Back to Journals » Infection and Drug Resistance » Volume 14
A Simulated Client Exploration of Nonprescription Dispensing of Antibiotics at Drugstores for Pediatric Acute Diarrhea and Upper Respiratory Infection in Lahore, Pakistan
Authors Malik UR , Chang J, Hashmi F , Atif N, Basir H, Hayat K , Khan FU , Kabba JA, Lambojon K , Fang Y
Received 15 January 2021
Accepted for publication 23 February 2021
Published 22 March 2021 Volume 2021:14 Pages 1129—1140
DOI https://doi.org/10.2147/IDR.S301812
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Usman Rashid Malik,1– 3 Jie Chang,1– 3 Furqan Hashmi,4 Naveel Atif,1– 3 Hareem Basir,5 Khezar Hayat,1– 3,6 Faiz Ullah Khan,1– 3 John Alimamy Kabba,1– 3 Krizzia Lambojon,1– 3 Yu Fang1– 3
1Department of Pharmacy Administration and Clinical Pharmacy, School of Pharmacy, Xi’an Jiaotong University, Xi’an, 710061, People’s Republic of China; 2Center for Drug Safety and Policy Research, Xi’an Jiaotong University, Xi’an, 710061, People’s Republic of China; 3Research Institute for Drug Safety and Monitoring, Institute of Pharmaceutical Science and Technology, China’s Western Technology Innovation Harbour, Xi’an, 710000, People’s Republic of China; 4University College of Pharmacy, University of the Punjab, Lahore, 54000, Pakistan; 5Royal Albert Edward Infirmary, Wigan, WN1 2NN, UK; 6Institute of Pharmaceutical Sciences, University of Veterinary and Animal Sciences, Lahore, 54000, Pakistan
Correspondence: Yu Fang
Department of Pharmacy Administration and Clinical Pharmacy, School of Pharmacy, Xi’an Jiaotong University, Xi’an, 710061, People’s Republic of China
Tel +86-29-8265-5132
Fax +86-29-8265-5424
Email [email protected]
Introduction: The excessive consumption of antibiotics is a significant contributor to antimicrobial resistance, especially in children. Children are often advised antibiotics for viral infections. In developing countries, drugstores are a prime source of easy access to nonprescription antibiotics. Moreover, in Pakistan, their irrational use is an “everyday routine”. The study, therefore, aimed to evaluate the dispensing of nonprescription antibiotics to children.
Methods: Using pediatric acute diarrhea and acute upper respiratory infection as disease scenarios, a simulated client, cross-sectional study was conducted in Lahore, Pakistan, to explore the antibiotics’ ease of availability at both categories of drugstores (pharmacies and medical stores) from November 1st, 2019 to January 31st, 2020. Chi-square (χ2) test was used to compare the differences in practices of different categorical variables. Multivariable logistic regression was applied to analyze the association of various factors with antibiotics dispensing.
Results: Antibiotics were dispensed without prescription in 456 (59%) of 773 simulated visits out of which 425 (93.2%) were dispensed on the advice of the drugstore staff. A qualified pharmacist was available in only 164 (21.2%) cases. Of the 386 visits for acute diarrhea and 387 for acute upper respiratory infection, nonprescription antibiotic dispensing occurred in 259 (67.1%) and 197 (50.9%) visits, respectively. There were considerable differences (p-value < 0.05) in the practices and antibiotics dispensing between each disease scenario presented. Moreover, antibiotics were less commonly dispensed at pharmacist-supervised drugstores compared to unsupervised ones.
Conclusion: Overall, inappropriate dispensing practices were prevalent to a large extent at the drugstores, and antibiotics were effortlessly obtainable without prescription. The quality of the services provided, especially by the non-pharmacist staff, was also not satisfactory. Therefore, the Drug Regulating Authority of Pakistan must enforce strict implementation of drug laws at the drugstores without delay, especially in major cities to help curb the felonious use of antibiotics.
Keywords: antibiotics, nonprescription, drugstores, community pharmacies, simulated client, Pakistan
Introduction
The decline in the discovery of new antibiotic molecules and a corresponding increase in antimicrobial resistance (AMR) levels is conceding the management of infectious diseases and is posing a significant threat to human life globally.1 AMR has become an issue of international priority in the last two decades, and the World Health Organization (WHO) in their meeting of Global Action Plan (2015) on AMR clearly stated that the prudent use of antibiotics has become a need of the hour to control AMR.2 The inappropriate use of antibiotics increases hospital stay, high costs, increased adverse effects, treatment failures, and the development of resistance to antibiotics.3,4 The excessive and irrational consumption of antibiotics is noticed more often in low- and middle-income countries than in the developed world.5
WHO’s Antibiotic Consumption Surveillance Report (2016–2018) stated that the use of antibiotics appears to be significantly high in certain parts of the world.6 Several factors, including economic growth and access to antibiotics, have driven this global growth in consumption.7 Drugstores represent one of the most vital antimicrobial sources worldwide.8 Various simulated client (SC) studies conducted worldwide to evaluate the nonprescription availability of antibiotics at drugstores had reported their widespread irrational use for nonbacterial infections.8–14 According to the WHO’s latest multi-country public awareness survey, 93% of people had their most recent antimicrobial taken from a pharmacy and drugstore.1 Such antibiotics are either recommended by a healthcare provider or obtained from several pharmacy outlets without a formal prescription. Antibiotics sale without a prescription is prohibited in many countries, yet community pharmacies/drugstores constitute a significant source of non-prescribed antibiotics.15 Often, in developing countries, there is either a complete absence of regulations for the selling of antibiotics or, otherwise, laws exist but there is a lack of enforcement of these regulations.16 Apart from the lack of governance in the health sector, the behavioral and socio-economic conditions of customers are important factors that cause the nonprescription use of antibiotics.17
Children, particularly infants, are vulnerable to bacterial infections. Across Asia, one child dies every 2 minutes because of diseases instigated by resistant bacteria.18 Antibiotics are the most widely prescribed drugs for children in hospitals and the community.19 Statistics from low-income and middle-income countries show that, due to the emergence of resistance to first-line antibiotics, 70% of hospital-acquired neonatal infections may not be treated effectively using the WHO-approved regimen.20 Also, children suffer from viral infections more often than adults.21 Antibiotics are often recommended to children who have viral or non-infectious illnesses. In some cases, children who suffer from infections for which narrow-spectrum drugs are suggested and recommended are frequently advised broad-spectrum antibiotics.22
In Pakistan, the mortality rate among children under 5 years is highest in South Asia (69/1000).23 Being a country of lower-middle-income status, antibiotics selling at drugstores without prescription is a problem of serious concern in Pakistan. The current legislation in Pakistan prohibits the sale of antibiotics without a valid prescription from a registered medical doctor.24 Still, evidence indicates that drugstores have a common practice of dispensing antibiotics irrationally for acute infections due to a lack of knowledge and/or commercial or business interests.25 Furthermore, a wide disparity exists in terms of education, knowledge, and quality of services provided at drugstores in Pakistan.26,27 Various studies conducted to evaluate self-medication with antibiotics have revealed high prevalence rates of antibiotics’ self-use, especially for gastrointestinal and respiratory problems.5,28 Health professionals, especially pharmacists and other pharmacy staff, have a prime duty to mitigate the misuse of antibiotics at the community level.29 In the last few years, no study has been conducted in Pakistan to evaluate dispensing practices for children at the drugstores of Pakistan. Therefore, the current study was designed to assess the nonprescription antibiotics dispensed in children at drugstores of the capital city of Punjab province of Pakistan, using the simulated client method.
Materials and Methods
Study Setting
Lahore, a metropolitan city and the capital of Punjab Province in Pakistan, was chosen as a target city for our study. The city spans over 1772 square kilometers, accommodates approximately 12.6 million people and has the most advanced setup of drugstores in the province. Lahore is geographically divided into 10 administrative towns and is comprised of urban and suburban populations. These towns are Aziz Bhatti Town, Data Ganj Baksh Town, Gulberg Town, Allama Iqbal Town, Lahore Cantonment Area, Nishtar Town, Samanabad Town, Shalimar Town, Ravi Town and Wahga Town.30
Study Design
A cross-sectional survey was conducted on drugstores of Lahore, Pakistan from November 1st, 2019 to January 31st, 2020 by using the simulated client method to evaluate general practices regarding the over-the-counter (OTC) sale of antibiotics. There are two categories of drugstores in Pakistan, namely, pharmacy and medical store. Pharmacies require the license of a pharmacist and medical stores require assistant pharmacist licensure. Both categories of drugstores can dispense an antibiotic with a legal prescription. Therefore, both categories located in all towns were included in the study. An updated list of registered pharmacies and medical stores of Lahore city was obtained from the Primary and Secondary Healthcare Department (P&SHD) of Punjab Province, and the final sample list was generated from that full list of registered pharmacies and medical stores in Lahore.
Sampling and Sample Size
There are 3947 registered drugstores in all 10 towns of Lahore city, excluding the distributors and wholesalers. A proportionate stratified random sampling procedure was used for the selection of drugstores based on the geographical towns. At first, a separate list of drugstores was generated for all 10 administrative towns. Then, from each list of individual towns, a sample list was generated through random selection by using the “rand()” function in Microsoft Excel. At a minimum, 8% of drugstores (including both pharmacies and medical stores) from each town were selected to make the best representative sample.
The sample size for the study was calculated by Raosoft Sample Size Calculator by assuming a 50% prevalence of nonprescription use of antibiotics, 5% margin of error, and 95% confidence interval (CI).31 The final sample size obtained was 351 drugstores, however, keeping in view the difficulties for simulated clients in searching the locations of drugstores and the possibility of shut-down of a few of the stores, a total of 400 drugstores were chosen out of 3947 outlets.
Simulated Scenarios
The pediatric acute diarrhea and acute upper respiratory tract infection (URTI) were chosen as fictional disease scenarios to visit the selected drugstores. Acute diarrhea and acute URTI are mostly non-bacterial infections. In children, acute diarrhea is typically caused by rotavirus and sometimes due to food poisoning or bacteria. The typical symptoms are loose stools (no blood in stool) with tiredness or weakness. Acute URTI in children also is of viral origin in most instances, and the typical symptoms may include a runny nose, nasal congestion, sneezing, and cough with or without fever. The management of these acute diseases in most of the cases should be symptomatic, and the use of antibiotics in such cases does not have an added advantage. In our study, we developed standard protocols for each disease scenario [Appendix A] and provided adequate training to the simulated clients who acted as a relative of a 3–5 -years-old child having a problem of acute diarrhea or acute URTI.
Data Collection Procedure
A predesigned data record form was adopted from a previous study conducted to evaluate antibiotics sales at community pharmacies.9 The form was modified according to local settings. Eight undergraduate pharmacy students having adequate medical background were engaged as simulated clients (SCs). They were adequately trained about the visit process and the disease scenarios under the supervision of a registered medical specialist and expert in the field of pharmacy practice. Each SC strictly followed the predesigned standardized procedure and presented the same scenario in all visits.
The clients first visited the drugstore, observed some basic parameters about the store and the staff, and then presented the disease scenario. After completion of the visit, they filled the data record form containing information about baseline characteristics, antibiotics dispensed, and patient counseling. Two levels of demand were presented by the SCs to get the medication for the assumed disease condition. At the first level of demand, the client told the pharmacy attendant about the symptoms of the disease and demanded a suitable medication. In case the staff did not dispense the antibiotics at the first level, the client then directly demanded from the staff to dispense any antibiotics in the second level of demand. The simulated clients did not buy any medicines and instead presented a suitable reason to avoid the purchase of medicines before leaving the drugstore. The clients presented an acute diarrhea scenario at 386 drug-stores and an acute URTI at 387 outlets. The outlets which were closed during the client visit and those which were untraceable were excluded from the study.
To ensure the quality of the survey and consistency of the data collected, the clients rehearsed the visit process and scenarios many times to make sure they do not mislay the recommended guidelines. Furthermore, they visited a few drugstores to achieve fluency in their presentation and to get acclimatized to the actual situations before starting the main study.
Statistical Analysis
The data were first entered and then analyzed using the IBM-SPSS version 22.0. The percentage of antibiotics dispensed without prescription was the primary outcome of the study. Descriptive statistics were applied to calculate frequencies and percentages. A Chi-square test was used to (i) compare the differences in dispensing practices between both disease scenarios, (ii) pharmacy practice with and without the supervision of qualified pharmacists and (iii) dispensing practices at both categories of drugstores. Multivariate logistic regression was also applied to evaluate the association of different factors with the nonprescription dispensing of antibiotics.
Ethical Approval
Ethical approval was obtained by the Biomedical Ethics Committee for Medical Research of Xi’an Jiaotong University (Approval number:2019–0161) and Ethics Committee of University College of Pharmacy, University of the Punjab, Lahore, Pakistan. The P&SHD, Government of Punjab was approached for formal approval and consent of the current study. The department formally approved and issued a list of drugstores to be included in the study. Since it was a simulated client study, therefore, did not require the informed consent of the respondents, however, it was approved by the ethics committees.
Results
Overall Dispensing Practices
Overall, 773 visits were made to the selected drugstores in all 10 administrative towns. From 773 visits, only in 28 (3.6%) cases, the attending staff was female. The antibiotics were dispensed in 456 (59%) cases, mostly (93.2%) were provided at the first demand level without mentioning the need for an antibiotic. A licensed pharmacist was present on duty in only 164 (21.2%) visits. In 643 (83.2%) visits, the staff did not even bother to request a prescription from the SCs and provided counseling about the dispensed drugs in only 307 (39.7%) cases (Table 1). The multivariable logistic regression data showed a significantly high proportion of nonprescription dispensing of antibiotics in seven administrative towns of the city (Table 2).
 |
Table 1 Characteristics and Practices of Visited Drugstores (Total Simulated Visits N=773) |
 |
Table 2 Factors Associated with Dispensing of Antibiotics without Prescription |
Of the 456 simulated visits in which an antibiotic was provided to the SCs for either childhood diarrhea or URTI, 261 (57.2%) inquired further about the disease/patient condition, and 148 (32.5%) asked whether the patient had previously taken any drug or treatment. However, only 20 (4.4%) questioned about the patient’s history of drug allergy. Counseling about antibiotics usage was provided in 231/456 (50.7%) cases. Interestingly, in 6/456 (1.3%) cases, the staff requested a prescription from the SCs and still dispensed the antibiotics. In 13/456 (2.9%) cases, the staff, after providing an antibiotic for the disease condition, recommended the customer to visit a physician for further advice (Figure 1).
 |
Figure 1 Staff response for simulated visits in which antibiotics were dispensed (n=456). |
The most frequently dispensed antibiotics for pediatric acute diarrhea were metronidazole 171 (54.6%), cefixime 88 (28.1%), and ciprofloxacin 48 (15.3%). Other less frequent antibiotics were amoxicillin, erythromycin, and clarithromycin. For acute URTI, cefixime was the commonly recommended and dispensed antibiotic, 102 (49.8%), followed by Co-Amoxiclav 32 (15.6%), ciprofloxacin 14 (6.8%), erythromycin 14 (6.8%), amoxicillin 13 (6.3%) and azithromycin 10 (4.9%). Some other antibiotics like clarithromycin, levofloxacin, cefuroxime, cefadroxil, and co-trimoxazole were also provided to SC in fewer cases (Figure 2).
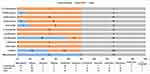 |
Figure 2 Antibiotics dispensed at drugstores for simulated disease scenarios (N=518, two antibiotics were dispensed at one time in 62 simulated visits). |
Dispensing Practices for Acute Diarrhea and Acute Upper Respiratory Infection
Out of 386 drugstores visited for acute diarrhea, antibiotics were dispensed in 259 (67.1%) cases out of which 236 (91.1%) were given to the customers without even asking for an antibiotic (Demand Level 1). Surprisingly, in 55/259 (21.2%) visits where the antibiotic was dispensed, two antibiotics were handed over to the SCs at a time. Only in 62/386 (16.1%) cases, the staff asked for a prescription from the clients when they requested an antibiotic, and in 71/386 (18.4%) visits, the staff recommended the client to visit a physician for better advice. For acute URTI, antibiotics were readily available to the clients without a prescription in 197 (50.9%) (Approximately half) visits, and 189/197 (95.9%) were dispensed at the first level of demand. In 7/197 (3.6%) situations, two antibiotics were given to the clients at a time. Prescriptions were not requested from the SCs in 319/387 (82.4%) visits (Table 3).
 |
Table 3 Differences in Practices of Drugstores for Each Disease Scenario Presented |
The results indicated significant differences (p-value <0.05) between the disease scenarios in terms of the proportion of antibiotics dispensed, the number of antibiotics dispensed at a single simulated visit, and in the counseling services provided to SCs with p-values <0.001, <0.001 and 0.003, respectively. The multivariate logistic regression also showed a significant association between the dispensing of nonprescription antibiotics and the disease scenarios presented with an odds ratio (OR) 0.468 (95% CI 0.344–0.636) and p <0.001, for acute URTI (Table 2).
Dispensing Practices of Pharmacist and Non-Pharmacist Supervised Drugstores
There was a significant difference in the majority of practices and services provided at the drugstores (better at drugstores supervised by pharmacists than unsupervised ones). A statistically significant difference was seen in the frequency of antibiotics dispensed (p= 0.001), inquiries about patients’ condition (p <0.001), request of a prescription from the SCs (p <0.001), referral to the physician (p <0.001) and counselling about medications (p =0.001). The availability of qualified pharmacists at drugstores was limited to only 164 (21.2%) visits. The drugstores with a pharmacist dispensed antibiotics in 78/164 (47.6%) cases, whereas those without a qualified pharmacist dispensed in 378/604 (62.1%) cases. Inquiries about patients’ disease status were asked in 84.1% of cases in pharmacist-supervised stores, which is relatively high compared to 52.2% in unsupervised stores. Additionally, counseling about dispensed medications was provided more often (51.2%) in comparison to non-pharmacist supervised stores (36.6%) (Table 4).
 |
Table 4 Differences in Practices Between the Drugstores Supervised by Pharmacist and without Pharmacist |
Dispensing Practices at Different Categories of Drugstores
A significant difference was observed in the staff characteristics and their behaviors at different categories of drugstores (pharmacies and medical stores). Antibiotics were significantly more conveniently available from the medical stores than pharmacies (p=0.002). The proportion of female staff was significantly higher (p <0.001) at pharmacies compared to medical stores where the female staff was only found to be working in 3 (0.7% cases). The differences were also seen in other practices, such as inquiry about patient condition, requesting a prescription from the customer, and referral to a physician (p <0.05) (Table 5).
 |
Table 5 Differences in Characteristics and Practices of Different Categories of Drugstores |
Discussion
This study discloses the misuse and irrational dispensing of antibiotics in children from Lahore city of Punjab Province, which was much higher for both acute diarrhea and acute URTI. Excessive antimicrobial dispensing at drugstores has also been reported in another province of Pakistan for acute diarrhea32 and was also prevalent many years ago in a few cities of Pakistan.33,34 In 2017, Pakistan reacted immediately to address the issue of increased emergence of AMR and formulated a National Action Plan (NAP) following the proposals presented by WHO to promote the rational and appropriate use of antibiotics and to enforce their availability with a legal prescription. Despite the existence of strict legislation and a quick response to WHO’s Global Action Plan on AMR, our study demonstrates that irrational dispensing practices have not yet been mitigated and retail stores are still an easy source of obtaining antibiotics unlawfully. Poor antimicrobial control at community levels, despite strict policies, was also observed in many studies conducted in Asian, African, and European countries.9–12,35–37
During our survey, it was found that there was an absence of qualified pharmacists in a significantly high number of drugstores. This implies that either the majority of the drugstores had not employed pharmacists or the licensed pharmacists were not on duty during the visits of simulated clients. Approximately 79% of pharmacies were not supervised by a pharmacist. Another simulated study conducted in a South Asian country reported the absence of pharmacists at the drugstores.13 On the contrary, in studies conducted in Saudi Arabia and a South European country (Belgium), there was an abundance of qualified pharmacists at drugstores.12,38 The presence of qualified pharmacists did not significantly affect the dispensing of antibiotics in a study conducted in northern Nigeria and a nationwide study conducted in China.39,40 On the contrary, in another study in China, it was found that the presence of a pharmacist was significantly associated with a lower likelihood of dispensing antibiotics without a prescription.9 Also, in Sri Lanka and Hungary, a reduction in the dispensing of antibiotics was observed because of the presence of a community pharmacist at the drugstores.13,41,42 In addition to an increased proportion of antibiotics dispensed due to the non-availability of pharmacists, our study also demonstrates that unsupervised drugstores resulted in a significantly poor quality of health services in terms of inquiries about patient condition, medical history, and counseling practices. Most of the staff did not even ask about the signs and symptoms of the children. It seemed that in any case, the choice of the antibiotic was already made after knowing the age of the child, irrespective of whether the presence of other symptoms.
Cefixime and ciprofloxacin were commonly dispensed for pediatric diarrhea and URTI. The frequent administration of a broad-spectrum antibiotic like cefixime alters the normal flora of the colon. Moreover, third-generation cephalosporins and fluoroquinolones are associated with community-acquired Clostridium difficle infections, which have lethal consequences for children in terms of increased mortality, high costs, and longer hospital stay.43 Thus, the usefulness of these antibiotics in pediatric acute infections has a big question mark because these antibiotic drugs may be hazardous for children’s health. Ciprofloxacin was also commonly dispensed in some simulation studies conducted in China, Sri Lanka, Lebanon, and India.9,13,14,44 The increased consumption of fluoroquinolones is also associated with the increased emergence of methicillin-resistant staphylococcus aureus (MRSA).45 Fluoroquinolone use in Pakistan has grown considerably over a few years, and the Drug Registration Board has issued an advisory regarding the use of fluoroquinolones because they tended to cause serious side effects like tendon rupture, irreversible nerve damage, and peripheral neuropathy.46
The considerably lower cost of medications and their convenient over-the-counter access make them tend to be an appealing choice for caretakers. It was noticed that several of the antibiotics provided for the children in this study were self-prescribed by the drugstore staff. In our study, more than 93% of antibiotics were dispensed at the desire and advice of the drugstore staff (Demand Level 1), either because of their limited knowledge or business interests. This indicates that the motive of the drugstores to promote their businesses and/or the inappropriate clinical norms prevalent in the society are driving factors for increased improper use of antibiotics at retail outlets besides customer expectations or therapeutic necessities. In some studies, antibiotics were dispensed at the recommendation of the drugstore staff.11,44,47 Conversely, in many simulated studies, antibiotics were mostly sold or dispensed by customer demand instead of on the advice and recommendation of the attending staff.9,48,49 Patient pressure and fear of losing the loyalty of customers are also the most driving reasons in high-income countries which compel the pharmacists to dispense antibiotics over-the-counter.42
Prescriptions were requested from the SCs in only 16.8% of cases which indicates that strict implementation of the drug rules is required at the drugstores. A massive decline in the dispensing of antibiotics was observed after a strict implementation of no antibiotic dispensing policy in Saudi Arabia.50 However, the Ministry of Health of Pakistan took several initiatives after the reporting of increased AMR levels in typhoid cases due to the extensive use of antibiotics.51 For example, a campaign was launched recently by the Primary and Secondary Healthcare Department of the Punjab Province and official notification has been issued to monitor the sale of prescription-based antibiotics at all drugstores in the Punjab Province. However, the active participation of policymakers in the campaign and strict implementation of the drug rules will determine the fate of the irrational use of antibiotics in Pakistan.
Some limitations might be associated with our study. First, there may have been some variations in the perceived characteristics of the drugstores and their staff by the simulated clients. An effort was made to minimize this disparity through comprehensive training and hands-on practical visits to some drugstores before starting the main study. Still, the dissimilarity cannot be overruled entirely. Second, the SCs only presented the disease scenarios for children. So, the findings might not directly generate dispensing practices for adults and elderly people. Finally, the study was carried out at drugstores located in urban and suburban population. Therefore, the practices in the rural population, which might be dissimilar, remained undisclosed.
Conclusions
The malpractice of dispensing nonprescription antibiotics is highly prevalent at the drugstores of Lahore, Pakistan. Most of the antibiotics were dispensed by non-qualified and less-trained staff and also not according to standard disease management guidelines. This reflects the incorrect practices as well as a lack of awareness among the staff regarding the accurate use of antibiotics. For that reason, it is the right time to restrict the open-market availability of prescription-only antibiotics by imposing high surveillance on the drugstores to avoid the hazardous effects of these medications. The strict implementation of prescription-only sales of antibiotics by the Drug Regulatory Authority of Pakistan in the major cities such as capital cities of each province can be a useful first step to mitigate the irrational use of antibiotics.
Acknowledgments
We express gratitude and appreciation to the pharmacy students of University College of Pharmacy, University of The Punjab, Lahore, Pakistan, who acted as simulated clients for the collection of data from the drugstores.
Funding
The research was funded by the “Young Talent Support Plan,” “High Achiever Plan” of Health Science Center, Xi’an Jiaotong University, Xi’an, China, and the Central University Basic Research Fund. (Grant number: 2015qngz05).
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization (WHO). Antibiotic Resistance: Multi-Country Public Awareness Survey. 2015. Available from: http://apps.who.int/iris/bitstream/10665/194460/1/9789241509817_eng.pdf?ua=1.
2. World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available from: https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/.
3. Marquet K, Liesenborgs A, Bergs J, Vleugels A, Claes N. Incidence and outcome of inappropriate in-hospital empiric antibiotics for severe infection: a systematic review and meta-analysis. Crit Care. 2015;19(1):1. doi:10.1186/s13054-015-0795-y
4. Goossens H, Ferech M, Vander Stichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–587. doi:10.1016/s0140-6736(05)17907-0
5. Shah JJ, Ahmad H, Rehan BB, et al. Self-medication with antibiotics among non-medical university students of Karachi: a cross-sectional study. BMC Pharmacol Toxicol. 2014;15(1):1–7. doi:10.1186/2050-6511-15-74
6. World Health Organization (WHO). WHO Report on Surveillance of Antibiotic Consumption. 2018.
7. Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14(8):742–750. doi:10.1016/S1473-3099(14)70780-7
8. Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11(9):692–701. doi:10.1016/S1473-3099(11)70054-8
9. Chang J, Xu S, Zhu S, et al. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: a mixed cross-sectional and longitudinal study. Lancet Infect Dis. 2019;3099(19):1–10. doi:10.1016/s1473-3099(19)30324-x
10. Horumpende PG, Sonda TB, van Zwetselaar M, et al. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: a simulated clients approach. PLoS One. 2018;13(11):1–14. doi:10.1371/journal.pone.0207465
11. Llor C, Cots JM. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis. 2009;48(10):1345–1349. doi:10.1086/598183
12. Driesen A, Vandenplas Y. How do pharmacists manage acute diarrhoea in an 8-month-old baby? A simulated client study. Int J Pharm Pract. 2009;17(4):215–220. doi:10.1211/ijpp.17.04.0004
13. Zawahir S, Lekamwasam S, Aslani P. Antibiotic dispensing practice in Sri Lankan community pharmacies: a simulated client study. Res Soc Adm Pharm. 2019;15(5):584–590. doi:10.1016/j.sapharm.2018.07.019
14. Yaacoub SG, Koyess V, Lahoud N, et al. Antibiotic prescribing for acute uncomplicated cystitis in Lebanese community pharmacies using a simulated patient. Pharm Pract (Granada). 2019;17(4):1–8. doi:10.18549/PharmPract.2019.4.1604
15. Cars O, Nordberg P. Antibiotic resistance-the faceless threat. Int J Risk Saf Med. 2005;17:103–110.
16. Hadi MA, Karami NA, Al-Muwalid AS, et al. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): a cross-sectional survey in Makkah Province, Saudi Arabia. Int J Infect Dis. 2016;47:95–100. doi:10.1016/j.ijid.2016.06.003
17. Collignon P, Athukorala P-C, Senanayake S, Khan F, Conly J. Antimicrobial resistance: the major contribution of poor governance and corruption to this growing problem. PLoS One. 2015;10(3):1–13. doi:10.1371/journal.pone.0116746
18. Cars O, Högberg L. Innovating for antibacterial resistance. ESCMID News. 2008;2(23):22–24.
19. Gerber JS, Newland JG, Coffin SE, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126(6):1067–1073. doi:10.1542/peds.2010-1275
20. Zaidi AKM, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365(9465):1175–1188. doi:10.1016/S0140-6736(05)71881-X
21. van Houten CB, Cohen A, Engelhard D, et al. Antibiotic misuse in respiratory tract infections in children and adults- a prospective, multicentre study (TAILORED treatment). Eur J Clin Microbiol Infect Dis. 2019;38(3):505–514. doi:10.1007/s10096-018-03454-2
22. Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–1061. doi:10.1542/peds.2011-1337
23. World Bank. The Under-5 Mortality Rate in Pakistan in 2018. Available from: https://data.worldbank.org/indicator/SH.DYN.MORT?contextual=region&end=2018&locations=PK&start=1960.
24. Ministry of National Health Services Regulations & Coordination G of P. Antimicrobial resistance: national action plan Pakistan. 2017. Available from: https://www.nih.org.pk/amr-national-action-plan-pakistan/.
25. Saleem Z, Hassali MA, Hashmi FK, Godman B, Saleem F. Antimicrobial dispensing practices and determinants of antimicrobial resistance: a qualitative study among community pharmacists in Pakistan. Fam Med Community Health. 2019;7:3. doi:10.1136/fmch-2019-000138
26. Hussain A, Ibrahim MIM. Qualification, knowledge and experience of dispensers working at community pharmacies in Pakistan. Pharm Pract. 2011;9(2):93–100. doi:10.4321/s1886-36552011000200006
27. Butt ZA, Gilani AH, Nanan D, Sheikh AL, White F. Quality of pharmacies in Pakistan: a cross-sectional survey. Int J Qual Health Care. 2005;17(4):307–313. doi:10.1093/intqhc/mzi049
28. Gillani AH, Ji W, Hussain W, Imran A. Antibiotic self-medication among non-medical university students in Punjab, Pakistan: a cross-sectional survey. Int J Environ Res Public Health. 2017;14(10):1152. doi:10.3390/ijerph14101152
29. Gastelurrutia MA, Larrañaga B, Garay Á, Echeveste FA, Fernandez-Llimos F. Impact of a program to reduce the dispensing of antibiotics without a prescription in Spain. Pharm Pract (Granada). 2013;11(4):185–190. doi:10.4321/S1886-36552013000400002
30. Administrative Towns of Lahore. Available from: https://lgcd.punjab.gov.pk/tma_lahore.
31. Raosoft Sample Size Calculator. Available from: http://www.raosoft.com/samplesize.html.
32. Khan A, Iqbal Q, Haider S, Khalid A, Hassali MA, Saleem F. Acute diarrheal management in adults: a simulated client study at community pharmacies of Quetta City, Pakistan. J Pharm Pract Community Med. 2019;5(1):13–17. doi:10.5530/jppcm.2019.1.3
33. Hussain A, Ibrahim MIM. Management of diarrhoea cases by community pharmacies in 3 cities of Pakistan. East Mediterr Health J. 2012;18(6):635–640. doi:10.26719/2012.18.6.635
34. Hussain A, Ibrahim MIM, Malik M. Assessment of disease management of acute respiratory tract infection at community pharmacies through simulated visits in Pakistan. Lat Am J Pharm. 2012;31(10):1435–1440.
35. Ekwochi U, Chinawa JM, Obi I, Obu HA, Agwu S. Use and/or misuse of antibiotics in management of diarrhea among children in Enugu, Southeast Nigeria. J Trop Pediatr. 2013;59(4):314–316. doi:10.1093/tropej/fmt016
36. Vogler S, Vitry A, Ud-Bin-Babar Z. Prices of oncology medicines in European countries, Australia and New Zealand. J Pharm Policy Pract. 2015;8(Suppl 1):P16. doi:10.1186/2052-3211-8-s1-p16
37. Torres NF, Solomon VP, Middleton LE. Identifying the commonly used antibiotics for self-medication in urban Mozambique: a qualitative study. BMJ Open. 2020;10(12):1–10. doi:10.1136/bmjopen-2020-041323
38. Al-Mohamadi A, Badr A, Bin Mahfouz L, Samargandi D, Al Ahdal A. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm J. 2013;21(1):13–18. doi:10.1016/j.jsps.2011.11.003
39. Abubakar U, Tangiisuran B. Knowledge and practices of community pharmacists towards non-prescription dispensing of antibiotics in Northern Nigeria. Int J Clin Pharm. 2020;42(2):756–764. doi:10.1007/s11096-020-01019-y
40. Chen J, Wang YM, Jie CX, Hesketh T. Ease of access to antibiotics without prescription in Chinese pharmacies: a nationwide cross-sectional study. Lancet. 2018;392:80. doi:10.1016/s0140-6736(18)32709-0
41. Zawahir S, Lekamwasam S, Aslani P. Community pharmacy staff’s response to symptoms of common infections: a pseudo-patient study. Antimicrob Resist Infect Control. 2019;8(1):1–10. doi:10.1186/s13756-019-0510-x
42. Gajdács M, Paulik E, Szabó A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: a cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics. 2020;9(2):2. doi:10.3390/antibiotics9020041
43. Adams DJ, Eberly MD, Rajnik M, Nylund CM. Risk factors for community-associated clostridium difficile infection in children. J Pediatr. 2017;186:105–109. doi:10.1016/j.jpeds.2017.03.032
44. Shet A, Sundaresan S, Forsberg BC. Pharmacy-based dispensing of antimicrobial agents without prescription in India: appropriateness and cost burden in the private sector. Antimicrob Resist Infect Control. 2015;4(1):1–7. doi:10.1186/s13756-015-0098-8
45. Parienti -J-J, Cattoir V, Thibon P, et al. Hospital-wide modification of fluoroquinolone policy and meticillin-resistant Staphylococcus aureus rates: a 10-year interrupted time-series analysis. J Hosp Infect. 2011;78(2):118–122. doi:10.1016/j.jhin.2011.03.008
46. Center for Disease Dynamics E and P (CDDEP). Situation Analysis Report on Antimicrobial Resistance in Pakistan – Findings and Recommendations for Antibiotics Use and Resistance. 2017. doi:10.1017/CBO9781107415324.004
47. Bin Abdulhak AA, Altannir MA, Almansor MA, et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: a cross sectional study. BMC Public Health. 2011;11(1):1–5. doi:10.1186/1471-2458-11-538
48. Chang J, Ye D, Lv B, et al. Sale of antibiotics without a prescription at community pharmacies in urban China: a multicentre cross-sectional survey. J Antimicrob Chemother. 2017;72(4):1235–1242. doi:10.1093/jac/dkw519
49. Shi L, Chang J, Liu X, et al. Dispensing antibiotics without a prescription for acute cough associated with common cold at community pharmacies in Shenyang, Northeastern China: a cross-sectional study. Antibiotics. 2020;9(4):1–16. doi:10.3390/antibiotics9040163
50. Alrasheedy AA, Alsalloum MA, Almuqbil FA, et al. The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev Anti Infect Ther. 2020;18(1):87–97. doi:10.1080/14787210.2020.1705156
51. Primary and Secondary Healthcare Department G of P. Monitoring of prescription based sale of Schedule B and Schedule D drugs. Available from: https://pshealthpunjab.gov.pk/.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
