
 |
Table 5 Biofilm Formation of Bacterial Isolates from CAUTIs Patients of Arba-Minch General Hospital, 2019 |
Discussion
In our study the overall prevalence of symptomatic CAUTIs was 16.9% (95% CI: 12.3–22.3). This finding is similar to studies conducted in China 15.8%,16 Uganda 15.3%17 and Sudan 16.37%.18 The prevalence of CAUTIs in our study is lower than studies done in India 42.9%2 and Nigeria 60.9%.19 However it is higher than studies conducted in USA 1.41%,6 Italy 6.2%20 and Australia 0.9%.21 The variation in prevalence of CAUTIs might be due to various reasons such as the gender of the patient, infection prevention policies which include aseptic task, catheter care, duration of catheterization and close drainage system. In addition overall variation in prevalence of CAUTIs could be attributed to difference in study protocols, sample size, methodological variation and duration of study.
Diabetic mellitus patients were more than 5 times more likely to develop CAUTIs than their counterparts and this was found to be statistically significant. Our result is in line with different studies conducted in Egypt,23 India2 and Korea.22 This may be due to impairment of host defenses, including decreased polymorphonuclear leukocyte mobilization, chemotaxis, and phagocytic activity related to hyperglycemia, and this increases the adherence of bacteria to the bladder epithelial cells.24 Moreover, the presence of glycosuria may favor growth of bacteria and promote their colonization and biofilm formation on catheter surface when urinary catheters are indwelling. Place where catheter is inserted showed a statistically significant association with CAUTIs. Patients who had catheter insertion at the surgical ward were 3.6 times more likely to develop CAUTIs than patients who had catheter insertion in the operation room. This finding is comparable with findings of a study conducted in Italy.20 This might be due to inappropriate technique of catheter insertion, poor hand hygiene and not following aseptic technique of catheter insertion. Therefore, the need to review the existing policy and guidelines on the insertion and care of urinary catheter in our health-care settings is indisputable.
The most frequently isolated UTI pathogens were E. coli (40.47%) followed by Klebsiella spp (21.43%) which was comparable with studies conducted in Uganda17 and Ethiopia.25 The predominance of these bacteria in the gut as normal flora may result in an infection of the urinary tract by contaminating the urethra and ascending into the bladder during catheter insertion. Studies conducted in Italy,20 Thailand26 and Sudan18 showed that P. aeruginosa or Enterococcus species were the most frequent bacterial isolates. This difference in distribution of bacterial isolates may be due to differences in environmental conditions, duration of catheterization and the organisms’ uniqueness to each facility.
The present study showed that Gram-negative bacteria isolates showed high level of resistance to the commonly prescribed drugs. Gram-negative bacteria isolates were resistant to ampicillin (100%), tetracycline (86.6%) and cotrimoxazole (83.3%) which is similar to studies conducted in Korea27 and Nigeria.7 However bacterial isolates showed high level of susceptibility to nitrofurantoin (96.7%), amikacin (84.8%) and meropenem (87.9%). The lower resistance to these drug could be their rare local availability and higher cost compared with others. In contrast to our findings decreased susceptibility was observed for nitrofurantoin in Uganda17 and Nigeria.7
In the present study 73.8% of bacterial isolates were in vitro positive for biofilm formation with 69.7% and 88.9% for Gram-negative and Gram-positive isolates, respectively. This finding is comparable with studies reported from India 71.23%,28 Pakistan 73.4%13 and Ethiopia 79.7%.25 However lower biofilm-forming bacteria than the present study were reported in Egypt with 43.3%29 and India 27%.30 The difference in biofilm-formation patterns among bacterial isolates may be due to differences in strain types, number of bacterial isolates, sample sizes, geographic locations, and methodological variations to assess biofilm formation.
Conclusion
The overall magnitude of catheter-associated urinary tract infection was 16.9%. Escherichia coli, Klebsiella spp. and Enterococcus spp. were the predominant etiologies of CAUTIs among catheterized patients. Nitrofurantoin, amikacin and meropenem are the drugs of choice for empirical therapy of CAUTIs. The majority of bacterial isolates had higher rates of resistance to commonly prescribed antimicrobials. Therefore, treatment and management of CAUTIs should be based on the knowledge of bacterial etiology and their antibiotic resistance patterns. Periodic monitoring of antimicrobial resistance patterns helps physicians to choose antimicrobial agents for empiric treatment of CAUTIs.
Limitation of the Study
It was not possible to include fungal pathogens due to budget constraints and the laboratory setup where the research was conducted. Additionally, for antimicrobial susceptibility testing of vancomycin it is recommended to use the minimum inhibitory concentration (MIC) method, but this was not included because of budget constraints.
Abbreviations
UTI, Urinary tract infection; BPH, Benign prostatic hyperplasia; CAUTIs, Catheter-Associated Urinary Tract Infections; AOR, Adjusted odd ratio; CFU, Colony forming unit; CLSI, Clinical and Laboratory Standards Institute; CLED, Cysteine Lactose Electrolyte Deficient Agar; CoNS, Coagulase negative Staphylococcus; CI, Confidence Interval; COR, Crude odd ratio; FDA, Food and Drug Administration; HAI, Hospital acquired infection; ICU, Intensive Care Unit; IUC, indwelling urinary catheter; MDR, Multi-drug Resistance; MHA, Mueller Hinton Agar; MRSA, Methicillin Resistant Staphylococcus aureus; spp., species; TSI, Triple Sugar Iron agar.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to ethical and confidentiality reasons but are available from the corresponding author on reasonable request under the Ethics Committee’s approval.
Ethics Approval and Consent to Participate
The proposal of this study was ethically approved by Institutional Review Board (IRB) of Arba Minch University College of Medicine and Health Sciences. Permission was obtained from Arba Minch General Hospital. The study participants’ age was ≥18. Before starting data collection, the purpose of the study was explained to all study participants and written informed consent was obtained. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors would like to thank those who were involved in this research.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Arba Minch University. The funding agencies had no involvement in the design of the study, data collection and analysis, interpretation of data and writing the manuscript.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Nicolle LE. Catheter associated urinary tract infections. Antimicrob Resist Infect Control. 2014;3(1):1–8. doi:10.1186/2047-2994-3-23
2. Leelakrishna P, Karthik R. A study of risk factors for catheter associated urinary tract infection. Int J Adv Med. 2018;5(2):334. doi:10.18203/2349-3933.ijam20180525
3. Apisarnthanarak A, Thongphubeth K, Sirinvaravong S, Kitkangvan D, Yuekyen C, Warachan B. Effectiveness of multifaceted hospitalwide quality improvement programs featuring an intervention to remove unnecessary urinary catheters at a tertiary care center in Thailand. Infect Control Hosp Epidemiol. 2007;28(7):791–798. doi:10.1086/518453
4. Garg S, Prakash S, Bhatia N, Daga M. Urinary catheterization in medical wards. J Glob Infect Dis. 2010;2(2):83. doi:10.4103/0974-777X.62870
5. Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625–663.
6. Letica-Kriegel AS, Salmasian H, Vawdrey DK, Youngerman BE, Green RA, Furuya EY. Identifying the risk factors for catheter-associated urinary tract infections: a large cross-sectional study of six hospitals. BMJ Open. 2019;9:1–7. doi:10.1136/bmjopen-2018-022137
7. Taiwo S, Aderounmu A. Catheter associated urinary tract infection: aetiologic agents and antimicrobial susceptibility pattern in Ladoke Akintola University Teaching Hospital, Osogbo, Nigeria. Afri J Biomed Res. 2009;9(3):141–148. doi:10.4314/ajbr.v9i3.48897
8. Gould CV, Umscheid C, Agarwal R, Kuntz G, Pegues D. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):119–126.
9. Haslund Mcquiston J, Rosborg Dinesen M, Sternhagen Nielsen AB, Llor C, Bjerrum L. Different recommendations for empiric first-choice antibiotic treatment of uncomplicated urinary tract infections in Europe. Scand J Prim Health Care. 2013;31(4):235–240. doi:10.3109/02813432.2013.844410
10. Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7(2):342–347. doi:10.3201/eid0702.010240
11. Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) patient safety component manual, CDC; 2019. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/6pscVAPcurrent.pdf.
12. Tesfahunegn Z, Asrat D, Woldeamanuel Y, Estifanos K. Bacteriology of surgical site and catheter related urinary tract infections among patients admitted in Mekelle Hospital, Mekelle, Tigray, Ethiopia. Ethiop Med J. 2009;47(2):117–127.
13. Sabir N, Ikram A, Zaman G, Satti L, Gardezi A, Ahmed A. Bacterial biofilm-based catheter-associated urinary tract infections: causative pathogens and antibiotic resistance. Am J Infect Control. 2017;45(10):1101–1105. doi:10.1016/j.ajic.2017.05.009
14. Wayne PA; CLSI. Performance Standards for Antimicrobial Susceptibility Testing.
15. Stepanović S, Vuković D, Hola V, Di Bonaventura G, Djukić S, Ćirković I. Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS. 2007;115(8):891–899. doi:10.1111/j.1600-0463.2007.apm_630.x
16. Xie DS, Lai RP, Nie SF. Surveys of catheter-associated urinary tract infection in a university hospital intensive care unit in China. Braz J Infect Dis. 2011;15(3):296–297.
17. Musinguzi B, Kabajulizi I, Mpeirwe M, Turugurwa J, Kabanda T. Incidence and etiology of catheter associated urinary tract infection among admitted patients at Kabale Regional Referral Hospital, South Western Uganda. Adv Infect Dis. 2019;09(03):183–196. doi:10.4236/aid.2019.93014
18. Ahmed M. Pattern of nosocomial urinary tract infections among sudanese patients. Br Microbiol Res J. 2012;2(2):53–61. doi:10.9734/BMRJ/2012/1255
19. Onipede A, Oyekale T, Olopade B, Olaniran O, Oyelese A, Ogunniyi T. Urinary pathogens and their antimicrobial susceptibility in patients with indwelling urinary catheter. Sierra Leone J Biomed Res. 2010;2(1):47–53. doi:10.4314/sljbr.v2i1.56607
20. Barbadoro P, Labricciosa FM, Recanatini C, Gori G, Tirabassi F, Martini E. Catheter-associated urinary tract infection: role of the setting of catheter insertion. Am J Infect Control. 2015;43(7):707–710. doi:10.1016/j.ajic.2015.02.011
21. Gardner A, Mitchell B, Beckingham W, Fasugba O. A point prevalence cross-sectional study of healthcare-associated urinary tract infections in six Australian hospitals. BMJ Open. 2014;4(7):1–9. doi:10.1136/bmjopen-2014-005099
22. Lee JH, Kim SW, Yoon BI, Ha US, Sohn DW, Cho YH. Factors that affect nosocomial catheter-associated urinary tract infection in intensive care units: 2-year experience at a single center. Korean J Urol. 2013;54(1):59–65. doi:10.4111/kju.2013.54.1.59
23. Aly S, Tawfeek R, Mohamed I. Bacterial catheter-associated urinary tract infection in the intensive care unit of Assiut University Hospital. Al-Azhar Assiut Med J. 2016;14(2):52. doi:10.4103/1687-1693.192652
24. Hakeem LM, Bhattacharyya DN, Lafong C, Janjua KS, Serhan JT, Campbell IW. Diversity and complexity of urinary tract infection in diabetes mellitus. Br J Diabetes Vasc Dis. 2009;9(3):119–125. doi:10.1177/1474651409105654
25. Awoke N, Kassa T, Teshager L. Magnitude of biofilm formation and antimicrobial resistance pattern of bacteria isolated from urinary catheterized inpatients of Jimma University Medical Center, Southwest Ethiopia. Int J Microbiol. 2019;2019:1–9. doi:10.1155/2019/5729568
26. Kotikula I, Chaiwarith R. Epidemiology of catheter-associated urinary tract infections at maharaj nakorn chiang mai hospital, northern thailand. Southeast Asian J Trop Med Public Health. 2018;49(1):113–122.
27. Park JJ, Seo YB, Kim SR, Park HJ, Eom JS, Yoo H. Incidence of catheter-associated urinary tract infection in hospitals with less than 300 beds. Korean J Healthc Assoc Infect Control Prev. 2019;24(1):11–18. doi:10.14192/kjhaicp.2019.24.1.11
28. Sayal P, Singh K, Devi P. Detection of bacterial biofilms in patients with indwelling urinary catheter. Center Info BioTechnol J Microbiol. 2014;3(3):9–16.
29. Mahmoud N, Abdallah A, Elsayed SB, Yassin MM. Biofilm forming bacteria isolated from urinary tract infection, relation to catheterization and susceptibility to antibiotics. Int J Biotechnol Mol Biol Res. 2011;2(10):172–178.
30. Tayal R, Baveja S, De A. Analysis of biofilm formation and antibiotic susceptibility pattern of uropathogens in patients admitted in a tertiary care hospital in India. Int J Health Allied Sci. 2015;4(4):247. doi:10.4103/2278-344X.167648
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
