Back to Journals » Infection and Drug Resistance » Volume 11
Microbial spectrum and drug-resistance profile of isolates causing bloodstream infections in febrile cancer patients at a referral hospital in Addis Ababa, Ethiopia
Authors Arega B , Woldeamanuel Y , Adane K, Sherif AA , Asrat D
Received 23 March 2018
Accepted for publication 16 June 2018
Published 18 September 2018 Volume 2018:11 Pages 1511—1519
DOI https://doi.org/10.2147/IDR.S168867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Balew Arega,1,2 Yimtubezinash Woldeamanuel,2 Kelemework Adane,3 Abdulaziz A Sherif,4 Daniel Asrat2
1College of Health Sciences, Debre Markos University, Debre Markos, 2Department of Microbiology, Immunology, and Parasitology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, 3Department of Microbiology and Immunology, College of Health Sciences, Mekelle University, Mekelle, 4Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Background: The spectrum of pathogens causing bloodstream infections (BSIs) in cancer patients has shown significant fluctuations in different geographical areas and time. We studied the microbial spectrum and drug-resistance profile of pathogens causing BSIs in febrile cancer patients at a referral hospital in Ethiopia.
Methods: This cross-sectional study was conducted between December 2011 and June 2012 at Tikur Anbessa Hospital in Addis Ababa. Blood cultures from febrile cancer patients (n=107) were performed. Bacterial and fungal pathogens were identified and antimicrobial susceptibility testing done for the bacterial isolates using the Kirby–Bauer disk diffusion method.
Results: A total of 82 pathogens were isolated from 112 blood culture tests of the 76 patients: 71 (86.6%) of the isolates were bacteria and 11 (13.4%) were fungi. The majority (60.5% [43 of 71]) of the isolates were Gram-positive bacteria, where Staphylococcus aureus was predominant (72% [31 of 43]), and 68% of S. aureus isolates were resistant to ceftriaxone and oxacillin. Gram-negative bacteria accounted for 39.5% (28 of 71) of the isolates. Stenotrophomonas maltophilia (17.9% [five of 28]) was the most frequent Gram-negative isolate. In Gram-negative bacteria, the highest rates of resistance were observed in amoxicillin–clavulanic acid (80% [12 of 15]), followed by ceftriaxone (73.3%) and trimethoprim–sulfamethoxazole (73.3%). Multidrug resistance (resistance to three or more types of antibiotics, in this case to ceftriaxone, tetracycline, and trimethoprim-sulfamethoxazole) was observed in 26.3% (13 of 43) of Gram-positive and 40% (six of 16) of Gram-negative bacteria. Neutropenia was an independent risk factor for BSIs (P=0.02).
Conclusion: Gram-positive bacteria were the predominant etiologic agents of BSIs in Ethiopian patients with cancer. Both Gram-positive and Gram-negative bacteria showed an increasing level of resistance for most of the antibiotics used for empiric therapy. Routine bacterial surveillance and study of their resistance patterns must be an essential component of cancer-related infection control and care in our setting.
Keywords: bloodstream infections, cancer patients, bacteria, drug resistance
Background
Cancer patients, particularly those with hematological malignancies, are disproportionately at high risk of developing bloodstream infections (BSIs), with a risk of infection about ten times that of noncancer patients.1 BSIs are common causes of in-hospital morbidity and mortality in such patients.2 In addition, pathogens causing BSIs are increasingly becoming drug resistant making the problem much worse, especially in countries with limited resources.3,4
Bacteria are the primary causative agents of BSIs, with significant fluctuations in the spectrum of the isolates over time.5,6 Gram-negative bacteria were the predominant causative agents of BSIs in the 1960s, but this later changed toward Gram-positive bacteria.7,8 However, there are still some studies in support of the Gram-negative predominance, especially in developing countries. In addition, due to increasing numbers of immunocompromised hosts, fungal pathogens, such as yeasts9 (mainly Candida spp.) and molds (mainly Aspergillus spp.) have been indicated as the main causes of invasive fungal infection (IFI) in cancer patients.10,11 Frequent hospitalization, exposure to invasive procedures, use of broad-spectrum antibiotics, and chemotherapy have been indicated as the most important risk factors for infections in cancer patients.12,13 Chemotherapy renders cancer patients neutropenic, making them more susceptible to potentially life-threatening BSIs.14,15 The treatment of infections in patients with cancer often relies on the use of established guidelines with consideration of the local microbiology and antibiotic-sensitivity patterns of possible etiologic agents.16 This is because the spectrum and drug-resistance profile of pathogens causing BSIs in such patients have shown significant fluctuations in different geographical areas and time points.5,17 Unlike this fact, in our study setting, almost all cancer patients with febrile episodes start empirical antibacterial therapy, and possible regimen change is done based on the clinical response of patients. Apart from our previous report on rare (uncommon) bacterial infections in the same setting,18 to our knowledge there has been no comprehensive study to investigate the microbial spectrum and drug-resistance profile of pathogens causing BSIs in cancer patients from Ethiopia. This study determined the microbial spectrum and drug-resistance profile of pathogens causing BSIs in febrile cancer patients at a referral hospital in Ethiopia.
Methods
Study setting, design, and population
This institution-based cross-sectional study was done at Tikur Anbessa Hospital in Addis Ababa, the only cancer-referral and -treatment center ever to function fully in Ethiopia. Data were collected between December 2011 and June 2012. All febrile cancer patients visiting the hospital’s outpatient departments and those admitted to the Internal Medicine ward and Oncology Radiotherapy Center were investigated for inclusion. Adult febrile cancer patients (>18 years old) who had not started antibiotics and providing informed consent (written) were included in the study. Samples were collected from 107 patients at first episodes of fever, both from neutropenic and nonneutropenic patients.
Specimen collection
Two sets (10 mL each) of venous blood were collected aseptically within 24 hours from each patient. Samples drawn were then poured into blood culture bottles and incubated aerobically at 37°C. Daily inspection of culture bottles was done for up to 7 days. A structured questionnaire was also used to collect data on the sociodemographic and clinical characteristics of the patients, including age, sex, type of cancer, neutrophil counts, cancer therapy, and history of antibiotic therapy.
Blood culture and identification
Gram staining was performed from the blood culture broths that showed visible growth. Evidence for growth was considered based on the appearance of colonies growing on top of red cells, turbidity, gas bubbles, or hemolysis. In addition, blind subculturing was done if a visible growth was not detected within 24 hours. Terminal subculturing was done for bottles that did not show visible growth within 7 days. Based on clues from Gram-staining results, we subcultured organisms on chocolate agar, blood agar, MacConkey agar, and Sabouraud dextrose agar (SDA). Two sets of SDA were inoculated for each sample, one incubated at 37°C and the other at room temperature. We incubated bacterial cultures aerobically at 37°C for up to 24–48 hours and the SDA for 2 weeks.
Gram-positive bacteria were identified using coagulase and catalase tests. Enterobacteriaceae isolates and nonfermentative Gram-negative bacilli were identified using analytical profile index (API20E) and API-NE identification kits (BioMérieux, Lyon, France), respectively. For initial identification of Candida albicans, the germ-tube test was used. The thermotolerance test was employed to differentiate C. albicans from C. dubliniensis. Identification of non-C. albicans at a species level was not possible, due to limitations of diagnostics in our setting.
Antimicrobial susceptibility testing
For antimicrobial susceptibility testing, the disk diffusion method was used. Following the standard operating procedures, we mixed three to five bacterial colonies with 5 mL saline to prepare a suspension equivalent to a 0.5 McFarland standard. By using a sterile swab, the entire surface of the Mueller–Hinton agar was inoculated with bacterial suspensions. After the Mueller–Hinton agar had been dried for 3–5 minutes at room temperature, nine antibiotic disks (Oxoid) were dispensed on the surface of each plate. Amoxicillin–clavulanate (30 µg), chloramphenicol (30 µg), tetracycline (30 µg), sulfamethoxazole–trimethoprim (25 µg), ceftriaxone (30 µg), and ampicillin (10 µg) were used for both Gram-positive and Gram-negative bacterial isolates. Nalidixic acid (30 µg), gentamicin (10 µg), and ciprofloxacin (5 µg) were used only for Gram-negative isolates, whereas oxacillin (5 µg), and penicillin G (10 units) were used only for Gram-positive bacteria. The inoculated plates were incubated for 24–48 hours at 37°C. Isolates were classified as sensitive, intermediate, and resistant based on diameters of zones of inhibition measured by a caliper. The standardized table supplied by the Clinical Laboratory Standard Institute was used for estimation of zone of inhibition. We used Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922), and Pseudomonas aeruginosa (ATCC 27853) as reference strains for quality control of culture and antimicrobial susceptibility testing. The identification of true coagulase-negative Staphylococcus (CoNS) was considered when there was growth in the two bottle sites.
Data analysis
After data entry had been completed using EpiData Entry version 3.1 software, it was transferred to SPSS version 16 for analysis. Risk factors for BSIs (culture-positive) were assessed in comparison with culture-negative (used as a control). Variables with P-values of <0.25 in the bivariate analysis were included in the multivariate logistic regression to determine the association of potential factors with BSIs. P≤0.05 was considered statistically significant.
Ethical issues
The study was approved by the Addis Ababa University College of Health Science Ethical Review Committee. Written informed consent was obtained from all study participants or their caregivers if the patients were too ill to provide consent. Participation in the study was voluntary. The patients’ culture and susceptibility testing results were immediately reported to physicians for treatment and management guidance.
Results
Patient profiles
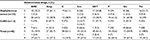
A total of 107 adult febrile cancer patients were included in the study: 55 (51.4%) females and 52 (48.6%) males. The mean age of study participants was 35.5 years. More than half (56 [52.3%]) the participants were neutropenic and 81 (75.7%) suffered from leukemia. All the patients who took cancer therapy 76 (71%) received only chemotherapy. The majority (95% [72 of 76]) of patients were in the first cycle of chemotherapy, and 57% (61 of 107) had taken antibiotics previously. Of these, the majority (64% [39 of 61]) received ceftriaxone only, 13% (11 of 61) received both ceftriaxone and vancomycin, and the rest (13% [11 of 61]) were given ceftriaxone, vancomycin, and ciprofloxacin, while 75% (81 of 107) had total parenteral nutrition during our investigation. However, none of them had either central intravenous or indwelling intravenous devices. Table 1 shows detailed clinical characteristics of the study participants.
Microbial spectrum of BSI
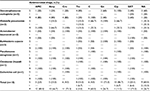
The microbial spectrum of the BSIs is shown in Table 2. Of the study participants, 76 of 107 (71%) were culture-positive for bacteremia and/or fungemia. Overall, 112 blood cultures were performed and 82 pathogenic bacteria and/or fungi identified: 71 (87.6%) isolates were bacteria and 10 (12.3%) were fungi. Blood cultures were positive in 56 (73.7%) leukemia, 15 (19.8%) lymphoma, and five (6.5%) solid-tumor patients. Fifty (66.0%) of the culture-positive cases were neutropenic. The majority (60.5% [43 of 71]) of bacterial isolates were Gram-positive organisms, S. aureus being the predominant pathogen (72% [31 of 43]). The remaining Gram-positive pathogens (39.5%) were CoNS. Of 43 Gram-positive bacteria isolated, 65% (28 of 43) were from neutropenic patients (P=0.03).
  | Table 2 Distribution of bacterial and fungal pathogens causing bloodstream infections (n=107) |
Gram-negative bacteria accounted for 39.5% (28 of 71) of isolates in which nonfermenting Gram-negative bacilli (NF-GNBs) predominated (60.7% [17 of 28]). Stenotrophomonas maltophilia (17.9% [five of 28]) was the most frequent Gram-negative pathogen, followed by Klebsiella pneumoniae (7.1% [three of 28]). Of 28 Gram-negative bacteria, 75% (21 of 28) were isolated from neutropenic patients (P=0.005). Eleven (13.5%) of the isolates were fungi. C. albicans accounted for 63.6% (seven of eleven) of the pathogenic fungi isolated (Table 2). Ten (13.2%) of the 76 patients had polymicrobial infections: seven (70%) with bacterium–bacterium and three (3%) bacterium–fungus coinfections. Seven (70%) of the coinfections were due to S. aureus and NF-GNBs, two (20%) were due to S. aureus and C. albicans, and one (10%) was due to K. pneumoniae and C. albicans.
Risk factors for BSIs
Table 3 shows relationships between BSIs and participants’ clinical and sociodemographic characteristics. Neutropenia was found to be an independent risk factor for BSIs in a multivariate analysis (P<0.001). Being male was also significantly associated with BSIs (crude OR 2.8, 95% CI 0.69–6.5; P=0.042), but only in the bivariate analysis.
  | Table 3 Risk factors associated with blood culture proven bloodstream infections Notes: aWithin previous 3 months for ≥7 days. Abbreviation: COR, crude OR. |
Antibiotic susceptibility of bacterial isolates
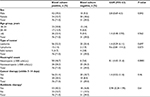
Antibiotic-resistance patterns of Gram-positive bacteria (n=43) against the eight antimicrobial agents is shown in Table 4. Overall, the highest rates of resistance were observed for ceftriaxone (67.4% [29 of 43]), oxacillin (67.4% [28 of 43]), and amoxicillin–clavulanic acid (62.7% [26 of 43]). S. aureus showed the highest rates of resistance for these three antibiotics as well. The lowest level of resistance was observed in sulfamethoxazole–trimethoprim (30.2% [13 of 43]).
Table 5 shows results for those Gram-negative bacteria for which susceptibility testing was available (n=15). We did not perform susceptibility testing for Sphignomonas spp., as confirmatory methods are not yet available for this bacterium. In Gram-negative bacteria, the highest rates of resistance were observed for amoxicillin–clavulanic acid (80% [12 of 15]), followed by ceftriaxone (73.3%) and sulfamethoxazole–trimethoprim (73.3%). Ciprofloxacin was the most effective antibiotic for Gram-negative pathogens, with 86.6% sensitivity. All five isolates of S. maltophilia were 100% resistant to chloramphenicol. All K. pneumoniae (fermenting rod) isolates were also 100% resistant to chloramphenicol and ceftriaxone. Resistance for more than three (tetracycline, sulfamethoxazole–trimethoprim, and ceftriaxone) types of antibiotic (multidrug resistance) was observed in 26.3% (13 of 43) of the Gram-positive and 40% (six of 16) of the Gram-negative bacteria.
Discussion
Except for a single report on rare bacterial pathogens by the same authors,18 to our knowledge, this study is the first comprehensively to address microbial spectrum and drug-susceptibility patterns of pathogens causing BSIs in cancer patients from Ethiopia. Gram-positive bacteria (60%) were found to be the predominant pathogens causing BSIs among febrile cancer patients in our study setting. Similar research from developed countries has shown Gram-positive predominance (54%, Gram-positive vs 45% Gram-negative), but large variability among hospitals and countries has been noted.19 In this regard, recent studies from the USA (72.8%)20 and Turkey (74%)21 showed that Gram-negative bacteria were predominant, while a report from UK22 revealed the contrary.
On the other hand, similar reports from most developing countries still reveal the Gram-negative predominance.23–25 The relatively lower use of indwelling medical devices, as well as low utilization of prophylactic antibiotic regimens in cancer patients, have been indicated as factors in the dominance of Gram-negative bacteria in these countries.4,26 Although these conditions hold true in our setting, the predominance of Gram-positive bacteria in our case might be due to several factors. First, more than half (57%) of the underlying cases in our study were with acute leukemia for which intensive chemotherapy was given and 33% of cases were older than 44 years. These two factors had already been identified as risk factors for severe mucositis,27 which facilitates entry of oral normal flora to the blood. Moreover, unlike the current study, some studies from developing countries have included samples other than blood, such as urine and stool, which might have increased the proportion of isolated Gram-negative bacteria.28
S. aureus (43.6%) was the most frequently identified pathogen in this study, and this finding is similar to those reported from Sudan (72.7%),29 North America (18%),30 and Japan (35%).31 However, the latest studies from the UK22 and Ghana14 and others from southeast Iran (12.3%),32 South Africa (24.3%),33 and Malaysia (23%)34 showed that CoNS was the predominant Gram-positive pathogen. The relatively lower prevalence of CoNS (16.9%) in our study might have been due to the low proportion of catheterized patients.
Furthermore, S. aureus showed the highest rates of drug resistance. About 68% and 64.5% of S. aureus isolates were resistant to ceftriaxone and oxacillin, respectively. This finding is comparable to similar reports from Egypt,35 Taiwan,36 and Pakistan.4 However, other studies have reported a lower resistance proportion for ceftriaxone.30,37,38 This high resistance rate in our study could have been due to the fact that these antibiotics have already been in use for empirical therapy of patients with cancer in our setting. The higher resistance rate for ceftriaxone is an important issue, as this antibiotic has been commonly used to treat critically ill patients in our country.39
In similar studies conducted previously, the most predominant Gram-negative bacteria isolated from BSIs in patients with cancer were those in the Enterobacteriaceae family including E. coil, K. pneumoniae, and/or P. aeruginosa.4,20,21,40 In our study, NF-GNBs were the most frequent (61%) Gram-negative isolates. S. maltophilia (17.9%) was predominant in this group. This finding is in agreement with a previous report by the SENTRY surveillance program.41 The shift to NF-GNBs (mainly S. maltophilia) in our study might have been due to the selective pressure imposed by overuse of broad-spectrum β-lactams in our setting.42 In the current study, 57% of patients had received broad-spectrum β-lactams, and all S. maltophilia was isolated from such patients. In addition, the bacteria’s capability to adhere easily to invasive medical devices and colonize fluids and irrigation solutions used in hospitals could have increased the risk of infections with these bacteria in our setting.43 This increased proportion of NF-GNBs observed in our study is an important concern. Research has shown that most NF-GNBs are often intrinsically resistant to commonly used antimicrobial agents.41 In our study, all five S. maltophilia isolates were 100% resistant to chloramphenicol, and the majority (80%) were resistant to ampicillin and ceftriaxone.
The overall proportion of IFIs in our study (13.5%) is comparable with recent studies from the USA (14%),20 Brazil (12.8%),42 and Japan (13%).31 Yeasts (mainly Candida spp.) were the main cause of IFIs (63.6%), which is in agreement with studies in other areas.10,11 Only 18.2% of candidemia was due to non-C. albicans spp., which is contrary to many studies from developed countries that showed an apparent increase in the proportion of non-C. albicans spp. Increased use of azoles has been reported as a factor in the increasing trend of non-C. albicans spp.10,44 In the current study, none of the participants had used an antifungal agent, and this could have been the reason for the lower proportion of non-C. albicans spp. The predominance of C. albicans candidemia in our setting would however have practical importance, as it can be differentiated easily by a germ-tube test. Moreover, we also isolated an unusual opportunistic yeast pathogen (Rhodotorula) from a 21-year-old male neutropenic patient with acute myeloid leukemia. Tuon and Costa documented this pathogen as a cause of fungemia in immunocompromised patients.45 In general, with an increasing population of immunocompromised, absence of sufficient choice of antifungal agents, and poor diagnostic facilities, such fungal isolates would become a challenge for our setup.
A substantial proportion of cases in the current study (13.2%) suffered from polymicrobial infections. Similarly, in a recent study from Barcelona, 10.2% BSIs in cancer patients were due to polymicrobial infections.46 To make matters worse, about 40% of Gram-negative bacteria in the current study were multidrug resistance. This is comparable to that observed in Pakistan.4 This high rate of polymicrobial infections and multidrug resistance is an important public health concern that needs to be addressed. Studies have shown that these infections have higher morbidity and mortality rates.32,40 Polymicrobial infections are difficult to treat, and the patient will develop compilations.40 The implication of multidrug resistance is much worse. If patients do not respond to commonly used antibiotics, their ultimate fate will be severe complications and death.47 Therefore, appropriate use of antibiotics should be ensured in our setting. Treatment of the patient should be based on actual information regarding the etiologic agent and antimicrobial testing. Ciprofloxacin was found to have a low resistance rate in this study, and hence could be a good choice for empirical treatment in our setting.
Many factors influence the prevalence, severity, and general patterns of microbial etiology of BSIs among cancer patients. Being neutropenic is an independent risk factor for BSIs.48,49 Neutrophils are the prime cells against invading microorganisms, expressly bacterial pathogens. A decrease in their number (neutropenia) is the most serious hematological toxicity, which is often observed in patients with cancer receiving chemotherapy.50 Being male was also associated with BSIs in the bivariate analysis. Other research has also reported similar relationships.1 The reason for this difference remains controversial, but possible factors, such as increased infective endocarditis in males,51 higher likelihood of males to receive aggressive care, and differences in hormonal influence, have been postulated as possible reasons.1,51 Our study was not without limitations. Anaerobic microorganisms were not isolated, as we only used aerobic culture techniques. Since this study used blood samples only, the range of bacterial pathogens to be isolated was limited.
Conclusion
Gram-positive bacteria were found to be the predominant pathogens isolated from BSIs in Ethiopian febrile cancer patients. Fungemia due to C. albicans was a common fungal BSI in our study setting. Neutropenia was significantly associated with BSIs. Both Gram-positive and Gram-negative bacteria showed an increasing level of resistance for most antibiotics that have been used for empirical therapy. Therefore, routine determination of the microbial and drug-resistance spectrum of pathogens should be an essential component of cancer-related infection control and care in our setting.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors are grateful to all staff members of the Internal Medicine and Oncology Radiotherapy Center of Tikur Anbesa Hospital for their kind collaboration during the data collection. We would also like to thank the School of Graduate Studies of Addis Ababa University for the financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
Danai PA, Moss M, Mannino DM, Martin GS. The epidemiology of sepsis in patients with malignancy. Chest. 2006;129(6):1432–1440. | ||
Velasco E, Byington R, Martins CS, Schirmer M, Dias LC, Gonçalves VM. Bloodstream infection surveillance in a cancer centre: a prospective look at clinical microbiology aspects. Clin Microbiol Infect. 2004;10(6):542–549. | ||
Hughes WT, Armstrong D, Bodey GP, et al. 2002Guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002;34(6):730–751. | ||
Butt T, Afzal RK, Ahmad RN, Salman M, Mahmood A, Anwar M. Bloodstream infections in febrile neutropenic patients: bacterial spectrum and antimicrobial susceptibility pattern. J Ayub Med Coll Abbottabad. 2004;16(1):18–22. | ||
Ramphal R. Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis. 2004;39(Suppl 1):S25–S31. | ||
Rolston KV, Bodey GP. Bacterial infections in cancer patients. In: Lyman GH, Crawford J, editors. Cancer Supportive Care: Advances in Therapeutic Strategies. New York: Informa Healthcare; 2008:73–88. | ||
Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on Gram-positive and resistant bacteria. Clin Infect Dis. 1999;29(3):490–494. | ||
Oppenheim BA. The changing pattern of infection in neutropenia patients. J Antimicrob Chemother. 1998;41(Suppl 4):7–11. | ||
Silva V, Díaz MC, Febré N. Invasive fungal infections in Chile: a multicenter study of fungal prevalence and susceptibility during a 1-year period. Med Mycol. 2004;42(4):333–339. | ||
Horn DL, Morrison DC, Opal SM, Silverstein R, Visvanathan K, Zabriskie JB. What are the microbial components implicated in the pathogenesis of sepsis? Report on a symposium. Clin Infect Dis. 2000;31(4):851–858. | ||
Pasqualotto AC, Rosa DD, Medeiros LR, Severo LC. Candidaemia and cancer: patients are not all the same. BMC Infect Dis. 2006;6:1. | ||
Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol. 2002;20(15):3276–3281. | ||
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med. 1998;244(5):379–386. | ||
Crawford J, Dale DC, Lyman GH. Chemotherapy-induced neutropenia. Cancer. 2004;100(2):228–237. | ||
Cebon J, Layton JE, Maher D, Morstyn G. Endogenous haemopoietic growth factors in neutropenia and infection. Br J Haematol. 1994;86(2):265–274. | ||
Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56–e93. | ||
Montassier E, Batard E, Gastinne T, Potel G, de la Cochetière MF. Recent changes in bacteremia in patients with cancer: a systematic review of epidemiology and antibiotic resistance. Eur J Clin Microbiol Infect Dis. 2013;32(7):841–850. | ||
Arega B, Wolde-Amanuel Y, Adane K, Belay E, Abubeker A, Asrat D. Rare bacterial isolates causing bloodstream infections in Ethiopian patients with cancer. Infect Agent Cancer. 2017;12:40. | ||
Mikulska M, Viscoli C, Orasch C, et al. Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Infect. 2014;68(4):321–331. | ||
Islas-Muñoz B, Volkow-Fernández P, Ibanes-Gutiérrez C, Villamar-Ramírez A, Vilar-Compte D, Cornejo-Juárez P. Bloodstream infections in cancer patients: risk factors associated with mortality. Int J Infect Dis. 2018;71:59–64. | ||
Gedik H. Antibiotic resistance status and its costs in hematological patients: a two-year analysis. Caspian J Intern Med. 2017;8(4):276–281. | ||
Raja NS, Gupta S, O’Neill B. Bacterial spectrum and antimicrobial-resistance pattern of bloodstream infections in neutropenic and non-neutropenic adult cancer patients. J Patient Saf Infect Control. 2017;5(2):83–88. | ||
Obeng-Nkrumah N, Labi AK, Acquah ME, Donkor ES. Bloodstream infections in patients with malignancies: implications for antibiotic treatment in a Ghanaian tertiary setting. BMC Res Notes. 2015;8:742. | ||
Mangaraj J, Barkataki D. Microbiological profile of blood stream infection in neutropenic patient in a tertiary care centre. Int J Curr Microbiol App Sci. 2017;6(3):1137–1145. | ||
Mangaraj O, Barkataki D, Mohan DG. Gram negative bacilli causing blood stream infection in febrile neutropenic patients in a tertiary care centre. Int J Contemp Med Res. 2017;4(7):1599–1603. | ||
Kurtaran B, Candevir A, Tasova Y, et al. Hospital-acquired blood-stream infections in cancer patients between 2005 and 2007 in a Turkish university hospital. Arch Clin Microbiol. 2010;1(2):4. | ||
O’Brien SN, Blijlevens NM, Mahfouz TH, Anaissie EJ. Infections in patients with hematological cancer: recent developments. Hematology Am Soc Hematol Educ Program. 2003;2003(1):438–472. | ||
Rolston KV. Bacterial infection in neutropenic cancer patients: an overview. Iran J Clin Infect Dis. 2009;4(2):115–122. | ||
Elseed Y, Ibrahim M, Ahmed WA. Isolation and identification of aerobic bacterial pathogens from septicaemic cancer patients in Khartoum, Sudan. Clin Med J. 2015;1(4):122–125. | ||
Mutnick AH, Kirby JT, Jones RN. Cancer Resistance Surveillance Program: initial results from hematology–oncology centers in North America. Ann Pharmacother. 2003;37(1):47–56. | ||
Kanamaru A, Tatsumi Y. Microbiological data for patients with febrile neutropenia. Clin Infect Dis. 2004;39(Suppl 1):S7–S10. | ||
Nejad ZE, Ghafouri E, Farahmandi-Nia Z, Kalantari B, Saffari F. Isolation, identification, and profile of antibiotic resistance of bacteria in patients with cancer. Iran J Med Sci. 2015;35(2):109–115. | ||
Louw VJ, van der Westhuizen J, Rautenbach W, van der Berg E, Wamelink M, Joubert G. The antibiotic susceptibility of bacteria isolated from blood cultures during episodes of neutropenic fever in patients with myeloid leukaemia. South Afr J Epidemiol Infect. 2010;25(2):9–11. | ||
Baskaran ND, Gan GG, Adeeba K, Sam IC. Bacteremia in patients with febrile neutropenia after chemotherapy at a university medical center in Malaysia. Int J Infect Dis. 2007;11(6):513–517. | ||
Ashour HM, el-Sharif A. Microbial spectrum and antibiotic susceptibility profile of gram-positive aerobic bacteria isolated from cancer patients. J Clin Oncol. 2007;25(36):5763–5769. | ||
Chen CY, Tang JL, Hsueh PR, et al. Trends and antimicrobial resistance of pathogens causing bloodstream infections among febrile neutropenic adults with hematological malignancy. J Formos Med Assoc. 2004;103(7):526–532. | ||
Zahid KF, Hafeez H, Afzal A. Bacterial spectrum and susceptibility patterns of pathogens in adult febrile neutropenic patients: a comparison between two time periods. J Ayub Med Coll Abbottabad. 2009;21(4):146–149. | ||
Saghir S, Faiz M, Saleem M, Younus A, Aziz H. Characterization and anti-microbial susceptibility of Gram-negative bacteria isolated from bloodstream infections of cancer patients on chemotherapy in Pakistan. Indian J Med Microbiol. 2009;27(4):341–347. | ||
Abebe FA, Berhe DF, Berhe AH, Hishe HZ, Akaleweld MA. Drug use evaluation of ceftriaxone: the case of Ayder Referral Hospital, Mekelle, Ethiopia. Int J Pharm Sci Res. 2012;3(7):2191–2195. | ||
Rolston KV. Bacterial infection in neutropenic cancer patients: an overview. Arch Clin Infect Dis. 2009;4(2):115–122. | ||
Sader HS, Jones RN. Antimicrobial susceptibility of uncommonly isolated non-enteric Gram-negative bacilli. Int J Antimicrob Agents. 2005;25(2):95–109. | ||
Velasco E, Thuler LC, Martins CA, et al. Epidemiology of bloodstream infections at a cancer center. Sao Paulo Med J. 2000;118(5):131–138. | ||
de Oliveira-Garcia D, dall’Agnol M, Rosales M, et al. Fimbriae and adherence of Stenotrophomonas maltophilia to epithelial cells and to abiotic surfaces. Cell Microbiol. 2003;5(9):625–636. | ||
Viscoli C, Girmenia C, Marinus A, et al. Candidemia in cancer patients: a prospective, multicenter surveillance study by the Invasive Fungal Infection Group (IFIG) of the European Organization for Research and Treatment of Cancer (EORTC). Clin Infect Dis. 1999;28(5):1071–1079. | ||
Tuon FF, Costa SF. Rhodotorula infection: a systematic review of 128 cases from literature. Rev Iberoam Micol. 2008;25(3):135–140. | ||
Royo-Cebrecos C, Gudiol C, Ardanuy C, Pomares H, Calvo M, Carratalà J. A fresh look at polymicrobial bloodstream infection in cancer patients. PLoS One. 2017;12(10):e0185768. | ||
Gudiol C, Tubau F, Calatayud L, et al. Bacteraemia due to multidrug-resistant Gram-negative bacilli in cancer patients: risk factors, antibiotic therapy and outcomes. J Antimicrob Chemother. 2011;66(3):657–663. | ||
Pagano L, Tacconelli E, Tumbarello M, et al. Bacteremia in patients with hematological malignancies: analysis of risk factors, etiological agents and prognostic indicators. Haematologica. 1997;82(4):415–419. | ||
Swati M, Gita N, Sujata B, Farah J, Preeti M. Microbial etiology of febrile neutropenia. Indian J Hematol Blood Transfus. 2010;26(2):49–55. | ||
Crawford J, Dale DC, Lyman GH. Chemotherapy-induced neutropenia. Cancer. 2004;100(2):228–237. | ||
Uslan DZ, Steckelberg JM, Cockerill FR, Sauver JL, Wilson WR, Baddour LM. Age and sex associated trends in bloodstream infection: a population-based study in Olmsted County, Minnesota. Arch Intern Med. 2007;167(8):834–839. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.