Back to Journals » Clinical Ophthalmology » Volume 13
Comparison Of Surgical Outcomes Of 360° Circumferential Trabeculotomy Versus Sectoral Excisional Goniotomy With The Kahook Dual Blade At 6 Months
Authors Hirabayashi MT , Lee D, King JT , Thomsen S, An JA
Received 10 July 2019
Accepted for publication 27 September 2019
Published 15 October 2019 Volume 2019:13 Pages 2017—2024
DOI https://doi.org/10.2147/OPTH.S208468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Matthew T Hirabayashi,1 Dayeong Lee,1 Joshua T King,1 Samuel Thomsen,1,2 Jella A An1,2
1University of Missouri Columbia School of Medicine, Columbia, MO, USA; 2Department of Ophthalmology, Mason Eye Institute, University of Missouri School of Medicine, Columbia, MO, USA
Correspondence: Jella A An
Department of Ophthalmology, University of Missouri Columbia, 3215 Wingate Court, Columbia, MO 65201, USA
Tel +1 573 884 1311
Fax +1 573 884 3330
Email [email protected]
Purpose: To compare reductions in intraocular pressure (IOP) and IOP-lowering medication use following sectoral excisional goniotomy with the Kahook Dual Blade (KDB) or 360° trabeculotomy (via either Trab360 or gonioscopy-assisted transluminal trabeculotomy [GATT]) in eyes with open-angle glaucoma (OAG) undergoing phacoemulsification cataract surgery.
Methods: A retrospective review was conducted to collect data from adult subjects with early to advanced primary or secondary OAG undergoing phacoemulsification combined with either KDB or 360° trabeculotomy (Trab360 or GATT) between August 1, 2016 and July 30, 2018 for which 6-month follow-up was available. Data collected included IOP, glaucoma medications, adverse events, and additional IOP-lowering procedures. The primary outcome measure was surgical success (≥20% IOP or ≥1 medication reduction without additional IOP-lowering procedures) at 6 months.
Results: Data were collected from 74 eyes of 61 subjects undergoing KDB excisional goniotomy and 27 eyes of 25 subjects undergoing 360° trabeculotomy (19 eyes of 17 subjects undergoing Trab360 and 8 eyes of 8 subjects undergoing GATT). At 6 months, 81.7% (58/71) of KDB eyes and 84.6% (22/26) of 360° trabeculotomy eyes achieved surgical successes (P=0.737). Mean IOP reductions and medication reductions were similar between groups at 6 months. However, more eyes undergoing KDB than Trab360/GATT achieved target IOP ≤18 mmHg (80.0% [56/70] vs 59.3% [16/27], P=0.040) and ≤15 mmHg (61.4% [43/70] vs 25.9% [7/27], P=0.003) without further IOP-lowering interventions at 6 months. The nature and frequency of adverse events were similar between groups.
Conclusions: Both KDB and Trab360 or GATT procedures similarly lowered both IOP and the need for IOP-lowering medications during the first 6 postoperative months. More eyes undergoing KDB excisional goniotomy than 360° trabeculotomy attained target IOP ≤18 mmHg and ≤15 mmHg at 6 months. A full 360° trabecular bypass may not be necessary to achieve maximal efficacy from this class of micro-invasive glaucoma procedures.
Keywords: Kahook Dual Blade, goniotomy, Trab360, GATT, MIGS
Plain Language Summary
Glaucoma is a disease of the optic nerve associated with elevated eye pressure (IOP). New micro-invasive glaucoma surgeries are safer than traditional filtering surgeries and allow for earlier intervention to prevent further glaucoma progression and blindness. Kahook Dual Blade (KDB) Goniotomy and 360° trabeculotomy (Trab360 or gonioscopy-assisted transluminal trabeculotomy [GATT]) are two examples of these procedures and they are easily combined with cataract surgery. KDB typically removes 90°of the trabecular meshwork (circular filtering system responsible for a large portion of the aqueous outflow resistance that causes elevated eye pressure) while Trab360/GATT remove 360°. We found that while both of these procedures are effective and safe in lowering IOP and need for medication without any vision-threatening complications, more eyes treated with KDB achieved lower IOP at 6 months. Our results suggest that removal of the full 360° trabecular meshwork may not be necessary to achieve desirable surgical outcome in adult patients with glaucoma when combined with cataract surgery.
Introduction
The development and commercialization of micro-invasive glaucoma surgeries (MIGS) have expanded the indications for glaucoma surgery. MIGS procedures as initially described in 2012 share in common an ab interno approach, minimal trauma to the target tissue, at least modest efficacy, an extremely high safety profile, and rapid recovery with minimal detrimental impact on quality of life.1 In principle, these were blebless procedures, although more recently, two bleb-based procedures have been developed and are considered to belong in the MIGS family,2–4 one of which requires and ab externo approach,4 demonstrating the broadening of the MIGS umbrella with innovation over time. While traditional procedures such as trabeculectomy and tube-shunt implantation have typically been reserved for eyes recalcitrant to non-surgical therapy, MIGS procedures are now routinely performed in medically well-controlled eyes to reduce the medication burden and as an early intervention in eyes requiring intraocular pressure (IOP) reduction without first exhausting all medication classes and laser options.5–7
MIGS procedures are classified on the basis of their route of aqueous humor drainage: to Schlemm’s canal, the supraciliary space, or the subconjunctival space. Most procedures in common use today seek to bypass the trabecular meshwork (TM), which is the site of aqueous outflow resistance and the reason why IOP is elevated in eyes with primary open-angle glaucoma (POAG). This can be accomplished by incising the TM, excising TM, or by the implantation of a device that shunts aqueous humor across the diseased tissue.5–7 These various approaches have not been comprehensively compared. A single retrospective study compared excisional goniotomy with the Kahook Dual Blade (KDB, New World Medical, Inc, Rancho Cucamonga, CA) to implantation of a trabecular micro-bypass device (iStent, Glaukos, Inc., San Clemente, CA) and found greater IOP and medication reduction in eyes undergoing KDB excisional goniotomy.8 One possible explanation for this difference is the area of improved aqueous filtration: excisional goniotomy typically removes 3–4 clock hours of TM, while the trabecular micro-bypass has a luminal diameter of only 120 microns (<1 clock hour).4
It is reasonable to hypothesize that IOP reduction would be proportional to the extent of diseased TM bypassed to allow aqueous to flow into the distal outflow system. Under such a hypothesis, a 360° trabeculotomy—as can be accomplished by Trab360 (Sight Sciences, Inc., Menlo Park, CA)9 or gonioscopy-assisted transluminal trabeculotomy (GATT)10—should produce greater IOP reductions than the ~120° excisional goniotomy accomplished using the KDB. To address this issue, we report a 6-month retrospective comparison of KDB excisional goniotomy versus 360° trabeculotomy (either Trab360 or GATT) in combination with cataract performed at our institution.
Methods
This was a retrospective analysis of data from adult glaucoma patients undergoing elective phacoemulsification cataract surgery combined with either a sectoral excisional goniotomy (using the Kahook Dual Blade) or a 360° trabeculotomy (using a microcatheter) by or under the direct supervision of a single surgeon (JAA) at the University of Missouri in Columbia from August 1, 2016 to July 30, 2018 (IRB# 2012683). A de-identified data set was analyzed. The protocol was reviewed and approved by the relevant ethics committee (Institutional Review Board), and a waiver of consent was granted. Only procedures performed with cataract extraction were considered as they were most often done together at this institution.
Data were drawn from the charts of adult patients with early to advanced primary or secondary open-angle glaucoma and a visually significant cataract who had a minimum of six months of postoperative follow-up. Data collected included demographic information, visual acuity (VA), IOP, IOP-lowering medications, adverse events, and additional IOP-lowering interventions. VA was measured using the Snellen chart at 20 feet or its equivalent. All IOP assessments were performed by the surgeon or a trained technician using Goldmann applanation tonometry.
Surgical Procedures
All procedures began with a temporal near-clear 2.4 mm incision into the anterior chamber. Patients’ heads were positioned and microscopes adjusted to allow visualization of the nasal angle by Swan-Jacob gonio prism.
Sectoral excisional goniotomy (the KDB group) was performed according to the KDB’s Instructions For Use.11 The KDB was inserted into the anterior chamber and the tip used to make an initial incision into the TM. With its heel resting in Schlemm’s canal, the instrument was then advanced counterclockwise through TM approximately 2 clock hours to one extreme of the planned excision. The instrument was then repositioned at the opposite extreme of the planned excision, approximately 2 clock hours clockwise from the initial entry point, TM engaged once more, and the instrument advanced toward its initial entry point until the full ~4 clock hour length of the intended excision was complete. A single strip of TM spanning approximately 4 clock hours (or 90–120°) was then removed with micro forceps or Utrata forceps.
360° trabeculotomy (the Trab360/GATT group) was performed via one of two procedures: Trab360 or GATT. Trab360 was performed using the manual instrument designed for this procedure as described in its Directions For Use.12 The device was inserted into the anterior chamber. The tip of the instrument was used to make initial incision into the TM, then the catheter was fed into Schlemm’s canal circumferentially 180°, grasped through TM, and pulled to unroof the TM and inner wall of Schlemm’s canal. This was repeated on the remaining 180° of the angle, creating a total 360° circumferential TM incision. GATT was performed using an iTrack illuminated microcatheter according to the procedure’s original description.10 The microcatheter was inserted into the anterior chamber. A 1–2 mm goniotomy was created in the nasal angle with a 25-gauge needle through the temporal incision site. Microsurgical forceps were then introduced through the temporal site and used to feed the catheter into Schlemm’s canal circumferentially 360°. The distal end of the microcatheter was then retrieved with microforceps as it circled around to its original point of entry, and both ends of the catheter were cheesewired, creating a total 360° circumferential TM incision.
Each of the three procedures was followed by standard phacoemulsification with intraocular lens implantation. Viscoelastic was completely removed from the anterior chamber at the end of the procedure. Eyes were filled with balanced salt solution and intracameral moxifloxacin at the conclusion of each surgery to achieve IOP in the mid-20s to minimize blood reflux. Topical broad-spectrum antibiotics were used for 1 week, and prednisolone acetate 1% was tapered from 4 times daily over the first postoperative month. Postoperative hyphema precautions were advised for 2 weeks, including elevating the head of the bed and sleeping with a hard shield. Patients were re-examined 0–1 day, 1–2 weeks, and 1, 3, and 6 months postoperatively. Preoperative IOP-lowering medications were continued in the postoperative period, and if target IOP was achieved, medications were reduced by no more than 1 medication per visit.
Outcomes Assessed
The primary outcome measure was surgical success defined as ≥20% IOP reduction or ≥1 medication reduction without additional IOP-lowering procedures, including laser trabeculoplasty. This two-option goal reflects the indications for surgery, which included IOP reduction in some eyes and medication reduction in others. Secondary outcome measures included the proportion of eyes achieving target IOPs of ≤18 mmHg and ≤15 mmHg, mean IOP and medication reduction, and any complications or additional IOP-lowering procedures needed. For this analysis, an IOP spike was defined as IOP >30 mmHg at any time point, and a steroid response was defined as IOP ≥28 mmHg and >25% increased from baseline while on topical prednisolone with subsequent IOP reduction >25% upon discontinuation of prednisolone.19 Early postoperative reflux microhyphema is common to all angle surgeries and was noted but was not considered an adverse event within the first 2 postoperative weeks, unless it required treatment.
Analysis
Data were analyzed in SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). Two-tailed independent t-tests or Mann Whitney U and chi-square or Fisher’s exact tests were employed to assess baseline characteristics. A logistic regression with fixed patient effect was conducted to assess for associations between type of goniotomy procedure and success, achievement of 6-month target IOPs, complications, and additional procedures. A generalized linear mixed model was used to determine the relationship between goniotomy procedure and IOP or medication reduction, to account for the contribution of both eyes in some subjects. The level of significance was taken to be <0.05. Values are reported as mean ± standard deviation (SD) for normally distributed data, median and interquartile range (IQR) for non-normally distributed data, and percentages for categorical variables unless otherwise specified.
Results
Overall, data were drawn from the health records of 74 eyes from 61 patients undergoing sectoral excisional goniotomy with the KDB and 27 eyes of 25 patients undergoing 360° trabeculotomy (19 eyes of 17 patients via Trab360 and 8 eyes from 8 patients via GATT). Demographic and baseline data are given in Table 1. The two groups were well matched for demographic characteristics. Mean baseline IOP and the number of IOP-lowering medications were similar between groups (P>0.05).
 |
Table 1 Baseline Demographic And Glaucoma Status Data |
Surgical success (≥20% IOP reduction or ≥1 medication reduction without additional IOP-lowering procedures) was assessed beginning at Week 1 (Table 2) and tended to increase slightly over time, likely resulting from incremental medication withdrawals in at-target eyes. At the 6-month primary endpoint, success was achieved in 81.7% of KDB eyes and 84.6% of Trab360/GATT eyes (P=0.737).
 |
Table 2 Surgical Success Rates (≥20% IOP Reduction Or ≥1 Medication Reduction Without Additional IOP-Lowering Procedures), Mean IOP, And Mean Medication Data For Both Groups At Each Time Point |
Mean IOP data are also given in Table 2 and Figure 1. Across the 5 postoperative time points, mean IOP reductions of 3.3 ± 6.8–2.9 ± 5.4 were seen in KDB eyes and 3.2± 9.4–2.9 ± 6.8 in Trab360/GATT eyes. At Month 6, mean IOP reductions were 2.9 ± 5.4 in KDB eyes and 2.9 ± 6.8 in Trab360/GATT eyes (P=0.417). Also at Month 6, more eyes undergoing KDB than Trab360/GATT achieved target IOP ≤18 mmHg (80.0% [56/70] vs 59.3% [16/27], P=0.040) and ≤15 mmHg (61.4% [43/70] vs 25.9% [7/27], P=0.003) without further IOP-lowering interventions.
 |
Figure 1 IOP for sectoral excisional goniotomy with KDB or Trab360/GATT in the 6-month follow-up period. |
Data on IOP-lowering medication use are also given in Table 2 and Figure 2. Across the 5 postoperative time points, mean medication reductions of 0.5 ± 1.2–1.1 ± 1.3 were seen in KDB eyes and 2.3 ± 1.4–1.4 ± 1.4 in Trab360/GATT eyes. At Month 6, mean medication reductions were 1.1 ± 1.3 in KDB eyes and 1.2 ± 1.1 in Trab360/GATT eyes (P=0.641).
 |
Figure 2 IOP-lowering medications for sectoral excisional goniotomy with KDB or Trab360/GATT in the 6-month follow-up period. |
Safety data are given in Table 3. The most common adverse event was new-onset cystoid macular edema, occurring in 3 (4.1%) KDB eyes and 3 (11.1%) Trab360/GATT eyes. Less common adverse events included layered hyphema (more than 2 weeks postoperatively) and steroid-related IOP elevations. Postoperative blood reflux within 2 weeks was frequently observed in both groups (86.5% [64/74] in the excisional goniotomy eyes and 85.2% [23.27] in the 360° trabeculotomy eyes), none requiring treatment or washout. There were no vision-threatening complications in either group.
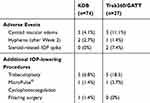 |
Table 3 The Nature And Frequency Of Adverse Events And Additional IOP-Lowering Procedures By Group, N (%) |
Additional IOP-lowering procedures were performed in 9.5% (7/74) of KDB eyes and 22.2% (6/27) of Trab360/GATT eyes (Table 3) due to insufficient IOP lowering or evidence of further glaucoma progression within the 6 months of follow-up. All additional IOP-lowering procedures in both groups occurred after 3 months of surgery. The most common of these was laser trabeculoplasty (either MicroPulse® laser trabeculoplasty [Iridex, Inc, Mountain View, CA] or selective laser trabeculoplasty) in both groups. One patient in the KDB group required a filtering procedure with the gel micro-stent (XEN, Allergan, Inc., Irvine, CA).
Discussion
In this study, both excisional goniotomy with the KDB and 360° trabeculotomy with Trab360 or GATT, in combination with cataract extraction, produced comparable mean reductions in both IOP and the need for IOP-lowering medications through 6 months of postoperative follow-up. Significantly more KDB eyes than Trab360/GATT eyes achieved target IOP of ≤18 mmHg and ≤15 mmHg at the Month 6 time point.
In the current study, both the limited and complete TM procedures lowered IOP by approximately 10–15% while reducing the medication burden by approximately 50%. In prospective and retrospective studies of excisional goniotomy with the KDB performed at the time of cataract surgery, mean IOP reductions of ~25% have been reported with follow-up periods of 6–12 months.8,13,14 We recently reported a series of eyes undergoing KDB-Phaco in which the mean IOP reduction was only 12%; however, these eyes had a mean baseline IOP of only 17.1 mmHg and underwent surgery primarily with the goal of medication reduction.15 Similar results were reported in a series with mean IOP of 17.4 mmHg and IOP reduction of ~14%.16 In these same studies, the IOP-lowering medication burden was reduced by ~50%.8,13–15 GATT has been reported to lower IOP by ~30–45% and IOP medications by ~30–60% at 6 months.10,17 Trab360 has produced IOP and medication reductions of ~30%.9 The smaller IOP reductions but similar medication reductions seen in both groups in the current study versus the published literature suggest that more eyes in our study underwent surgery for medication reduction than for IOP reduction, a hypothesis supported by the relatively low baseline IOP in both groups (~17–18 mmHg).
Given the substantial difference in the extent of TM opened in these two groups (~4 clock hours or 120° by KDB versus 360° by Trab360/GATT), the equal or better performance of KDB excisional goniotomy is not immediately intuitive. One possible explanation is that there is a dose–response threshold effect such that TM incision/excision beyond ~120° provides no additional aqueous humor outflow or IOP reduction. A second possible explanation pertains to the nature of the surgery. Trab360 and GATT are incisional procedures that leave intact anterior and posterior leaflets of the TM, while the KDB performs an excisional goniotomy, removing a strip of TM and leaving a gap between the residual anterior and posterior TM leaflets. In theory, aqueous humor should flow more freely through a patent gap in the TM than through the two adjacent sides of incised TM—in fact, a pressure gradient may be required to overcome a valve effect maintained by the intact and opposed TM leaflets following incisional trabeculotomy.
This study is limited by its retrospective nature. IOP measurements were taken according to the routine clinical protocol (single readings by single operators) rather than a more robust research protocol (multiple readings by a masked operator and unmasked recorder). Medication withdrawal was at the investigator’s discretion rather than via a prespecified approach. Selection bias was limited, however, by selection of all cases meeting the minimal eligibility criteria within the specified time frame.
Conclusion
In summary, both sectoral excisional goniotomy with the KDB and 360° trabeculotomy with Trab360 or GATT procedures lowered both IOP and the need for IOP-lowering medications during the first 6 postoperative months. More eyes undergoing KDB excisional goniotomy than 360° trabeculotomy achieved target IOP ≤18 mmHg and ≤15 mmHg at 6 months. A full 360° TM procedure may not be necessary to achieve maximal efficacy from this class of micro-invasive glaucoma procedures.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Acknowledgments
The authors acknowledge Tony Realini, MD, MPH, for assistance with manuscript preparation, and Amy Folkerts for professional editing and manuscript submission support. The abstract was presented at the American Glaucoma Society Annual Meeting; March 14-17, 2019; San Francisco, CA.
Disclosure
Dr. An served as a consultant for New World Medical, Inc. The authors report no other conflicts of interest in this work.
References
1. Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23:96–104. doi:10.1097/ICU.0b013e32834ff1e7
2. Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi:10.1016/j.ajo.2017.07.023
3. Sheybani A, Dick HB, Ahmed II. Early clinical results of a novel ab interno gel stent for the surgical treatment of open-angle glaucoma. J Glaucoma. 2016;25:e691–6. doi:10.1097/IJG.0000000000000352
4. Batlle JF, Fantes F, Riss I, et al. Three-year follow-up of a novel aqueous humor microshunt. J Glaucoma. 2016;25:e58–e65. doi:10.1097/IJG.0000000000000368
5. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi:10.2147/OPTH.S80490
6. Agrawal P, Bradshaw SE. Systematic literature review of clinical and economic outcomes of micro-invasive glaucoma surgery (Migs) in primary open-angle glaucoma. Ophthalmol Ther. 2018;7:49–73. doi:10.1007/s40123-018-0131-0
7. Bovee CE, Pasquale LR. Evolving surgical interventions in the treatment of glaucoma. Semin Ophthalmol. 2017;32:91–95. doi:10.1080/08820538.2016.1228393
8. Dorairaj SK, Kahook MY, Williamson BK, Seibold LK, ElMallah MK, Singh IP. A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction. Clin Ophthalmol. 2018;12:791–797. doi:10.2147/OPTH.S158403
9. Sarkisian SR, Mathews B, Ding K, Patel A, Nicek Z. 360° ab-interno trabeculotomy in refractory primary open-angle glaucoma. Clin Ophthalmol. 2019;13:161–168. doi:10.2147/OPTH.S189260
10. Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology. 2014;121:855–861. doi:10.1016/j.ophtha.2013.11.001
11. New World Medical, Inc. Kahook Dual Blade. Instructions for Use. Rancho Cucamonga, CA; 2018. Available from: https://www.newworldmedical.com/Clients/NewWorldMedical/Content/NWMCorp/media/pdf/KDB_Product_Brochure_IFU_revE_50-0069.pdf.
12. Sight Sciences, Inc. Trab360 Trabeculotomy Instrument. Menlo Park, CA; 2015. Available from: http://sightsciences.com/shared/download/trab360/TRAB360%20US%20Product%20Brochure.pdf.
13. Dorairaj SK, Seibold LK, Radcliffe NM, et al. 12-month outcomes of goniotomy performed using the Kahook Dual Blade combined with cataract surgery in eyes with medically treated glaucoma. Adv Ther. 2018;35:1460–1469. doi:10.1007/s12325-018-0755-4
14. ElMallah MK, Seibold LK, Kahook MY, et al. 12-month retrospective comparison of Kahook Dual Blade excisional goniotomy with istent trabecular bypass device implantation in glaucomatous eyes at the time of cataract surgery. Adv Ther. 2019;36:2515–2527. doi:10.1007/s12325-019-01025-1
15. Hirabayashi MT, King JT, Lee D, An JA. Outcome of phacoemulsification combined with excisional goniotomy using the kahook dual blade in severe glaucoma patients at 6 months. Clin Ophthalmol. 2019;13:715–721. doi:10.2147/OPTH.S196105
16. Le C, Kazaryan S, Hubbell M, Zurakowski D, Ayyala RS. Surgical outcomes of phacoemulsification followed by istent implantation versus goniotomy with the Kahook Dual Blade in patients with mild primary open-angle glaucoma with a minimum of 12-month follow-up. J Glaucoma. 2019;28:411–414. doi:10.1097/IJG.0000000000001143
17. Rahmatnejad K, Pruzan NL, Amanullah S, et al. Surgical outcomes of gonioscopy-assisted transluminal trabeculotomy (gatt) in patients with open-angle glaucoma. J Glaucoma. 2017;26:1137–1143. doi:10.1097/IJG.0000000000000802
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
