Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 8
A randomized, double-blind, placebo-, and positive-controlled clinical pilot study to evaluate the efficacy and tolerability of standardized aqueous extracts of Terminalia chebula and Terminalia bellerica in subjects with hyperuricemia
Authors Usharani P , Nutalapati C , Pokuri V, Kumar U, Taduri G
Received 13 November 2015
Accepted for publication 3 March 2016
Published 22 June 2016 Volume 2016:8 Pages 51—59
DOI https://doi.org/10.2147/CPAA.S100521
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Arthur E. Frankel
Pingali Usharani,1 Chandrasekhar Nutalapati,1 Venkata Kishan Pokuri,1 Chiranjeevi Uday Kumar,1 Gangadhar Taduri,2
1Department of Clinical Pharmacology and Therapeutics, 2Department of Nephrology, Nizam's Institute of Medical Sciences, Panjagutta, Hyderabad, India
Objectives: To evaluate the efficacy and tolerability of standardized aqueous extracts of Terminalia chebula and Terminalia bellerica versus febuxostat and placebo on reduction in serum uric acid levels in subjects with hyperuricemia.
Materials and methods: A total of 110 eligible subjects with hyperuricemia were enrolled and randomized to either of the five treatment groups – T. chebula 500 mg twice a day (BID), T. bellerica 250 mg BID, T. bellerica 500 mg BID, placebo BID, and febuxostat 40 mg once daily plus an identical placebo – for a duration of 24 weeks. Serum uric acid levels were measured at baseline and at the end of 4, 8, 12, 16, 20, and 24 weeks. Statistical analysis was done using GraphPad Prism Software 4.
Results and interpretation: All active treatment groups showed a reduction in serum uric acid levels compared to baseline and placebo. Significant reduction in mean serum uric acid levels started as early as 4 weeks following treatment, compared to baseline, with T. bellerica (500 and 250 mg), febuxostat (P<0.001), and T. chebula 500 mg (P<0.01); an increase in serum uric acid levels was seen with placebo (P<0.05). The serum uric acid levels became steady after 16 weeks of treatment and remained the same until the end of 24 weeks. The reduction of serum uric acid levels in the T. bellerica 500 mg group was nearly twice that of the T. chebula 500 mg group as well as T. bellerica 250 mg group at all time points. T. bellerica 500 mg reduced serum uric acid levels from 8.07±0.87 to 5.78±0.25 compared to febuxostat, which reduced serum uric acid levels from 8.53±0.97 to 4.28±0.67 (P<0.001) at the end of 24 weeks. The efficacy of T. bellerica appeared to be dose dependent. All the formulations were well tolerated.
Conclusion: T. bellerica has the potential for treating hyperuricemia as it was devoid of any serious adverse effects in the present study. Further studies are needed to confirm this potential.
Keywords: hyperuricemia, febuxostat, Terminalia chebula, Terminalia bellerica
Introduction
Asymptomatic hyperuricemia is common and is found in about 5%–8% of adult males. A serum uric acid level more than 10 mg/dl may cause progression of hyperuricemia and lead to symptoms of gout.1 Hyperuricemia affects patient survival by inducing or aggravating cardiovascular disease (CVD) and is also a risk factor for renal disease progression. The increase in uric acid levels may reflect tissue hypoxia or increased oxygen free radical formation.1 Most studies have linked hyperuricemia to poor clinical outcomes due to its marked association with CVD and renal disease.2,3 A recent increase in the prevalence and incidence of hyperuricemia might be explained by similar increases in adverse lifestyle habits such as consumption of purine-rich diets and excess alcohol. Other important factors include obesity, increasing diuretic use, and the increasing aging population.4
Purines (adenine and guanine) and pyrimidines (cytosine, thymine, uracil) play fundamental roles in the replication of genetic material, gene transcription, protein synthesis, and cellular metabolism. Abnormalities of nucleotide metabolism include relatively common diseases such as hyperuricemia and gout, where there is an increased production or diminished excretion of the metabolic end product of purine metabolism (uric acid), to rare enzyme deficiencies that affect purine and pyrimidine synthesis or degradation. The knowledge of these biochemical pathways has led, in some instances, to the development of specific forms of treatment such as the use of allopurinol, and, recently, xanthine oxidase (XO)-inhibitor febuxostat to reduce uric acid production.5,6
As the global scenario is now changing toward the use of plant products having a traditional medicinal use, various effects of compounds isolated from plants should be explored for the treatment of different types of diseases. Terminalia chebula7 and T. bellerica have a wide spectrum of pharmacological and medicinal activities.8 Although they have a number of pharmacological activities due to the presence of various types of bioactive compounds, particularly on inflammatory conditions like arthritis and gout, the possible mechanism of anti-inflammatory action could be due to inhibition of inducible nitric oxide synthase.9 T. bellerica and T. chebula, along with other exotic species, have reportedly shown effect against renal pathologies.10 The antioxidant property of T. bellerica and T. chebula has been demonstrated in several studies,11 and the probable mechanism of action of the antioxidant property is inhibition of XO,12 an enzyme involved in the synthesis of uric acid, which could explain the hypouricemic effect of these compounds. In vitro XO inhibitory activity of T. chebula, T. bellerica, and allopurinol was determined (Natreon, Inc., New Brunswick, NJ, USA),28 and it was found that both the test products were as efficacious as allopurinol in inhibiting XO activity (data from file). Thus, the current study was planned to evaluate the effect of T. chebula, T. bellerica versus febuxostat and placebo on serum uric acid levels in patients with hyperuricemia.
Objectives
The primary objective was to compare the efficacy of T. chebula and T.bellerica versus febuxostat and placebo in terms of reduction in serum uric acid levels in patients with hyperuricemia, whereas the secondary objective was to evaluate the safety and tolerability of the treatments.
Materials and methods
Study design
The study was a prospective, randomized, double-blinded, placebo-controlled pilot study conducted in the Department of Clinical Pharmacology and Therapeutics, Nizam’s Institute of Medical Sciences (NIMS), between June 2014 and March 2015. A total of 110 patients were enrolled to receive the study treatment in a randomized manner. The study was approved by the NIMS Ethics Committee, and all the subjects gave written informed consent prior to their participation in the study. The study was registered with Clinical Trials Registry-India (CTRI) and the registration number is Ref/2014/09/007548.
Subjects of either sex with hyperuricemia, aged between 18 and 69 years, with serum uric acid level ≥6.0 and ≤12.0 mg/dL, and who were not on any hypouricemic agents, subjects who were willing to comply with the requirements of the study, and subjects who were willing to give voluntary written informed consent were enrolled in the study. Patients with a gout flare during screening or baseline visit, patients currently using aspirin or other nonsteroidal anti-inflammatory drugs, diuretics, other medications with known urate-lowering effects, patients with history or presence of nephrolithiasis or uncontrolled hypertension or diabetes, hepatic and renal impairment, pregnant or lactating females, or those with secondary hyperuricemia (eg, due to myeloproliferative disorder or organ transplant) were excluded.
The sample size calculation was based on the assumption that there will be a mean decrease of 2 mg/dL of serum uric acid from baseline to the end of treatment. A sample size of 88 evaluable cases would provide an 80% power to estimate the reduction in serum uric acid at 5% level of significance at the end of the study. Anticipating 20% dropout rates, 110 subjects were enrolled to get 88 evaluable cases at the end of the study.
After screening, all the eligible subjects were randomized to either of the five treatment groups in a double-blinded fashion for a duration of 24 weeks. Computer-generated randomization was used. The subjects in Group A and Group B received one capsule of T. chebula and T. bellerica 500 mg, respectively, orally twice a day (BID) after food. Group C subjects were given one capsule of T. bellerica 250 mg orally BID after food. The subjects in Group D were given one tablet of febuxostat 40 mg (encapsulated in a capsule identical in size and color to that of other test products) orally in the morning after food and an identical placebo capsule in the evening after food. Finally, Group E subjects received one placebo capsule each orally BID after food.
Study medications
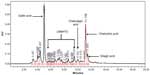
T. chebula (AyuFlex®; Natreon, Inc.) capsule is an aqueous extract of the edible fruit of T. chebula containing not less than 39% of chebulinic acid + chebulagic acid + other low-molecular-weight hydrolysable tannins and is highly standardized by high-performance liquid chromatography (HPLC). HPLC chromatogram of this extract is shown in Figure 1.
T. bellerica (Ayuric®, Natreon, Inc) capsule is an aqueous extract of the edible fruit of T. bellerica containing not less than 15% of chebulinic acid + chebulagic acid + other low-molecular-weight hydrolysable tannins and is highly standardized by HPLC. HPLC chromatogram of this extract is shown in Figure 2.
A Waters HPLC 2695 with PDA Detector (Waters™ 2996, Photodiode Array Detector; Waters Corporation, Milford, MA, USA) was used for HPLC analysis of T. chebula and T. bellerica, and Empower software was used for data evaluation. The column used for analysis was a reverse phase LiChrosorb® RP-18 (Particle size 5 μm, 4×250 mm) column, Merck KGaA, Darmstadt, Germany, with a reverse phase guard column.
According to the Ayurvedic Pharmacopoeia of India, the prescribed dose for T. chebula and T. bellerica is 3–6 g. As very few clinical data are available on these two products, a dose range between 500 and 1,000 mg/d was taken for this study. These are very commonly used Ayurvedic medicines in India and are one of the components of a very popular product on the market, called Triphala.
The study included only patients with asymptomatic hyperuricemia and not those with gout. In case of appearance of symptoms of gout in any of the groups, a tablet of ibuprofen 400 mg was planned as a rescue medication.
Subjects were asked to report for follow-up visits at 4, 8, 12, 16, 20, and 24 weeks of therapy. At each visit, efficacy and safety were evaluated. Serum uric acid levels were measured at baseline and at the end of 4, 8, 12, 16, 20, and 24 weeks. Lab investigations to assess safety by analyzing hematological, hepatic, and renal biochemical parameters were done at baseline, at the end of 24 weeks therapy, and also as and when required (in case of any adverse drug reaction). Subjects were asked about the presence of adverse drug reactions, and the same was recorded in the case report form. Compliance to therapy was assessed by pill count method.
Outcome measures
The primary outcome measures were the absolute and mean percentage reduction in serum uric acid levels from baseline to the end of 24 weeks of treatment. Secondary outcome measures were the percentage of patients whose serum uric acid levels decreased to ≤6.0 mg/dL following treatment at the end of 24 weeks and tolerability, which was assessed at the end of 24 weeks as good – no serious side effects, fair – mild-to-moderate side effects, poor – severe side effects, and withdrawal of therapy.
Statistical analysis
The data were presented as mean ± standard deviation. Primary outcome measures were analyzed as the absolute change and mean percentage change in serum uric acid levels from baseline to 4, 8, 12, 16, 20, and 24 weeks of treatment. Secondary outcome measures were analyzed as the proportion of patients who achieved a target serum uric acid level (≤6 mg/dL) in each group at the end of 24 weeks of treatment. Paired t-test was used to compare the mean change from baseline to posttreatment (4, 8, 12, 16, 20, and 24 weeks of treatment) within group, while analysis of variance was used for between-group comparisons. All statistical analyses were performed using the GraphPad Prism Software 4 (GraphPad Software Inc., San Diego, CA, USA).
Results
A total of 110 eligible subjects were enrolled in the study, and 88 completed 24 weeks of treatment. Twenty-two subjects were lost to follow-up during the course of the study. Finally, 18 subjects in the T. chebula 500 mg group, 18 subjects in the T. bellerica 500 mg group, 17 subjects in the T. bellerica 250 mg group, 18 subjects in the febuxostat 40 mg group, and 17 subjects in the placebo group completed 24 weeks of treatment.
The demographic characteristics of all the five study groups are shown in Table 1. There were no significant differences between treatment groups in baseline characteristics including age, weight, and body mass index, indicating a homogeneous population.
  | Table 1 Demographic data |
The absolute change and the mean percentage reduction among the treatment groups at the end of 4, 8, 12, 16, and 20 weeks of treatment are shown in Table 2.
At the end of 4 weeks of treatment, when the absolute change in serum uric acid levels was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), and febuxostat (D) versus placebo (E), with a P-value <0.001. Similarly, when the mean percentage reduction in serum uric acid levels was compared, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), and febuxostat (D) versus placebo (E) with a P-value <0.001.
At the end of 8 weeks of treatment, when the absolute change in serum uric acid levels was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. Similarly, when the mean percentage reduction of serum uric acid levels was compared, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg(B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001.
At the end of 12 weeks of treatment, when the absolute change in serum uric acid levels was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus T. bellerica 250 mg (C), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. Similarly, when the mean percentage reduction of serum uric acid levels was compared, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001.
At the end of 16 weeks of treatment, when the absolute change in serum uric acid levels was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus T. bellerica 250 mg (C), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. Similarly, when the mean percentage reduction of serum uric acid levels was compared, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus T. bellerica 250 mg (C), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001.
At the end of 20 of weeks treatment, when the absolute change in serum uric acid levels was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg(B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. Similarly, when the mean percentage reduction of serum uric acid levels was compared, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001.
Serum uric acid levels at the end of 24 weeks of treatment
There was highly significant reduction in mean serum uric acid levels after 24 weeks of treatment compared to baseline in all the four active treatment groups, ie, T. chebula 500 mg, T. bellerica 500 mg, T. bellerica 250 mg, and febuxostat 40 mg (P<0.001). However, statistically, a significant increase in mean serum uric acid levels was seen with the placebo group.
When the absolute change in serum uric acid levels at the end of 24 weeks of treatment was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. No statistical significance (P=ns) was observed between T. chebula 500 mg (A) versus T. bellerica 500 mg (B) and T. chebula 500 mg (A) versus T. bellerica 250 mg (C), whereas absolute change in serum uric acid levels was found to be significant (P<0.05) for other group comparisons, as shown in Table 3 and Figure 3.
  | Figure 3 Mean percentage change in serum uric acid levels at the end of 24 weeks. |
When the mean percentage reduction in serum uric acid levels at the end of 24 weeks of treatment was compared among the five treatment groups, it was found to be highly significant for T. chebula 500 mg (A) versus febuxostat (D), T. chebula 500 mg (A) versus placebo (E), T. bellerica 500 mg (B) versus febuxostat (D), T. bellerica 500 mg (B) versus placebo (E), T. bellerica 250 mg (C) versus febuxostat (D), T. bellerica 250 mg (C) versus placebo (E), and febuxostat (D) versus placebo (E), with a P-value <0.001. No statistical significance (P=ns) was observed for T. chebula 500 mg (A) versus T. bellerica 250 mg (C), whereas the mean percentage reduction in serum uric acid levels was found to be significant (P<0.01; P<0.05) for other group comparisons, as shown in Table 3 and Figure 3.
The percentage of subjects who achieved the target serum uric acid level ≤6 mg/dL by the end of 24 weeks of treatment was the secondary outcome measure. All the subjects in the febuxostat group achieved the target serum uric acid level ≤6 mg/dL, whereas 88.8% in T. bellerica 500 mg, 22.2% in T. chebula 500 mg, and 11.76% in T. bellerica 250 mg achieved the target serum uric acid level ≤6 mg/dL, respectively. However, none of the subjects in the placebo group achieved the target serum uric acid level ≤6 mg/dL. Many subjects in the febuxostat group achieved the target serum uric acid levels at the end of 8 weeks of treatment, with a mean serum uric acid level of 6.00±0.57, whereas many patients in the T. bellerica 500 mg group achieved the target serum uric acid levels at the end of 12 weeks of treatment, with a mean serum uric acid level of 6.00±0.63.
All treatments were well tolerated. Two patients in the febuxostat group had mildly elevated total bilirubin, and one patient in the febuxostat group complained of nausea and vomiting. One patient in the T. chebula group had mild gastrointestinal intolerance. None of the patients in the T. bellerica groups had any adverse effect. However, no subject in either group discontinued the study due to adverse events.
Discussion
Reduction and maintenance of serum uric acid levels to <6.0 mg/dL, a range below the limit of solubility of urate in serum, is usually the treatment goal in the management of hyperuricemia.13–15 Urate-lowering pharmacotherapy is a keystone in the management of hyperuricemia. Uricosuric drugs, which enhance renal uric acid excretion, and XO enzyme inhibitors like allopurinol and febuxostat, which reduce uric acid production, are the mainstay of treatment.16 Although allopurinol is well tolerated, it may cause drowsiness, hypersensitivity reaction that may appear after months or years of therapy, toxic epidermal necrolysis, or Steven–Johnson syndrome (rare). Febuxostat can cause liver function abnormalities, nausea, joint pain, and rash. It may also cause myocardial infarction and stroke, but the number of studies available are insufficient to establish a causal relationship between febuxostat therapy and the cardiovascular events.17 So, there is always a pursuit to develop drugs that are highly effective but with fewer or no adverse effects and are also cost-effective.
There is a very long history of use of herbal drugs for the treatment of a plethora of medical conditions. They also form the basis of the origin of much of modern medicine.18 The last few decades has seen an ever-increasing inclination toward the development of drugs from plants having therapeutic qualities. About 25% of all modern medicines are thought to be derived from higher plants. Currently, the major pharmaceutical companies have been demonstrating an interest in investigating higher plants as sources for new structures and also for the development of standardized phytotherapeutic agents with proven efficacy, safety, and quality.19
T. chebula is one of the widely used plants in Ayurvedic medicine. The fruit powder of T. chebula is said to be effective against diseases ranging from digestive problems and coronary disorders to allergic and infectious disease like cough and skin disorders. Aqueous or ethanolic extract of the powder is said to have hepatoprotective, cardioprotective, renoprotective, antioxidative, antidiabetic, anti-inflammatory, analgesic, anticancer, and radioprotective, properties. T. chebula is supposed to have a significant quantity of gallic acid, ellagic acid, tannic acid, β-sitosterol, ethyl gallate, chebulic acid, ascorbic acid, and mannitol, which are responsible for its various pharmacological properties.20,21 In one study, the aqueous extract of T. chebula was shown to inhibit XO activity and was also shown to be an excellent scavenger of DPPH radicals.22 In another study, it has been shown that increased XO activity leads to enhanced superoxide radical production from the liver.23 Superoxide and hydrogen peroxide radicals are generated during the oxidation of hypoxanthine to uric acid. These radicals play a crucial role in cancer and inflammatory conditions. Quercitin,7-neohespiridosylluteolin, 4,7-dimethyl quercitin, and 3-rutinosylkaempferol seem to possess superoxide scavenging activity as well as XO inhibitory capacity. Quercetin is an important compound found in T. chebula. Thus, it helps in reducing the production of uric acid by inhibiting XO.23 T. bellerica is classified as an expectorant in Ayurvedic medicine.24 It also has antidiabetic, anticancer, and antimicrobial properties. The phytosterols, triterpenoids, glycosides, tannins, and phenolic compounds present in it seem to account for its anti-inflammatory, analgesic, antimicrobial, antioxidant, and antitumor properties.25 T. bellerica is an important constituent of Triphala, an Ayurvedic formulation commonly used in India.26 In one study, it was seen that in addition to possessing superoxide radical scavenging activity, it also inhibited uric acid formation, which was indicative of its XO enzyme inhibitory activity. The study described the XO-inhibitory activity of Triphala by the estimation of uric acid formation; uric acid formed was estimated by HPLC, and the results revealed that Triphala not only exhibited superoxide radical scavenging ability, but also had XO enzyme inhibitory activity.27
Conclusion
In our study, all the groups had homogeneous baseline characteristics. Treatment with T. chebula 500 mg, T. bellerica 500 mg, 250 mg, or febuxostat 40 mg for a period of 24 weeks in hyperuricemic subjects has shown a significant reduction in serum uric acid levels when compared to baseline and placebo at 16 weeks at which point it stabilized. T. bellerica 500 mg produced statistically higher reduction in outcome parameters as compared to T. chebula 500 mg, proving to be nearly twice as effective as T. chebula 500 mg as well as T. bellerica 250 mg. However, T. bellerica 500 mg is only about 60% as effective as febuxostat. In addition, the efficacy of T. bellerica appears to be dose dependent.
All the study medications were well tolerated and no serious adverse events were observed, with none of the patients in the T. bellerica groups having any adverse effect, and none of the patients discontinuing the study due to any adverse event. T. bellerica has excellent potential for the treatment for hyperuricemia and gout; however, additional studies are needed to confirm this potential.
Acknowledgment
Capsules of AyuFlex® 500 mg, Ayuric® 250 and 500 mg, febuxostat 40 mg tablets encapsulated in same size and color capsules as the other test products and placebo capsules were all supplied by Natreon, Inc., New Brunswick, NJ, USA. We thank Natreon, Inc., which supplied the test drug and the identical placebo capsules, Dr IV Shravanti, the Ayurvedic physician and Mr N Muralidhar – research associate, for their help during the period of study.
Disclosure
The authors report no conflicts of interest in this work.
References
Busuioc M, Voroneanu L, Hogas S, Covic M, Gusbeth-Tatomir P, Covic A. Pathogenetic impact of hyperuricemia in renal and cardiovascular disease. BANTAO J. 2007;5(1):1. | |
Edwards NL. The role of hyperuricemia and gout in kidney and cardiovascular disease. Cleve Clin J Med. 2008;75(5):S13–S16. | |
Baker JF, Krishnan E, Chen L, Schumacher HR. Serum uric acid and cardiovascular disease:recent developments, and where do they leave us? Am J Med. 2005;118:816–826. | |
Roddy E. Hyperuricemia, gout and lifestyle factors. J Rheumatol. 2008;35:1689–1691. | |
Robert LW. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY:McGraw-Hill; 2011. | |
Becker MA, Schumacher HR, Espinoza LR, et al. The urate-lowering efficacy and safety of febuxostat in the treatment of the hyperuricemia of gout:the CONFIRMS trial. Arthritis Res Ther. 2010;12(2):R63. | |
Bag A, Bhattacharyya SK, Chattopadhyay RR. The development of Terminalia chebula Retz (Combretaceae) in clinical Research. Asian Pac J Trop Biomed. 2013;3(3):244–252. | |
Lobo V, Patil A, Phatak A, Chandra N. Free radicals, antioxidants and functional foods:impact on human health. Pharmacogn Rev. 2010;4(8):118–126. | |
Sekhar S, Ruma K, Ramachandra KK, Siddapura RN, Harischandra SP. Potential anti-inflammatory bioactives from medicinal plants of Western Ghats, India. Pharmacogn Commun. 2012;2(2):2–12. | |
BallabhB, Chaurasia OP, Ahmed Z, Singh SB. Traditional medicinal plants of cold desert Ladakh-used against kidney and urinary disorders. J Ethnopharmacol. 2008;118(2):331–339. | |
Hazra B, Sarkar R, Biswas S, Mandal N. Comparative study of the antioxidant and reactive oxygen species scavenging properties in the extracts of the fruits of Terminalia chebula, Terminalia belerica and Emblica officinalis. BMC Complement Altern Med. 2010;10:20. | |
Sandhya T, Lathika KM, Pandey BN, et al. Protection against radiation oxidative damage in mice by Triphala. Mutat Res. 2006;609(1):17–25. | |
Perez-Ruiz F, Atxotegi J, Hernando I, Calabozo M, Nolla JM. Using serum urate levels to determine the period free of gouty symptoms after withdrawal of long-term urate-lowering therapy:a prospective study. Arthritis Rheum. 2006;55:786–790. | |
Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II:management. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2006;65:1312–1324. | |
Terkeltaub RA. Clinical practice. Gout. N Engl J Med. 2003;349:1647–1655. | |
Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat, a novel nonpurine selective inhibitor of xanthine oxidase:a twenty-eight-day, multicenter, phase II, randomized, double-blind, placebo-controlled, dose-response clinical trial examining safety and efficacy in patients with gout. Arthritis Rheum. 2005;52(3):916–923. | |
Grosser T, Smyth E, Fitzgerald GA. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 12th ed. New York, NY:McGraw-Hill; 2011:997–998. | |
Vickers A, Zollman C, Lee R. Herbal medicine. West J Med. 2001; 175(2):125–128. | |
Calixto JB. Efficacy, safety, quality control, marketing and regulatory guidelines for herbal medicines (phytotherapeutic agents). Braz J Med Biol Res. 2000;33(2):179–189. | |
Khandelwal VKM, Koneri R, Balaraman R, Kandhavelu M. Biological activities of some Indian medicinal plants. J Adv Pharm Educ Res. 2011;1:12–44. | |
Thiruchelvi R, Duraikannu A, Subramanian M, Kandasamy S. Protective effects of Terminalia chebula fruit extract against cadmium-induced nephrotoxicity in rats. Int J Environ Biol. 2012;2(3):108–112. | |
Naik GH, Priyadarsini KI, Naik DB, Gangabhagirathi R, Mohan H. Studies on the aqueous extract of Terminalia chebula as a potent antioxidant and a probable radioprotector. Phytomedicine. 2004;11(6):530–538. | |
Khan KH. The effect of regular intake of Terminalia chebula on oxidative stress in mice originated from Salmonella typhimurium. EurAsia J BioSci. 2009;3:113–121. | |
Saraswathi MN, Karthikeyan M, Kannan M, Rajasekar S. Terminalia belerica. Roxb – a phytopharmacological review. Int J Res Pharm Biomed Sci. 2012;3(1):96–99. | |
Abraham A, Mathew L, Samuel S. Pharmacognostic studies of the fruits of Terminalia bellerica (Gaertn.) Roxb. J Pharmacogn Phytochem. 2014;3(2):45–52. | |
Shinde V, Dhalwal K, Mahadik KR. Review on antioxidant potential of some important medicinal plants. Pharmacologyonline. 2007;2:1–11. | |
Naik GH, Priyadarsini KI, Hari M. Free radical scavenging reactions and phytochemical analysis of Triphala, an ayurvedic formulation. Curr Sci. 2006;90:1100–1105. | |
Palanisamy U, Cheng HM, Masilamani T, Subramaniam T, Ling LT et al. Rind of the rambutan, Nephelium lappaceum, a potential source of natural antioxidants. Food Chemistry. 2008;109(1):54–63. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.