Back to Journals » Infection and Drug Resistance » Volume 12
Antimicrobial susceptibility changes of Escherichia coli and Klebsiella pneumoniae intra-abdominal infection isolate-derived pathogens from Chinese intra-abdominal infections from 2011 to 2015
Authors Zhang H, Tong D, Johnson A, Zhang G, Xu Z, Yang Y, Zhang J, Li D, Duan S, Wang Y , Yang Q, Xu Y
Received 11 April 2019
Accepted for publication 25 July 2019
Published 9 August 2019 Volume 2019:12 Pages 2477—2486
DOI https://doi.org/10.2147/IDR.S211952
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Hui Zhang,1 Dawei Tong,1 Aaron Johnson,2 Ge Zhang,1 Zhipeng Xu,1 Yang Yang,1 Jingjia Zhang,1 Dongxue Li,1 Simeng Duan,1 Yao Wang,1 Qiwen Yang,1 Yingchun Xu1
1Department of Microbiology, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Science, Beijing 100730, People’s Republic of China; 2Department of Microbiology, International Health Management Associates, Schaumburg, IL 60173-3817, USA
Background: To explore the susceptibility trends of antimicrobials and resistance increase to antibiotics of Enterobacteriaceae isolated from patients in China with intra-abdominal infections (IAI) from 2011 to 2015.
Methods: MIC90 and MIC50 values of 12 commonly used antibiotics from Escherichia coli and Klebsiella pneumoniae isolated from IAI samples were determined.
Results: A total of 8,477 Gram-negative bacterial pathogens were collected from 21 medical centers in China. The majority of IAI isolate-derived pathogens were E. coli (3,854, 45.5%) and K. pneumoniae (1,670, 19.7%) of which 1,990 (23.5%) were consecutively collected from community acquired (CA) and 6,186 (73.0%) from hospital acquired (HA) IAIs. The drugs with the highest efficacy against E. coli and K. pneumoniae isolates derived from IAI samples were imipenem, ertapenem, amikacin and piperacillin-tazobactam. MIC90 values for piperacillin-tazobactam were 64 μg/mL in 2015 with fluctuations from 16–64 μg/mL through the years for E. coli, but were stable at ≥64 μg/mL from 2011 to 2015 for K. pneumoniae isolates. Susceptibilities to ertapenem, imipenem and amikacin were high for E. coli isolates throughout the study, but K. pneumoniae isolated from abscesses, colon and peritoneal fluid collected from medical and surgical ICUs showed an increasing trend of carbapenem resistance in 2015.
Conclusion: In 2015 there was a trend of enhanced carbapenem resistance, particularly for K. pneumoniae isolated from IAI samples obtained from patients in ICUs.
Keywords: MIC, Enterobacteriaceae, intra-abdominal infection, carbapenems, cefepime, piperacillin-tazobactam
Introduction
The Study for Monitoring Antimicrobial Resistance Trends (SMART) program was established in 2002 as a worldwide system to establish the susceptibilities to antibiotics of facultative anaerobic and aerobic Gram-negative bacteria in vitro. Various surveillance programs monitoring IAI pathogens have reported that the percentage of extended beta-lactamase (ESBL) producing bacteria have increased during the last decade particularly in Asia,1,2 with the predominant pathogens being K. pneumonia and E. coli. The most recent studies recorded IAI pathogen susceptibilities of these Enterobacteriaceae to amikacin, carbapenems and piperacillin-tazobactam,3–6 but also an increasing resistance to carbapenems.6–9 However, there were differences in the resistance patterns according to the region of China studied,10 and generally resistance was less for community acquired compared to nosocomial infections11,12 while ICUs have been identified as a major source of resistant Enterobacteriaceae infections in hospitals.13–15 In the current investigation, MIC50 and MIC90 values were analyzed in order to determine the resistance trends of K. pneumoniae and E. coli isolated from IAI patients to carbapenems (imipenem and ertapenem), cephalosporins (ceftriaxone, cefepime ceftazidime, cefotaxime and cefoxitin), a broad-spectrum β-lactam antibiotic plus a beta-lactamase inhibitor combination (piperacillin–tazobactam) drug, an aminoglycoside (amikacin) and 2 fluoroquinolones (levofloxacin and ciprofloxacin) between 2011 and 2015 in China.
Samples and methodology
Isolates obtained from IAI patients
The Human Research Ethics Committee of our hospital approved the study protocols (Et. Number: S-K238) and decided that patient consent was not required.
In total, 1,670 K. pneumoniae and 3,854 E. coli isolates were detected in IAI samples, with a total of 8,477 Enterobacteriaceae and non-Enterobacteriaceae present during surgery or in paracentesis specimens from 2011 to 2015 (2011, n=1,908; 2012, n=1,898; 2013, n=1,614; 2014, n=1,574; 2015, n=1,483) from 21 centers across 7 regions of China namely the north, northeast east, central China, Jiang-zhe region, south and southeast, with a range of 77 to 250 samples per year per hospital, which were consecutively collected. The majority of the IAI specimens were collected during surgery, including some paracentesis samples, and were taken from the appendix, gall bladder, small intestine, colon, rectum, pancreas, stomach, liver, peritoneal fluid and abscesses. Isolates were identified using local site procedures and then sent for analysis to the clinical microbiology laboratory of Peking Union Medical College Hospital and for re-identification using MALDITOF MS (Vitek MS, BioMérieux, France).
Any isolates that contained the same species and genus from a particular patient were excluded from the study. Pathogens were identified using the standard methodology adopted in each clinical microbiology laboratory carrying out the tests. Isolates were deemed community-associated (CA) and hospital-associated (HA), if found in a sample taken <48 h or >48 h after an individual was admitted to a hospital.11
Minimum inhibitory concentration determination method
Pathogen susceptibility to antibiotic tests was carried out at the Peking Union Medical College Hospital Center laboratory using customized MicroScan broth microdilution techniques between 2011 and 2014, and with the aid of a Trek Diagnostic System (Thermo Scientific) in 2015. Minimum inhibitory concentrations (MIC)90/MIC50 were determined using interpretations of susceptibility that were based on defined CLSI clinical breakpoints.16 Isolates were exposed to ceftriaxone, cefepime, amikacin, ceftazidime, ertapenem, piperacillin–tazobactam, imipenem and levofloxacin as recommended by appropriate guidelines for the management and diagnosis of complex IAIs.17 These drugs may be administered to hospitalized patients with IAIs caused by Gram-negative K. pneumoniae and E. coli pathogens. In addition, cefotaxime, cefoxitin and ciprofloxacin were included.
According to the Clinical and Laboratory Standards Institute methodology,18 ESBL was confirmed if cefotaxime or ceftazidime MICs were ≥ 2 µg/mL and their MICs decreased ≥8 fold when used in combination with clavulanic acid (4 µg/mL).
For each MIC test batch, reference strains of E. coli American Type Culture Collection (ATCC) 25922 and K. pneumonia (ATCC 700603) were used as quality control strains. The results were analyzed only if the quality control test results fell within acceptable ranges.
Statistical analysis
SPSS ver. 21.0 (SPSS Inc., Chicago, US) was used to carry out all statistical analyses. The susceptibility or resistance rates of all the Gram-negative isolates combined were determined using appropriate breakpoints for each species. The trend was analyzed using a chi-squared trend test for susceptibility and resistance rates. A P-value <0.05 was considered to be a statistically significant difference.
Results
Distribution of all isolates from CA and HA in IAI infected patients
In total, 8,477 isolate-derived pathogens were collected from patients with IAI infections from 2011 to 2015, including non-Enterobacteriaceae and Enterobacteriaceae pathogens. Table 1 shows the basic demographic characteristics of the included patients.
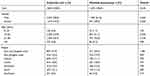 |
Table 1 Demographic characteristics of the included patients |
Most of the isolate-derived pathogens were Enterobacteriaceae including K. pneumoniae and E. coli, which accounted for 19.7% and 45.5% of all IAIs respectively, of which 1,990 (23.5%) were collected from CA and 6,186 (73.0%) from HA IAIs. The distribution trend of E. coli from 2011 to 2015 showed that the HA E. coli infection rates of IAI patients were more than double those of CA IAIs. Similarly, the incidence of HA IAIs caused by K. pneumoniae was more than 3 fold that of CA IAIs throughout the years of the study (Table 2).
 |
Table 2 Distribution of isolates from hospital acquired (HA) and community acquired (CA) intra-abdominal infections |
Distribution of K. pneumoniae and E. coli IAIs in various tissues/organs and different Chinese hospital departments from 2011 to 2015
Next, we analyzed the distribution trends of K. pneumoniae and E. coli from IAI patients in a number of different departments and in various tissues and organs.
For E. coli, the majority of IAI isolate-derived strains were sampled in general surgery departments (60.00–76.00%) and some came, to a lesser extent, from general medical, followed by surgical ICUs and emergency rooms (Figure 1A). The major distribution of E. coli from IAI samples was found mainly in the gall bladder, with an increase from 2011 to 2015, followed by the peritoneal fluid and abscesses, but became less prevalent in abscesses through the years (Figure 1B).
For isolates infected with K. pneumoniae, a similar distribution trend was detected in IAI patients treated in different hospital departments (Figure 2A), but in parallel with a similar predominance of gall bladder and peritoneal fluid infections, K. pneumoniae caused IAIs occurred to a lesser extent than E. coli in the appendix and to a greater degree in liver infections (Figure 2B).
 |
Figure 2 Distribution of K. pneumoniae isolates from IAI patients in (A) different departments, (B) tissues and organs. Abbreviations: IAI, intra-abdominal infection; ICU, intensive care unit. |
Prevalence of ESBL+ K. pneumoniae and E. coli strains in isolates from IAIs between 2011 and 2015
As shown in Figure 3, the distribution of ESBL+ K. pneumoniae and E. coli strains from obtained from HA IAIs was about 10% higher than ESBL+ isolates from CA IAIs between 2011 and 2014. Only CA K. pneumoniae and E. coli IAIs caused by ESBL+ strains were reduced between 2014 and 2015 (Figure 3).
Susceptibility of K. pneumoniae and E. coli collected from IAI samples from different hospital departments to ertapenem and imipenem between 2011 and 2015
The susceptibilities of E. coli isolated from IAIs to ertapenem and imipenem were over 80% in most hospital departments except medical ICUs, which showed lower susceptibility to ertapenem in 2015 compared to the previous 4 years.
Similarly, susceptibilities of K. pneumoniae isolated from IAIs to ertapenem and imipenem were generally >80%, but with higher fluctuations throughout the years. Particularly in ICUs, susceptibilities to ertapenem dropped to <80% between 2011 and 2015, which was also the trend for imipenem (Figure 4).
Susceptibilities of IAI isolate-derived E. coli and K. pneumoniae strains from different tissues/organs to ertapenem and imipenem between 2011 and 2015
Susceptibility overall to E. coli was >80% for both ertapenem and imipenem in all tissues and organs, except for other sample sources in 2015, and for small intestine samples in 2014. However, beside some temporary fluctuations in the former years, particularly during 2015, the susceptibility of IAIs caused by K. pneumoniae fell in ertapenem and imipenem tests for samples obtained from abscesses, colon, peritoneal fluid and other sources (Figure 5).
Comparison of 11 commonly used antimicrobial agent resistances of K. pneumoniae and E. coli IAI isolate-derived pathogens from 2011 to 2015
Next, from 2011 to 2015 we analyzed the susceptibilities of IAI isolate-derived K. pneumoniae and E. coli IAI isolates to 11 commonly prescribed antimicrobial agents (Table 3). In general, E. coli was highly susceptible to amikacin (>90%) with few changes through the years and to the carbepenems, ertapenem and imipenem (both >89.2%), but since 2011, the resistance to carbapenems has shown a gradually increasing trend with higher MIC90 values. MIC90 and antibiotic-resistance values to the antimicrobial agent combination piperacillin/tazobactam also showed high susceptibilities against E. coli, but in 2015 the MIC90, MIC50 concentrations and resistance percentages were somewhat higher than in previous years.
 |
Table 3 Susceptibility of K. pneumoniae and E. coli isolates obtained from intra-abdominal infections patients to 12 commonly prescribed antimicrobials from 2011 to 2015 (units: µg/mL) |
In addition, although in 2015 the drugs with the greatest efficacy against K. pneumoniae isolated from IAI samples were imipenem, ertapenem and amikacin (84.00%, 81.6% and 86.1%, respectively), the resistance of K. pneumoniae isolates gradually increased from 2011 to 2015, with a parallel decline of MIC50 and MIC90 concentrations to these drugs.
Discussion
A global study revealed that IAIs constituted 19.6% of all infections in ICUs and the mortality was higher than those caused by other infections (29.4% vs 24.4%, P <0.001), though most patients were treated with antibiotics (98.1%). However, only for two-thirds of these patients were microbial cultures reported,19 indicating that empirical antimicrobial treatments are commonly applied in clinical practice underlining the importance of local antimicrobial susceptibility data. In the present study, we explored the susceptibility trends of E. coli and K. pneumoniae isolated from IAI patients from 2011 to 2015, which accounted for 46.1% and 22.2%, respectively of all consecutively collected samples, indicating that these Enterobacteriaceae were the predominant pathogens of IAIs, a finding in accordance with previously published literature.20 The majority of K. pneumoniae and E. coli specimens were obtained during general surgery and the sources were mainly from peritoneal fluid, abscesses and the gall bladder, but IAIs caused by K. pneumoniae occurred to a lesser extent in the appendix and to a greater degree in liver infections compared with E. coli. This change has been attributed in the literature to an increased incidence of K. pneumoniae-induced pylephlebitis.21 In general, MIC90 values were often ≥32 μg/mL, particularly for cefepime in K. pneumoniae and E. coli strains isolated from IAIs, although fluctuations were detected mainly for K. pneumoniae. Similar but more pronounced trends were found for piperacillin–tazobactam MIC90s. The ESBL rates dropped in the years after 2013 particularly for K. pneumoniae strains isolated from IAIs, but this trend was not reflected in lower resistance rates to cephalosporins especially during 2015. Since also the resistance rate to cefoxitin, which is used for ESBL producer raised in 2015 other mechanisms like AmpC overexpression and porin loss might have developed.22
There was a trend of an increasing ertapenem MIC90 for E. coli from 0.5 to 1 and from 0.25 to 1 for imipenem between 2013 and 2015, which is in line with a previous study on Asian intra-abdominal and urinary tract infections, with reported imipenem and ertapenem MIC90 values for Enterobacteriaceae of 1 between 2013 and 2015. However, the MIC90 values of ertapenem (>4) and imipenem (8 to >32) for K. pneumoniae isolated from IAIs in our 2014–2015 study were higher than the reported values of 0.25 and 0.5 by Karlowsky and colleagues.4
MIC90 values of imipenem for K. pneumoniae reached ≥32 μg/mL, particularly in abscesses, colon and peritoneal fluid samples in 2015, which were collected from medical, surgical ICUs and general surgery departments. Especially for ICUs, a high incidence of carbapenem resistant K. pneumoniae infections have also been reported in other studies.23,24 However, a general trend of increasing carbapenem resistant K. pneumoniae stains has been described for China in 2014.25
The trend of increasing carbapenem MICs for K. pneumonia is similar to vancomycin MICs for Staphylococcus aureus in recent years, particularly in Asia, a finding attributed to excessive use of vancomycin, which might also be the case for K. pneumoniae strains that were resistant to imipenem26–29 However, the trend of a rising resistance of K. pneumoniae to carbapenem, particularly in ICUs, should be closely monitored, a finding that is in close agreement with previous reports in the literature.30–32
Conclusion
For the treatment of E. coli-induced IAIs, imipenem and ertapenem are still an option although the MIC90 values increased above the sensitivity level of 0.5–1 μg/mL, but they were still not in the resistance ranges of ≥2 and 4 μg/mL. In contrast, K. pneumoniae isolates derived from IAIs became predominantly resistant to ertapenem and imipenem, particularly during 2014 and 2015.
Ethics approval and consent to participate
The protocol has been reviewed by the human research ethics committee of the Institutional Review Board (IRB) of the Peking Union Medical College Hospital and since the project falls under the category observational study and all bacterial strains were from residual samples used in clinical diagnosis or were strains from their subcultures, it has been determined to meet the criteria for exemption. This project does not involve any patient information nor does it affect the normal diagnosis and treatment of patients, and after consultation with the IRB, formal ethical approval was reviewed and waived and written patient consent was not required (Ethics Approval Number: S-K238).
Availability of data and materials
The data that support the findings of this study are directly available from MSD China, but the SMART database is not in the public domain. Data are also available from the authors upon reasonable request and with permission of MSD China.
Acknowledgment
Medical writing assistance and editorial assistance was provided by Shanghai BIOMED Science Technology (Shanghai, China) through funding provided by MSD China. This study was supported by a grant from Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. This study was supported by National Key Research and Development Program of China (2018YFC1200100, 2018YFC1200105), CAMS Initiative for Innovative Medicine (Grant No. 2016-I2M-3-014).
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Aaron Johnson received financial support in the form of salaries from International Health Management Associates, which receives funding from MSD to administer the SMART program and for SMART-related travel and consultation expenses. The authors report no other conflicts of interest in this work.
References
1. Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Hsueh PR, Paterson DL. Emergence of high levels of extended-spectrum-beta-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the Study for Monitoring Antimicrobial Resistance Trends (SMART) program, 2007. Antimicrob Agents Chemother. 2009;53(8):3280–3284. doi:10.1128/AAC.00426-09
2. Baquero F, Hsueh PR, Paterson DL, et al. In vitro susceptibilities of aerobic and facultatively anaerobic gram-negative bacilli isolated from patients with intra-abdominal infections worldwide: 2005 results from Study for Monitoring Antimicrobial Resistance Trends (SMART). Surg Infect (Larchmt). 2009;10(2):99–104. doi:10.1089/sur.2008.0020
3. Toh HS, Chuang YC, Huang CC, et al. Antimicrobial susceptibility profiles of Gram-negative bacilli isolated from patients with hepatobiliary infections in Taiwan: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART), 2006–2010. Int J Antimicrob Agents. 2012;40 Suppl:S18–S23. doi:10.1016/S0924-8579(12)70005-5
4. Karlowsky JA, Hoban DJ, Hackel MA, Lob SH, Sahm DF. Antimicrobial susceptibility of Gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Asia-Pacific countries: SMART 2013–2015. J Med Microbiol. 2017;66(1):61–69. doi:10.1099/jmm.0.000421
5. Lob SH, Badal RE, Bouchillon SK, Hawser SP, Hackel MA, Hoban DJ. Epidemiology and susceptibility of Gram-negative appendicitis pathogens: SMART 2008–2010. Surg Infect (Larchmt). 2013;14(2):203–208. doi:10.1089/sur.2012.034
6. Zhang H, Yang Q, Liao K, et al. Update of incidence and antimicrobial susceptibility trends of Escherichia coli and Klebsiella pneumoniae isolates from Chinese intra-abdominal infection patients. BMC Infect Dis. 2017;17(1):776. doi:10.1186/s12879-017-2757-2
7. Jean SS, Hsueh PR, Group SA-P. Distribution of ESBLs, AmpC beta-lactamases and carbapenemases among Enterobacteriaceae isolates causing intra-abdominal and urinary tract infections in the Asia-Pacific region during 2008–14: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART). J Antimicrob Chemother. 2017;72(1):166–171. doi:10.1093/jac/dkw398
8. Hsueh PR, Badal RE, Hawser SP, et al. Epidemiology and antimicrobial susceptibility profiles of aerobic and facultative Gram-negative bacilli isolated from patients with intra-abdominal infections in the Asia-Pacific region: 2008 results from SMART (Study for Monitoring Antimicrobial Resistance Trends). Int J Antimicrob Agents. 2010;36(5):408–414. doi:10.1016/j.ijantimicag.2010.07.002
9. Chen YH, Hsueh PR, Badal RE, et al. Antimicrobial susceptibility profiles of aerobic and facultative Gram-negative bacilli isolated from patients with intra-abdominal infections in the Asia-Pacific region according to currently established susceptibility interpretive criteria. J Infect. 2011;62(4):280–291. doi:10.1016/j.jinf.2011.02.009
10. Zhang H, Yang Q, Liao K, et al. Antimicrobial susceptibilities of aerobic and facultative gram-negative bacilli from intra-abdominal infections in patients from seven regions in China in 2012 and 2013. Antimicrob Agents Chemother. 2015;60(1):245–251. doi:10.1128/AAC.00956-15
11. Zhang S, Huang W. Epidemiological study of community- and hospital-acquired intraabdominal infections. Chin J Traumatol. 2015;18(2):84–89. doi:10.1016/j.cjtee.2015.07.003
12. Montravers P, Lepape A, Dubreuil L, et al. Clinical and microbiological profiles of community-acquired and nosocomial intra-abdominal infections: results of the French prospective, observational EBIIA study. J Antimicrob Chemother. 2009;63(4):785–794. doi:10.1093/jac/dkp005
13. Perez F, Endimiani A, Ray AJ, et al. Carbapenem-resistant Acinetobacter baumannii and Klebsiella pneumoniae across a hospital system: impact of post-acute care facilities on dissemination. J Antimicrob Chemother. 2010;65(8):1807–1818. doi:10.1093/jac/dkq191
14. Routsi C, Pratikaki M, Platsouka E, et al. Risk factors for carbapenem-resistant Gram-negative bacteremia in intensive care unit patients. Intensive Care Med. 2013;39(7):1253–1261. doi:10.1007/s00134-013-2914-z
15. Zurawski RM. Carbapenem-resistant enterobacteriaceae: occult threat in the intensive care unit. Crit Care Nurse. 2014;34(5):44–52. doi:10.4037/ccn2014602
16. CLSI. Clinical and Laboratory Standards Institute (CLSI) M100-S25. Performance Standards of Antimicrobial Susceptibility Testing. Twenty-fifth Informational Supplement. Wyane (PA): CLSI; 2015.
17. Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(2):133–164. doi:10.1086/649554
18. CLSI. Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, 10th Ed, Approved Standard M07-A10. Wayne (PA); 2015.
19. De Waele J, Lipman J, Sakr Y, et al. Abdominal infections in the intensive care unit: characteristics, treatment and determinants of outcome. BMC Infect Dis. 2014;14:420. doi:10.1186/1471-2334-14-420
20. Sartelli M, Catena F, Ansaloni L, et al. Complicated intra-abdominal infections worldwide: the definitive data of the CIAOW Study. World J Emerg Surg. 2014;9:37. doi:10.1186/1749-7922-9-37
21. Wang YF, Chang CC, Lee TC, et al. Recent trend of pylephlebitis in Taiwan: Klebsiella pneumoniae liver abscess as an emerging etiology. Infection. 2013;41(6):1137–1143. doi:10.1007/s15010-013-0497-9
22. Shi W, Li K, Ji Y, et al. Carbapenem and cefoxitin resistance of Klebsiella pneumoniae strains associated with porin OmpK36 loss and DHA-1 beta-lactamase production. Braz J Microbiol. 2013;44(2):435–442. doi:10.1590/S1517-83822013000200015
23. Saidel-Odes L, Borer A. Limiting and controlling carbapenem-resistant Klebsiella pneumoniae. Infect Drug Resist. 2013;7:9–14. doi:10.2147/IDR.S44358
24. Wang Z, Qin RR, Huang L, Sun LY. Risk Factors for Carbapenem-resistant Klebsiella pneumoniae Infection and Mortality of Klebsiella pneumoniae Infection. Chin Med J (Engl). 2018;131(1):56–62. doi:10.4103/0366-6999.221267
25. Hu FP, Guo Y, Zhu DM, et al. Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005–2014. Clin Microbiol Infect. 2016;22 Suppl 1:S9–S14. doi:10.1016/j.cmi.2016.01.001
26. Chang W, Ma X, Gao P, Lv X, Lu H, Chen F. Vancomycin MIC creep in methicillin-resistant Staphylococcus aureus (MRSA) isolates from 2006 to 2010 in a hospital in China. Indian J Med Microbiol. 2015;33(2):262–266. doi:10.4103/0255-0857.148837
27. Jensen US, Skjot-Rasmussen L, Olsen SS, Frimodt-Moller N, Hammerum AM, Group DS. Consequences of increased antibacterial consumption and change in pattern of antibacterial use in Danish hospitals. J Antimicrob Chemother. 2009;63(4):812–815. doi:10.1093/jac/dkp043
28. Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014;5(6):229–241. doi:10.1177/2042098614554919
29. Zhang S, Sun X, Chang W, Dai Y, Ma X. Systematic review and meta-analysis of the epidemiology of vancomycin-intermediate and heterogeneous vancomycin-intermediate staphylococcus aureus isolates. PLoS One. 2015;10(8):e0136082. doi:10.1371/journal.pone.0136082
30. Labarca J, Poirel L, Ozdamar M, Turkoglu S, Hakko E, Nordmann P. KPC-producing Klebsiella pneumoniae, finally targeting Turkey. New Microbes New Infect. 2014;2(2):50–51. doi:10.1002/nmi2.42
31. Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012;25(4):682–707. doi:10.1128/CMR.05035-11
32. Tangden T, Giske CG. Global dissemination of extensively drug-resistant carbapenemase-producing Enterobacteriaceae: clinical perspectives on detection, treatment and infection control. J Intern Med. 2015;277(5):501–512. doi:10.1111/joim.12342
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




