Back to Journals » Infection and Drug Resistance » Volume 13
Drug Therapy Problems and Predictors Among Patients Admitted to Medical Wards of Dilla University Referral Hospital, South Ethiopia: A Case of Antimicrobials
Received 3 February 2020
Accepted for publication 26 May 2020
Published 12 June 2020 Volume 2020:13 Pages 1743—1750
DOI https://doi.org/10.2147/IDR.S247587
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Joachim Wink
Nigatu Addisu Bekele,1 Jarsso Tadesse Hirbu2
1Department of Pharmacy, College of Medical and Health Sciences, Dilla University, Dilla, Ethiopia; 2Department of Internal Medicine, College of Medical and Health Sciences, Dilla University, Dilla, Ethiopia
Correspondence: Nigatu Addisu Bekele Tel +251-934 08 8585
Email [email protected]
Purpose: To assess antimicrobial use-related problems and associated factors among patients admitted to medical wards of Dilla University Referral Hospital.
Patients and Methods: A hospital-based prospective observational study design was employed to assess the antimicrobial use-related problems among adult patients admitted to Dilla University Referral Hospital from 5 March to 4 September 2018. The antimicrobial therapy was reviewed to assure compliance with the recommendations of the national guidelines or evidence-based international clinical guidelines and drug therapy problem was identified. The logistic regression model was fit to determine the association between the different factors and the occurrence of drug therapy problems. Odds ratio was used to show a comparison of factors contributing to drug therapy problems. Statistical significance was considered at p-value < 0.05.
Results: In this follow-up to 229 participants, the prevalence of antimicrobial therapy-related problem was 70.74%. “Noncompliance to therapy” was the most frequent DTP experienced by 68 (29.69%) of the patients followed by “needs additional drug therapy” seen among 31 (13.54%) patients. “Adverse drug reaction” was the least and experienced by 7 (3.06%) patients. Others include: dosage too low among 22 (9.61%), dose too high among 17 (8.30%), unnecessarily prescribed antimicrobials among 17 (7.42%) and ineffective antimicrobials among 8 (3.49%) patients. Compared with those who used less than four drugs, the use of four to six (AOR: 4.024) and seven and above (AOR: 13.516) drugs were determinants for antimicrobial use problems. Additionally, infectious cases not addressed by the national guideline (AOR: 3.328) and the unavailability of appropriate lab values results within 48 hours of hospital admission (AOR: 1.285) were determinants for antimicrobial use problems.
Conclusion: Antimicrobial use problem was prevalent with 0.94-problems-per-patient. Polypharmacy, coverage of national guidelines and availing laboratory values within 48 hours of hospital admission were independent determinants of antimicrobial use problems.
Keywords: antimicrobials, drug therapy problems, Dilla University Referral Hospital
Introduction
Antimicrobials are the most commonly prescribed drugs in many developed and developing countries.1–3 At present, antimicrobial drugs constitute the largest single group of drugs procured by most developing countries.4 Inappropriate use of antibiotics was common especially in developing countries with poor health care systems.5 Nearly half of hospitalized patients receive antibiotics and up to 50% of antimicrobial use is unnecessary or inappropriate so, antibiotic-associated drug-related problems (DRPs) occur frequently and no significant improvement has been achieved on this issue in the last 3 decades. The irrational use of antimicrobials and emergence of antimicrobial-resistant pathogens cause large health care costs annually.6–8
A decrease in the development of new antibiotics and an alarming increase of antibiotic resistance has resulted in significant public health challenges to health care workers, health policymakers and the population around the world in general.1,9
World Health Organization’s global surveillance report of 2014 on antimicrobial resistance revealed that antibiotic resistance is no longer a prediction for the future; it is a problem by now, globally, and decreasing the capacity to treat common infections in the community and hospitals. Unless there will be urgent, coordinated action, the world is heading towards a post-antibiotic era, in which common infectious diseases cannot be treated and start killing though it has been treatable for decades.10
Though antimicrobial resistance occurs naturally over time, usually through genetic changes, misuse and overuse of antimicrobials are accelerating this process. Additionally, novel resistance mechanisms are being detected and spread globally, threatening our ability to treat known infectious cases, resulting in prolonged morbidity and high mortality rate.11
Irrational use of antimicrobials accelerates the emergence of resistant microorganisms. Misuse can be as a result of irrational prescribing practice, including prescribing unwanted antimicrobial medicines, incorrect selection of medicine, or at wrong dosage; self-treatment in countries in which antimicrobial medicines are freely available; not completing a course of antimicrobial medicines or taking them for too long; lack of regulations or standards for health care workers; and misuse and overuse in animal husbandry and agriculture. Overuse of antimicrobial medicines by the public and by the medical profession was a potential problem in all regions.12
In developing countries, patients frequently waste limited household resources on unnecessary antimicrobial therapy.13 In these countries, antimicrobials are prescribed for 44–97% of hospitalized patients often unnecessarily or inappropriately.14
Particularly, the appropriate antimicrobial utilization in the case of hospitalized patients is crucial not only in ensuring an optimal outcome, but in curtailing the emergence of resistance and containing costs.15 When infections become resistant to the first-line regimen, more costly therapies must be initiated. A longer duration of management increases health care costs as well as the economic burden on families and societies.10
Antimicrobials use in hospitals may be influenced by a different patient or facility-related factors.16
Ethiopia as a country has no national policy launched on antimicrobial use; neither do the hospitals, including DURH have their own antimicrobial use guidelines or controlling systems to assure effective treatment and limit the use of broad-spectrum antimicrobials, thereby reducing the selection of resistant micro-organisms. Additionally, the absence of infectious disease specialists and clinical pharmacists paved a way for use of available antimicrobials as per the unrestricted judgment of each practitioner. The consequences of inadequate antimicrobial therapy are also high. Moreover, the published studies have studied the antimicrobial use evaluation and patterns of antimicrobial use, which, however, do not identify the different patterns of inappropriate antimicrobial uses and their contributing factors. The investigators, therefore, conducted this study to assess the magnitude and patterns of antimicrobial use problems and to identify the associated factors.
Patients and Methods
Study Area and Period
Dilla University Referral Hospital is one of the referral hospitals in South Ethiopia serving the catchment population of nearly 2 million with a bed capacity of 151. It is the only referral hospital after Hawassa to the border of Ethio-Kenya. The internal medicine department of the hospital consists of over 38 beds for inpatients and is run by 5 senior internists. The hospital has no institution specific treatment guidelines and antimicrobial use guidelines.
Study Design and Data Analysis
Prospective observational study design was employed. Patients hospitalized to DURH medical wards from 5 March to 4 September 2018 those fulfilled the inclusion criteria. The inclusion criteria were: patients older than 18 years who were on any form of antimicrobials for the treatment of infectious disease at least for than 24 hours and those who had an indication for any form of antimicrobials. Patients with prophylactic antimicrobials and those with topical antimicrobials were excluded from the study.
The antimicrobial therapy was reviewed to assure compliance with the recommendations of the national guidelines or/and evidence-based international clinical guidelines. The charts of all hospitalized patients who either received an antimicrobial agent or in need of antimicrobial agent were reviewed and recorded by data collecting pharmacists in a patient-specific protocol with data collection format on a daily basis. Laboratory investigation, ordered by physicians to confirm the presence and/or type of infection was recorded and checked against the diagnosis. Adherence-related issues were addressed with observation and interviews. CPGs of the IDSA was used for disease cases not addressed by Ethiopian national guidelines.
The problem associated with antimicrobial therapy was then classified as “drug therapy problem”which was defined as any undesirable event experienced by a patient that involves, or is suspected to involve, drug therapy, and that interferes with achieving the desired goals of therapy and requires professional judgment to resolve.17 These problems were categorized into one of seven types of drug therapy problems.
- Unnecessary Drug Therapy: The drug therapy is unnecessary because the patient does not have a clinical indication at this time.
- Needs Additional Drug Therapy: Additional drug therapy is required to treat or prevent a medical condition or illness from developing.
- Ineffective Drug: The drug product is not being effective at producing the desired response or outcome.
- Dose Too Low: The dosage is too low to produce the desired response or outcome.
- Adverse Drug Reaction: The drug is causing an adverse reaction.
- Dose Too High: The dosage is too high, resulting in undesirable toxic effects.
- Noncompliance: The patient is not able or willing to take the drug therapy as intended.
The Statistical Package for Social Science (SPSS) programs version 20.0 for Windows was used to enter and analyze the data. Descriptive statistics were used to analyze the different types of DTPs identified. The logistic regression model was fit to determine the association between the different factors and the occurrence of the different types of DTPs. Odd ratios were used to show a comparison of factors contributing to drug therapy problems. Statistical significance was considered at p-value <0.05.
Ethical Consideration
Ethical approval was obtained from the Institutional Review Board (IRB) of Medical and Health Sciences, Dilla University. After explaining the purpose and procedures of the study, written informed consent was obtained from all participants and the study was conducted in accordance with the Declaration of Helsinki. All drug therapy problems identified during the data collection were handled carefully by investigators and discussed accordingly to solve the problem and protect the patient from harm or injury.
Results
During the study period, 229 patients were followed up. Over half, 118 (51.53%) of the study participants were male. 54 (23.58%) of study participants belonged to the age group 45–54 and 10% were elderly patients. Over two-third of the patients (68.12%) were married and 138 (60.26%) had a monthly average of less than 1500ETB. Only 34 (14.85%) of all study participants had a college education and 33 (14.41%) of them had no formal education at all (Table 1).
 |
Table 1 The Sociodemographic Characteristics of Patients Admitted to DURH |
National treatment guidelines of the country addresses 198 (86.46%) of the diagnosed infectious diseases. The remaining 31 (13.54%) cases were managed based on the clinical expertise of the treating physicians.
Of all total 229 patients with infectious diseases, the laboratory values of 181 (79.04%) patients were available within 48 hours of hospital admission to support the diagnosis of infectious diseases (Table 2).
 |
Table 2 The Health Facility Factors Related to Antimicrobial Use, Among Patients Admitted to DURH |
Right after admission, the medication history of only 61 (26.64%) patients were taken and the remaining were not asked about their previous medication use at all. Of these 61 patients, 39 had used drugs within the previous three months. 14 (35.90%) of these 39 patients with drug history used antimicrobials within the previous three months and the remaining 25 (64.10%), either did not use antimicrobials or could not identify the types of drugs they used whether it is antimicrobial or not.
176 (76.86%) of the patients had at least one comorbid condition and 30 (13.10%) of them were with three and above different comorbid cases at admission.
During follow-up, one fourth (25.76%) of the patients used less or equal to 3 drugs while nearly half (51.97%) used four to six drugs.
More than half (58.08%) of the patients stayed in the hospital for 8 −14 days. Six (2.62%) patients stayed for more than three weeks (Table 3).
 |
Table 3 Patient Characteristics Related to Antimicrobials Use in DURH |
All seven drug therapy problems were seen in this study. “Noncompliance” was the most frequent DTP which was experienced by 68 (29.69%) of the patients followed by “needs additional drug therapy” seen among 31 (13.54%) patients. “Actual/potential adverse drug reaction” was the least and experienced by 7 (3.06%) patients. Others were also remarkable in frequency and include Dosage too low among 22 (9.61%), dose too high among 17 (8.30%), unnecessary antimicrobials among 17 (7.42%) and ineffective antimicrobials among 8 (3.49%) patients (Table 4).
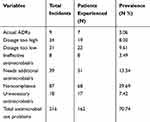 |
Table 4 Types of Antimicrobial Use Problems Identified in DURH |
The Incidence of Antimicrobial Use Problems
A total of 338 antimicrobial containing orders were prescribed for the 229 patients during the follow-up. Among these, antimicrobial-related drug therapy problems had occurred among 162 (70.74%) of the patients. No antimicrobial-related drug therapy problem was observed for the remaining 67 (29.26%) patients.
As far as the incidence density of antimicrobial use problems was considered, the problem-per-patient was calculated to be 0.94 and problem-per-order was 0.64 (Table 5). The incidence of problems per person-days was 0.083 implying the risk of occurrence of an antimicrobial-related drug therapy problem for each patient being about 8.30% every day. This incidence is calculated during a total of 2593 person-days-of follow-up. No same patient was readmitted with the same or different infectious disease during our follow-up study. Therefore problems per person and problem per admission can be used interchangeably.
 |
Table 5 The Incidence of Antimicrobial Use Problems in DURH |
Predictors of Drug Therapy Problems
Among different patient-related factors, sociodemographic characteristics of the patient have no significant association with the development of DTP.
During data analysis, variables with a p-value of <0.25 in binary logistic regression were taken to multivariate analysis to fit for the appropriate model.
During binary analysis, the presence of comorbid cases and the total number of drugs prescribed for a patient has an association with the development of DTP. Not taking medication history at patient admission time seems to increase the risk, but it was not statistically significant.
With multivariate analysis, total drugs prescribed, for a patient during the hospital stay, unavailability of laboratory results within 48 hours of hospital admission and disease conditions that are not addressed by the existing national guidelines remained statistically significant and affecting the development of drug therapy problems.
When compared with patients with fewer number prescribed drugs, patients with polypharmacy seem to be at increased risk for DTP. As clearly seen Table 6 below, patients with 4–6 drugs were about four times at increased risk of having antimicrobial-related drug therapy problem as compared to those with less than four different drugs (AOR=2.020–8.017at 95% CI with p-value=0.000). Similarly, compared to the same patients taking less than four drugs, patients with seven and above number of drugs were nearly 13 times at risk of having drug therapy problems (AOR=4.678–39.051 at 95% CI with p-value=0.000)
 |
Table 6 Multivariate Logistic Regression Analysis for the Predictors of Antimicrobial Use Problems Among Patients Admitted to Medical Wards of DURH |
The availability of appropriate lab values results within 48 hours of hospital admission has a strong association with the development of drug therapy problems in this study. Accordingly, compared with patients whose laboratory value is availed within 48 hours of admission, patients with no lab value within 48 hours were 3.383 times more likely to have DTP (AOR=1.285–8.907 at 95% CI with p-value=0.014)
Not all cases were addressed by the national guidelines in this study and national guideline coverage has a strong association with the development of DTP. So accordingly, a case which was not addressed by national treatment guideline was about 3.328 times more likely to result in drug therapy problems as compared with those cases that were addressed by national treatment guidelines (AOR= 1.015–10.909 at 95% CI with p-value =0.047). Number of days a patient stayed in a hospital seems to increase the risk of having DTP though statistically insignificant.
Discussion
A six-month prospective interventional study was conducted among 229 admitted patients at the medical ward of DURH.
167 (70.74) of patients in the follow-up developed at least one antimicrobial-related drug therapy problem during their hospital stay. This finding is much higher than the finding in hospitals in Chicago (49%),18 Turkish pediatric hospital (46.7%),19 and Switzerland (37%).20 The finding was comparable with the finding of the study conducted in the surgery ward of Jimma university medical center (69.3%).21 However, it was observed to be lower than the prevalence in the medical ward of JimmaUniversity Specialized Hospital (75.7%),22 Kyrgyzstan (73.3%)23 and Egyptian university hospital (88.7%).24
Among the seven types of different drug therapy problems, the most frequent type identified was Noncompliance experienced by 68 (29.69%) patients. It was much lower than the study in Portugal (57.71%).25 However, it was higher than the finding in JUSH (17%).22 This difference might be a result of the study setting as the study done in Portugal was in a community setting. The difference from studies done in JUSH and JUMC might be a result of the difference in the availability of drugs, difference in specialties and study duration as it was conducted for a long time in our case.
Needs additional drug therapy was the second most frequent drug therapy problem encountered in 31 (13.54%) of the patients. It was less than the finding in JUSH (29.6%)22 and USA (37.9%).26 This low prevalence might be due to the illegibility criteria set for the participants in a study conducted in the USA, all types of diseases were included whereas our study focused on diseases of infectious origin only. Again, the study conducted in JUSH was less addressed by national guidelines (80.3%) compared to our study (86.46%) which might have affected the rational antimicrobial selection among these studies. Additionally, our study excluded antimicrobial use for prophylaxis which was included in the study conducted in JUSH.
The prevalence of “Too low dose” was much lower than the finding in the USA (28%)26 and different studies conducted in surgery ward (32.9%)21 and medical ward (28.9%)22 of JUSH. Such differences might be contributed as a result of a relatively well addressed disease cases by the national guideline and introduction of pharmaceutical care as a measure to improve patient outcome and combat antimicrobial resistance strategies, a global burden a medical world facing.
Administration/order/of “Ineffective antimicrobial” was 3.49% in this study which was less than the finding in JUSH (9.2%),22 Kyrgyzstan (32.9%)23 and Switzerland (7.6%).20 The investigators associated this low prevalence as the majority of the antimicrobial used in this setup were broad-spectrum with increased antimicrobial coverage. The use of these broad-spectrum antimicrobials became common due to a lack of well-established diagnostic set up and unavailability of culture-based diagnosis. This overuse of broad-spectrum antimicrobials might contribute a lot to the development of antimicrobial resistance and it needs urgent and coordinated intervention. In addition to the mentioned justifications, ineffectiveness was not scientifically proven post antimicrobial therapy and it was judged merely based on disease and drug categories.
Unnecessary antimicrobial was prescribed/administered in 7.42% of patients. It was much lower than the prevalence in JUSH (28.9%),22 Kyrgyzstan (48.6%),23 Switzerland (17.5%)20 and the USA (30%).26 This difference might be due to different reasons including study in JUSH included prophylactic use of antimicrobials, the study in the USA is at the outpatient setting where inappropriate prescribing is common, in general.
The prevalence of ADR was found to be 3.06% in this study which was lower than the prevalence in South Korea (62.8%),27 Taiwan (24.1%),28 India (5.53%)29 and JUSH (8.6%).22 This less prevalence of ADR might be because we included the actual ADRs only. However, the finding was higher than the finding in Kerala, India (0.3%).30 The prevalence in our study was much higher than that of Kerala probably following the truth that researchers in Kerala considered reported ADRs only. Underreporting might contribute to underestimation.
Following multivariate analysis, predictors of antimicrobial use problems were identified. This analysis revealed that polypharmacy, unavailability of laboratory results within 48 hours of hospital admission and the coverage of the infectious cases by the national treatment guideline were predictors of the drug therapy problems in this study. Accordingly, compared with those who used less than four drugs during their hospital stay, the use of four to six and seven and above number of different types drugs were found to be determinants for antimicrobial use problems with adjusted odds ratios of 4.024 (2.020–8.017) with p value=0.000 and 13.516 (4.678–39.051) with p value= 0.000, respectively.
The main reason may be that increased number of total drugs used might result in drug–drug interactions leading to adverse drug reactions, diminished effectiveness of one medication due to metabolic actions of other medications, confusion with the regard to medication use resulting in missed doses, extra doses, and other related errors. This was also inline with studies in Norway31 and Singapore32 which revealed that polypharmacy was one of the most important predictors for drug therapy problems and the number of drug-related problems per patient was linearly related to the number of drugs used on admission.
The other independent predictor of antimicrobial use-related problems was the availability of appropriate laboratory values within 48 hours of hospital admission. This can be justified as delayed laboratory values might result in inappropriate drug selection which could be either changed or adjusted later. Or incase there was no appropriate laboratory set up for a particular case, initiation of empirical therapy which depends on clinicians’ expertise disease epidemiology could take place. On top of this, impairment of major organs involved in drug metabolism and excretion, if their functional test was not conducted and appropriate regimen is selected or dose adjusted accordingly, might result in drug therapy problems.
The third independent predictor of antimicrobial use problem showed by multivariate analysis was the inclusion of infectious disease in the national guidelines. Compared with those patients whose cases were covered by national guidelines, patients whose cases were not addressed by national guidelines encountered significantly higher antimicrobial use problems (AOR: 3.328 [1.015–10.909] with p vaue= 0.047).
This finding was inline with a study done in Jimma22 and it may be due to lack of standardized approach consistent for all clinicians in the absence of national guidelines and the practice may vary among different physicians. Additionally, a study conducted in Kazakhstan33 over eight years revealed that regardless of a decrease in the total consumption of antibacterial, there was an irrational use of drugs urging the development of appropriate guidelines and such initiatives enhanced appropriate use of antibiotics in Republic of Srpska.34 So, the researchers strongly recommend availing comprehensive and update guidelines as it significantly decreases this inconsistent use of antimicrobials which results in antimicrobial use problems.
Conclusion
Antimicrobial use problem was prevalent and was detected in most of the patients with 0.94-problems-per-patient. Most of the drug therapy problems were due to the unavailability of the preferred antimicrobial regimen, inability of confirming the infection and identifying the infecting agent, and lack of antimicrobial use guidelines. Polypharmacy, coverage of the national guidelines and availing laboratory values within 48 hours of hospital admission were independent determinants of antimicrobial use problems.
Abbreviations
ADR, Adverse Drug Reactions; AOR, Adjusted Odds Ratio; CPGs, Clinical Practice Guidelines; DTP, Drug Therapy Problems; DURH, Dilla University Referral Hospital; ETB, Ethiopian Birr; JUSH, Jimma University Specialized Hospital; USA, United States of America.
Acknowledgments
We are grateful to Dilla University Referral Hospital management and health care professionals who supported us during the data collection. Our appreciation also goes to the data collectors who showed the maximum effort in acquiring appropriate data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ferech M, Coenen S, Malhotra Kumar S, Dvorakova K, Hendrickx E, Suetens C. European surveillance of antimicrobial consumption (ESAC): outpatient antibiotic use in Europe. J Antimicrob Chemother. 2006;58(2):401–407. doi:10.1093/jac/dkl188
2. Van Bijnen EM, Den Heijer CD, Paget WJ, et al. The appropriateness of prescribing antibiotics in the community in Europe. BMC Infect Dis. 2011;11(293). doi:10.1186/1471-2334-11-293.
3. Ahiabu MA, Tersbol BP, Biritwum R, Bygbjerg IC, Magnussen P. A retrospective audit of antibiotic prescriptions in primary health-care facilities in Eastern Region,Ghana. Health Policy Plan. 2015;31(2):250–258. doi:10.1093/heapol/czv048
4. Aryanti R, Hilbrand H. Determinants of Antimicrobial Use in the Developing World. Child Health Research Project Special Report. 2002;4(1):5–22. Available from: https://www.scribd.com/document/379817732/Determinants-of-Antimicrobial-Use-in-the-Developing-World. Accessed June 8, 2020.
5. Kardas P, Devine S, Golembesky A, Roberts C. A systematicreviewandmeta-analysis of misuse of antibiotic therapies in the community. Int J Antimicrob Agents. 2005;26(2):106–113. doi:10.1016/j.ijantimicag.2005.04.017
6. Blix HS, Viktil KK, Moger TA, Reikvam A. Risk of drug-related problems for various antibiotics in hospital: assessment by use of a novel method. Pharmacoepidemiol Drug Saf. 2008;17(8):834–841. doi:10.1002/pds.1595
7. Implementing Antimicrobial Stewardship Programs in Health Systems. Continuing Education Discussion Guide; 2011:2–11
8. Burke J. Maximizing appropriate antibiotic prophylaxis for surgical patients. Clin Infect Dis. 2001;33(2):78–83. doi:10.1086/321861
9. WHO. The World Health Report. A Safer Future: Global Public Health Security in the 21st Century; 2007.
10. WHO. Antimicrobial Resistance Fact Sheet N°194; 2015.
11. WHO: Antimicrobial resistance; Fact sheets, Available from: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
12. Superbugs. Use of Antimicrobial Medicines. At Issue Health. Green Haven Publishing:66. ISBN: 987-0-7377-7656-0
13. Suttajit S, Wagner AK, Tantipidoke R, Ross-Degnan D, Sitthi-amorn C. Patterns, appropriateness, and predictors of antimicrobial prescribing for adults with upper respiratory infections in urban slum communities of Bangkok. Southeast Asian J Trop Med Public Health. 2005;36(2):489–497.
14. WHO. Worldwide Country Situation Analysis: Response to Antimicrobial Resistance; 2015.
15. Nina S, Victor L. Rational empiric antibiotic prescription in the ICU. CHEST. 2000;117(5):1496–1499. doi:10.1378/chest.117.5.1496
16. Banja WD. Antibiotic Use in Two Hospitals in West Wollega, Ethiopia. Nelson Mandela Metropolitan University; 2007:33–77.
17. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management.
18. Toubes E, Singh K, Yin D, et al. Risk factors for antibiotic-resistant infection and treatment outcomes among hospitalized patients transferred from long-term care facilities: does antimicrobial choice make a difference? Clin Infect Dis. 2003;36(6):724–730. doi:10.1086/368081
19. Ceyhan M, Yildirim I, Ecevit C, et al. Inappropriate antimicrobial use in Turkish pediatric hospitals: a multicenter point prevalence survey. Int J Infect Dis. 2010;14(1):e55—61. doi:10.1016/j.ijid.2009.03.013
20. Cusini A, Rampini SK, Bansal V, et al. Different patterns of inappropriate antimicrobial use in surgical and medical units at a tertiary care hospital in Switzerland: a prevalence survey. PLoS One. 2010;5(11):e14011.
21. Tefera GM, Feyisa BB, Kebede TM. Antimicrobial use–related problems and their costs in surgery ward of Jimma University Medical Center: prospective observational study. PLoS One. 2019;14(5):e0216770.
22. Yadesa TM, Gudina EK, Angamo MT. Antimicrobial use-related problems and predictors among hospitalized medical in patients in Southwest Ethiopia: prospective observational study. PLoS One. 2015;10(12):e0138385. doi:10.1371/journal.pone.0138385
23. Baktygul K, Marat B, Ashirali Z, Harun-or-rashid MD, Sakamoto J. An assessment of antibiotics prescribed at the secondary health-care level in the Kyrgyz republic. Nagoya J. Med. Sci. 2011;73(3–4):157–168.
24. Azza MH, Omaima I, Magdy EG. Surveillance of antibiotic use and resistance in orthopaedic department in an Egyptian university hospital. Int J Infect Control. 2011;7(1).
25. Fernandes M, Leite A, Basto M, et al. Non-adherence to antibiotic therapy in patients visiting community pharmacies. Int J Clin Pharm. 2014;36(1):86–91. doi:10.1007/s11096-013-9850-4
26. Cipolle RJ, Linda MS, Peter CM. Pharmaceutical Care Practices: The Clinician’s Guide.
27. Jung IY, Kim JJ, Lee SJ, et al. Antibiotic-related adverse drug reactions at a tertiary care hospital in South Korea. Biomed Res Int. 2017. doi:10.1155/2017/4304973
28. Sun HY, Chen YC, Wang YW, Gau CS, Chang SC. A prospective study of antimicrobial-related adverse drug reactions in hospitalized patients. J Microbiol Immunol Infect. 2008;41(2):151–159.
29. Jindal M, Sharma RK. Antimicrobial-related adverse drug reaction In a tertiary care hospital. Asian J Pharm Clin Res. 2017;10(8):229–231.
30. Shamna M, Dilip C, Ajmal M, et al. A prospective study on adverse drug reactions of antibiotics in a tertiary care hospital. Saudi Pharm J. 2014;22(4):303–308. doi:10.1016/j.jsps.2013.06.004
31. Viktil KK, Blix HS, Moger TA, Reikvam A. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br J Clin Pharmacol. 2007;63(2):187–195. doi:10.1111/j.1365-2125.2006.02744.x
32. Koh Y, BteMoideenKutty F, Li SC. Drug-related problems in hospitalized patients on polypharmacy: the influence of age and gender. Ther Clin Risk Manag. 2005;1(1):39–48. doi:10.2147/tcrm.1.1.39.53597
33. Zhussupova G, Skvirskaya G, Reshetnikov V, et al. The evaluation of antibiotic consumption at the inpatient level in Kazakhstan from 2011 to 2018. Antibiotics. 2020;9(2):57. doi:10.3390/antibiotics9020057
34. Bojanic L, Markovic-Pekovic V, Skrbic R, et al. Recent initiatives in the Republic of Srpska to enhance appropriate use of antibiotics in ambulatory care; their influence and implications. Front Pharmacol. 2018;9:442. doi:10.3389/fphar.2018.00442
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
