Back to Journals » International Journal of Women's Health » Volume 8
Exploring Australian women’s level of nutrition knowledge during pregnancy: a cross-sectional study
Authors Bookari K, Yeatman H, Williamson M
Received 7 April 2016
Accepted for publication 18 June 2016
Published 16 August 2016 Volume 2016:8 Pages 405—419
DOI https://doi.org/10.2147/IJWH.S110072
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Khlood Bookari,1 Heather Yeatman,1 Moira Williamson2,3
1School of Health and Society, Faculty of Social Sciences, 2School of Nursing, Faculty of Science, Medicine and Health, University of Wollongong, Wollongong, NSW, 3School of Nursing and Midwifery, Higher Education Division, Central Queensland University, Noosaville, QLD, Australia
Background: The Australian Guide to Healthy Eating (AGHE) for pregnancy provides a number of food- and nutrition-related recommendations to assist pregnant women in optimizing their dietary behavior. However, there are limited data demonstrating pregnant women’s knowledge of the AGHE recommendations. This study investigated Australian pregnant women’s knowledge of the AGHE and related dietary recommendations for maintaining a healthy pregnancy. The variations in nutrition knowledge were compared with demographic characteristics.
Methods: A cross-sectional study assessed eight different nutrition knowledge domains and the demographic characteristics of pregnant women. Four hundred women across Australia completed a multidimensional online survey based on validated and existing measures.
Results: More than half of the pregnant women surveyed (65%) were not familiar with the AGHE recommendations. The basic recommendations to eat more fruit, vegetables, bread, and cereals but less meat were poorly understood. An in-depth investigation of knowledge of nutrition information revealed misconceptions in a range of areas, including standard serving size, nutrients content of certain foods, energy density of fat, and the importance of key nutrients in pregnancy. Univariate analysis revealed significant demographic variation in nutrition knowledge scores. Multiple regression analysis confirmed the significant independent effects on respondents’ nutrition knowledge score (P<0.000) of the education level, income, age, stage of pregnancy, language, and having a health/nutrition qualification. The model indicated that independent variables explained 33% (adjusted R2) of the variance found between respondents’ knowledge scores.
Conclusion: Australian pregnant women’s knowledge regarding AGHE for pregnancy and other key dietary recommendations is poor and varies significantly with their demographic profile. The setting of dietary guidelines is not sufficient to ensure improvement in their nutrition knowledge. It is essential that women receive support to achieve optimal and healthy diets during pregnancy.
Keywords: Australian Guide to Healthy Eating for pregnancy, nutrition knowledge, pregnancy, health
Introduction
An optimally nourishing diet is important for health during pregnancy. Poor diet places women at a higher risk of unhealthy gestational weight gain,1 which can negatively impact mothers’ and babies’ health, causing a range of poor maternal and infant outcomes.2 Exposure of the unborn baby to maternal obesity, diabetes, and excessive gestational weight gain can increase his/her risk of developing childhood obesity and chronic diseases later in life.3,4 Yet, many women do not sustain an optimal diet prior to and during pregnancy. Some pregnant women’s diets lack key nutrients, including folate, fiber, and iron.5 Their diets do not comply with official dietary guidelines with respect to consumption of some major food groups (including bread and cereals, fruit, vegetables, grains, and protein foods [nuts, beans, eggs, and fish]), and many are characterized as being high in processed meat, soft drinks, and takeaway foods.5–10
A number of behavioral change theories such as the planned behavior theory,11 social cognitive theory,12 and transtheoretical model13 recognize the important role that nutrition knowledge, attitudes, and motivations can play in the process of food choices. Such theories assume a rational relationship in the intersection of beliefs, attitudes, intentions, and behaviors for “volitional behavior”. Sapp14 argued that for individuals to adopt a rational approach to food intake, they first needed to reach a “high threshold level of ‘how-to’ and ‘awareness’ nutrition knowledge”. Conversely, incomplete knowledge and false beliefs can lead to ill-formed intentions and nonrational nutrition behavior. The same could be said for dietary behavior in pregnancy. Women’s accurate knowledge of dietary guidelines during pregnancy may assist them to make appropriate food choices and to achieve a balanced diet for themselves and their unborn babies as it may assist them to reject false or nonevidence-based messages or uninformed advice from family, friends, and social media.
Pregnancy is an important time to increase women’s awareness about healthy eating.15 Pregnant women recognize diet as important to fetal health and are more likely to be mindful of nutrition, seek health advice, and modify their diets.16 Nutrition knowledge has been positively associated with maternal dietary behavior17,18 and use of supplements.19 Nutrition education also has been shown to have beneficial effects on pregnancy outcome,20 reducing the number of infants born >4 kg, reducing the incidence of respiratory distress syndrome, and producing shorter length of stay in hospitals.21
Many countries around the world22,23 have established dietary guidelines to improve eating habits of individuals through their lifespan. Dietary guidelines are considered a foundation of any strategy to promote the consumption of healthy foods.9 In Australia, the Australian Dietary Guidelines24 provide recommendations on health, weight management and nutrition, and food safety for the general population and specific information for pregnant women.25,26 The revised Australian Dietary Guidelines were published in 2013 and included changes to the information provided for pregnant women, such as the recommended number of serves of fruit, vegetables, bread and cereals, dairy, and meat and its alternatives, and the standard serve size for bread and cereals group. The revised Australian Guide to Healthy Eating (AGHE) for pregnant women references the Institute of Medicine’s guidelines for weight gain during pregnancy.25 A number of Australian government websites provide useful, evidence-based information on healthy eating, weight management, management of discomfort, staying active, the need for and potential dangers of supplementation, and the importance of key nutrients and food safety during pregnancy.25–28
Having information available does not necessarily translate into increases in pregnant women’s nutrition knowledge. Little has been reported on Australian women’s knowledge of these guidelines and other food- and nutrition-related recommendations. The existing studies have focused on investigating either women’s awareness of specific single nutrients required during pregnancy29–31 or their knowledge of AGHE recommendations for adults in the general population.8 Women’s knowledge of food handling practices and weight gain during pregnancy has also been examined separately in the previous studies.32,33 Understanding pregnant women’s level of knowledge of the AGHE and specific nutrition and dietary recommendations during pregnancy is important for guiding the development of effective approaches to support women in maintaining a healthy diet and avoiding harmful excessive weight gain during pregnancy.
A number of studies have noted demographic variations in nutrition knowledge. Identifying groups of pregnant women who might be at risk of having inadequate nutrition knowledge could permit the adoption of well-targeted and effective communication strategies regarding pregnancy nutrition. A study32 indicated that higher levels of knowledge about “high Listeria risk foods” were associated with a number of sociodemographic characteristics of pregnant women. These included first language (English), planned pregnancy, and household income (>AU$50,000/yr). Other studies8,29 found that women with higher educational levels demonstrated the highest levels of “nutrition knowledge”, “knowledge about the consequences of folic acid deficiency” and “knowledge about the adverse health outcomes associated with low iodine intake” during pregnancy.
The purpose of this study was to:
- survey pregnant women’s level of knowledge of the AGHE for pregnancy and relevant dietary and nutrition recommendations for maintaining a healthy pregnancy; and
- identify demographic differences related to knowledge levels.
Methods
Study design
To recruit pregnant women, this cross-sectional study used convenience sampling. To minimize the potential for social desirability bias, the survey was designed to be administered online and self-completed and the participation was anonymous.
Survey development
A multidimensional survey was developed for this study based on an existing survey34 and components from four validated surveys.32,35–37 The survey explored five major dimensions using a total of 109 items. The dimensions assessed were pregnant women’s:
- reported adherence to the five food groups and extras (six items);
- attitudes toward key nutrition topics (17 items);
- level of motivation to maintain a healthy diet (four items);
- knowledge of the AGHE during pregnancy and a range of diet-related matters (70 items); and
- knowledge of guidelines for weight gain and its management during pregnancy (12 items).
Demographic characteristics recorded included prior pregnancies, stage of pregnancy, planned pregnancy, age, marital status, level of education, household income, first language, possession of a health/nutrition-related qualification, whether seen by a dietitian/nutritionist, and the classification of women’s body mass index (BMI) based on Institute of Medicine 2009 guidelines.
The survey instrument was developed in early 2012 and implemented between October 2012 and July 2013. As a check on face validity, the survey questions were reviewed individually by a supervisory team (one with an expertise in public health nutrition and another with midwifery expertise) and four accredited practising dietitians (including a maternal health dietitian) to ensure they reflected the AGHE recommendations for pregnant women published prior to February 2013 and the dietary and nutrition recommendations for maintaining a healthy pregnancy as provided on the Australian government website (prior to the same date). A statistician (an accredited practicing dietitian and expert on question construction) then reviewed the survey to ensure that it did not contain common errors (eg, leading, confusing, or double-barreled questions).
The survey was pilot tested first with five researchers (dietitians) from the School of Health Science at the University of Wollongong (UOW). This was followed by pilot testing of the survey with a small convenience sample of ten pregnant women to determine time for survey completion, identify items that lacked clarity, and ensure that the instructions and contents were easily comprehensible and layout was acceptable.38 Modifications were consequently made to some existing questions (for clarity), and a few items were added. The UOW Human Research Ethics Committee, which included a dietitian, reviewed and approved the survey. All authors were involved in revising the final version of the survey and making changes based on the feedback received during pilot testing.
The reliability was calculated for three dimensions of the survey, including “women’s attitudes toward key nutrition topics”, “women’s level of motivation to maintain a healthy diet”, and “women’s knowledge of the AGHE during pregnancy and a range of diet-related matters”. Each dimension was explored using a set of items intended to assess different aspects of that single attribute. The reliability test was not calculated for the remaining dimensions, which included “women’s reported adherence to the five food groups and extras” and “women’s knowledge of guidelines for weight gain and its management during pregnancy”, as these two dimensions contained multidimensional scale questions (eg, open-ended questions, multiple choice). For the other three dimensions, the α coefficients were slightly >0.8, which suggests that the scales had good internal consistency. The information about the five dimensions of the survey and the reliability results is presented in Table 1.
This article reports only on the fourth dimension: women’s knowledge of the AGHE during pregnancy and a range of diet-related matters. The nutrition knowledge section contained eight domains assessing nutrition knowledge (consisting of 70 items). Details of the survey domains relating to nutrition knowledge and demographic information collected and reported on in this study are in Table 2. Knowledge was assessed with multiple-choice questions, with a majority of questions (67) having one correct response option, while two questions (on multivitamins and supplements in pregnancy) had more than one correct response option. The respondents were asked to choose from a range of different scales answers such as “true, false, don’t know”; “yes, no, not sure”; “high, low, not sure”; “less than one serve, one serve, more than one serve, not sure”; or a choice of four different food options and “not sure”. To score the survey, correct responses to nutrition knowledge questions were scored as 1, while incorrect and “not sure” responses were scored as 0. Responses for each domain were added to give a total domain score, and the eight domain scores were added to give an overall nutrition knowledge score, with a maximum possible score of 72.
Survey administration
All data were obtained online using an online survey instrument. Recruitment took place between October 2012 and July 2013. To maximize response rates, different recruitment strategies were used to invite pregnant women to complete the online survey independently (Figure 1). The pregnant women were recruited either through verbal invitation or via distribution of invitation leaflets. Women were approached directly at two pregnancy/baby expos (fairs) held in Wollongong and at antenatal clinic waiting rooms of the participating hospitals. Seven public hospitals with antenatal clinics in New South Wales (NSW), Australia, were invited to participate with all but two responding and agreeing to participate. The pregnant women were provided with information verbally on the purpose of the survey and informed that participation was voluntary. If they agreed to participate, they were provided with an iPad to complete the survey at the time without any input from researcher or given an information leaflet with a link to complete the survey online at a later time.
  | Figure 1 The study recruitment strategy. |
The study invitation leaflets were distributed at two baby stores located in NSW and in the Australian “Bounty Mother To Be Bags”. These bags contained product samples and information for the pregnant women and were distributed at hospitals/pharmacists/chemists across NSW. Additional women from across Australia participated via an unplanned snowball effect in which survey respondents promoted the survey to their friends verbally and through social media (Facebook and pregnancy website/discussion boards).
Measures and outcomes
This article reports on the eight domains of nutrition knowledge of pregnant women and on the relationship of demographic variation to knowledge levels.
Statistical analysis
Raw data were downloaded from the SurveyMonkey website and the iPads and transferred to the Statistical Package for the Social Sciences software (Version 22.0; IBM Corporation, Armonk, NY, USA). For the purposes of analysis for this study, only results from fully completed surveys were included. Comparisons between the study cohorts were not possible as no record was kept of the different methods of data collection. Cronbach’s alpha and Kuder and Richardson Formula 20 were calculated to measure reliability of measurements with scale type of questions and with dichotomous choices, respectively.
Scores were calculated for each domain and also for the overall nutrition knowledge (a total of the eight domains). Women’s prepregnancy BMIs were calculated based on the self-reported prepregnancy weight and height.39 Descriptive and inferential statistics were used to describe and analyze the data. One-way ANOVA and independent t-test were used to assess the variations in the mean total scores of nutrition knowledge based on categories of demographic factors. Predictors of women’s nutrition knowledge were identified via multiple linear regression analyses. Given the relatively high number of factors, only factors that were significantly associated with women’s nutrition knowledge (in one-way ANOVA and independent t-test, P<0.05) were included in the regression analysis to prevent overcomplicated presentation of the results.40 Then the association of each predictor with the nutrition knowledge score when adjusted for other predictors was identified using multiple linear regression analyses. Significance was identified at P<0.05.
Ethical approval
The study was approved by the UOW Human Research Ethics Committee, South Eastern Sydney and Illawarra Area Health Service, and South Western Sydney Local Health District sites (Campbelltown/Liverpool hospitals). Participant’s information sheet was included in the first page of the on-line survey. The consent was implicitly taken by including the following statement at the same page “By completing the survey you agree to take part in the study”.
Results
Study sample characteristics
Responses were received from 472 pregnant women, 72 of whom did not fully complete the survey. The demographic characteristics of survey respondents are presented in Table 3. Of the 400 women who fully completed the questionnaire, 328 (82%) were from the state of NSW, the majority spoke English as their first language (83%), and more than half (53.3%) held a university degree. Just over half (52.2%) were in their third trimester, 37.8% were in their second trimester and the remainder (10%) in their first trimester. For approximately half of respondents (49%), this was their first pregnancy. Approximately 40% of the respondents were classified as either “overweight” (20.5%; BMI 25–29.9 kg/m2) or “obese” (19.3%; BMI ≥30 kg/m2).
Summary of descriptive statistics of the eight nutrition knowledge domains
Table 4 summarizes the mean score achieved by respondents across each of the eight nutrition knowledge domains assessed. The percentage of mean score (the average percentage of the score relative to the total possible score) is provided for each domain to enable the interdomain comparison. The respondents showed the highest levels of knowledge for “food safety practice in pregnancy” (84.22% correct), “diet–health relationship” (71.16% correct), and “nutrient sources” (66.81% correct). Lowest scores were achieved for knowledge of the “multivitamin and supplements during pregnancy” (48.40% correct) and “importance of key nutrients in pregnancy” (46.50% correct).
Recommended intakes of five food groups and extras
Approximately two-thirds (65.2%, n=261) of respondents stated they were not familiar with the AGHE for pregnant women. Although 34.8% (n=139) of respondents indicated that they were familiar with the AGHE recommendations, analysis indicated that there was no difference in their awareness of recommended intake of the five major food groups compared to those who answered that they were not aware of the AGHE (P<0.63). The respondents were asked to identify, from a list of multiple-choice options, the correct number of serves/day of each of the five major food groups in the AGHE. The respondents demonstrated a high level of awareness of recommended intake for the “extras” (86.5%, n=346) but less awareness of recommended intake of dairy foods (56.5%, n=226). Less than half of the respondents were aware of the recommended intakes for fruit and vegetables (45%, n=179), bread and cereals (34.5%, n=138), and meat and its alternative food groups (28.5%, n=114).
Food sources of nutrients
In this domain, the respondents’ understanding of food sources of certain macro- and micronutrients and energy density of fat was assessed (Table 5). The majority of respondents could successfully identify food sources as high or low in added sugar for most items, including strawberry yoghurt (69.8%, n=279), muesli bar (79.2%, n=317), bananas (83.2%, n=333), and 35% orange juice (89.2%, n=357). Some misperceptions were evident for a number of areas: salt content of pasta, with only 55.2% (n=221) identifying it as low in salt; dietary fiber content of cornflakes, with only 56.5% (n=226) identifying it as a low source of fiber; and saturated fat content of avocado, with only 60% (n=240) of respondents identifying it as a low source of saturated fat. When asked to identify food sources high or low in salt, half of the items were answered correctly, including sausages as high in salt (87.2%, n=349) and spinach as low in salt (90.8%, n=363); however, only 12.8% (n=51) of the pregnant women correctly identified wholegrain bread as high in salt.
  | Table 5 Women’s awareness of food sources of certain macro- and micronutrients and energy density of fat |
The respondents were able to identify food sources high in iron (63.7%, n=255), iodine (65.2%, n=261), and omega-3 fatty acids (90%, n=360) but less able to correctly identify foods that were a high source of vitamin A (38%, n=152). The majority of women (62%, n=248) did not identify liver as a high source of vitamin A, among a list including cheese and sweet potato. Seventy-eight percent of respondents (n=314) were unable to recognize that fat is the macronutrient that has the most kilojoules (calories) compared to sugar and alcohol.
Healthy meal proportion and serving size
The respondents were asked to identify correct constituent proportions for a healthy meal from pictures showing plates with different proportions of the various food groups. The respondents were also asked to identify the standard portion size of certain food items from each food group. The majority of the women (75.5%, n=302) were able to recognize the plate that represented a healthy dinner plate. The respondents were unable to identify the standard serving size of the following food items: grapes (54% incorrect, n=216), cheese (64.8%, n=259), strawberries (74%, n=296), cooked rice/pasta (82.5%, n=330), and yogurt (90%, n=360). Just over half of the respondents were able to select the standard serving size for breakfast cereal flakes or porridge (50.5%, n=203) and chocolate bars (55.8%, n=223), while 67% (n=268) correctly identified the standard serve size for meat pie.
Choosing everyday foods
The maximum possible score for knowledge about choosing everyday foods was 3. Most respondents (73.8%, n=295) were able to answer two out of three questions correctly. The question answered incorrectly by the majority of the respondents (86.5%, n=346) related to the healthier serving options of pasta and sauce (amounts and proportions) of spaghetti bolognese.
Vitamins and other supplements in pregnancy
Women’s awareness about the recommendations for supplements in pregnancy was explored, including vitamins and other recommended supplements (folic acid and iodine), as well as those vitamins for which there were dangers associated with excessive doses (vitamin A, vitamin D, and vitamin B6). The National Health and Medical Research Council message for women to take folic acid supplements during pregnancy was understood by the majority of the respondents (93.5%, n=374); however, only half of the respondents (51.7%, n=207) were aware of the correct recommendation for iodine supplementation during pregnancy.
The women were asked to identify micronutrients for which there was a risk associated with excessive intake, from a list including zinc, vitamin A, magnesium, vitamin D, and vitamin B6. Three in ten women indicated that they were not aware of any micronutrients that posed a risk associated with excessive intake. Half of the respondents were able to correctly identify one (n=205) nutrient, and only 11% correctly identified two nutrients (n=46) out of possible three. Less than one-third of the women (30%) correctly identified all the three nutrients (vitamin A, vitamin D, and vitamin B6) as micronutrients that may pose a risk when taken during pregnancy. The highest level of awareness was for vitamin A (56.3%, n=225) and the lowest for vitamin D (17.5%, n=70).
Diet–health relationship
Domain six explored respondents’ knowledge of dietary behaviors that can assist in managing some common pregnancy discomforts, including nausea/vomiting, heartburn, and constipation. Most respondents correctly identified that eating “less fatty and spicy foods” (79.8%, n=315), “eating smaller meals more often” (88%, n=352), as well as “avoiding regular large snacks” (90.2%, n=361) would help minimize the effect of nausea and vomiting during pregnancy. Inversely, more than half of the respondents (56.5%, n=226) incorrectly indicated that eating sweet biscuits in the morning would help in managing morning sickness.
A large proportion of respondents were aware of the potential to minimize the effect of heartburn during pregnancy by “avoiding lying down shortly after eating” (77.8%, n=311) and eating “small frequent meals and nutritious snacks” (83%, n=332) and “less fatty and spicy foods” (86%, n=344). Conversely, only 27.2% (n=109) of the respondents correctly identified that eating less sugar would not help in managing heartburn discomfort.
The majority of the respondents were aware that “exercising regularly” (89.2%, n=357) and “eating more fruit and vegetables” (92.8%, n=371) could assist in resolving constipation in pregnancy. However, more than two-third (69.5%, n=278) incorrectly identified that “eating less spicy and salty foods” would assist in resolving constipation.
Importance of key nutrients during pregnancy – iodine and omega-3
Just over half (57%; n=228) of the respondents identified iodine as an important micronutrient for healthy development of the fetal brain, while only 36% (n=144) identified omega-3 fatty acids as a nutrient that could help in the development of a fetus’s eyes, brain, and nervous system.
Food safety practice in pregnancy
In the final survey domain, the respondents’ knowledge of issues related to food safety was assessed. The questions focused on personal hygiene (hand washing), food preparation/storage (using the same surface for cutting raw meat and vegetables, reheating food, storage of food at appropriate temperature, storage of raw meat in refrigerator, correct temperature of refrigerator), and safe foods and fish to consume, as well as Listeria contamination issues in pregnancy. All the questions were answered correctly by the majority of the respondents, ranging from 95.2% (n=381) for hand washing to 78.5% (n=314) for reheating food. When presented with a list of options of unsafe and safe foods to eat, 93.5% (n=374) of the respondents identified the correct response. Similarly, when presented with a list of safe and unsafe fish to eat during pregnancy, 74% (n=296) of the women answered correctly.
Demographic variation in nutrition knowledge
Descriptive statistics
From a univariate analysis, the women who scored highest in a number of knowledge domains and in the overall knowledge score were in their first trimester (μ=48.80, standard deviation [SD] =4.71, P<0.001), had one child (μ=46.21, SD =6.70, P<0.001), had planned their pregnancy (μ=46.21 vs μ=41.60, P<0.000), had higher education (μ=48.14, SD =6.34, P<0.000), identified English as their first language (μ=46.20 vs μ=41.18, P<0.000), were married/de facto (μ=45.73, SD =7.43, P<0.001), aged 30–39 years (μ=47.05, SD =6.75, P<0.000), and had annual household incomes of ≥AU$50,000 (μ=47.67, SD =6.56, P<0.000).
The respondents with a health/nutrition-related qualification had significantly greater levels of overall nutrition knowledge (μ=48.60 vs μ=44.69, P<0.000). Of 67 respondents, only 58 provided their qualification details. These included 22 with allied health qualifications, including one with a master degree in exercise rehabilitation and nutrition and dietetics; 17 nurses and one midwife; two participants with medical degrees; two dentists; two with a health degree/Bachelor of Arts; two with a public health degree; one immunologist; and one veterinarian. Of the remaining eight participants, one had a certificate in children’s services, one had a first aid certificate, one had a food safety certificate, one had certificates III and IV in fitness, one had studied a subject on ecotrophology, one was a food technology teacher, one was a pastry chef, and one was a chef by trade.
There was no significant difference in the respondents’ knowledge in most of the domains (seven out of eight) between women who accessed a dietitian and/or nutritionist and those who had not. The latter respondents scored higher only in the “choosing everyday foods” domain (μ=1.80 vs μ=1.58, P<0.002). The reasons for seeing a nutritionist/dietitian varied, including gestational diabetes management (54.9%, n=67), weight management (18.8%, n=23), dietary management during pregnancy (4.9%, n=6), or other reasons (general health and well-being, gallstones, low iron, irritable bowel syndrome, lactose intolerance, acne control, bad eating, and dietary management for teenager; 19.6%, n=24). The respondents indicated that they had seen a dietitian and/or nutritionist either within the last month (26.23%, n=32/122) or from between 1 and 6 months (27.05%, n=33/122) or >6 months (46.72%, n=57/122) from the time they completed the survey. Further analysis revealed that the respondents who had access to a nutritionist/dietitian for managing their gestational diabetes were the only group that scored significantly lower than the other groups in “recommended intakes for the five food groups” (μ=2.07, SD =0.95, P<0.001), “food choices” (μ=1.34, SD =0.72, P<0.000), and on their total score of nutrition knowledge (μ=42.54, SD =7.33, P<0.013). There was not any statistically significant difference between the respondents according to their BMI categories.
Multivariate analysis
Multiple linear regression analysis was undertaken to confirm the independent relationships between demographic factors and respondents’ knowledge of nutrition in pregnancy (Table 6). Only the significant factors from the univariate analysis were included in the final model. The independent factors significantly associated with better nutrition knowledge scores (at the 0.05 level) were as follows: highest household income category (≥AU$50,000; β=0.214, P<0.000), highest education category (tertiary and higher; β=0.225, P<0.000), English as mother’s first language (β=−0.216, P<0.000), age (β=0.154, P<0.001), first trimester for pregnancy (β=−0.101, P<0.016), having a health/nutrition-related qualification (β=−0.099, P<0.020), and having one child (β=−0.096, P<0.028).
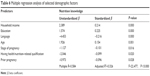  | Table 6 Multiple regression analysis of selected demographic factors |
The model indicates that independent variables explain 32% (adjusted R2) of the variance found between respondents’ knowledge scores (Table 6). The highest category of education and household income were correlated with better nutrition knowledge. Women who indicated that English was their first language, had one child, and held a health/nutrition-related qualification had a greater level of nutrition knowledge. However, nutrition knowledge was lower among women who were in the third trimester of pregnancy and fell within the younger age group.
Discussion
To our knowledge, this is the first study to conduct an in-depth investigation into Australian pregnant women’s pregnancy-specific nutrition knowledge of the AGHE and other relevant dietary and nutritional recommendations for maintaining a healthy pregnancy. The findings of this study indicate a lack of knowledge among pregnant women in most of the nutrition knowledge areas, such as the AGHE recommendations and basic messages of eating more fruit and vegetables as well as bread and cereals but less meat. The pregnant women also held misconceptions in a range of areas, including standard serving sizes, nutrient content (salt, dietary fiber, saturated fat, and vitamin A) of certain foods, energy density of fat, and the importance of key nutrients in pregnancy. The pregnant women who had a lower education level, had a lower income, were in a younger age group, were in the third trimester of pregnancy, had more than one child, and had English as their second language were least knowledgeable. Although knowledge alone is not sufficient to make changes in the dietary behavior, it can be a key factor to initiate such changes.
For this study, the survey questions on the recommended serves of fruit/vegetables (4/5–6 serves/d), bread/cereal (4–6 serves/d), meat and its alternatives (1.5 serves/d), and dairy (2 serves/d) reflected the AGHE for pregnant women at the time of implementing the survey. The updated AGHE recommends 2/5 serves/d for fruit/vegetables, 8.5 serves/d for bread/cereals, 3.5 serves/d for meat and its alternatives food group, and 2.5 serves/d for dairy foods. The other key change in the 2013 AGHE was to the standard serving sizes for bread/cereals, which were approximately halved. As the data collection of the current study commenced prior to the release of the updated AGHE, the results of this study report on the pregnant women’s knowledge of the earlier AGHE. However, as the levels of knowledge were found to be low (only 34.8% of women were familiar with the AGHE), the subsequent changes to the AGHE for pregnant women are likely to result in even lower levels of knowledge of current dietary recommendations for a healthy pregnancy, at least initially.
Knowledge is one of many factors required to change a person’s behavior,14 and maternal nutrition knowledge is significantly associated with the nature of the maternal diet.18 In this study, the pregnant women showed high level of knowledge about the issues related to food safety, “diet–health relationship”, and “nutrients sources” and deficit level of knowledge on topics including “choosing everyday food”, “recommended daily intakes of five food groups”, “serving size”, “supplements during pregnancy”, and “importance of key nutrients in pregnancy”. Even when the knowledge of the daily recommended intakes of certain food groups (dairy, for example) was averaged (56.5% had the correct answer), understanding of the standard serve size details within these groups was quite low (cheese, 35% and yoghurt, 10%). These findings are in line with the earlier Australian studies that explored knowledge of recommended dietary practice in pregnancy8,41 and more generally within a community sample.35 The low awareness of the dietary guidelines (recommended daily intakes of core food groups and standard serving sizes) is of concern. This may hinder pregnant women’s ability to consume a balanced diet in recommended amounts of core food groups, resulting in their having poor dietary intakes.
High consumption of salt, sugar, and fat, and insufficient intake of fiber by pregnant women have been reported in a number of Australian studies.7,33,42 In this study, a high proportion of the pregnant women were unaware of the energy density of fat (78%), the type of foods low or high in fat (86%), and the salt content of bread (87%). This may indicate that pregnant women’s poor knowledge of some common aspects of nutrition may result in suboptimal diets. The greater availability of energy-dense, nutrient-poor products43 further increases the importance of educating women regarding the foods with high-energy density, high fat, and salt.
There was variation in the women’s knowledge of the importance of omega-3 and iodine and their recognition of the need for supplementing with folic acid and iodine. They also varied in their ability to identify foods containing high levels of key nutrients (namely, omega-3 fatty acids, iron, vitamin A, and iodine). In Australia, the NHMRC recommends supplementation with folic acid and iodine during pregnancy.26 Consistent with other studies,29,30 most of the women (90%) in this study were aware of the need for folic acid supplementation, but less than half (48.3%) were aware of the recommendation for iodine supplementation. The recommendation for supplementing with iodine was only introduced in 2010 as opposed to 1992 for folic acid,44 which may explain the difference in awareness. This low level of knowledge of the need for iodine supplementation may result from health care professionals not discussing iodine supplementation with pregnant women, perhaps reflecting their own poor levels of knowledge.30,45 Maternal health care professionals should be supported and encouraged to provide such information to pregnant women, particularly as studies have shown that pregnant women expect nutrition information from their health care professionals.33,46
Fish contains important nutrients like omega-3 fatty acids, which are important for the development of a fetus’s brain, eyes, and nervous system.47,48 For pregnant women, it is recommended to consume two to three serves (1 serve =50 g) per week of any fish and seafood, excluding any large and predatory fish that may contain high levels of mercury.49 In this study, a majority of women were aware of the safest fish type and sources of omega-3 fatty acids; however, they had poor knowledge of their importance during pregnancy. Earlier national and international studies have reported a similar lack of knowledge on the importance of omega-3 fatty acids for women during pregnancy.31,50 Although health care professionals’ advice and accessible resources played a vital role in women’s decision about fish consumption during pregnancy,50 studies have reported a shortage of available education resources and lack of communication between health care professionals and pregnant women about omega-3 fatty acids and their importance during pregnancy.31,50,51 Improved strategies to increase awareness of such information among pregnant women are required.
The low level of knowledge relating to food that is a rich source of vitamin A (liver) is concerning, especially during pregnancy. Although liver is a rich source of key nutrients such as iron and folate, avoiding it in pregnancy is recommended as it contains a high level of vitamin A and the upper safer limit is uncertain.52 A high dose of vitamin A in pregnancy poses a serious risk of birth defects.53 Although our study did not provide information on how this low awareness of vitamin A-rich source food could affect pregnant women’s food choices, written comments (open text sections of the survey) in the present study indicated that some women may be influenced by some of nonevidence-based information. For example, a few women added comments that were in favor of the “Paleo diet”, and they thought it the healthiest dietary pattern they could follow. This may reflect the influence of contemporary popular media (including social media), which contains many articles advertising and promoting nonevidence-based dietary practices such as the “Paleo diet” that may encourage pregnant women to consume organ meat such as liver.54 Adopting such a diet could put women’s and their babies’ health at risk. Women are more likely to change their diet if they believe it benefits their baby.55 However, it is important that pregnant women’s nutrition and dietary knowledge is evidence based.
Developing evidence-based dietary guidelines provides a foundation for promoting healthy eating, but it is important to ensure that the target audiences become knowledgeable about them in order to achieve beneficial results. The results of this study indicate that important information about the AGHE for pregnancy and other key public health nutrition messages need to be made more available to women. This could be achieved by using mass media that provides several powerful avenues for such communication.24 In addition, health professionals may be considered an important avenue for communication of evidence-based dietary guidelines. They have regular contact with pregnant women, are considered as trusted and preferred sources of information,16 and women gain more support when health professionals emphasize educational resources.46,56 However, practitioners have been found to have low level of nutrition knowledge45 and may not be equipped to assist their patients. How best to support health professionals to become effective nutrition educators would be a valuable area of further research.
In line with other studies on general populations35 and pregnant women,8 this study found that pregnant women’s nutrition knowledge was positively associated with age, household income, and education level. Nutrition knowledge has been reported to be positively associated with pregnant women’s self-reported dietary behavior.17,18 Other studies and reports suggest that a lack of nutrition knowledge may reflect a social gradient, with poor nutrition knowledge linked with lower diet quality and thus to poorer health outcomes.8,57 Nutrition education is needed to target those in high-risk groups.
In this study, latter trimesters in pregnancy were found to be negatively associated with the maternal nutrition knowledge score, with the pregnant women in their first trimester having the highest levels of knowledge. Recent studies in Australia have shown that women’s interest in receiving nutrition information is highest in early pregnancy.33,41 Thus, the provision of timely, evidence-based nutritional education for women during pregnancy might be of benefit, especially at the very early stage of pregnancy when critical fetal development is occurring. Ongoing nutrition education throughout the pregnancy may also be warranted, given the lower nutrition knowledge scores of women who are more advanced in their pregnancy and who may be particularly vulnerable to unwelcome weight gain. The observed relationship between lower nutrition knowledge of women with gestation diabetes who had seen a dietitian/nutritionist is new and needs additional exploration. This finding may suggest that individual dietary counseling for these women may focus more on carbohydrate counts and glycemic control, which may differ from the general dietary advice for healthy pregnant women. These disparities were not assessed in this study.
Limitation and strength
The limitations of this study should be noted. The results of this study cannot be generalized due to the nonrepresentative nature of the convenience, cross-sectional sample obtained mostly from NSW, Australia. Language may have been a barrier that excluded non-English-speaking women who may be at higher risk of low knowledge compared to English-speaking women. Categorizing the demographic questions limits the ability to compare the current study sample’s demographic characteristics to the state and national profiles. The strength of our research is that the results provide valuable insights into the level of understanding of maternal-related nutrition information in a large sample of Australian pregnant women that can be used to inform interventions for this group.
If pregnant women are to be better informed of the nutritional needs and practices required for the health of themselves and their children, studies investigating the sources of information and forms of support preferred by pregnant women need to be undertaken. This would provide important information for the development of effective education programs for pregnant women to establish and motivate positive dietary behavior change.
Conclusion
The findings of this study indicate a lack of knowledge among pregnant women in most of the nutrition knowledge areas. Although knowledge alone cannot ensure dietary behavioral changes, it can be a key factor in the initiation of such changes. The establishment of official dietary guidance is not sufficient to ensure that women are equipped with the knowledge necessary to optimize their diets for the health of themselves and their unborn babies. Health care providers have an important role in promoting knowledge of healthy eating for pregnant women.
Acknowledgments
The authors wish to acknowledge the Saudi Arabian Higher Education Ministry for PhD scholarship funding; the South East Sydney and Illawarra Area Health Services, South Western Sydney Local Health District sites, and midwives who assisted with the recruitment of the respondents; all pregnant women who participated in this study; Associate Professor Marijka Batterham for statistical advice; Doctor Joanna Russell for her comments on the primary data analysis stage; Doctor Alexis St George for constructive comments on earlier drafts of this manuscript; Ms Elaine Newby who assisted in the editing of this article; and Doctor Gilly Hendrie for her cooperation and great readiness to help. The abstract of this article with interim findings was presented at the 30th ICM Triennial Congress – Midwives58 and at the Australian College of Midwives Biennial Conference.59 The current article includes work based on the PhD thesis submitted by the main author, Khlood Bookari, and parts of it have been published.17,60
Author contributions
K Bookari is the main author and is responsible for designing study survey, collecting and analyzing data, writing the initial manuscript, and revisions. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Renault KM, Carlsen EM, Nørgaard K, et al. Intake of sweets, snacks and soft drinks predicts weight gain in obese pregnant women: detailed analysis of the results of a randomised controlled trial. PLoS One. 2015;10(7):e0133041. | ||
Callaway L, Prins J, Chang A, McIntyre H. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Aust. 2006;184(2):56–59. | ||
Catalano PM, Ehrenberg HM. The short- and long-term implications of maternal obesity on the mother and her offspring. BJOG. 2006;113(10):1126–1133. | ||
Institute of Medicine (IOM). Weight Gain during Pregnancy: Reexamining the Guidelines. Washington, DC: The National Academies Press; 2009. | ||
Hure A, Young A, Smith R, Collins C. Diet and pregnancy status in Australian women. Public Health Nutr. 2009;12(06):853–861. | ||
Morton SM, Grant CC, Wall CR, et al. Adherence to nutritional guidelines in pregnancy: evidence from the growing up in New Zealand birth cohort study. Public Health Nutr. 2014;17(09):1919–1929. | ||
Wen LM, Flood VM, Simpson JM, Rissel C, Baur LA. Dietary behaviours during pregnancy: findings from first-time mothers in southwest Sydney, Australia. Int J Behav Nutr Phys Act. 2010;7(1):13. | ||
McLeod ER, Campbell KJ, Hesketh KD. Nutrition knowledge: a mediator between socioeconomic position and diet quality in Australian first-time mothers. J Am Diet Assoc. 2011;111(5):696–704. | ||
Blumfield M, Hure A, MacDonald-Wicks L, Patterson A, Smith R, Collins C. Disparities exist between national food group recommendations and the dietary intakes of women. BMC Womens Health. 2011;11(1):37. | ||
Malek L, Umberger W, Makrides M, Zhou JS. Adherence to the Australian dietary guidelines during pregnancy: evidence from a national study. Public Health Nutr. 2016;19(7):1155–1163. | ||
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. | ||
Bandura A. A social cognitive theory: an agentic perspective. Asian J Soc Psychol. 1999;2:21–41. | ||
Prochaska JO, Velicer WF. The transtheoretical model of health behaviour change. Am J Health Promot. 1997;12(1):38–48. | ||
Sapp G. Incomplete knowledge and attitude-behavior inconsistency. Soc Behav Pers. 2002;30(1):37. | ||
Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202(2):135.e131–135.e138. | ||
Szwajcer EM, Hiddink GJ, Koelen MA, van Woerkum CMJ. Nutrition-related information-seeking behaviours before and throughout the course of pregnancy: consequences for nutrition communication. Eur J Clin Nutr. 2005;59(S1):S57–S65. | ||
Bookari K, Yeatman H, Williamson M [webpage on the Internet]. Falling short of dietary guidelines – what do Australian pregnant women really know? A cross sectional study. Women Birth. 2016. Available from: http://www.sciencedirect.com/science/article/pii/S187151921630049X. Accessed June 16, 2016. | ||
Williams L, Campbell K, Abbott G, Crawford D, Ball K. Is maternal nutrition knowledge more strongly associated with the diets of mothers or their school-aged children? Public Health Nutr. 2012;15(08):1396–1401. | ||
Popa AD, Niţă O, Graur LI, et al. Nutritional knowledge as a determinant of vitamin and mineral supplementation during pregnancy. BMC Public Health. 2013;13:1105. | ||
Hui A, Back L, Ludwig S, et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomised controlled trial. BJOG. 2012;119(1):70–77. | ||
Dodd JM, Cramp C, Sui Z, et al. The effects of antenatal dietary and lifestyle advice for women who are overweight or obese on maternal diet and physical activity: the limit randomised trial. BMC Med. 2014;12:161. | ||
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans. Washington, DC: U.S. Government Printing Office; 2010. | ||
European Food Information Council [webpage on the Internet]. Food-Based Dietary Guidelines in Europe; 2009. Available from: http://www.eufic.org/article/en/expid/food-based-dietary-guidelines-in-europe/. Accessed April 15, 2014. | ||
National Health & Medical Research Council. Eat for Health – Dietary Guidelines for Australians: A Guide to Healthy Eating. Canberra, ACT: Commonwealth of Australia; 2013. | ||
National Health and Medical Research Council. Eat for Health: Healthy Eating When You’re Pregnant or Breastfeeding. Canberra, ACT: Commonwealth of Australia; 2013. | ||
National Health and Medical Research Council. Healthy Eating during Your Pregnancy: Advice on Eating for You and Your Baby. Canberra, ACT: Commonwealth of Australia; 2013. | ||
Australian Health Ministers’ Advisory Council. Clinical Practice Guidelines: Antenatal Care – Module 1. Canberra, ACT: Australian Government Department of Health and Ageing; 2012. | ||
Australian Health Ministers’ Advisory Council. Clinical Practice Guidelines: Antenatal Care – Module 2. Canberra, ACT: Australian Government Department of Health and Ageing; 2014. | ||
El-mani S, Charlton KE, Flood VM, Mullan J. Limited knowledge about folic acid and iodine nutrition in pregnant women reflected in supplementation practices. Nutr Diet. 2014;71(4):236–244. | ||
Lucas CJ, Charlton KE, Brown L, Brock E, Cummins L. Antenatal shared care: are pregnant women being adequately informed about iodine and nutritional supplementation? Aust N Z J Obstet Gynaecol. 2014;54(6):515–521. | ||
Sinikovic DS, Yeatman HR, Cameron D, Meyer BJ. Women’s awareness of the importance of long-chain omega-3 polyunsaturated fatty acid consumption during pregnancy: knowledge of risks, benefits and information accessibility. Public Health Nutr. 2009;12(04):562–569. | ||
Bondarianzadeh D, Yeatman H, Condon-Paoloni D. Listeria education in pregnancy: lost opportunity for health professionals. Aust N Z J Public Health. 2007;31(5):468–474. | ||
Wilkinson SA, Tolcher D. Nutrition and maternal health: what women want and can we provide it? Nutr Diet. 2010;67(1):18–25. | ||
Skouteris H, McPhie S, Hill B, et al. Health coaching to prevent excessive gestational weight gain: a randomized-controlled trial. Br J Health Psychol. 2016;21(1):31–51. | ||
Hendrie GA, Coveney J, Cox D. Exploring nutrition knowledge and the demographic variation in knowledge levels in an Australian community sample. Public Health Nutr. 2008;11(12):1365–1371. | ||
Worsley A, Wang WC, Byrne S, Yeatman H. Different patterns of Australian adults’ knowledge of foods and nutrients related to metabolic disease risk. J Nutr Sci. 2014;3:e14. | ||
Hoerr SL, Horodynski MA, Lee S-Y, Henry M. Predictors of nutritional adequacy in mother–toddler dyads from rural families with limited incomes. J Am Diet Assoc. 2006;106(11):1766–1773. | ||
Colton D, Covert RW. Designing and Constructing Instruments for Social Research and Evaluation. 1st ed. San Francisco, CA: Jossey-Bass; 2007. | ||
WHO. Global Database on Body Mass Index: BMI Classification. Geneva: World Health Organisation; 2006. | ||
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson Education; 2013. | ||
de Jersey S, Nicholson J, Callaway L, Daniels L. An observational study of nutrition and physical activity behaviours, knowledge, and advice in pregnancy. BMC Pregnancy Childbirth. 2013;13(1):115. | ||
De Jersey SJ, Ross LJ, Himstedt K, McIntyre HD, Callaway LK; for the BSG. Weight gain and nutritional intake in obese pregnant women: some clues for intervention. Nutr Diet. 2011;68(1):53–59. | ||
Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–679. | ||
National Health Medical Research Council. Revised statement on the relationship between dietary folic acid and neural tube defects such as spina bifida. J Paediatr Child Health. 1994;30(6):476–477. | ||
Arrish J, Yeatman H, Williamson M [webpage on the Internet]. Australian midwives and provision of nutrition education during pregnancy: a cross sectional survey of nutrition knowledge, attitudes, and confidence. Women Birth. Available from: http://dx.doi.org/10.1016/j.wombi.2016.03.001. Accessed March 27, 2016. | ||
Szwajcer EM, Hiddink GJ, Koelen MA, van Woerkum CMJ. Written nutrition communication in midwifery practice: what purpose does it serve? Midwifery. 2009;25(5):509–517. | ||
Hibbeln JR, Davis JM, Steer C, et al. Maternal seafood consumption in pregnancy and neurodevelopmental outcomes in childhood (alspac study): an observational cohort study. Lancet. 2007;369(9561):578–585. | ||
Al MD, van Houwelingen AC, Hornstra G. Long-chain polyunsaturated fatty acids, pregnancy, and pregnancy outcome. Am J Clin Nutr. 2000;71(1 suppl):285s–291s. | ||
NSW Food Authority. Pregnancy and Food Safety. Taree, NSW: NSW Food Authority; 2014. | ||
Bloomingdale A, Guthrie LB, Price S, et al. A qualitative study of fish consumption during pregnancy. Am J Clin Nutr. 2010;92(5):1234–1240. | ||
Emmett R, Akkersdyk S, Yeatman H, Meyer BJ. Expanding awareness of docosahexaenoic acid during pregnancy. Nutrients. 2013;5(4):1098–1109. | ||
The Department of Health & Human Services [webpage on the Internet]. Pregnancy and diet; 2014. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-and-diet. Accessed July 8, 2016. | ||
Véronique A-B, Gérard P. Vitamin a in pregnancy: requirements and safety limits. Am J Clin Nutr. 2000;71(5 suppl):1325s–1333s. | ||
Noël S [webpage on the Internet]. A paleo guide to pregnancy. Available from: http://paleoleap.com/paleo-guide-to-pregnancy/. Accessed March 30, 2016. | ||
Troxell H, Anderson J, Auld G, et al. Omega-3 for baby and me: material development for a WIC intervention to increase DHA intake during pregnancy. Matern Child Health J. 2005;9(2):189–197. | ||
Stapleton H, Kirkham M, Thomas G. Qualitative study of evidence based leaflets in maternity care. BMJ. 2002;324(7338):639. | ||
Queensland Health. The Social Determinants of Health Support Package: Nutrition – Fact Sheet. Brisbane, QLD: Queensland Health; 2003. | ||
Bookari K, Yeatman H, Williamson M. Nutrition during pregnancy – exploring women’s knowledge and models of nutrition communication. Paper presented at: ICM 30th Triennial Congress – Midwives; 1–5 June 2014; Prague, Czech Republic. | ||
Bookari K, Yeatman H, Williamson M. Exploring pregnant women’s current level of nutrition knowledge, attitudes, and readiness for dietary change during pregnancy. Women Birth. 2013;26(suppl 1):S23. | ||
Bookari K, Yeatman H, Williamson M. Australian pregnant women’s awareness of gestational weight gain and dietary guidelines: opportunity for action. J Pregnancy. 2016;2016:9. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




