Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
How does the efficacy and safety of Oralair® compare to other products on the market?
Authors Larenas-Linnemann D
Received 23 September 2015
Accepted for publication 17 November 2015
Published 27 May 2016 Volume 2016:12 Pages 831—850
DOI https://doi.org/10.2147/TCRM.S70363
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Video abstract presented by Désirée Larenas-Linnemann. Abstract: Due to differences between allergen immunotherapy (AIT) trials in patient populations, trial design (including primary efficacy variables), the definition of a pollen season, data analy
Views: 1833
Désirée Larenas-Linnemann
Pediatric Allergy and Asthma Clinic, Department of Investigation, Hospital Médica Sur, México City, México
Abstract: Due to differences between allergen immunotherapy (AIT) trials in patient populations, trial design (including primary efficacy variables), the definition of a pollen season, data analysis, and comparisons between AIT products with existing data, is not possible nor valid. The efficacy of two grass pollen AIT tablets, Oralair® and Grazax®/Grastek®, should not be compared by looking at the percentage of score improvement in their respective trials. However, the evidence available concerning the efficacy and safety in trials can be compared by paying close attention to the scientific quality of the trials, details in the administration schedules, and safety issues. It can be concluded due to the high level of evidence available, that Oralair® is effective in a pre (2-months)-coseasonal schedule to reduce symptoms and medication use, and improve a patients’ quality of life during the treatment season. For the long-term, where the quality of efficacy evidence is moderate at 2-year posttreatment due to a high dropout rate, the pre (4-months)-coseasonal schedule should be used. No clinical efficacy data exists for starting treatment in-season, but the clinical onset of action of Oralair® is detectable after only 1 month of treatment. In the pivotal trials in Europe and the USA, no tablet-related epinephrine was needed, though some rare severe local reactions have been reported. Research for Grazax®/Grastek® showed that the long-term efficacy needs a continuous 3-year administration (moderate-low quality evidence available), and in two patients, tablet-related epinephrine was given. Further details on the comparative efficacy of both tablets would only be possible if both were evaluated in the same, adequately powered trial.
Keywords: sublingual allergen immunotherapy, grass pollen, allergic rhinitis, allergic conjunctivitis, tablet allergen immunotherapy
Introduction
Allergic rhinoconjunctivitis (ARC) is one of the most commonly occurring chronic respiratory conditions, which worldwide has been reported to affect between 10% and 30% of the population.1 The most important inhalant allergen in Central Europe is Timothy grass pollen (Phleum pratense). On the other side of the Atlantic, in the USA it is among the top three most frequently found allergic sensitizers, while in the more Northern regions of the USA, tree pollens gain a greater importance.2 Over 80% of the ARC patients seen by allergists come in with a moderate–severe form of the disease.3 Consequently, although at first sight ARC does not seem to be a disorder of major significance, taken into account the severity of the disease and the frequent co-morbidities such as rhinosinusitis,4 otitis media with effusion, and asthma, all impact on the quality of life (QoL) of the patient, it therefore, has to be considered a public health issue of importance.
As of today, allergen immunotherapy (AIT) remains the only disease-modifying treatment offered to patients with ARC and allergic asthma. After a century of subcutaneous (SC) applications, the sublingual (SL) route has been of growing importance in the last few years.5 This is especially so after the “big trials”6 and Cochrane meta-analyses7,8 reported an affirmative effect. Positive outcomes on symptoms and medication scores in pivotal trials convinced authorities to approve SL immunotherapy, first in Europe as an SL solution, and more recently in Europe and the USA as SL tablets. As such, the SL-AIT now covers approximately half the AIT market in some European countries. This trend was clearly shown by McDonell et al who conducted a retrospective cohort study using IMS® Disease Analyzer (IMS HEALTH GmbH& Co. OHG [IMS], Frankfurt am Main, Germany) in Germany over a 7-year period (September 2005 – December 2012).9 Data from 18,850 patients with a prescription for grass pollen AIT were analyzed. Although the majority of the patients still received SC-AIT, there was a statistically significant tendency for a rise in the SL-AIT prescription rate, from 8% during 2006/2007 to 29% during 2011/2012.9 Also in the USA a rise in SL-AIT prescription tendency was detected, even though the absolute percentage of patients that are prescribed SL-AIT versus SC-AIT is still low10 and can be expected to have risen after the Food and Drug Administration (FDA) approval of SLIT tablets in 2014.
Since the first trials on SL immunotherapy almost 3 decades ago, dosing of the SL-AIT solution has been a major issue that has still not been completely resolved. This could be due to the fact that with SL-AIT not only the quality and exact quantity of the administered extract determine its efficacy but also the vehicle and other factors that are involved in the local allergen uptake.11 Due to this fact, major allergen manufacturers in Europe started researching SL tablets in order to have a product with a fixed dose and formulation. As grass pollen is one of the most prominent causes of ARC, the allergen selected for the tablet trials and posterior marketing has been the grass pollen SL tablet.
With the grass pollen SL-AIT tablets on the market, allergists now have several options for allergen-specific immunotherapy in patients with ARC (and allergic asthma) due to grass pollen. The authors focused on one of the grass pollen SL-AIT tablets on the market, Oralair®, and how data on this product compared to data on other grass pollen AIT possibilities.
Indications for Oralair®
In Europe, Oralair® is indicated for the treatment of allergic rhinitis with or without conjunctivitis induced by grass pollen in adults, adolescents, and children (>5 years of age) with clinically relevant symptoms, confirmed by a positive skin test and/or a positive specific serum immunoglobulin E (sIgE) test.
In the USA, the FDA approved Oralair® in 2014. According to the US product sheet, the indications are almost the same as those in Europe with two minor differences. The FDA specified the indication further, adding after “[…] positive specific sIgE testing for any of the five grass species contained in this product.” Also, the FDA set the age limits for Oralair® between 10 and 65 years.
Composition of Oralair®, a five-grass pollen tablet
Oralair® contains the natural allergens of pollens from several cross-reacting grasses. These are all species from different tribes of the Northern pasture grasses: cock’s-foot or orchard grass (Dactylis glomerata L.), sweet vernal grass (Anthoxanthum odoratum L.), rye-grass (Lolium perenne L.), Kentucky bluegrass or meadow-grass (Poa pratensis L.) and Timothy grass (P. pratense L.). The latter is commercially the most important perennial grass in the USA as it is widely cultivated for hay from the Northeast to South of Missouri. Pollen release starts in late spring and lasts until mid-autumn. The most important grass in the Southern regions of the USA, Bermuda grass (Cynodon dactylon), which has certain unique allergens different from the group of grasses mentioned earlier,12 is not included in the tablet. As such, Oralair® is indicated to patients allergic to one or several of the Northern pasture grasses.
Comparative efficacy
Although it has been more than a decade since the first Cochrane meta-analysis on SL-AIT7 convinced the medication community on the clinical efficacy of SL-AIT, the value of analyzing several trials with SL-AIT products grouped together in meta-analyzes is progressively being questioned of late. This is especially so after a group of experts made an in-depth analysis of the outcome variables used in different trials,13 which led them to conclude that the heterogeneity between trials is large, especially between trials conducted by different allergen manufacturers. Previously, world leaders in the field had already made recommendations for trials with AIT in an effort to harmonize the design of AIT trials.14
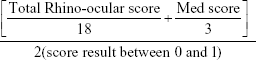
As both symptoms and medication use are two linked variables, a combined symptom–medication score is the preferred primary efficacy variable. However, some trials use only the symptom score as their main outcome. Even among the trials using a combined symptom–medication score, these are not constructed in the same manner: some investigators use the 6-item total symptom score–in which nasal and ocular symptoms all are scored 0–3 adding up to a maximum total of 18 points, to which then the value of the medication score (0–3 per day) is added. This approach results in a sub-valuation of the medication score, as there is a top daily symptom score of 18, whereas the top daily medication score can only reach 3. This is why other researchers use the same rhinoconjunctivitis symptom score, but calculate a balanced symptom–medication score as follows:
|
|
Investigators from Stallergenes constructed an adjusted symptom score, in which the daily symptoms were adjusted according to medication intake from the previous 2 days.15 However, as no other company used this method, scientists were asked by the authorities to recalculate the results of the 5-year pivotal trial of Oralair® with the more conventional symptom–medication score and these results were published in 2015.16 Two papers on the same data-set have now been published for the long-term efficacy of Oralair®.15,16
Another variable that is different between trials is the definition of the pollen season. Some investigators defined the start of the pollen season in their trial as the presence of 3 consecutive days with a pollen count of 10 grains/m3 or more, while others defined the start of the season with a higher pollen count (see Table 2 for details of specific trials). This is important for the outcome of the trial and directly affects the symptom score difference between active and placebo treatments. Investigators from the Imperial College in London showed that the higher the pollen count, the greater the difference in symptom scores between the patients in the placebo and the AIT group.17,18
The last variation related to outcome variables we mention here is the expression of the results of the symptom and medication scores. In AIT trials, it is quite common for a remarkable group of subjects to not take any rescue medication at all. This holds true for both the active and the placebo groups. As such, the mean values for rescue medication use for placebo and active treatment arms do not differ too much, skewed by a high rate of zero scores. Presenting the data as median values is much less sensitive to several zero values and normally shows a larger difference between active and placebo. Thus, if symptom reduction is expressed as the difference between active pre-posttreatment and placebo pre-posttreatment median values, the percentage of gain is generally higher than that expressed as the percentage of difference between mean values pre-posttreatment of the AIT versus the placebo group. When reviewing a paper and the percentage gain is presented, the reader needs to check if the authors are showing the percentage gain in median or in mean score values.
Making such an in-depth analysis leads to the conclusion that the efficacy from one product to the other by comparing the percentage of improvement in scores between product A, as observed in trial A, versus product B in trial B, should not be compared. Only products evaluated in trials with the same methodology, patient population, and with the same analysis and presentation of the data can be directly compared in their efficacy. Such trials, until now, have not been published for the AIT grass tablets.
What can be concluded concerning AIT efficacy from the published trials
What can be concluded from the trials conducted with grass pollen AIT and specifically, with the five-grass tablet Oralair®, is the level of evidence to support the efficacy of the products in certain situations. The level of evidence is directly related to the quality of the trials published. Conventionally, double-blind, placebo-controlled, randomized trials have been considered as the highest level of evidence; however, specific flaws in the design and presentation of a double-blind, placebo-controlled, randomized trial can reduce its quality of evidence, eg, underpowered trials, trials with indirect outcome measures, or trials with selective presentation of the data. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system for the evaluation of the quality of published data takes all of these variables into account and assigns quality of evidence on a four-step scale, from very low to high.
In the “Grass pollen subcutaneous AIT” and “Grass pollen sublingual AIT” sections, the quality of evidence that exists in the published literature up until now is reviewed. This focuses on the efficacy of grass pollen AIT with specific administration schedules and in specific patient groups, focusing on SL-AIT with liquid and tablet formulations. To put the results in a broader context, the evidence existing for grass pollen SC-AIT will also be reviewed.
Grass pollen subcutaneous AIT
A Cochrane meta-analysis from 2007 showed that SC-AIT for seasonal allergic rhinitis was effective with a reduction in the symptoms score (standard mean difference [SMD] −0.73) and in the medication score (SMD −0.57).3 Fifty-one double-blind, placebo-controlled (DBPC) trials were included, but of those only 15 were suitable to add to the symptom score analysis (Table 1). Moreover, most trials were small, with between ten and 25 subjects in the active group. Among the trials that fulfilled the inclusion criteria, there was only one large trial with over a 100 subjects in the active group. This was a GRADE high-quality of evidence trial (Table 2), in which two doses of standardized alum-adsorbed Timothy grass pollen were tested against a placebo.39
  | Table 1 Number and quality according to GRADE of the double-blind, placebo-controlled, randomized trials of SC-AIT in patients with SAR included in the Cochrane meta-analysis 2007 |
      | Table 2 Quality of evidence (according to the GRADE approach) of SLIT studies on Oralair®, and several pivotal trials with other grass pollen formulations |
Although both doses, 10,000 and 100,000 SQ-U (standard quality units), every 6 weeks were effective in reducing symptoms and medication scores, the higher dose was more so. Interestingly, treatment was started on average 38 weeks preseasonally and thus patients received SC-AIT for almost a year, even though the schedule was officially called a precoseasonal schedule (Table 3).
  | Table 3 Clinical efficacy of SLIT: focus on five-grass tablet Oralair® |
As for safety, in the high-dose group there were nine subjects (4.4%) with a grade 3 systemic adverse reaction, while in the low-dose group there was none.4
The long-term data for grass-pollen SC-AIT was reported from a trial conducted at the end of the previous millennium in which symptom and medication scores maintained the improvement accomplished after 3 years of continuous SC-AIT, when in a double-blind randomized study extension patients were continued for another 2 years on SC-AIT or on a placebo.41
With these robust data supporting the efficacy and long-term effects of grass pollen SC-AIT with a high-dose standardized extract started long before the pollen season, there have been few new trials with conventional SC-AIT in grass pollen-allergic patients over the past years.49 This is probably due to the fact that in the field of SC-AIT the focus of investigators has changed over time, from documenting efficacy to shortening the buildup phase50,51 and enhancing the safety, using hypoallergenic formulations or recombinant molecules.
Grass pollen SL-AIT in adult and pediatric patients: efficacy for one season
Precoseasonal schedule in adult and pediatric patients
Didier et al conducted the pivotal “big trial” that showed a dose–response efficacy for precoseasonally administered Oralair® in 628 patients.19 After a short buildup phase incrementing the daily dose with 100 index of reactivity (IR) 4 months before season-start, patients then continued onto the dose pertaining to their randomized group. No clinical benefit was found in the 100IR group, while the 300IR and 500IR groups showed similar results in favor of the AIT over placebo. As a result, the 300IR dose (25 μg of group 5 grass pollen major allergen) was selected as the optimal dose for commercialization.19 The same investigational team went on to define the optimal duration of the preseasonal phase in another long-term study. Both 2- and 4-month preseasonal treatments with Oralair® were equally effective in reducing symptoms during the subsequent pollen season.20
Two years later, Wahn et al confirmed the efficacy and safety of the five-grass tablet in children.21 The study design recruited children ≥4 years of age and showed improved symptom and medication scores, both during the pollen season21 and during the peak pollen season.22
In a US trial of 438 patients,5 similar results were found to those by Didier et al.19 There were however, several minor differences between both trial setups. In the US trial, the patients received directly the 300IR dose without up-dosing, the pollen season definition was homogenized with another grass-tablet sublingual immunotherapy (SLIT) trial, and authorities asked the investigators to change the primary efficacy parameter to a daily combined symptom–medication score (DCS). DCS and the adjusted symptom score all statistically improved significantly in the active group. As opposed to other trials, patients in the placebo group had free access to the rescue medication and their rescue medication score was higher than that of the active group. Even so, the patient-rated overall improvement during the trial worked out positively for the active group.
In the intention-to-treat data, the DCS reached a 28% improvement over placebo, which is more than the World Allergy Organization (WAO) recommended 20% cutoff defined as a clinically relevant outcome. Also, in this US trial, specific sIgE was not an inclusion criterion. An interesting observation in this trial became clear in a post hoc analysis grouping those patients with Timothy pollen sIgE as either <0.1 or ≥0.1 kU/L. In the group with sIgE <0.1 kU/L, no treatment effect could be detected.45
During the same time Cox et al’s45 trial was conducted, another grass pollen tablet was researched: the fast dissolving Timothy grass pollen tablet, Grazax®/Grastek®. There are three main differences between this formulation and Oralair®. First, Oralair® is composed of the pollens of five cross-reactive grasses, while Grazax®/Grastek® only includes Grazax® timothy grass pollen. Second, the quantity of group 5 major allergen in Oralair® is stated to be approximately 25 μg, while that of Grazax®/Grastek® is 15 μg; and third, the excipient of Grazax®/Grastek® contains fish gelatingelatin, which allows for very fast dissolving of the tablet once put under the tongue; the dissolving of Oralair® takes somewhat longer.
Putting these details aside, the most important point is the clinical performance of the product. In this sense, Grazax®/Grastek® has also shown to be effective in a one-season preseasonal (8-week)-coseasonal schedule. In Europe, large DBPC trials, both in adults24 and in children ≥4 years of age52 found that Grazax®/Grastek® reduced symptom and medication scores and improved QoL, as tested with the validated, disease-specific, rhinoconjunctivity QoL questionnaire. Similar results were obtained in the US trials in adults,30,53 adolescents,30 and in children aged ≥5 years.28,30 In a post hoc analysis of pooled evidence from several trials with the fast-dissolving tablet it became clear that the best results were obtained in patients with a 4-month preseasonal period, compared to those with a shorter preseasonal treatment phase.54
All the aforementioned trials were GRADE 4, high-quality trials (Table 2). Thus, high-quality evidence exists to state that both grass pollen tablets are effective in a 2-month precoseasonal schedule in adults and children with ARC in Europe and in the USA. For Grazax®/Grastek®, 4-month preseasonal is best.
Preseasonal schedules
Until now there have been no publications on the grass tablet SL-AIT in a merely preseasonal schedule. The only recent preseasonal study with grass pollen SL-AIT was conducted by Bozek et al6 with a five-grass liquid formulation, delivering 240IR sublingually 5 days per week in elderly allergic rhinitis patients. A marked reduction in symptom and medication scores was documented during the 3rd year’s pollen season after 4-month preseasonal administration over 3 consecutive years.31 The GRADE quality of this trial was 1–2, (very) low. In conclusion, there exists no evidence for efficacy of preseasonal only administration of the grass tablets.
Coseasonal schedules with in-season starting
As many patients visit their physicians when they are already presenting symptoms, it is often not possible to start AIT preseasonally. This is why the possibility of in-seasonal starting of AIT was explored. The first point in analyzing this option is the safety issue, with SL-AIT tablets being highly concentrated it might therefore not be safe to start them in-season. For Grazax®/Grastek®, there is some evidence with respect to the safety of such management; however, no clinical outcomes of efficacy were reported.55
In conclusion, there is no evidence on the clinical efficacy of coseasonal administration of the grass pollen tablets. There is limited, favorable evidence existing on the safety of Grazax®/Grastek® started in-season.
Mono- and polysensitized subjects
In all of the previously described trials, more than half of the patients were polysensitized. Especially in the US trials, polysensitization rates of over 80% were reported.28,45 In the 3-year Oralair® trial, analysis were conducted on this subgroup of patients, reporting the same efficacy as in the mono-sensitized patient group.20 Also, in an analysis of pooled data from several trials with Grazax®/Grastek®, Calderon et al concluded that polysensitized patients benefit as much, if not more, from AIT as monosensitized patients.56 Great care should be taken in interpreting these statements, as investigators are only referring to the benefit of the grass pollen AIT tablets for the ARC patient during the 2 months’ pollen season.
In conclusion, during the grass pollen season, polysensitized ARC patients benefit at least as much, if not more, from the grass pollen tablets as monosensitized patients.
Grass pollen SL-AIT in adult patients: efficacy over subsequent seasons
Administering Oralair® over 3 consecutive years in a precoseasonal schedule demonstrated sustained efficacy in the reduction of symptom and medication scores year after year, both with a 2-month and with a 4-month preseasonal start.20 Dahl et al25 and Durham et al57 also documented the sustained efficacy of Grazax®/Grastek®. However, the administration of the latter was in a continuous year-round daily schedule, as opposed to the 6-months-per-year, precoseasonal schedule of Oralair® (Table 3). Both these trials delivered moderate–high quality of evidence, GRADE 3–4 (Table 2).
In conclusion, both grass pollen tablets have sustained clinical efficacy when administered year after year, for Oralair® in a precoaseasonal schedule and for Grazax®/Grastek® during continuous administration.
Grass pollen SL-AIT in adult patients: long-term efficacy posttreatment
The aforementioned 3-year trials of Oralair® and Grazax®/Grastek® went on into respective extension phases of 2 years posttreatment, during which the patients continued to score seasonal symptoms and rescue medication use, but without any further SL-AIT. Three years treatment of preseasonal (4-month)-coseasonal Oralair® resulted in a statistically significant reduction in the combined symptom and medication scores, even after 2 years off-treatment. However, if the preseaonal phase was reduced to only 2 months, a trend toward long-term efficacy was registered without reaching statistical significance. Because of the high dropout rate in such long trials, the quality of evidence is moderate, GRADE 3 (Table 2).
For Grazax®/Grastek®, 3 years of continuous administration also led to a 2 years posttreatment clinical efficacy, as expressed by the combined symptom–medication score. As this trial was originally planned for only 1 year, during the extension phase to 3 treatment years plus, in the post-AIT years more than 60% of the patients were lost, resulting in the quality of evidence being low–moderate, GRADE 2–3.
Thus, long-term efficacy of a 3-year course of SL-AIT after 2 years off-treatment was shown for Oralair® with a pre (4-month)-coseasonal dosing schedule, and for Grazax®/Grastek® with a continuous daily dosing schedule. The quality of evidence for these results is moderate and low-moderate respectively.
Grass pollen SL-AIT in adult patients: onset of action
Almost all trials focused on the efficacy of the grass pollen AIT during the course of the whole pollen season. Until now, there has been only one trial that directly investigated the onset of action.23 This was done between the 2007 and 2008 grass pollen seasons by Horak et al in the Vienna Allergen Chamber, the first allergen challenge chamber (ACC) in function. The ACC allows a controlled pollen exposure to a group of grass pollen-allergic patients simultaneously under standard conditions. After a pre-randomization challenge to select patients with a certain minimum rhinoconjunctivitis symptom score in order to assure the inclusion of moderate–severe allergic patients, 89 subjects were randomized to 4-month treatment with Oralair® (n=45) or placebo (n=44). After the baseline challenge and the start of the AIT, subjects were rechallenged in the ACC during 4 hours sessions at 1 week, 1, 2, and 4 months. The symptom score in the Oralair® group was lower during each test-session in comparison with the placebo, even at 1 week, but the difference reached statistical significance by the 1-month challenge. At months 2 and 4, the difference in symptoms score improvement during challenge between active and placebo steadily grew until a relative mean improvement compared with the placebo of 29.3%. As the sample size was not calculated to power the study for the secondary endpoints of nasal airflow, nasal secretion weight, and skin prick test reactivity, no statistically significant differences could be detected between active and placebo groups in these parameters, although tendencies were toward improvement in the active group. The investigators concluded that Oralair® shows a symptom reduction on pollen-exposure from ≥1 month of treatment.23
In conclusion, after 1 month of treatment with Oralair®, the symptom exacerbation due to pollen exposure in an ACC, is reduced, compared to the placebo.
Safety
The initial trials with Oralair® were cautiously started with a short buildup phase of 5 days up-dosing.19 In this first dose-finding trial, mild treatment-emergent adverse events (TEAEs) were frequent and found in >60% of the subjects in each of the dosing groups. However, there was a dose–response relationship for discontinuation due to TEAEs of 3.8%, 5.2%, and 6.9% in the 100IR, 300IR, 500IR dosing groups, respectively, and 0% in the placebo group. Yet, there were no serious study treatment-related AEs.19 Thus, since the product did not seem to cause any major systemic AEs, subsequent trials started directly with the 300IR tablet, with the indication to take the first tablet under strict medical supervision. As such, in the 3-year European trial by Didier et al20 and in the US trial by Cox et al,45 the study-subjects took the 300IR tablet from day 1 onward. The AE profile of Oralair® maintains more or less stable between the various subsequent trials: mild–moderate oral symptoms at study start are seen in more than half of the patients, but very rarely lead to discontinuation. Moreover, the discontinuation rate due to TEAEs progressively declines season after season: from 6% in the 1st year, to 0.6% and 0% in years 2 and 3, respectively.20 Also, two serious drug-related TEAEs only occurred during the first year: one severe local allergic reaction and one because of angioedema, both leading to permanent discontinuation from the study.
Although none of the large European trials used epinephrine, in the US trials of the grass tablets, patients were instructed to carry an epinephrine autoinjectorautoinjector. In the USA, during the Oralair® study there were no serious TEAEs. During the European trials, 11/228 (4.8%) in the active group withdrew because of TEAEs.45
In the ACC trial by Horak et al7 conducted out of season, all patients in the active group were given the 300IR tablet from the start, and no patient withdrew because of an AE. Sixty percent of the patients in the active group experienced a TEAE versus 31.8% of the placebo patients, but these were mild local events, (oral pruritus and throat irritation) lasting normally <2 weeks.
Observational, “real-life” studies can be useful complements to the results of randomized controlled trials. An observational, real-life safety study of a five-grass pollen SL tablet was conducted in children and adolescents (5–17 years old) to evaluate the safety and AEs with Oralair®. Of the 796 fully documented patients, 27.4% experienced at least one adverse drug reaction during the study, 11.8% on the 1st day of dosing. Seventy-five percent of those were of mild–moderate severity and no adrenaline was used. Seventy-six (9.2%) of the subjects discontinued the SL-AIT because of an AE.58
In the fast-dissolving grass tablet trials, Durham et al24 reported that more than half of the patients had mild local reactions, oral sensations, that had a median duration of 4 and 10.5 days in both of the highest dosing groups of this trial (15 μg Phl p five daily). In these groups, 5.1% of subjects withdrew because of an AE. One serious drug-related AE was reported in the middle-dosing group (5 μg Phl p five daily): one patient had uvula edema, which resolved without medication and the patient continued in the study.24 In the Grastek® US trial, 82% experienced an AE (77% in placebo group). Most of them were local mild–moderate reactions that resolved in a mean of 1–7 days. There were 5.2% discontinuations due to AE. Two subjects were administered epinephrine, one of them being in the SLIT group who developed dysphagia, uvular edema, and pharyngeal edema at the application site, along with a macular rash and chest discomfort (WAO grade 1 systemic reaction59). After treatment with antihistamine, epinephrine, and prednisone, the event was controlled within an hour, without any further repercussions.53 In the pediatric trial, two Grastek® patients received epinephrine, but only one was due to a reaction to the tablet, with this child developing lip angioedema, slight dysphagia, and intermittent cough immediately after the first dose (day 1) of grass AIT. After the investigator administered epinephrine the symptoms resolved. The event was graded as of moderate severity by the investigator.28
In the US trials, at least two subjects administered erroneously epinephrine, misinterpreting symptoms as if they were due to an allergic reaction.28,29
In conclusion, local allergic reactions were very common in the first 1–2 weeks of treatment. Neither of the grass pollen tablets caused anaphylactic shock or fatalities in trials, although some grade 1–3 systemic AE (WAO Grading system59) have been seen, and in the US trial, epinephrine autoinjector prescription is warranted. Several systemic reactions have been treated at the office, as most have been after the first dose. In two Grastek® US trials, an epinephrine autoinjector was used, because of a tablet-related reaction (one patient each).28,29 Discontinuation because of AE ranged between 5% and 9%.
Conclusion
Currently two SL tablets exist on the market for the treatment of grass pollen–induced ARC, one being a five-grass pollen tablet, Oralair®, the other being the fast-dissolving Timothy grass pollen tablet, Grazax®/Grastek®. Comparing the efficacy of these two tablets with existing data is not possible as both have been tested in different clinical trials. As discussed in this paper and also observed previously,60 the definition of combined symptom–medication scores and single symptom or medication scores varies between trials, as do the study design, study population, and other variables. This is one of the flaws of meta-analysis and makes comparing efficacy indirectly in meta-analysis doubtful.
However, what can be stated based on the existing evidence is the efficacy and safety of the tablets in specific dosing schedules, patient groups, and situation. Moreover, depending on trial details, a level of evidence can be assigned to each of these situations. As such, we have a high degree of evidence for the efficacy of Oralair® in a pre (2-month)-coseasonal schedule for individual pollen seasons and subsequent pollen seasons.8–10 However, the long-term posttreatment effect is best accomplished with the pre (4-month)-coseasonal schedule,10 be it that here the level of evidence is moderate due to a dropout rate after 5 years of approximately 40%. Similar efficacy and safety have been found for pediatric and polysensitized patient groups, be it only for variables recorded during the pollen seasons. Obviously, efficacy of the grass pollen AIT in polysensitized patients with symptoms outside the grass-pollen season cannot be expected.
For Grazax®/Grastek®, very similar results are published on efficacy, with the difference that the 4-month preseasonal schedule gave the best results in an analysis of pooled data from three DBPC trials,11 and the long-term efficacy has only been documented after a continuous, all-year-round administration schedule for 3 years, with low–moderate quality of evidence available.12
Concerning safety, local, mild–moderate adverse reactions are very common the first 1–2 weeks of the treatment, but generally disappear when treatment is continued. Also, they are less common and less severe when treatment is restarted before the next pollen season, with precoseasonal Oralair®.9 In the Oralair® trials, no use of epinephrine has been documented. In trials with Grazax®/Grastek®, an epinephrine autoinjector was used in two patients because of adverse reactions, judged to be probably tablet-related.13,14 Discontinuation due to tablet-related adverse reactions, mostly moderate–severe local reactions in the oral cavity, is very similar in the DBPC trials, ranging ~5% for both tablets. In a post-marketing Oralair® trial it was 9%.
For patients (Europe ≥5 years of age, USA ≥10 years of age) with grass pollen–induced allergic rhinitis with or without conjunctivitis, confirmed by the presence of sIgE to Northern Pasture grass pollens, the pre (4-month)-coseasonal administration of Oralair® for 3 subsequent years is an effective and safe management strategy with long-term efficacy for at least 2 years posttreatment. Administration for only 6 months of the year, as opposed to the continuous administration needed for long-term effects of Grazax®/Grastek®, is favorable from a pharmacoeconomic point of view. Even though the safety profile for Oralair® is clean for anaphylactic shock and WAO grade 4–5 systemic reactions, and no epinephrine was used in the pivotal trials with this tablet, in the USA, an epinephrine autoinjector has to be prescribed together with either of the tablets.
Disclosure
DL has received honoraria in Mexico from GlaxoSmithKline, Boehringer Ingelheim, Mit-Pharma, Novartis, and MEDA. DL is currently receiving a grant from Novartis, Sanofi, GlaxoSmithKline, TEVA, MSD, Pfizer, AstraZeneca, MEDA, and Senosiain. She is on the speaker’s bureau for MSD, Pfizer, AstraZeneca, MEDA, Glenmark, MIT-Pharma and The DVB safety board. The author reports no other conflicts of interest in this work.
References
Pawankar R, et al. (2013). “The WAO White Book on Allergy (Update. 2013).” Available from: http://www.worldallergy.org/UserFiles/file/WAO-White-Book-on-Allergy_web.pdf. Accessed December 2, 2015. | ||
Sedaghat AR, Phipatanakul W, Cunningham MJ. Characterization of aeroallergen sensitivities in children with allergic rhinitis and chronic rhinosinusitis. Allergy Rhinol (Providence). 2014;5(3):143–145. | ||
Larenas-Linnemann D, Michels A, Dinger H, et al. In the (sub)tropics allergic rhinitis and its impact on asthma classification of allergic rhinitis is more useful than perennial-seasonal classification. Am J Rhinol Allergy. 2014;28(3):232–238. | ||
Sedaghat AR, Phipatanakul W, Cunningham MJ. Prevalence of and associations with allergic rhinitis in children with chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol. 2014;78(2):343–347. | ||
Canonica GW, Cox L, Pawankar R, et al. Sublingual immunotherapy: World Allergy Organization position paper 2013 update. World Allergy Organ J. 2014;7(1):6. | ||
Durham SR. Sublingual immunotherapy: what have we learnt from the ‘big trials’? Curr Opin Allergy Clin Immunol. 2008;8(6):577–584. | ||
Wilson DR, Lima MT, Durham SR. Sublingual immunotherapy for allergic rhinitis: systematic review and meta-analysis. Allergy. 2005;60(1):4–12. | ||
Radulovic S, Calderon M, Wilson S, Durham S. Sublingual immunotherapy for allergic rhinitis: an updated Cochrane systematic review and meta-analysis. Allergy. 2007;62(s83):167–171. | ||
McDonell AL, Wahn U, Demuth D, et al. Allergy immunotherapy prescribing trends for grass pollen-induced allergic rhinitis in Germany: a retrospective cohort analysis. Allergy Asthma Clin Immunol. 2015;11(1):19. | ||
Sikora JM, Tankersley MS. Perception and practice of sublingual immunotherapy among practicing allergists in the United States: a follow-up survey. Ann Allergy Asthma Immunol. 2013;110(3):194–197. | ||
Larenas-Linnemann D, Mosges R. Dosing of European sublingual immunotherapy maintenance solutions relative to monthly recommended dosing of subcutaneous immunotherapy. Allerg Asthma Proceedings. 2015;37(1):50–56. | ||
Esch RE. Grass pollen allergens. Clin Allergy Immunol. 2008;21:107–126. | ||
Pfaar O, Demoly P, Gerth van Wijk R, et al. Recommendations for the standardization of clinical outcomes used in allergen immunotherapy trials for allergic rhinoconjunctivitis: an EAACI Position Paper. Allergy. 2014;69(7):854–867. | ||
Canonica GW, Baena-Cagnani CE, Bousquet J, et al. Recommendations for standardization of clinical trials with allergen specific immunotherapy for respiratory allergy. A statement of a World Allergy Organization (WAO) taskforce. Allergy. 2007;62(3):317–324. | ||
Didier A, Malling HJ, Worm M, et al. Post-treatment efficacy of discontinuous treatment with 300IR 5-grass pollen sublingual tablet in adults with grass pollen-induced allergic rhinoconjunctivitis. Clin Exp Allergy. 2013;43(5):568–577. | ||
Didier A, Malling HJ, Worm M, Horak F, Sussman GL. Prolonged efficacy of the 300IR 5-grass pollen tablet up to 2 years after treatment cessation, as measured by a recommended daily combined score. Clin Transl Allergy. 2015;5:12. | ||
Durham SR, Emminger W, Kapp A, et al. SQ-standardized sublingual grass immunotherapy: confirmation of disease modification 2 years after 3 years of treatment in a randomized trial. J Allergy Clin Immunol. 2012;129(3):717–725. | ||
Durham SR, Nelson HS, Nolte H, et al. Magnitude of efficacy measurements in grass allergy immunotherapy trials is highly dependent on pollen exposure. Allergy. 2014;69(5):617–623. | ||
Didier A, Malling HJ, Worm M, et al. Optimal dose, efficacy, and safety of once-daily sublingual immunotherapy with a 5-grass pollen tablet for seasonal allergic rhinitis. J Allergy Clin Immunol. 2007;120(6):1338–1345. | ||
Didier A, Worm M, Horak F, et al. Sustained 3-year efficacy of pre- and coseasonal 5-grass-pollen sublingual immunotherapy tablets in patients with grass pollen-induced rhinoconjunctivitis. J Allergy Clin Immunol. 2011;128(3):559–566. | ||
Wahn U, Tabar A, Kuna P, et al. Efficacy and safety of 5-grass-pollen sublingual immunotherapy tablets in pediatric allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2009;123(1):160–166. | ||
Halken S, Agertoft L, Seidenberg J, et al. Five-grass pollen 300IR SLIT tablets: efficacy and safety in children and adolescents. Pediatr Allergy Immunol. 2010;21(6):970–976. | ||
Horak F, Zieglmayer P, Zieglmayer R, et al. Early onset of action of a 5-grass-pollen 300-IR sublingual immunotherapy tablet evaluated in an allergen challenge chamber. J Allergy Clin Immunol. 2009;124(3):471–477. | ||
Durham SR, Yang WH, Pedersen MR, Johansen N, Rak S. Sublingual immunotherapy with once-daily grass allergen tablets: a randomized controlled trial in seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006;117(4):802–809. | ||
Dahl R, Kapp A, Colombo G, et al. Sublingual grass allergen tablet immunotherapy provides sustained clinical benefit with progressive immunologic changes over 2 years. J Allergy Clin Immunol. 2008;121(2):512–518. | ||
Nieminen K, Valovirta E, Savolainen J. Clinical outcome and IL-17, IL-23, IL-27 and FOXP3 expression in peripheral blood mononuclear cells of pollen-allergic children during sublingual immunotherapy. Pediatr Allergy Immunol. 2010;21(1 Pt 2):e174–e184. | ||
Bufe A, Eberle P, Franke-Beckmann E, et al. Safety and efficacy in children of an SQ-standardized grass allergen tablet for sublingual immunotherapy. J Allergy Clin Immunol. 2009;123(1):167–173. | ||
Blaiss M, Maloney J, Nolte H, Gawchik S, Yao R, Skoner DP. Efficacy and safety of timothy grass allergy immunotherapy tablets in North American children and adolescents. J Allergy Clin Immunol. 2011;127(1):64–71. | ||
Nelson HS, Nolte H, Creticos P, Maloney J, Wu J, Bernstein DI. Efficacy and safety of timothy grass allergy immunotherapy tablet treatment in North American adults. J Allergy Clin Immunol. 2011;127(1):72–80. | ||
Maloney J, Bernstein DI, Nelson H, et al. Efficacy and safety of grass sublingual immunotherapy tablet, MK-7243: a large randomized controlled trial. Ann Allergy Asthma Immunol. 2014;112(2):146–153. | ||
Bozek A, Kolodziejczyk K, Warkocka-Szoltysek B, Jarzab J. Grass pollen sublingual immunotherapy: a double-blind, placebo-controlled study in elderly patients with seasonal allergic rhinitis. Am J Rhinol Allergy. 2014;28(5):423–427. | ||
Swamy RS, Reshamwala N, Hunter T, et al. Epigenetic modifications and improved regulatory T-cell function in subjects undergoing dual sublingual immunotherapy. J Allergy Clin Immunol. 2012;130(1):215–224. | ||
Wahn U, Klimek L, Ploszczuk A, et al. High-dose sublingual immunotherapy with single-dose aqueous grass pollen extract in children is effective and safe: A double-blind, placebo-controlled study. J Allergy Clin Immunol. 2012;130(4):886 e5–893 e5. | ||
Stelmach I, Kaluzinska-Parzyszek I, Jerzynska J, Stelmach P, Stelmach W, Majak P. Comparative effect of pre-coseasonal and continuous grass sublingual immunotherapy in children. Allergy. 2012; 67(3):312–320. | ||
Panzner P, Petráš M, Sýkora T, Lesná IK, Liška M. Both sublingual and supralingual routes of administration are effective in long-term allergen-specific immunotherapy. Allergy Asthma Proc. 2011;32(2):142–150. | ||
Panzner P, Petrás M, Sýkora T, Lesná I. Double-blind, placebo-controlled evaluation of grass pollen specific immunotherapy with oral drops administered sublingually or supralingually. Respir Med. 2008;102(9):1296–1304. | ||
Agostinis F, Foglia C, Bruno ME, Falagiani P. Efficacy, safety and tolerability of sublingual monomeric allergoid in tablets given without up-dosing to pediatric patients with allergic rhinitis and/or asthma due to grass pollen. Eur Ann Allergy Clin Immunol. 2009;41(6):177–180. | ||
Ahmadiafshar A, Maarefvand M, Taymourzade B, Mazloomzadeh S, Torabi Z. Efficacy of sublingual swallow immunotherapy in children with rye grass pollen allergic rhinitis: a double-blind placebo-controlled study. Iran J Allergy Asthma Immunol. 2012;11(2):175–181. | ||
Frew AJ, Powell RJ, Corrigan CJ, Durham SR. Efficacy and safety of specific immunotherapy with SQ allergen extract in treatment-resistant seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006;117(2):319–325. | ||
Walker SM, Pajno GB, Lima MT, Wilson DR, Durham SR. Grass pollen immunotherapy for seasonal rhinitis and asthma: a randomized, controlled trial. J Allergy Clin Immunol. 2001;107(1):87–93. | ||
Durham SR, Walker SM, Varga EM, et al. Long-term clinical efficacy of grass-pollen immunotherapy. N Engl J Med. 1999;341(7):468–475. | ||
Dolz I, Martínez-Cócera C, Bartolomé JM, Cimarra M. A double-blind, placebo-controlled study of immunotherapy with grass-pollen extract Alutard SQ during a 3-year period with initial rush immunotherapy. Allergy. 1996;51(7):489–500. | ||
Leynadier F, Banoun L, Dollois B, et al. Immunotherapy with a calcium phosphate-adsorbed five-grass-pollen extract in seasonal rhinoconjunctivitis: a double-blind, placebo-controlled study. Clin Exp Allergy. 2001;31(7):988–996. | ||
Ott H, Sieber J, Brehler R, et al. Efficacy of grass pollen sublingual immunotherapy for three consecutive seasons and after cessation of treatment: the ECRIT study. Allergy. 2009;64(9):1394–1401. | ||
Cox LS, Casale TB, Nayak AS, et al. Clinical efficacy of 300IR 5-grass pollen sublingual tablet in a US study: the importance of allergen-specific serum IgE. J Allergy Clin Immunol. 2012;130(6):1327–1334. | ||
Pajno GB, Caminiti L, Crisafulli G, et al. Direct comparison between continuous and coseasonal regimen for sublingual immunotherapy in children with grass allergy: a randomized controlled study. Pediatr Allergy Immunol. 2011;22(8):803–807. | ||
Stelmach I, Kaczmarek-Woźniak J, Majak P, Olszowiec-Chlebna M, Jerzynska J. Efficacy and safety of high-doses sublingual immunotherapy in ultra-rush scheme in children allergic to grass pollen. Clin Exp Allergy. 2009;39(3):401–408. | ||
Seidenberg J, Pajno GB, Bauer CP, La Grutta S, Sieber J. Safety and tolerability of seasonal ultra-rush, high-dose sublingual-swallow immunotherapy in allergic rhinitis to grass and tree pollens: an observational study in 193 children and adolescents. J Investig Allergol Clin Immunol. 2009;19(2):125–131. | ||
van der Valk JP, de Jong NW, Gerth van Wijk R. Review on immunotherapy in airway allergen sensitised patients. Neth J Med. 2015;73(6):263–269. | ||
Klimek L, Uhlig J, Mösges R, Rettig K, Pfaar O. A high polymerized grass pollen extract is efficacious and safe in a randomized double-blind, placebo-controlled study using a novel up-dosing cluster-protocol. Allergy. 2014;69(12):1629–1638. | ||
Larenas-Linnemann D. Allergen immunotherapy: an update on protocols of administration. Curr Opin Allergy Clin Immunol. 2015;15(6):556–567. | ||
Bufe A, Henmar H, Grønager P, Durham S. Sublingual immunotherapy with fast-dissolving grass tablets induces comparable IgG4 antibody and IgE-blocking responses in children and adults. J Allergy Clin Immunol. 2009;123(2):S75. | ||
Nelson H, Blaiss M, Nolte H, Wurtz SO, Andersen JS, Durham SR. Efficacy and safety of the SQ-standardized grass allergy immunotherapy tablet in mono- and polysensitized subjects. Allergy. 2013;68(2):252–255. | ||
Calderon MA, Birk AO, Andersen JS, Durham SR. Prolonged preseasonal treatment phase with Grazax sublingual immunotherapy increases clinical efficacy. Allergy. 2007;62(8):958–961. | ||
Reich K, Gessner C, Kroker A, et al. Immunologic effects and tolerability profile of in-season initiation of a standardized-quality grass allergy immunotherapy tablet: a phase III, multicenter, randomized, double-blind, placebo-controlled trial in adults with grass pollen-induced rhinoconjunctivitis. Clin Ther. 2011;33(7):828–840. | ||
Calderon MA, Cox L, Casale TB, Moingeon P, Demoly P. Multiple-allergen and single-allergen immunotherapy strategies in polysensitized patients: looking at the published evidence. J Allergy Clin Immunol. 2012;129(4):929–934. | ||
Durham S, Dahl R, Kapp A, et al. Sustained, disease-modifying effect of grass allergen tablet immunotherapy 1 year after completion of treatment. Allergy. 2009;64(S90):146. | ||
Eberle P, Brueck H, Gall R, Hadler M, Sieber J, Karagiannis E. An observational, real-life safety study of a 5-grass pollen sublingual tablet in children and adolescents. Pediatr Allergy Immunol. 2014;25(8):760–766. | ||
Cox L, Larenas-Linnemann D, Lockey RF, Passalacqua G. Speaking the same language: The World Allergy Organization Subcutaneous Immunotherapy Systemic Reaction Grading System. J Allergy Clin Immunol. 2010;125(3):569–574, 574 e1–574 e7. | ||
Calderon MA, Bernstein DI, Blaiss M, Andersen JS, Nolte H. A comparative analysis of symptom and medication scoring methods used in clinical trials of sublingual immunotherapy for seasonal allergic rhinitis. Clin Exp Allergy. 2014;44(10):1228–1239. | ||
Larenas-Linnemann D. Why direct efficacy comparison of SLIT tablets for rhino-conjunctivitis, based on existing data, is non-valid. Annals Allergy Asthma Immunol. Epub 2016. With permission from Elsevier. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.