Back to Journals » Infection and Drug Resistance » Volume 13
Risk Factors for Mortality of Inpatients with Pseudomonas aeruginosa Bacteremia in China: Impact of Resistance Profile in the Mortality
Authors Zhang Y, Li Y, Zeng J, Chang Y, Han S, Zhao J, Fan Y , Xiong Z , Zou X, Wang C, Li B, Li H, Han J, Liu X, Xia Y, Lu B , Cao B
Received 22 June 2020
Accepted for publication 2 September 2020
Published 12 November 2020 Volume 2020:13 Pages 4115—4123
DOI https://doi.org/10.2147/IDR.S268744
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sahil Khanna
Yulin Zhang,1 Yi Li,2 Ji Zeng,3 Yanzi Chang,4 Shouhua Han,5 Jiankang Zhao,1 Yanyan Fan,1 Zhujia Xiong,1 Xiaohui Zou,1 Chunlei Wang,1 Binbin Li,1 Haibo Li,1 Jiajing Han,1 Xinmeng Liu,1 Yudi Xia,1 Binghuai Lu,1 Bin Cao1,6,7
1Department of Pulmonary and Critical Care Medicine, Laboratory of Clinical Microbiology and Infectious Diseases, Center for Respiratory Diseases, National Clinical Research Center of Respiratory Diseases, China-Japan Friendship Hospital, Beijing 100029, People’s Republic of China; 2Department of Laboratory Medicine, Henan Provincial People’s Hospital, Zhengzhou, People’s Republic of China; 3Department of Laboratory Medicine, Wuhan Pu Ai Hospital of Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 4Department of Laboratory Medicine, Ningbo Medical Center Lihuili Hospital, Ningbo, People’s Republic of China; 5Department of Laboratory Medicine, Weifang No.2 People’s Hospital, Weifang, People’s Republic of China; 6Clinical Center for Pulmonary Infections, Capital Medical University, Beijing, People’s Republic of China; 7Tsinghua University-Peking University, Joint Center for Life Sciences, Beijing, People’s Republic of China
Correspondence: Binghuai Lu; Bin Cao
Department of Pulmonary and Critical Care Medicine, Laboratory of Clinical Microbiology and Infectious Diseases, Center for Respiratory Diseases, National Clinical Research Center of Respiratory Diseases, China-Japan Friendship Hospital, Chaoyang District, Beijing 100029, People’s Republic of China
Tel/Fax +86-10-84206257
Email [email protected]; [email protected]
Purpose: Pseudomonas aeruginosa bacteremia presents a severe challenge to hospitalized patients. However, to date, the risk factors for mortality among inpatients with P. aeruginosa bacteremia in China remain unclear.
Patients and Methods: This retrospective multicenter study was performed to analyze 215 patients with culture-confirmed P. aeruginosa bacteremia in five healthcare centers in China during the years 2012– 2019.
Results: Of 215 patients with P. aeruginosa bacteremia, 61 (28.4%) died during the study period. Logistic multivariable analysis revealed that cardiovascular disease (OR=3.978, P=0.001), blood transfusion (OR=5.855, P< 0.001) and carbapenem-resistant P. aeruginosa (CRPA) phenotype (OR=4.485, P=0.038) constituted the independent risk factors of mortality. Furthermore, both CRPA and multidrug-resistant P. aeruginosa (MDRPA) phenotypes were found to be significantly associated with 5-day mortality (Log-rank, P< 0.05).
Conclusion: This study revealed a high mortality rate amongst hospitalized patients with P. aeruginosa bacteremia, and those with cardiovascular diseases, CRPA and MDRPA phenotypes, should be highlighted and given appropriate management in China.
Keywords: risk factors, mortality, Pseudomonas aeruginosa, bacteremia
Introduction
Pseudomonas aeruginosa is a Gram-negative non-fermenting bacillus, leading to serious nosocomial infections, especially in immunocompromised individuals and those with neutropenia.1,2 The clinical outcomes in P. aeruginosa infected patients have been improved with the wide availability of antipseudomonal antibiotics in the past years. Unfortunately, the emergence of resistant P. aeruginosa strains due to the intrinsic and acquired resistance mechanism had increasingly drawn more attention.3–5 The organism has a tendency to cause multi-site infections, of which bacteremia is fatal, with a mortality rate ranging from 18% to 61%.6,7 Some studies have demonstrated that P. aeruginosa bacteremia could trigger severe septic shock and multiple organ failure, and result in high mortality rate and substantial medical costs.8
Poor outcomes of the bacteremia caused by P. aeruginosa could be explained by its virulence and the underlying diseases or conditions of the patients.9–11 The previous studies revealed that the prognosis could be closely associated with the severity of underlying diseases and delayed usages of effective antibiotics.6,12–16 In addition, the virulence genotype (exoU genotype) of P. aeruginosa was an independent marker related to early death in bacteremic patients.10 Besides, there are controversial data on the association between the clinical consequences and P. aeruginosa resistance profiles given that inappropriate antibiotics might result in treatment failure.9,16–21
Nowadays, the risk factors for mortality of inpatients with P. aeruginosa bacteremia in China remain unclear. Therefore, we conducted a retrospective multicenter cohort study, aiming to explore the risk factors of in-hospital death for patients and investigate the influence of the resistance profiles on P. aeruginosa bacteremia mortality.
Methods
Ethical Statement
This study was approved by the Ethics Committee of China-Japan Friendship Hospital with approval number 2019–122-K84, and the Declaration of Helsinki was followed throughout. The written informed consent from participants was waived because it focused only on the epidemical features of P. aeruginosa bacteremia, and the privacy of involved subjects was not affected.
Study Populations
We performed a retrospective analysis of 215 patients with P. aeruginosa bacteremia, who visited China-Japan Friendship Hospital (CJFH, 69 cases) during 2016–2019, Henan Provincial People’s Hospital (79 cases) during 2017–2019, Ningbo Medical Center Lihuili Hospital (30 cases) during 2012–2019, Wuhan Pu Ai Hospital of Huazhong University of Science and Technology (36 cases) during 2017–2019 and Weifang No.2 People’s Hospital (1 case) during the period of 2019. Patients with blood cultures positive for P. aeruginosa were retrieved in the microbiology laboratory databases from the five participating centers.
Clinical Data Collection
Data collected included demographic details, underlying conditions (diabetes mellitus, chronic lung disease, chronic renal failure, liver disease, solid organ cancer, cardiovascular disease, solid-organ transplantation, hematological disease and benign biliary tract disease), the source of infection (primary site of infection such as lung, soft-tissue, biliary tract, urinary tract, catheter-related, and peritoneum), nosocomial or community-acquired infection, comorbid condition (corticosteroid treatments received, immune deficiency, neutropenia, intravenous catheterization, blood transfusion, and coinfection with other bacteria), antibiotic use (monotherapy and combined antibiotic therapy), requirement for ventilatory support, ICU admission, hospital length of stay (LOS) and all-cause death.
Microbiological Studies
Microbiological data were obtained for following analysis from the CJFH because of the high mortality rate (60.9%) there and the geographically uneven data in other hospitals. The tested antimicrobial agents were as follows: aztreonam, gentamicin, tobramycin, ceftazidime, cefoperazone-sulbactam, cefepime, piperacillin, piperacillin-tazobactam, ticarcillin-clavulanate, imipenem, meropenem, amikacin, levofloxacin, ciprofloxacin and colistin. Antimicrobial susceptibility testing and analysis were performed according to the guidelines of Clinical and Laboratory Standards Institute.22
Definition
The presence of P. aeruginosa in blood culture and the clinical features related to the P. aeruginosa infection were defined as P. aeruginosa bacteremia. Only the first event was enrolled in the analysis if a patient presented ≥2 culture-confirmed P. aeruginosa bacteremia during the study period. The primary site of infection was defined as the most possible source of infection responsible for P. aeruginosa bacteremia on the basis of medical records, including lung infection, soft-tissue infection, biliary tract infection, urinary tract infection, catheter-related infection and peritoneum infection.23 It was defined as the bacteremia of unknown origin when the source of the infection was unclear.23 Nosocomial infection was defined as the P. aeruginosa bacteremia (1) that occurred more than 48 h after admission to hospital, or (2) that occurred less than 48 h after admission to hospital in cases who had been hospitalized in other hospitals within the 2 weeks prior to admission.16,17 Community-acquired infection was defined as the P. aeruginosa bacteremia that occurred less than 48 h after admission to hospital in patients who had never been in hospital or nursing home.16 An absolute neutrophil count of <500/mL was defined as neutropenia.10 The presence of immune deficiency was defined as the receipt of immunosuppressive therapy (immunosuppressive agent, chemotherapy or radiotherapy) during the P. aeruginosa bacteremia.10 Antibiotic monotherapy was defined as the treatment with only one of the following antibiotics: aztreonam, cefoperazone-sulbactam, ceftazidime, ticarcillin-clavulanate, piperacillin-tazobactam, cefepime, imipenem, meropenem, amikacin, levofloxacin, ciprofloxacin, colistin, and so on. Combination therapy consisted of the treatment with two or more above-mentioned antibiotics.24 CRPA is the definition that a strain is non-susceptible to one or both of imipenem and meropenem, and MDRPA consists of strains non-susceptible to at least one agent in three or more categories of antimicrobial agents.25,26
Statistical Analysis
Categorical variables are presented as frequencies and percentages. Continuous variables are described as mean and standard deviation (SD) or median and interquartile range (IQR). Comparisons of proportions were performed with chi-square and Fisher’s exact tests; continuous variables were compared using Student’s t-test. All probabilities were 2-tailed, with statistical significance defined as P≤0.05. A logistic regression model was used to analyze the risk factors for mortality of inpatients with P. aeruginosa bacteremia. All analyses were performed using PASW Statistics software, version 25.0.
Results
Clinical Characteristics and Outcomes of 215 Patients with P. aeruginosa Bacteremia
Demographic, clinical characteristics and outcomes of 215 patients with P. aeruginosa bacteremia are detailed in Table 1. Briefly, the mean age of the 215 patients was 60.5 years (SD 19.0 years), ranging from 10 months to 95 years, and 159 (74.0%) were male. Underlying diseases were present in 154 patients (71.6%), with cardiovascular disease (37.7%) being the most common underlying condition, followed by diabetes (25.1%), hematological disease (23.3%) and chronic lung disease (16.3%) (Table 1). The most common primary site of infection was lung (64, 29.8%), except for 70 cases (32.6%) for whom the primary site was unknown. Overall, 81.9% were from nosocomial acquisition. Furthermore, the comorbid conditions included neutropenia (18.6%), corticosteroid use (27.9%), immunosuppressive therapy (25.1%), intravenous catheterization (67.9%), blood transfusion (40.5%) and bloodstream coinfection with other bacteria (20.5%). During the hospitalization, a total of 209 patients (97.2%) received antimicrobial therapy regimen including antibiotic monotherapy in 91 (42.3%) and combined antibiotic therapy in 118 (54.9%); 69 patients (32.1%) received mechanical ventilation; 88 patients (40.9%) were admitted to ICU, and 61 patients (28.4%) died.
 |
Table 1 Demographic, Clinical Characteristics and Outcomes of 215 Patients with P. aeruginosa Bacteremiaa |
The comparison of demographic features, clinical characteristics and treatment of patients between survivors and non-survivors are shown in Table 1. The older mean age was observed in non-survivors (65.1 years) than survivors (58.7 years) (P=0.016). Moreover, chronic lung disease, cardiovascular disease, blood transfusion and bloodstream coinfection with other bacteria were also more common among non-survivors (all P<0.05, Table 1). Besides, both rates of ICU admission and invasive mechanical ventilation in non-survivors were higher than those in survivors (P<0.001, Table 1). Notably, 68.9% of non-survivors were from CJFH, followed by Wuhan Forth Hospital (18.0%) and three other centers. There were no significant differences between the two cohorts in rates and types of other underlying conditions, comorbid conditions, and length of hospital stay at admission (P>0.05, Table 1).
After adjusting for the influences of potentially confounding variables in a logistic regression model, factors including cardiovascular disease (OR=3.978, P=0.001), blood transfusion (OR=5.855, P<0.001) and hospitalization in CJFH (OR=9.031, P<0.001) were demonstrated to be independently associated with the mortality among all patients (Figure 1).
Clinical Characteristics and Outcomes of 69 Patients with P. aeruginosa Bacteremia in CJFH
As shown in Table 2, we further analyzed the clinical characteristics and outcomes of 69 patients (42 non-survivors and 27 survivors) with P. aeruginosa bacteremia in CJFH given that hospitalization in this hospital was demonstrated to be a risk factor of the mortality among the subjects. In univariable analysis, odds of death in hospitalized patients with cardiovascular disease and lung infection as the source of bacteremia was higher (P<0.05). Blood transfusion, ICU admission, invasive mechanical ventilation, combined antibiotic therapy, CRPA and MDRPA phenotypes were also proved to be associated with death (P<0.05, Table 2). Subsequently, the multivariate analysis was performed to determine which risk factors could be related to the mortality of inpatients in this center and the results are summarized in Figure 2. Cardiovascular disease (OR=5.329, P=0.010), blood transfusion (OR=7.938, P=0.011) and CRPA phenotype (OR=4.485, P=0.038) were found to be associated with increased odds of death in this hospital (Figure 2).
 |
Table 2 Demographic, Clinical Characteristics and Outcomes of 69 Patients with P. aeruginosa Bacteremiaa |
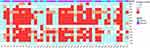
Impact of Resistance Profile in Mortality
The phenomenon was observed that the overall mortality was 60.9% (42/69) in CJFH and 40.6% (28/69) of patients died in the first 5 days of P. aeruginosa bacteremia. The resistance profile of P. aeruginosa strains from 42 non-survivors in this hospital is depicted in Figure 3 considering that CRPA phenotype was an independent risk factor for mortality. Obviously, the P. aeruginosa resistance in this cohort is serious in view of the fact that a total of 30 CRPA strains and 29 MDRPA strains were found in 42 non-survivors. Furthermore, the survival curve showed that both CRPA and MDRPA phenotypes were associated with 5-day death for P. aeruginosa bacteremia cases (Log rank, P<0.05, Figure 4A and B), with the 5-day mortality of 29.0% (20/69) and 31.9% (22/69) respectively (data not shown).
Discussion
P. aeruginosa bacteremia is a life-threatening infection in hospitalized patients with serious underlying conditions worldwide.9,27 However, to date, there are no studies in China that have comprehensively estimated the risk factors for death. This multicenter study revealed that the overall mortality of inpatients with P. aeruginosa bacteremia in China was 28.4%, similar to that reported in 9 countries (26.5%).27
As with the previous research,9,16,28,29 the present study had also demonstrated that the mortality was higher in patients with older ages, serious underlying host diseases (cardiovascular disease, chronic lung disease and diabetes mellitus), the primary site of lung infection and coinfection with other bacteria in univariate analysis. Even so, the results of the multivariate analysis indicated that cardiovascular disease, rather than others above, had 3.978 times the risk of death than those without. This result revealed a strong association between the poor clinical outcomes and underlying cardiovascular diseases of patients. Therefore, patients with serious underlying conditions, especially those with cardiovascular diseases, should be given timely treatment and care as appropriate.
It is noteworthy that the combination therapy has no beneficial influence on clinical outcomes in cohorts based on the fact that the higher mortality of 35.6% is observed in patients receiving combination therapy compared with that receiving monotherapy (19.8%, P<0.05). This is in keeping with the previous studies.27,30
The findings of this study suggested that the death risk of the patients receiving blood transfusion was 5.855 times higher than those without, as never reported in previous studies on P. aeruginosa bacteremia. In general, blood transfusion is performed strictly in mainland China to avoid transfusion-transmissible infections. The increased death risk of blood transfusion-related bacteremia might be the result of the immunosuppression caused by blood transfusion.31 Blood transfusion was thought to be related to the increased suppressor T cell activity and decreased natural killer cell activity in previous studies, therefore, adversely affected the patients’ survival.32,33 Anyway, unnecessary transfusions should be avoided to reduce the occurrence of bacteremia in hospital.34,35
Additionally, hospitalization in CJFH is noted to have a higher death risk than other centers in this study. Subsequently, our study further identifies the risk factors for inpatients mortality there. Apart from cardiovascular disease and blood transfusion, CRPA phenotype was identified as an independent risk factor of mortality in the population. In addition, a striking finding of the present study is that both CRPA and MDRPA phenotypes are significantly associated with 5-day mortality for P. aeruginosa bacteremia cases. Our results supported the findings from a previous investigation that patients with CRPA and MDRPA bacteremia were more likely to have a higher risk of 30-day mortality.29,36 These findings suggested that the high resistance levels of P. aeruginosa in invasive infections might be a therapeutic challenge for clinicians.37,38 Thus, an appropriate choice of effective antibiotics according to the antimicrobial sensitivity test in vitro is critical to improving poor outcomes for patients with P. aeruginosa bacteremia.29,36 Furthermore, the previous studies have reported the existence of the correlation between the virulence genotype and antimicrobial resistance including carbapenems.10,39 As a result, it is also essential to study the associations between virulence and CRPA or MDRPA phenotype to clarify the mechanism for disease severity in patients with drug-resistant phenotypes in future, which will provide the theory of basis for the development of novel antimicrobial agents.
In summary, this is a multicenter retrospective study to evaluate the risk factors for mortality in patients with P. aeruginosa bacteremia in China, in whom, cardiovascular disease, blood transfusion and CRPA phenotype were independent risk factors for the in-hospital mortality, and both phenotypes of CRPA and MDRPA were significantly associated with 5-day mortality. As such, P. aeruginosa bacteremia, especially in those with cardiovascular disease, CRPA and MDRPA phenotypes, should be increasingly appreciated and given appropriate management.
Abbreviations
ICU, intensive care unit; CRPA, carbapenem-resistant P. aeruginosa; CSPA, carbapenem-susceptible P. aeruginosa; MDRPA, multidrug-resistant P. aeruginosa; IQR, interquartile range; LOS, length of hospital stay; CJFH, China-Japan Friendship Hospital; OR, odds ratio.
Funding
This work was supported by the National Science Fund for Distinguished Young Scholars [grant number 81425001/H0104 to C.B]; CAMS Innovation Fund for Medical Sciences [CIFMS 2018-I2M-1-003 to C.B]; National Key Research and Development Program of China [grant number 2018YFC1200102 to L.B].
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Liu T, Zhang Y, Wan Q. Pseudomonas aeruginosa bacteremia among liver transplant recipients. Infect Drug Resist. 2018;11:2345–2356. doi:10.2147/IDR.S180283
2. Micek ST, Wunderink RG, Kollef MH, et al. An international multicenter retrospective study of Pseudomonas aeruginosa nosocomial pneumonia: impact of multidrug resistance. Crit Care. 2015;19:219. doi:10.1186/s13054-015-0926-5
3. Horcajada JP, Montero M, Oliver A, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev. 2019;32(4).
4. Oliver A, Mulet X, Lopez-Causape C, Juan C. The increasing threat of Pseudomonas aeruginosa high-risk clones. Drug Resist Updat. 2015;21–22:41–59.
5. Gajdacs M. Carbapenem-resistant but cephalosporin-susceptible Pseudomonas aeruginosa in urinary tract infections: opportunity for colistin sparing. Antibiotics (Basel). 2020;9(4).
6. Vidal F, Mensa J, Almela M, et al. Epidemiology and outcome of Pseudomonas aeruginosa bacteremia, with special emphasis on the influence of antibiotic treatment. Analysis of 189 episodes. Arch Intern Med. 1996;156(18):2121–2126. doi:10.1001/archinte.1996.00440170139015
7. Ammerlaan HS, Harbarth S, Buiting AG, et al. Secular trends in nosocomial bloodstream infections: antibiotic-resistant bacteria increase the total burden of infection. Clin Infect Dis. 2013;56(6):798–805. doi:10.1093/cid/cis1006
8. Cattaneo C, Antoniazzi F, Casari S, et al. P. aeruginosa bloodstream infections among hematological patients: an old or new question? Ann Hematol. 2012;91(8):1299–1304. doi:10.1007/s00277-012-1424-3
9. Pena C, Suarez C, Gozalo M, et al. Prospective multicenter study of the impact of carbapenem resistance on mortality in Pseudomonas aeruginosa bloodstream infections. Antimicrob Agents Chemother. 2012;56(3):1265–1272. doi:10.1128/AAC.05991-11
10. Pena C, Cabot G, Gomez-Zorrilla S, et al. Influence of virulence genotype and resistance profile in the mortality of Pseudomonas aeruginosa bloodstream infections. Clin Infect Dis. 2015;60(4):539–548. doi:10.1093/cid/ciu866
11. Cosgrove SE. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis. 2006;42(Suppl 2):S82–S89. doi:10.1086/499406
12. Lee CC, Lee CH, Hong MY. Risk factors and outcome of Pseudomonas aeruginosa bacteremia among adults visiting the ED. Am J Emerg Med. 2012;30(6):852–860. doi:10.1016/j.ajem.2011.05.029
13. Micek ST, Lloyd AE, Ritchie DJ, et al. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49(4):1306–1311. doi:10.1128/AAC.49.4.1306-1311.2005
14. Cheong HS, Kang CI, Wi YM, et al. Inappropriate initial antimicrobial therapy as a risk factor for mortality in patients with community-onset Pseudomonas aeruginosa bacteraemia. Eur J Clin Microbiol Infect Dis. 2008;27(12):1219–1225. doi:10.1007/s10096-008-0568-5
15. Kim YJ, Jun YH, Kim YR, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia; retrospective study of impact of combination antimicrobial therapy. BMC Infect Dis. 2014;14:161. doi:10.1186/1471-2334-14-161
16. Kang CI, Kim SH, Kim HB, et al. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003;37(6):745–751. doi:10.1086/377200
17. Lee CH, Su TY, Ye JJ, et al. Risk factors and clinical significance of bacteremia caused by Pseudomonas aeruginosa resistant only to carbapenems. J Microbiol Immunol Infect. 2017;50(5):677–683. doi:10.1016/j.jmii.2015.06.003
18. Dantas RC, Ferreira ML, Gontijo-Filho PP, Ribas RM. Pseudomonas aeruginosa bacteraemia: independent risk factors for mortality and impact of resistance on outcome. J Med Microbiol. 2014;63(Pt 12):1679–1687.
19. Suarez C, Pena C, Gavalda L, et al. Influence of carbapenem resistance on mortality and the dynamics of mortality in Pseudomonas aeruginosa bloodstream infection. Int J Infect Dis. 2010;14(Suppl 3):e73–e78. doi:10.1016/j.ijid.2009.11.019
20. Joo EJ, Kang CI, Ha YE, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia: clinical impact of antimicrobial resistance on outcome. Microb Drug Resist. 2011;17(2):305–312. doi:10.1089/mdr.2010.0170
21. Recio R, Mancheno M, Viedma E, et al. Predictors of mortality in bloodstream infections caused by Pseudomonas aeruginosa and impact of antimicrobial resistance and bacterial virulence. Antimicrob Agents Chemother. 2020;64(2).
22. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. PA: Clinical and Laboratory Standards Institute;2018.
23. Montero MM, Lopez MI, Knobel H, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bloodstream infections: what is the influence of XDR phenotype on outcomes? J Clin Med. 2020;9(2):514. doi:10.3390/jcm9020514
24. Pilmis B, Alby-Laurent F, Fasola ML, et al. Pseudomonas aeruginosa bloodstream infections in children: a 9-year retrospective study. Eur J Pediatr. 2020;179(8):1247–1254. doi:10.1007/s00431-020-03598-4
25. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281.
26. Gajdacs M, Batori Z, Abrok M, Lazar A, Burian K. Characterization of resistance in gram-negative urinary isolates using existing and novel indicators of clinical relevance: a 10-year data analysis. Life (Basel). 2020;10(2).
27. Babich T, Naucler P, Valik JK, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bacteraemia: a retrospective multicentre study. Int J Antimicrob Agents. 2020;55(2):105847. doi:10.1016/j.ijantimicag.2019.11.004
28. Hattemer A, Hauser A, Diaz M, et al. Bacterial and clinical characteristics of health care- and community-acquired bloodstream infections due to Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57(8):3969–3975.
29. Shi Q, Huang C, Xiao T, Wu Z, Xiao Y. A retrospective analysis of Pseudomonas aeruginosa bloodstream infections: prevalence, risk factors, and outcome in carbapenem-susceptible and -non-susceptible infections. Antimicrob Resist Infect Control. 2019;8:68. doi:10.1186/s13756-019-0520-8
30. Paul M, Leibovici L. Editorial commentary: combination therapy for Pseudomonas aeruginosa bacteremia: where do we stand? Clin Infect Dis. 2013;57(2):217–220.
31. Buddeberg F, Schimmer BB, Spahn DR. Transfusion-transmissible infections and transfusion-related immunomodulation. Best Pract Res Clin Anaesthesiol. 2008;22(3):503–517. doi:10.1016/j.bpa.2008.05.003
32. Ueta H, Kitazawa Y, Sawanobori Y, et al. Single blood transfusion induces the production of donor-specific alloantibodies and regulatory T cells mainly in the spleen. Int Immunol. 2018;30(2):53–67. doi:10.1093/intimm/dxx078
33. Zou Y, Song ZX, Lu Y, et al. Up-regulation of NKG2A inhibitory receptor on circulating NK cells contributes to transfusion-induced immunodepression in patients with beta-thalassemia major. J Huazhong Univ Sci Technol Med Sci. 2016;36(4):509–513. doi:10.1007/s11596-016-1616-5
34. Deng S, Feng S, Wang W, Zhu H, Gong Y. Bacterial distribution and risk factors of nosocomial blood stream infection in neurologic patients in the Intensive Care Unit. Surg Infect (Larchmt). 2019;20(1):25–30. doi:10.1089/sur.2018.085
35. Zhang L, Liao Q, Zhang T, Dai M, Zhao Y. Blood transfusion is an independent risk factor for postoperative serious infectious complications after pancreaticoduodenectomy. World J Surg. 2016;40(10):2507–2512. doi:10.1007/s00268-016-3553-7
36. Tam VH, Rogers CA, Chang KT, et al. Impact of multidrug-resistant Pseudomonas aeruginosa bacteremia on patient outcomes. Antimicrob Agents Chemother. 2010;54(9):3717–3722. doi:10.1128/AAC.00207-10
37. Gajdacs M, Burian K, Terhes G. Resistance levels and epidemiology of non-fermenting gram-negative bacteria in urinary tract infections of inpatients and outpatients (RENFUTI): a 10-year epidemiological snapshot. Antibiotics (Basel). 2019;8(3).
38. Gajdacs M, Urban E. Epidemiological trends and resistance associated with stenotrophomonas maltophilia bacteremia: a 10-year retrospective cohort study in a tertiary-care hospital in Hungary. Diseases. 2019;7(2).
39. Sawa T, Shimizu M, Moriyama K, Wiener-Kronish JP. Association between Pseudomonas aeruginosa type III secretion, antibiotic resistance, and clinical outcome: a review. Crit Care. 2014;18(6):668. doi:10.1186/s13054-014-0668-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.