Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 8
Effects of immediate postpartum contraceptive counseling on long-acting reversible contraceptive use in adolescents
Authors Kaewkiattikun K
Received 5 August 2017
Accepted for publication 3 October 2017
Published 30 October 2017 Volume 2017:8 Pages 115—123
DOI https://doi.org/10.2147/AHMT.S148434
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Alastair Sutcliffe
Kasemsis Kaewkiattikun
Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Bangkok, Thailand
Background: Adolescent pregnancy is a global public health problem, particularly repeated pregnancy. The best strategy to lower prevalence of adolescent pregnancy and repeated pregnancy is promoting highly effective long-acting contraceptive methods along with special counseling programs. Long-acting reversible contraception (LARC) is the ideal contraceptive of choice for adolescents. It is not known whether immediate postpartum contraceptive counseling increases postpartum LARC use in adolescents.
Objective: To compare LARC use between immediate and conventional postpartum contraceptive counseling and discover predictive factors of postpartum LARC use.
Materials and methods: This prospective, randomized controlled trial was conducted among postpartum adolescents at Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand, from 1 July 2016 to 31 March 2017. The participants were assigned to receive immediate postpartum contraceptive counseling or conventional postpartum contraceptive counseling. The primary outcome was postpartum LARC use. The secondary outcome was predictive factors for LARC use in postpartum adolescents.
Results: Of the 233 postpartum adolescents, postpartum LARC use was 87 of 118 (73.7%) in the immediate postpartum counseling group and 49 of 115 (42.6%) in the conventional postpartum counseling group (odds ratio 3.780, 95% CI 2.18–6.57, p<0.001). A significant predictive factor for LARC use in postpartum adolescents was immediate postpartum counseling (odds ratio 3.67, 95% CI 2.10–6.41, p<0.001).
Conclusion: Immediate postpartum contraceptive counseling led to a significant increase in postpartum use of LARC in adolescents, when compared with conventional (4–6 weeks) postpartum contraceptive counseling. Adolescent mothers who received immediate postpartum counseling were 3.67 times more likely to use LARC than those who received conventional postpartum counseling.
Keywords: long-acting reversible contraception (LARC), adolescent, contraception, contraceptive counseling, immediate postpartum contraceptive counseling
Introduction
An adolescent pregnancy is one that occurs in women <20 years of age. It is one of the major global public health issues. About 15 million adolescents give birth each year, roughly 11% of all births worldwide.1 According to Thailand Public Health Statistics, the Thai adolescent birth rate in 2012 was 53.8 per 1000 women aged 15–19 years, the highest rate in Southeast Asia and the second highest in the world.2,3
Adolescent pregnancy is known to have higher maternal, obstetrical, and neonatal risks. It is also associated with more adverse obstetric outcomes than adult pregnancy (e.g., poor maternal weight gain, anemia, gestational hypertension, preterm delivery, low-birth-weight babies and repeated pregnancy).4–7 Furthermore, adolescent-repeated pregnancy leads to adverse health, economic and developmental outcomes, particularly when the second pregnancy occurs within 2 years.8,9
The best strategy to lower prevalence of adolescent pregnancy and delay repeated pregnancy is promoting highly effective long-acting contraceptive methods along with special counseling programs. Of all contraceptive methods, long-acting reversible contraception (LARC) is the ideal first-line contraceptive of choice for adolescents. These methods are highly effective, safe, reversible and achieve better compliance than other methods.10 However, LARC use among adolescents is highly variable, dependent on access to healthcare and counseling. Moreover, timing of contraceptive counseling is an important factor in decision about contraception. Many earlier studies have reported the positive effects of contraceptive education or counseling on adolescent contraceptive use.11
Contraceptive counseling is an important part of family planning services. It is the cornerstone for providing accurate knowledge of contraceptive types and dispelling misconceptions about risks and side effects. Furthermore, it also offers proper advice for contraceptive choices to meet family planning needs and optimizing pregnancy spacing. A cluster randomized trial in 40 reproductive health clinics across the USA in 2011–2013 found the proportion of women using LARCs in the intervention group (LARCs counseling) was greater than the control group (standard contraceptive care) (2.3% vs 2.0%, coefficient for difference 0.004, 95% CI 0.003–0.004) and the pregnancy rate was lower in the intervention group than the control group (7.9 vs 15.4 per 100 person-years, hazard ratio 0.54, 95% CI 0.34–0.85)12
Contraceptive counseling may occur at any time of pregnancy, or even before it, from premarital, preconception, prenatal, immediately after birth, 4–6 weeks postpartum or any occasion. Nevertheless, most earlier reports often studied either the prenatal period, the postpartum period, or both. The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics recommend that discussion of contraceptive options and prompt initiation of a method postpartum should be a routine part of primary prenatal and postpartum care in all family planning clinics.13 The main reasons for counseling during these periods are increasing optimal contraceptive methods and extending the interval before subsequent pregnancies.
Effects of timing of counseling on contraceptive use are various and inconclusive. Many former studies reported the effects of contraceptive counseling at various point of postpartum and subsequent contraceptive use among women. A survey from New York City found that women counseled during the prenatal or postpartum, or both periods showed significantly increased odds of postpartum use of a more effective contraceptive method when compared with no counseling (32% vs 49% and 56%, respectively; P for trend <0.0001).14 Another population-based follow-up surveys conducted by the Italian National Institute of Health study revealed that contraceptive counseling to provide information, knowledge and awareness of contraception during pregnancy, childbirth and postpartum was strongly associated with effective postpartum contraceptive use.15 Therefore, there is no current standard of appropriate timing for contraceptive counseling.
Although studies have reported the effects of contraceptive counseling on postpartum contraceptive use among women, there are few prospective reports in medical literature that assess the impact of contraceptive counseling among adolescent women. Only 1 from 6 studies in adolescent women found a statistically significant positive impact of counseling on decreasing adolescent pregnancy.11,16 Nevertheless, there has not yet been a prospective study of contraceptive counseling during the immediate postpartum period among adolescents. This study will examine the associations between immediate postpartum contraceptive counseling with LARC use.
Materials and methods
A prospective, randomized, and single-blind trial was conducted among postpartum adolescent women at the Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand, from 1 July 2016 to 31 March 2017. Approval for the study was obtained from the Research Ethics Board at Faculty of Medicine Vajira Hospital and all the study subjects gave written informed consent during postpartum period. The trial was registered with www.clinicaltrials.in.th, registration number is TCTR20160920001.
The studied population consisted of all postpartum adolescent mothers (age 10–19 years) who were hospitalized and gave birth before reaching 20 years old at Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University. Inclusion criteria were Thai nationality adolescent mothers who could communicate in Thai, and sexually active (including both married and single marital status). Exclusion criteria were known learning difficulties or mental health problems, no need for contraception (divorce, hysterectomy or tubal sterilization), any conditions or allergies that contraindicated any contraceptive method, and refusal to participate in the study.
Sample size was calculated based on previous studies. There was significantly more contraceptive use at 6 months in mother who received health education at birth than in mothers who had not received health education at birth (odds ratio [OR] 1.62, 95% CI 1.06–2.5).17 The powers of 80% and a level of confidence of 95% were applied to determine the difference between groups. The ratio between each group was 1:1. The total number of participants was 222 (111 in each group). The randomization sequence was prepared by an independent data-coordinator with simple random sampling technic using a computer program. Participants were randomized and allocated into 2 groups. Based on a random allocation scheme derived from a computer-generated list of numbers, sealed and consecutively numbered opaque envelopes were prepared by a research assistant not involved in the study. All women were randomly allocated to 1 of the 2 study groups by opening the envelope during postpartum period.
All participants, who fulfilled the inclusion criteria, and their parents or legal guardians were informed of the trial processes on the postpartum ward by a research assistant. Since the participants were under the legal age of consent for this type of research, their parents or legal guardians provided informed consent on their behalf. Enrolled subjects completed a baseline questionnaire that included demographic information (age, weight, height, body mass index marital status, education, occupation, income), pregnancy intention, knowledge about contraception (assessed by asking what they knew about the different methods of contraception available, no formal tool used to assess the depth of participants’ knowledge), parity, number of antenatal care (ANC) visit, and mode of delivery. Participants were then randomly assigned in a 1:1 ratio to either the intervention group (immediate postpartum contraceptive counseling), or the control group (no immediate postpartum contraceptive counseling). No blinding of participants or counselors was feasible due to the nature of the intervention. Researcher did not know the participant’s allocation group and did not discuss the study with patients.
Eligible and consenting women in both groups received structured information and counseling by a specially trained family planning nurse. The intervention group was counseled during the immediate postpartum period (2–3 days postpartum, before hospital discharge) and at 4–6 weeks postpartum. The control group was counseled only at 4–6 weeks postpartum.
The counseling technique used in the present study was modeled after the GATHER technique for counseling, as used in the CHOICE project. GATHER is a client-centered and personalized counseling process. This technique includes 6 components: Greet each client in a friendly, polite, warm and respectful way to create a good relationship between counselor and client; Ask the client about her family planning needs; Tell the client about all the birth control methods available to her; Help the client make the decision that is best for her; Explain how to use the approved birth control method; Return visits or follow-up to discuss client’s concerns. Contraceptive information and counseling consist of postpartum contraceptive methods, effectiveness, advantages, disadvantages, risks, adverse effects and proper contraceptive method, especially LARC.18–19
After counseling, all participants could freely choose any contraceptive method as desired. No financial incentive was given to affect contraceptive choice or accept LARC use. In addition, no participants needed to pay any expense because the Thai National Health Security Office and the Faculty of Medicine Vajira Hospital supported all expenses for all contraceptive methods to promote contraception in adolescents. All contraceptive methods were available at the family planning unit. If adolescent mothers decided to use LARC methods, the family planning doctors would insert LARC (intrauterine devices or implants) at that time.
The primary outcome of this study was the proportion of participants choosing LARC comparing those who received immediate postpartum contraceptive counseling with those who received conventional postpartum contraceptive counseling. The secondary outcome was predicting factors of postpartum LARC use. The participant’s allocation group was unblinded before data analysis.
The data were analyzed by statistician using SPSS version 22 (IBM, Armonk, NY, USA). Chi-square test and Fisher’s exact test were used for categorical data and Student’s t-test was used for continuous data. Univariate and multivariate analyses were further entered into logistic regression analysis to determine independent predictors of LARC use and presented as OR and 95% CI. p-value of <0.05 was considered statistically significant. The need to register the trial was not recognized until the study was completed, and thus the trial was registered with www.clinicaltrials.in.th. Registration number is TCTR20160920001.
Results
This study was conducted between 1 July 2016 and 31 March 2017. Figure 1 shows the trial flow of the study. Two hundred and fifty eligible postpartum adolescent women were recruited, 10 were excluded due to divorce. A total of 240 women were randomly assigned to either the immediate contraceptive counseling group (study group), or to the no immediate contraceptive counseling group (control group). At 4–6 weeks postpartum, 2 in the study group and 5 in the control group lost to follow-up. A total 233 adolescent mothers were finally eligible for analysis in this study, 118 in study group and 115 in control group.
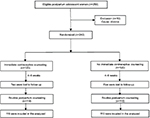  | Figure 1 Trial flow of the study population and the number of adolescent mothers in each group. |
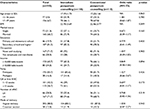
Table 1 shows baseline characteristics of adolescent mothers. Of all 233 participants, the majority were 17–19 years old (67.0%), married (68.7%), had a secondary/high school education (82.2%), had either no occupation or were currently studying (71.7%), had low income (65.7%), were primipara (83.7%), and had gestational age at first ANC >12 weeks (56.7%), number of ANC >4 (71.7) and delivered vaginally (88.0%). A comparison of adolescent mothers in the immediate postpartum counseling group (n-118) with the conventional postpartum counseling group (n-115) revealed no statistical difference in baseline characteristics between groups.
With regard to contraceptive behavior and family planning, most adolescent mothers had an unintended pregnancy (63.9%), despite most having contraceptive knowledge (76.8%). Previous contraceptive use before pregnancy was mainly of less effective methods (non LARC 97.0%). In the postpartum period, most of them intended to prolong the interval between next pregnancy for ≥3 years (96.1%), but postpartum contraceptive intention was still for less effective methods (non LARC 76.8%). However, postpartum contraceptive use was mainly LARC (58.4%) due to effect of immediate postpartum counseling.
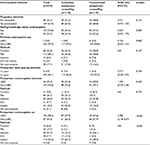
A total of 87 of 118 adolescent women (73.7%) in the immediate postpartum counseling group and 49 of 115 (42.6%) in the conventional (not immediate) postpartum counseling group used LARC for postpartum contraception. There was a statistically significant greater use of LARC in the immediate postpartum contraceptive counseling group than in the conventional postpartum counseling group (OR 3.780, 95% CI 2.18–6.57, p<0.001). However, other contraceptive behaviors, including pregnancy intention, knowledge about contraception, previous contraceptive use before conception, postpartum birth spacing intention, and postpartum contraceptive intention, were not significantly different between the 2 groups (p>0.05) (Table 2).
To analyze factors predicting LARC use, univariate regression analysis found that education, pregnancy intention, parity and immediate counseling were significant factors (p<1.0). After adjusting OR estimated by multiple logistic regression adjusting for education, pregnancy intention, parity and immediate counseling were analyzed. This study revealed that immediate counseling was the only significant predictive factors for LARC use in postpartum adolescents (Table 3). Adolescent mothers who received immediate postpartum counseling used LARC 3.67 times more than those who had received conventional postpartum counseling.
Discussion
In this randomized controlled trial, the author found that immediate postpartum contraceptive counseling in adolescent mothers was significantly correlated with increased use of LARC when compared with conventional postpartum contraceptive counseling (OR 3.780, 95% CI 2.18–6.57, p<0.001). Comparison with previous studies of immediate postpartum contraceptive counseling shows, this finding is consistent with the result of study in Nepal, in which women were randomly assigned to 4 groups to receive health education: immediately after birth and 3 months later, at birth only, at 3 months, and none. They found that women who received counseling immediately postpartum and a session 3 months later were more likely to use contraception at 6 months than those who attended only the later session (OR 1.62; 95% CI 1.06–2.50).17 Moreover, this study is also consistent with the result of a community-based cross-sectional study in South Ethiopia. They found that mothers who were counseled on LARC methods during the immediate postpartum period were greater users of LARC than those who were not counseled (OR 4.55; 95% CI: 1.94, 10.66, p-value <0.001).20
Nevertheless, the present study was a randomized controlled trial in postpartum adolescent mothers, which differed from both previous studies. In the study in Nepal, they studied all age groups of pregnant women (adults and adolescents), which was different from this study in terms of participants studied. The study in South Ethiopia was a community-based cross-sectional study in postpartum (41–365 day) women, which was different from this study in design and participants studied. However, a randomized controlled trial of postpartum adolescent mothers has not been performed previously.
Eligible participants in this study mostly had knowledge of contraception (76.8%), but contraceptive use before current pregnancy consisted mostly of less effective methods (condom and pills, 73.9%) or no contraception (17.1%), causing unintended pregnancy (63.9%) (Table 2). This finding is consistent with an institutional-based cross-sectional descriptive study in Nigeria. They found that knowledge of contraception was 87.7% among unmarried undergraduate students while prevalence of contraceptive use among sexually active students was only 15.63%.21 These findings led to a reconsideration of sex education curriculum for adolescents, especially contraceptive knowledge, and contraceptive campaign in adolescents.
In postpartum period, most adolescent mothers planned to postpone the next pregnancy by >3 years while intended postpartum contraceptive methods were short-acting reversible contraception (condom, pills and injection, 71.7%). This unmet need for contraception might be the major cause of repeated pregnancy in adolescents. However, most adolescent mothers in present study finally decided to use LARC for postpartum contraception. This changing of contraceptive preference and the decision to use LARC postpartum was the effect of immediate postpartum counseling. Adolescent mothers who received immediate postpartum contraceptive counseling showed greater LARC use than those who only received conventional postpartum counseling (87 of 118, 73.7% in immediate group and 49 of 115, 42.6% in conventional group). This finding was confirmed by multiple logistic regression analysis. Adolescent mothers who received immediate postpartum counseling used LARC 3.67 times more than those who received conventional postpartum counseling. Therefore, immediate postpartum contraceptive counseling is an important strategy to enable effective contraceptive use, address unmet needs for contraception and optimize birth spacing in adolescents.
There is clear evidence that contraceptive counseling is essential to promote contraceptive use,22,23 but the benefits depend on timing of counseling. Prenatal counseling theoretically lays the groundwork for postpartum contraceptive decisions, but many previous studies demonstrated that prenatal contraceptive counseling did not increase postpartum contraceptive use.24–26 This may be due to the long time taken to reach the postpartum period, when most pregnant women are focused on preparing for childbirth and newborn care. Counseling during 4–6 weeks postpartum period is conventional practice in almost all hospitals. It is useful in encouraging proper contraceptive decisions, and for discussing any concerns about changing a woman’s preference for contraception. Nevertheless, a prospective case–control study from Turkey found that an additional 6 weeks postpartum counseling did not increase postpartum use of modern contraception.27 Therefore, contraceptive counseling in either the prenatal or postpartum period may not be fully beneficial to increase postpartum contraceptive use. There is evidence that multiple sessions of counseling are promising for prolonged pregnancy spacing. For instance, a study from New York found that the prevalence of postpartum contraceptive use, including the use of more effective methods, was highest when contraceptive counseling was provided during both prenatal and postpartum periods.27 However, multiple sessions of counseling will take a lot of time to complete. Thus, health care providers should adapt according to their settings and resources.28
Contraceptive counseling in the immediate postpartum period may be the proper time for promotion of contraceptive use, because it is the best period when mothers are curious to know and ready to initiate contraceptive methods for prevention of further pregnancy. However, there was only 1 previous report from Nepal that demonstrated more contraceptive use in women following health education immediately after birth.1 In addition, findings from this study also confirmed the appropriateness of the immediate postpartum period for contraceptive counseling for increasing LARC use.
The results of this study indicate that health professionals should provide contraceptive counseling to adolescent mothers during the immediate postpartum period rather than the conventional 4–6 weeks postpartum period. This approach may be generalizable to post-abortion adolescents to prevent repeated pregnancy. Immediate post-abortion contraceptive counseling should lead to more LARC use than the usual 2–4 weeks post-abortion period. Additionally, postpartum adult mothers probably benefit from immediate postpartum contraceptive counseling for most proper contraceptive methods.
The strengths of this study included a prospective randomized controlled trial and low rate of loss to follow-up. Moreover, there was no financial barrier for LARC use because the Thai National Health Security Office supported all expenses for LARC. Therefore, all participants did not need to pay anything. However, the limitations of this study include factors that might affect contraceptive decisions, such as attitudes and beliefs about contraceptive use, male partner influence, socioeconomic status of family, accessibility to contraceptive services and reasons for choosing contraception that were not evaluated in this study. Further research would study continuation rate of LARC use between immediate postpartum counseling and conventional postpartum counseling mothers. Moreover, suggestions for future research should be extended to the study of LARC use in the general adolescent population to reduce adolescent pregnancy.
Conclusion
Immediate postpartum contraceptive counseling significantly increased LARC use in adolescent mothers. There were no predictive factors for LARC use in postpartum adolescents.
Acknowledgments
The author would like to express gratitude to all participants in this study and thank all staff of the Family Planning Unit, Department of Obstetrics and Gynecology Vajira Hospital for their support in the data collection. This research was funded by the Faculty of Medicine Vajira Hospital, Navamindradhiraj University. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The research protocol received ethical approval from the Vajira Institutional Review Board and Ethical Committee in June 2016.
Disclosure
The author reports no conflicts of interest in this work.
References
Rosen JR. Position Paper On Mainstreaming Adolescent Pregnancy In Efforts to Make Pregnancy Safer. Department of Making Pregnancy Safer. Geneva: World Health Organization; 20120. | ||
Sukrat B. Thailand adolescent birth rate: trend and related indicators. Thai J Obstet Gynaecol. 20134;22(14):155–216. | ||
UNICEF, Progress for Children: A Report Card on Adolescents. New York: The Institute; 20172. | ||
Liabsuetrakul T. Trends and outcomes of teenage pregnancy. Thai J Obstet Gynaecol. 20182;20(4):1962–165. | ||
Chandra PC, Schiavello HJ, Ravi B, Weinstein AG, Hook FB. Pregnancy outcomes in urban teenagers. Int J Gynaecol Obstet. 2002;79(2):117–122. | ||
Stevens-Simon C, McAnarney ER. Adolescent pregnancy. Gestational weight gain and maternal and infant outcomes. Am J Dis Child. 1992;146(11):1359–1364. | ||
Thaithae S, Thato R. Obstetric and perinatal outcomes of teenage pregnancies in Thailand. J Pediatr Adolesc Gynecol. 2011;24(6):342–346. | ||
Chinaglia M, Oliveira N, Silva J. Maternal and perinatal outcomes in multiparous adolescents. Revista de Ciencias Medicas. 2005;14(2):139–146. | ||
Rigsby DC, Macones GA, Driscoll DA. Risk factors for rapid repeat pregnancy among adolescent mothers: a review of the literature. J Pediatr Adolesc Gynecol. 1998;11(3):115–126. | ||
Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med 2012;366:1998–2007. | ||
Zapata LB, Tregear SJ, Curtis KM et al. Impact of contraceptive counseling in clinical settings: a systematic review. Am J Prev Med. 2015;49(2 Suppl 1):S31–S45. | ||
Harper CC, Rocca CH, Thompson KM et al. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomized trial. Lancet. 2015;386(9993):562–568. | ||
American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 7th ed. Washington, DC: American College of Obsetricians and Gynecologists; 2012. | ||
Zapata LB, Murtaza S, Whiteman MK et al. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015;212(2):171.e1–e8. | ||
Lauria L, Donati S, Spinelli A, Bonciani M, Grandolfo ME. The effect of contraceptive counselling in the pre-and post-natal period on contraceptive use at three months after delivery among Italian and immigrant women. Ann Ist Super Sanita. 2014;50(1):54–61. | ||
Brindis CD, Geierstanger SP, Wilcox N, McCarter V, Hubbard A. Evaluation of a peer provider reproductive health service model for adolescents. Perspect Sex Reprod Health. 2005;37(2):85–91. | ||
Bolam A, Manandhar DS, Shrestha P, Ellis M, Costello AM. The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised controlled trial. BMJ. 1998;316(7134):805–811. | ||
Rinehart W, Rudy S, Drennam M. GATHER guide to counselling. Popul Rep J. 1998;48:1–31. | ||
Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88(2):243–249. | ||
Tamrie YE, Hanna EG, Argaw MD. Determinants of long acting reversible contraception method use among Mothers in Extended Postpartum Period, Durame Town, Southern Ethiopia: a cross sectional community based survey. Health. 2015;7:1315–1326. | ||
Ahmed ZD, Sule IB, Abolaji ML, Mohammed Y, Nguku P. Knowledge and utilization of contraceptive devices among unmarried undergraduate students of a tertiary institution in Kano State, Nigeria 2016. Pan Afr Med J. 2017;26:103. | ||
Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57(4):659–673. | ||
Lee JK, Parisi SM, Akers AY, Borrerro S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26(7):731–736. | ||
Smith KB, van der Spuy ZM, Cheng L, Elton R, Glasier AF. Is postpartum contraceptive advice given antenatally of value? Contraception. 2002;65(3):237–243. | ||
Akman M, Tuzun S, Uzunera A, Basgul A, Kavak Z. The influence of prenatal counselling on postpartum contraceptive choice. J Int Med Res. 2010;38(4):1243–1249. | ||
Ayiasi RM, Muhumuza C, Bukenya J, Orach CG. The effect of prenatal counselling on postpartum family planning use among early postpartum women in Masindi and Kiryandongo districts, Uganda. Pan Afr Med J. 2015;21:138. | ||
Vural F, Vural B, Cakıroglu Y. The effect of combined antenatal and postnatal counselling on postpartum modern contraceptive use: prospective case-control study in Kocaeli, Turkey. J Clin Diag Res. 2016;10(4):QC04–QC07. | ||
Lopez LM, Hiller JE, Grimes DA, Chen M. Education for contraceptive use by women after childbirth (Review). Cochrane Database Syst Rev. 2012;8:1–35. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.