Back to Journals » Cancer Management and Research » Volume 12
A Sensitive and Simplified Classifier of Cervical Lesions Based on a Methylation-Specific PCR Assay: A Chinese Cohort Study
Authors Zhang L , Yu J, Huang W, Zhang H , Xu J, Cai H
Received 16 January 2020
Accepted for publication 24 March 2020
Published 15 April 2020 Volume 2020:12 Pages 2567—2576
DOI https://doi.org/10.2147/CMAR.S246103
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kenan Onel
Lei Zhang,1,* Jing Yu,1,* Wenxian Huang,2 Hongping Zhang,1 Jian Xu,3 Hongning Cai4
1Department of Gynecology, Yunnan Tumor Hospital and The Third Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, People’s Republic of China; 2Department of Pathology, Renmin Hospital of Wuhan University, Wuhan, Hubei, People’s Republic of China; 3Department of Clinical Lab, Weifang Maternal and Child Health Hospital, Weifang, Shandong, People’s Republic of China; 4Maternal and Child Health Hospital of Hubei Province and Women and Children’s Hospital of Hubei Province, Wuhan, Hubei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongning Cai
Department of Gynecology Oncology, Hubei Maternal and Child Health Hospital, No. 745 Wuluo Road, Hongshan District, Wuhan, Hubei, People’s Republic of China
Email [email protected]
Jian Xu
Department of Clinical Lab, Weifang Maternal and Child Health Hospital, Weifang, Shangdong, People’s Republic of China
Email [email protected]
Objective: The aim of this study is to assess the diagnostic and screening performance of a standardized methylation-specific real-time PCR assay targeting SOX1 and PAX1 genes for cervical cancer in a Chinese cohort.
Methods: Genomic DNA was extracted from cervical exfoliated cells and converted by sodium bisulfite and then analyzed by qMSP assay. Ct values were collected for PAX1 and SOX1 as target genes and β-actin as an endogenous reference gene. The samples included 295 cervicitis, 111 LSIL (low-grade squamous intraepithelial lesion), 51 HSIL (high-grade squamous intraepithelial lesion) and 30 cervical cancer.
Results: The Ct values decreased with the progression of cervical cancer from cervicitis, through LSIL and HSIL to cancer. The difference in Ct values between cytological grades was highly significant (p≤ 0.01) between grades either for PAX1 or for SOX1 except the difference between cervicitis and LSIL of SOX1. With the Ct cut-off values of PAX1 gene and SOX1 gene 38.6 and 38 and with the PAX1/SOX1 in combination, the positive rate of methylation in invasive cancer tissues was 100%, in contrast to 11.5% (95% CI: 8.67%– 14.33%) in cervicitis tissues, 45.1% (95% CI: 40.68%– 49.52%) in LSIL tissues, and 68.5% (95% CI: 64.37%– 72.63%) in HSIL tissues. The specificity and sensitivity of differentiating tumors from cervicitis were 0.957 (95% CI: 0.939– 0.975) and 1.00, respectively. The specificity and sensitivity of differentiation between cervicitis+LSIL and HSIL+cervical cancer were 0.881 (95% CI: 0.852– 0.91) and 0.748 (95% CI: 0.709– 0.787), respectively.
Conclusion: PAX1/SOX1 methylation could be translated into clinical practice for cervical neoplasia detection.
Keywords: Cervical cancer, DNA methylation, PAX1, SOX1, DMRs, qMSP detection
Introduction
Cervical cancer is among the most common gynecological malignant tumors in the world.1 It ranks second only to breast cancer in female malignant tumors.1 There are about 570,000 new cases and 311,000 deaths worldwide in 2015.1 Scientific research has confirmed that persistent infection of high-risk papillomavirus (hrHPV) is the main cause of cervical cancer.2,3 The development of invasive cervical cancers from the initial viral infections takes decades.4 Only if a standard physical examination is regularly made, more than 90% of cervical cancer can be found and prevented.5 Therefore, the selection of appropriate and effective diagnostic methods is of great significance for the prevention and treatment of cervical cancer.
At present, the regular methods for cervical cancer screen are Pap smear, HPV DNA detection and colposcopy.6 The successful promotion of Pap smear has greatly reduced the mortality and morbidity for patients with invasive cervical cancers in the past decades, but the accuracy of the tests varies greatly in different regions, depending on the performance of health care infrastructures and the experience of pathologists.7 HPV DNA detection is highly sensitive but poorly specific.7 Colposcopy is highly specific, but it requires a highly qualified operator.7 For this reason, new biomarkers for cervical intraepithelial neoplasia2+ have been identified with great effort to improve risk stratification, and to distinguish women with benign lesion from those who require more intensive management.8–10
Epigenetic changes may play a part in the development of cervical cancer which indicates that DNA methylation may be useful as a marker for cervical cancer screening.8–10 In 2008, Lai et al found six differentially methylated markers (SOX1, PAX1, LMX1A, NKX6-1, WT1 and OMECUT1) related to cervical cancer through methylation chips.11 Lim et al revealed that the methylation level of PAX1 gene gradually increased with the progression of cervical lesions.12 Sex determining region Y-box 1 (SOX1)13 gene and Paired box 1 (PAX1) gene,14 are tumor suppressors, which can inhibit cell proliferation and regulate the expression of invasion-related genes.13 The genes SOX1 and PAX1 have been reported as potential methylation biomarkers and studies have demonstrated their promise in the detection of cervical intraepithelial neoplasms (CIN) grade 3 and worse lesions (CIN3+).15–18 However, the published data were highly heterogeneous. No methylation markers can yet be utilized in cervical cancer screening or triage settings. Similar to other diagnostic molecular approaches, large, well-powered epidemiologic studies are still needed to identify and validate candidate methylation markers of cervical neoplasia. The key problems are: 1) whether the novel system is sensitive and specific enough to rival the traditional methods or become a complementary means of traditional cytological detection and HPV DNA detection; 2) whether the methylation detection system can be standardized and convenient for clinical application; 3) whether the novel system is population specific or regionally specific? All of these need to be tested by extensive and in-depth practice.
This study is intended to evaluate the diagnostic and screening performance of a methylation- specific real-time PCR assay, targeting the differentially methylated regions (DMRs) of PAX1 and SOX1 genes for cervical cancer in a Chinese cohort.
Materials and Methods
Patients and Clinical Specimens
During the period from October 2016 to December 2017, 487 specimens were collected from four medical centers in China, in order to assess the diagnostic and screening performance of the methylation detection kit ICervsureTM. 487 specimens were divided into two groups: the case group and control group. The case group included 111 LSIL (low-grade squamous intraepithelial lesion), 51 HSIL (high-grade squamous intraepithelial lesion) and 30 CSCC (cervical squamous cell carcinoma). The control group included 295 cervicitis confirmed by cytological examination.
All the case group patients were diagnosed as LSIL, HSIL or CSCC by cervical biopsy under colposcopy. The control group patients were recruited from healthy women who received routine screening, and were diagnosed as cervicitis by histopathological examination. This study was approved by the Ethics Committee of Yunnan Tumor Hospital (the Third Affiliated Hospital of Kunming Medical University), Weifang Maternal and Child Health Hospital, Renmin Hospital of Wuhan University and Maternal and Child Health Hospital of Hubei Province (Women and Children’s Hospital of Hubei Province) in China and was performed in accordance with the Helsinki Declaration. All participants provided written informed consent. All specimens were numbered and delinked from clinical information until data analysis.
The included specimens followed the criteria below: 1) women aged from 25 to 70 years, 2) women who had undergone cervical biopsy under colposcopy and diagnosed as LSIL, HSIL or CSCC and 3) women with clear results of histopathological examination and HPV test. The specimens with the following properties were excluded: patients having other malignant tumors, immunocompromised diseases, history of radio or chemotherapy, other cervical lesions, cervical surgery or current pregnancy.
Sampling Methods for Clinical Specimens
The specimens used in evaluation of the performance of the detection kit ICervsureTM were cervical exfoliated cells. Sampling was made as follows:
Patients took bladder lithotomy position, fully exposed the cervix, and removed from the excessive secretions. The tip of the sample brush was inserted into and pushed forward against the cervix. The brush was rotated in the same direction for 5 rounds. Immediately after sampling, the cervical exfoliated cells were put into the cell preservation solution and stored at 2–8° C for not more than 4 months. The cervical exfoliated cell preservation solution was bought from Hubei Ruixinchang Biotechnology Co., Ltd. (Ehan Equipment 20150189).
DNA Extraction and Bisulfite Transformation
Genomic DNA was extracted from clinical specimens using the Nucleic Acid Extraction and Purification kit (Wuhan Ammunition Life Science and Technology Co., Ltd, Wuhan, China) according to the manufacturer’s protocol. Sodium bisulfite treatment of genomic DNA from 1.4mL cell suspension was performed using the Bisulfite Conversion Kit (Wuhan Ammunition Life Science and Technology Co., Ltd, Wuhan, China) according to the manufacturer’s manual. The bisulfited DNA was stored at −80°C until using.
qMSP Analysis with the Detection Kit ICervsureTM
The ServsureTM is a methylation-specific detection kit developed by Wuhan Ammunition Life Science and Technology Co., Ltd. The testing information about the ICervsure kit can be found at http://www.ammulifetech.com/aigongshu.html, and information about the vendor at http://www.ammulifetech.com/. It is built on real-time multiplex polymerase chain reaction (qMSP) targeting the Sex determining region Y-box 1 (SOX1) gene and Paired box 1 (PAX1) gene. qMSP analysis was performed according to the manufacturer’s instruction of the detection kit ICervsureTM.
For the amplification reaction, 2 μL bisulfite-treated DNA (50 ng) was added in 25 μL amplification mix containing 1× Multiplex mix, 120nM of each primer (β-actin, PAX1 and SOX1), and 120 nM of TaqMan probe of each target. Amplification and real-time measurement were performed in the 7500 ABI system (Applied Biosystems, Foster City, CA, USA), using the following conditions: 10 min at 95°C followed by 45 cycles of 20 s at 95°C and 45 cycles of 30 s at 60°C.
Test Results Analysis
After qMSP amplification, 3 Ct values of PAX1, SOX1, and β-actin were produced from each sample. Ct values of PAX1, SOX1, and β-actin and the results of cytological tests from the 487 specimens were summarized in Supplementary 1. Negative results showing no amplified signal were given Ct = 45. Testing results with Ct values of β-actin≥36 were defined as detection failure. For each sample, qMSP positivity was identified according to the Ct cut-off values (Ct=38 for PAX1 and Ct=38.6 for SOX1). For each gene PAX1 or SOX1, the sample was described as positive when its Ct value was lower than the cut-off value and as negative when its Ct value was higher than the cut-off value. For a combination of PAX1 and SOX1, the sample was defined as positive only if any of these two genes showed a positive result.
The cut-off value of qMSP was determined by 10-time 10-fold cross-validation method. 487 clinical samples of cervical cancer (Supplementary Table 1) were split into 10 shares. Nine of them served as training data and one as testing data in turn. Correctness (or error rate) was obtained in each test. The accuracy (or error rate) data of 10 experiments were averaged to estimate the sensitivity of the algorithm. 10-fold cross-validation was repeated 10 times (10-fold cross-validation). The sensitivity value of each time was averaged as an estimate of the accuracy of the algorithm. According to the accuracy data obtained by 10-fold cross-validation, ROC curves and all associated statistics were generated. The optimal cut-off values were determined as maximizing the sum of sensitivity plus specificity.
On this basis, the positive rates of PAX1 and SOX1 methylation in specimens with different progression of disease were calculated.
Data Processing
SPSS 17.0 (IBM Corporation, Armonk, NY, USA) software was used for statistical analyses. Ct values obtained by qMSP were analyzed (Table 1) and plotted (Figure 1) according to clinical status using the exploration analysis of the description function. Two ended group-wise t test was used for the difference in the methylation level between different clinical states.
 |
Table 1 Statistical Features of Ct Values of DMR Genes PAX1, SOX1 and the Endogenous Gene β-Actin |
A “true positive” is the event that the test makes a positive prediction, and the subject has a positive result under the gold standard, and a “false positive” is the event that the test makes a positive prediction, and the subject has a negative result under the gold standard. Let A=true positive, B=false positive, C=true negative, D=false negative, then we have Sensitivity=A/(A+C)×100%, Specificity=D/(D+B) ×100%, and the Positive Predictive Value (PPV) =A/(A+B) × 100%.
Results and Analysis
Distribution of Ct Values of DMRs Was Closely Related to the Disease Progression of Cervical Cancer
According to cytological examination, 295 out of 487 patients were diagnosed with cervicitis, 51 with LSIL, 111 with HSIL and 30 with CC. In this study, 487 specimens were tested with the methylation detection kit ICervsureTM. The Ct values of PAX1, SOX2 and β-actin were produced for each specimen and analyzed by the exploratory analysis using SPSS software (Figure 1).
Figure 1 displays the exploratory data analysis of Ct values of the DMRs (PAX1, SOX1) in 487 patients. Each cytological grade composes of three box plots, representing the distribution of the Ct value of DMRs (PAX1 and SOX1) and the endogenous reference gene β-actin, respectively. The extremes of the boxes define the upper and lower quartiles and the centre lines define the median. Whiskers indicate 1.5× interquartile range (IQR). Beyond IQR are defined as the outliers. The black point indicates the extraordinary value which is 1.5 times the box height away from the upper or lower edge of the box. The asterisk * represents the extreme value, which is three times the box height away from the upper or lower edge of the box.
No matter what grade of the tissue (either cervicitis, LSIL, HSIL or cancer), the Ct value of endogenous reference gene β-actin varies slightly from 26.3±1.0 to 26.8 ±1.2, indicating that Ct value of β-actin gene was very consistent and no relationship with the progression of cervical cancer, and that the DNA quality and quantity of the detection system are well controlled. Ct values of precancerous lesion samples (LSIL and HSIL) vary greatly, while the Ct values of cancer tissues are relatively concentrated. The Ct value of PAX1 ranged from Ct=45 of cervical inflammation to Ct=29.9 of cancer. Similarly, Ct value of DMRSOX1 ranged from Ct=45 of cervical inflammation to Ct=29.2 of cancer.
Table 1 indicates the statistical features of Ct values of DMR genes PAX1, SOX1 and the endogenous gene β-actin. Mean Ct values of PAX1 were 43.4,39.7,36.9 and 30.5 for cervicitis, LSIL, HSIL and cancer, respectively, indicating that Ct values decreased with the progression of cervical cancer. The same trend was demonstrated for SOX1. It is worth noticing that the variation of Ct value in LSIL (SD=4.6 for PAX1, SD=4.8 for SOX1) and HSIL (SD=5.2 for PAX1, SD=6.5 for SOX1) is significantly larger than cervicitis (SD=2.9 for PAX1, SD=2.3 for SOX1) and cancer (SD=2.4 for PAX1, SD=1.0 for SOX1).
Ct values of different grades of the specimens were compared by t test. The difference in Ct value between cytological grades was highly significant (p≤0.01) between grades either for PAX1 or for SOX1 except the difference between cervicitis and LSIL of SOX1. It is indicated that there is a tendency that the more severe the disease the lower the Ct value, suggesting that the Ct value may become an indicator of cancer progression.
A Ct Cut-off Value Clearly Distinguishes Cancer from Non-Cancer Specimens
In order to evaluate the performance of the detection kit ICervsureTM in diagnosis of cervical cancer, ROC curve analysis was carried out (Figure 2). The specificity, sensitivity and AUC values are summarized in Table 2.
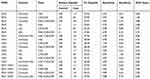 |
Table 2 Performance of the qMSP System in Detection of Clinical Specimens of Cervical Cancer |
 |
Figure 2 ROC curves of PAX1 and SOX1 assayed on scrapings of 487 patients (A–C). |
For cancer versus cervicitis, the specificity and sensitivity are 0.936 (95% CI: 0.914–0.958) and 1.00, respectively, for the PAX1 at the Ct cut-off value of 37.82; 0.996 (95% CI: 0.99–1.00) and 0.963 (95% CI: 0.946–0.980) for SOX1 at the Ct cut-off value of 32.20; 0.996 (95% CI: 0.99–1.00) and 1.00 for the combination of PAX1 and SOX1 at Ct cut-off value 31.93.
For HSIL+cancer versus cervicitis+LSIL, the specificity and sensitivity are 0.90 (95% CI: 0.873–0.927) and 0.75 (95% CI: 0.712–0.788), respectively, for PAX11 at the Ct cut-off value of 37.95; 0.926 (95% CI: 0.903–0.949) and 0.654 (95% CI: 0.612–0.696) for the SOX1 at the Ct cut-off value of 38.58; 0.881 (95% CI: 0.852–0.910) and 0.748 (95% CI: 0.709–0.787) for the combination of PAX1 and SOX1 at the cut-off value of 37.92.
Considering all the situations as shown in Table 2, we decided to choose Ct=38.0 as the cut-off value of PAX1 and Ct=38.6 as the cut-off value of SOX1 in the qMSP detection of the clinical specimens of cervical cancer. That is, the specimen is considered methylation positive when the qMSP Ct≤38.0 for PAX1 or qMSP Ct≤38.6 for SOX1. The specimen is considered methylation negative when the qMSP Ct≥38.0 for PAX1 and qMSP Ct≥38.6 for SOX1.
Methylation Rate Increases with the Progression of Cervical Cancer
Based on the Ct cut-off value (Ct=38 for PAX1 and 38.6 for SOX1), we were trying to transform quantitative Ct values into qualitative classification or positivity. Based on this classification, the positive rate was investigated for various grades of specimens. It was shown that the positive rate increased gradually with the disease progression regardless of PAX1 or SOX1 as the target. Results of qMSP detection were significantly positively correlated between PAX1 and SOX1 with the correlation coefficient r=0.8473.
As can be noted from Figure 3 that the probability of positive results increases with the progression of the disease. Single gene detection (PAX1 or SOX1) showed the same trend as double genes in combination. The positive rate of PAX1 was a little higher than that of SOX1 in cervical cancer samples of any grade. The detection rate of double gene detection was slightly higher than that of a single gene.
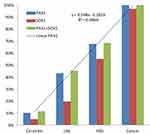 |
Figure 3 Detection rate of methylation among different cytological stages of cervical cancer. |
The frequency of methylation at both the PAX1 and SOX1 increases with the increase of disease progression. For cancer samples, the methylation frequency of PAX1 arrived at 100%. For the same grade samples, the methylation frequency of PAX1 was consistently higher than that of SOX1. The methylation frequency of PAX1 in LSIL samples amounted to 43.7% (95% CI: 39.3%-48.1%), while that of SOX1 samples was only 19.6% (95% CI: 16.1%-23.1%). The methylation frequency of PAX1 in HSIL samples was as high as 68.8% (95% CI: 64.7%-72.9%), while that of SOX1 samples was only 55.9% (95% CI: 51.5%-60.3%).
Clinical Specificity and Sensitivity Allows Practical Utility for Early Detection of Cervical Cancer
When PAX1 and SOX1 genes were detected separately, the specificity and sensitivity of PAX1 for cervical cancer were 0.934 (95% CI: 0.911–0.956) and 1.00, respectively, and that of SOX1 was 0.996 (95% CI: 0.990–1.00) and 0.963 (95% CI: 0.946–0.980). For the detection of LISIL and its above (LSIL, HSIL and CC), the positive coincidence rate, negative coincidence rate and total coincidence rate of PAX 1 were 73.9%, 88.8%, 84.5%, and those of SOX1 were 64.6%, 93.1% and 84.7%, respectively.
When PAX1 and SOX1 genes were detected in combination, the specificity and sensitivity of differentiating tumors from inflammation were 0.957 (95% CI: 0.939–0.975) and 1.00, respectively. The specificity and sensitivity of differentiation between inflammation + LSIL and HSIL + cervical cancer were 0.881 (95% CI: 0.852–0.709) and 0.748 (95% CI: 0.709–0.787), respectively.
Discussion
Cervical cancer is caused by human papillomavirus (HPV), which can be prevented and treated by HPV screening.7 However, this virus infection is very common, and in most cases infected cervical cells do not turn into cervical cancer.7 Therefore, positive HPV test results also need follow-up testing to the risk of each patient. Cytological examination is the primary shunt method at present, however, it lacks sensitivity and depends on experience. In these circumstances, ICervsureTM detection serves as a highly sensitive and specific tool for patients and doctors.
According to the meta analysis15 of PAX1 and SOX1 methylation as an initial screening method for cervical cancer, the pooled sensitivity, and specificity for PAX1 methylation test were 0.73 (95% CI: 0.70–0.75) and 0.87 (95% CI: 0.85–0.89), respectively, versus those of 0.71 (95% CI: 0.67–0.74) and 0.64 (95% CI: 0.61–0.67) for SOX1 methylation. Paralleled PAX1/SOX1 tests achieved AUC values of 0.89, under which, the pooled sensitivity was 0.72 (95% CI: 0.69–0.74); the pooled specificity was 0.77 (95% CI: 0.76–0.79), respectively. For the HPV DNA testing, it yielded a pooled sensitivity of 0.81 (95% CI: 0.77–0.85) and specificity of 0.70 (95% CI: 0.67–0.72). With a combination of PAX1 and SOX1 in this study, the detection rates of LSIL, HSIL and cervical cancer were 46% (95% CI: 41.6%-50.4%), 67.6% (95% CI: 63.4%-71.8%) and 100%, respectively. The specificity and sensitivity to distinguish between cervicitis and cervical cancer were 100% and 95.7% (95% CI: 93.9%-97.5%). The performance of ICervsureTM has updated the best record of qMSP assay targeting PAX1/SOX1 for cervical cancer and better than HPV DNA testing. In the present study, methylated CpG sites were recognized using specific primers and Taqman probes. Furthermore, the detection of fluorescence-labeled amplicons allows the sensitive and real-time measurement of the amplicons, thus enabling accurate quantification.
The positive predictive value of ICervsureTM was 107/152 = 70.39%, which is significantly higher than that of HPV (77/125 = 61.6%). Because most negative samples did not provide HPV test results, the positive predictive value of HPV in this experiment was considerably overestimated. Even this, ICervsureTM had significantly higher positive predictive value. Combined with HPV detection and ICervsureTM detection, the overall positive predictive value reached 81.9%. That is to say, positive predictive value of ICervsureTM is higher than HPV detection and the combination of ICervsureTM and HPV detection can improve the overall positive predictive value for cervical cancer detection. This is in accord with Tian et al19 and Lorincz et al.20 Tian et al also found that the dual methylated markers PAX1/ZNF582 resulted in a referral rate for colposcopic examination that was 24.4% of the rate for cytology.20
By now two reagent kits have been registered for cervical cancer detection worldwide. One is GynTect® produced by Oncgnostics company of German and another is QIAsure® by QIAGEN and Self-screen BV company. According to the product specifications for GynTect® available from https://www.oncgnostics.com/wp-content/uploads/2018/02/Eurogin-2017-talk.pdf and for QIAsure® available from http://www.egrinternational.com/QIAGEN/WomensHealth/QIAsure/PDF/Clinical-Data.pdf, the sensitivity of cancer detection is the same 100% for ICervsureTM, GynTect and QIAsure, but ICervsureTM has the highest sensitivity of HSIL detection, being 76/111=68.5% (ICervsureTM) > 53/80=66.3% (QIAsure®) > 30/49=61.2% (GynTect®). Sensitivity of HSIL+ detection was 250/331=83.1% (QIAsure®) > 107/142=75.4% (ICervsureTM) > 35/54=64.8% (GynTect. The specificity was 210/222=94.6% (QIAsure®) > 302/347=87.0% (ICervsureTM) > 133/160=75.5% (GynTect). ICervsureTM possesses moderate and balanced sensitivity and specificity.
There have been numerous studies on use of DMRs for cancer diagnosis. Methylation index has been the most frequently used to evaluate the methylation level with qMSP. There are a variety of methods for calculating methylation index (MI), including MI21=ΔCt, MI22=2−ΔCt MI17=10,000 × 2ΔCt where ΔCt=Ct(Target)-Ct(Endogenous reference). MI22=2−ΔΔCt where ΔΔCt = ΔCtsample - ΔCtcalibrator. MI17= Ct(Target)/Ct(Endogenous reference) and so on.22,23 The cycle threshold (Ct) values for each target were normalized for DNA input. The values for all samples were transformed into relative quantity. However, we found that the amplification efficiency of PAX1, SOX1 and β-actin was 1.04, 1.00 and 1.03, respectively and no significant difference between them. By strictly monitoring the initial sample size and controlling the Ct value of β-actin within a range of 26.5±1.2, the Ct value of DMRs becomes directly comparable. In this paper, we directly adopt Ct value to measure the methylation level and then convert the Ct value into methylation positivity according to the Ct cut point. This improvement greatly helps with the clinical application. The performance of PAX1 in combination with SOX1 seems not significantly better than that of the PAX1 single gene, although the combined test showed a slight improvement in precancerous detection (Figure 3). Further research is needed to determine whether the PAX1/SOX1 combination is superior to the PAX1 single gene.
Conclusion
PAX1 or SOX1 methylation could potentially be treated as an auxiliary biomarker for cervical cancer screening. With ICervsureTM we provide a molecular test on the basis of epigenetic markers, which allows the triage of patients with an abnormal Pap smear and subsequent positive HPV test result. In contrast to other methods available in cervical cancer screening ICervsureTM will have the potential to decrease the high number of unnecessary cervical biopsies and surgeries.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This work was supported by a grant from the Internal Research Institutions Foundation of Medical and Health Units in Yunnan Province (No.2018NS0063), and by a joint project of Hubei Provincial Health and Family Planning Commission (WJ2018H0156) with the title´Research on the diagnosis of cervical lesions based on HPV DNA methylation detection´.
Disclosure
Dr Lei Zhang reports grants from Internal Research Institutions Foundation of Medical and Health Units in Yunnan Province (No.2018NS0063), grants from joint project of Hubei Provincial Health and Family Planning Commission (No. WJ2018H0156), during the conduct of the study. Wuhan Ammunition life-tech Co., Ltd supported the production of testing kits for this project. All the authors declare that they have no other potential conflicts of interest in this study.
References
1. Bray F, Ferlay J, Soerjomataram I, Siege RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. 2018;68:394–424. doi:10.3322/caac.21492
2. Winer RL, Kiviat NB, Hughes JP, et al. Development and duration of human papillomavirus lesions, after initial infection. JID. 2005;191:731–738. doi:10.1086/427557
3. Crosbie EJ, Einstein MH, Franceschi S, Kitchener HC. Human papillomavirus and cervical cancer. Lancet. 2013;382:889–899. doi:10.1016/S0140-6736(13)60022-7
4. Fidler MM, Soerjomataram I, Bray F. A global view on cancer incidence and national levels of the human development index. IJC. 2016;139:2436–2446.
5. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. IJC. 2017;141:664–670.
6. Wright TC
7. Kjaer SK, Frederiksen K, Munk C, Iftner T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. JNCI. 2010;102:1478–1488. doi:10.1093/jnci/djq356
8. Wentzensen N, von Knebel Doeberitz M. Biomarkers in cervical cancer screening. Dis Markers. 2007;23:315–330. doi:10.1155/2007/678793
9. Shivapurkar N, Sherman ME, Stastny V, et al. Evaluation of candidate methylation markers to detect cervical neoplasia. Gynecol Oncol. 2007;107:549–553. doi:10.1016/j.ygyno.2007.08.057
10. Wentzensen N, Sherman ME, Schiffman M, Wang SS. Utility of methylation markers in cervical cancer early detection: appraisal of the state-of-the-science. Gynecol Oncol. 2009;112:293–299. doi:10.1016/j.ygyno.2008.10.012
11. Lai HC, Lin YW, Huang TH, et al. Identification of novel DNA methylation markers in cervical cancer. Int J Cancer. 2008;123:161–167. doi:10.1002/ijc.23519
12. Lim EH, Ng SL, Li JL, et al. Cervical dysplasia: assessing methylation status (Methylight) of CCNA1, DAPK1, HS3ST2, PAX1 and TFPI2 to improve diagnostic accuracy. Gynecol Oncol. 2010;119:225–231. doi:10.1016/j.ygyno.2010.07.028
13. Tsao CM, Yan MD, Shih YL, et al. SOX1 functions as a tumor suppressor by antagonizing the WNT/β‐catenin signaling pathway in hepatocellular carcinoma. Hepatology. 2012;56(6):2277–2287. doi:10.1002/hep.25933
14. Maulbecker CC, Gruss P. The oncogenic potential of Pax genes. EMBO J. 1993;12(6):2361–2367. doi:10.1002/j.1460-2075.1993.tb05890.x
15. Chen Y, Cui ZL, Xiao ZZ, et al. PAX1 and SOX1 methylation as an initial screening method for cervical cancer: a meta-analysis of individual studies in Asians. Ann Transl Med. 2016;4(19):365. doi:10.21037/atm.2016.09.30
16. Lai HC, Ou YC, Chen TC, et al. PAX1/SOX1 DNA methylation and cervical neoplasia detection: a Taiwanese gynecologic oncology group (TGOG) study. Cancer Med. 2014;3:1062–1074. doi:10.1002/cam4.253
17. Huang TH, Lai HC, Liu HW, et al. Quantitative analysis of methylation status of the PAX1 gene for detection of cervical cancer. Int J Gynecol Cancer. 2010;20:513–519. doi:10.1111/IGC.0b013e3181c7fe6e
18. Luan T, Hua Q, Liu X, et al. PAX1 methylation as a potential biomarker to predict the progression of cervical intraepithelial neoplasia: a meta-analysis of related studies. Int J Gynecol Cancer. 2017;27:1480–1488. doi:10.1097/IGC.0000000000001011
19. Tian Y, Wu Yuan NY, Liou YL, et al. Utility of gene methylation analysis, cytological examination, and HPV-16/18 genotyping in triage of high-risk human papilloma virus-positive women. Oncotarget. 2017;8(37):62274–62285. doi:10.18632/oncotarget.19459
20. Lorincz AT, Brentnall AR, Vasiljevic N, et al. HPV16 L1 and L2 DNA methylation predicts high-grade cervical intraepithelial neoplasia in women with mildly abnormal cervical cytology. IJC. 2013;133:637–644.
21. Huang YK, Peng BY, Wu CY, Su CT, Wang HC, Lai HC. DNA methylation of PAX1 as a biomarker for oral squamous cell carcinoma. Clin Oral Invest. 2014;18(3):801–808. doi:10.1007/s00784-013-1048-6
22. Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29(9):e45. doi:10.1093/nar/29.9.e45
23. Huang J, Liou YL, Kang YN, Tan ZR, Peng MJ, Zhou HH. Real-time colorimetric detection of DNA methylation of the PAX1 gene in cervical scrapings for cervical cancer screening with thiol-labeled PCR primers and gold nanoparticles. Int J Nan. 2016;11:5335–5347. doi:10.2147/IJN.S116288
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

