Back to Journals » Drug, Healthcare and Patient Safety » Volume 12
Areas of Potential Improvement for Hospitals’ Patient-Safety Culture in Western Ethiopia
Authors Garuma M, Woldie M , Kebene FG
Received 25 March 2020
Accepted for publication 14 June 2020
Published 5 August 2020 Volume 2020:12 Pages 113—123
DOI https://doi.org/10.2147/DHPS.S254949
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Siew Siang Chua
Melkamu Garuma,1 Mirkuzie Woldie,2,3 Feyera Gebissa Kebene4
1Nekemte Public Health Research and Referral Laboratory, East Wollega Zone, Oromia Region, Ethiopia; 2Fenot Project, Harvard T.H. Chan School of Public Health, Department of Global Health and Population, Addis Ababa, Ethiopia; 3Department of Health Policy and Management, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 4Department of Public Health, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia
Correspondence: Feyera Gebissa Kebene Email [email protected]
Background: Patient-safety culture is an important component of health-care quality and currentlyan issue of high concern globally. In Ethiopia, little is known about patient-safety culture in hospitals. We assessed the patient-safety culture and associated factors among health-care workers in public hospitals of East Wollega Zone, western Ethiopia.
Methods: This institution-based cross-sectional study was conducted among 421 health-care workers selected using simple random sampling from March 4 to March 29, 2019. A standardized measuring 12 patient safety–culture components was used for data collection. Data were cleaned and entered into EpiData version 3.1 and analysis done using SPSS version 25 (IBM). Bivariate and multivariate linear regression analyses were performed. Significance was set at 95% CI and p< 0.05, and unstandardized β-coefficients were used to measure extent of association.
Results: This study revealed that the level of patient-safety culture was 49.2% and patient safety culture–component scores ranged from 29.2% for nonpunitive responses to error to 77.9% for teamwork within a hospital unit. Age ≥ 45 years (β=13.642, CI: 5.324– 21.959; p=0.001), 1– 5 years’ experience at the current hospital (β=5.559, 95% CI 2.075– 9.042; p=0.002), and working in general hospitals (β=11.988, 95% CI 7.233– 16.743; p< 0.001) and primary hospitals (β=6.408, 95% CI 2.192– 10.624; p=0.003) were factors associated with better scores on patient-safety culture.
Conclusion: Overall scores for patient-safety culture were low. Improving the current state of patient safety in public hospitals would require tailored interventions to address low-scoring components, such as nonpunitive responses to error.
Keywords: patient-safety culture, public hospital, Ethiopia
Introduction
Patient safety is defined as the absence of preventable harm to a patient during the process of health care.1 Patient safety is a global concern, which is sometimes missed in Saudia Arabia due to the complexity of the health-care system2 (61%). Culture can be defined as the sum of values, experiences, attitudes, and practices that guide the behavior of a group. A culture of blame where mistakes are viewed as personal failures should be replaced by a culture where mistakes are seen as opportunities to improve the system.3 Furthermore, patient-safety culture is defined as the product of individual and group values, attitudes, perceptions, competence, and patterns of behavior that determine the commitment to, style, and proficiency of an organization’s health and safety management.4
Patient-safety culture is widely recognized as a significant driver in changing behavior and expectations to increase and emphasize safety within organizations.5 This implies a discipline of coordinated efforts to avoid patient harm caused during the process of health care itself.Patient safety and initiatives of developing safety cultures to assure patients from harm have slowly but steadily become one of the central concerns in quality improvement.6 Even though health interventions are intended to benefit the public, due to a complex combination of processes, technologies, and human interactions, there is an inevitable risk that adverse health-care events will happen. Identifying and reducing the occurrence of these errors and improving the safety and quality of health care have been brought forward as a priority issue for health services around the world.7,8
The capacity of an organization to obtain a patient-safety culture can be improved when creating and establishing a culture of safety among its professionals. The main characteristics of a safety culture include a commitment to discuss and learn from mistakes, recognition of the inevitability of errors, proactive identification of latent threats, and incorporation of a nonpunitive system for reporting and analyzing adverse events.9 Organizations with a positive safety culture are characterized by communications founded on mutual trust and shared perceptions of the importance of safety and the efficacy of preventive measures.10 Studies on patient-safety culture provide feedback to health-care systems with the possibility of implementing improvement measures based on the identification of specific problems.11 In recent years, a lot of developed and some developing countries have published surveys on patient-safety culture in hospitals.12 Assessing the existing safety culture in a hospital is the first stage of developing a patient-safety culture.13
In developed countries, though patient safety is now recognized as a top priority for hospital managers and policy-makers,14 the adverse medical events remain a significant source of morbidity and mortality across the globe, and no country has yet overcome all of its patient-safety problems.15 Data from well-funded and technologically advanced hospitals have shown that one in every ten patients admitted to hospital is affected by an adverse event (incidence rate of 10%).16
The situation is thought to be more challenging in developing countries, with higher risk of patient harm due to the limitation in resources, infrastructures, technologies, and human resources.17 Though evidence is limited in developing countries, the probability of patients being harmed in hospitals when receiving care might be much greater than that of industrialized nations. For instance, a report has claimed that the risk of health care–associated infection in developing countries is up to 20 times that of developed countries.18
According to research done on patient safety in developing countries — two African countries (Kenya and South Africa) and six Eastern Mediterranean countries (Egypt, Jordan, Morocco, Sudan, Tunisia, and Yemen) — in 26 hospitals with a cross-sectional survey showed that almost a third of patients who suffered a harmful incident died, 14% sustained permanent disability, 16% sustained moderate disability, 30% were left with minimal disability, and 8% of the patient harm could not be specified.19 When people receive health care, errors associated with care may result in serious harm, such as death, disability, or additional prolonged treatment. Also such errors may cause indirect health-care costs and productivity losses and affect customer perceptions, attitudes, and trust and providers’ confidence and integrity.20,21
In Africa, little is known and information is limited in scope about patient-safety culture.22 A WHO report stated that most countries in the African region lack national policies on safe health-care practices. Inappropriate funding and unavailability of critical support systems, including strategies, guidelines, tools, and patient-safety standards remain major concerns in Africa. Additionally, the report implied that understanding of the problems associated with patient safety was hampered by inadequate data.23
In Ethiopia, there is little empirical evidence on patient-safety culture and medical errors. However, circumstantial evidence shows that almost all medical errors have been treated traditionally through blaming, shaming, and punishment and most medical errors not reported or even hidden. Consequently, health-care workers and managers are not in a position to learn from mistakes committed in health-care organizations.24 Most tangible evidence on patient-safety culture comes from developed countries.25 Patient-safety culture is a relatively new focus, and little is known regarding its current status in public hospitals. Some studies done in Ethiopia found low overall levels of patient safety culture — 46.7%26 and 46%27 — and most patient safety culture–dimensions score also very low, which in turn become areas of improvement/intervention. Nevertheless, one of the ultimate aims of the Ethiopian National Health Care Quality strategy is to consistently ensure and improve patient safety. To contribute to this strategy, this study aimed to assess levels of patient-safety culture and try to identify associated factors among health-care workers of East Wollega Zone hospitals.
Methods
Study Design and Setting
This cross-sectional study was conducted from March 4 to 29, 2019, in East Wollega Zone. East Wollega Zone is one of the 18 zones in Oromia Regional State, with an area of 12,580 km2. It has 17 woredas (equivalent to districts) and one town. Nekemte is the zonal town, 328 km west of Addis Ababa. The zone has 2,413 health professionals of different categories, five public hospitals (two referral, one general, and two primary), 57 health centers, and 325 health posts. The hospitals deliver services in gynecology and obstetrics, surgery, pediatrics and child health, internal medicine, ophthalmology, and dentistry.
Study Participants
All health-care workers in the five public hospitals of East Wollega (Wollega University Referral Hospital, Nekemte Referral Hospital, Gidda Ayana General Hospital, Arjo Primary Hospital, and Sire Primary hospital) were the source population for this study. Those who had worked for at least 6 months were included. Sample size was determined using a single population-proportion formula with the assumption of an overall level of patient-safety culture of 46.7% from a recent study in hospitals of Jimma Zone,26 a 95% CI, and 5% margin of error. After considering a 10% nonresponse rate, the final sample size was 421 health-care workers. The sample size for each hospital was determined proportionally. In each hospital, health-care workers were stratified according to their profession. The number of sample point was determined by using a proportional-allocation formula for each stratum. Then, the required sample was selected using simple random sampling from each stratum/profession.
Data-Collection Tools and Procedures
The Hospital Survey on Patient Safety Culture (HSOPSC) developed by the Agency for Healthcare Research and Quality in the US was used.28 The original HSOPSC has been validated in US hospital settings29 and has already been used in other countries, such as Saudi Arabia, Canada, the UK, Belgium, Denmark, Norway, Taiwan, Egypt, Tunisia, and Ethiopia. Most items in the survey tool use the 5-point Likert scale of agreement (strongly disagree to strongly agree), and a few other items rate frequency of events (never to always). The survey measures seven unit-level aspects of safety culture with 24 items: supervisor/manager expectations and actions promoting safety (four items), organizational learning for continuous improvement (three items), teamwork within units (four items), communication openness (three items), feedback and communication about errors (three items), nonpunitive response to error (three items), and staffing (four items). The survey also measures three hospital-level aspects of safety culture with eleven items: hospital-management support for patient safety (three items), teamwork across hospital units (four items), hospital handoffs and transitions (four items), and outcomes of safety culture and overall perceptions of patient safety (four items). As such, a total of 39 HSOPSC items were used. Frequency of events reported was excluded in this study, because of no/ poor event-reporting system in Ethiopia. The instrument also includes 14 items that respondents were asked to provide limited background informationon.
Data were collected through structured self-administered questionnaires. Five diploma- and two bachelor-level nurses were assigned as data collectors and supervisors, respectively. These were recruited from health facilities outside the study hospitals. After data collectors had explained the purpose of the study and ensured willingness of the study participants, questionnaires were administered. Participants were allowed to complete the questionnaire whenever they could and return them during the data-collection period.
Study Variables
The outcome variable in this study was level of patient-safety culture among health-care workers. Independent variables were sociodemographic characteristics of the health workers, including sex, age, marital status, monthly salary, professional category, and education. Other covariates were type/level of hospital, working units, duration of employment at the current hospital, work experience in the current job, working hours per week, direct contact with patients, patient safety–training status, and participation in patient-safety programs.
Data Analysis
Data were checked, edited, coded, and entered into EpiData version 3.1 and exported to SPSS version 25 for further analysis. Descriptive statistics (frequencies, means, SD, percentages) were used to summarize sociodemographic and individual factors. Levels of patient-safety culture were measured by percentages of positive responses (agree and strongly agree or most of the time and always) for the eleven patient safety–culture dimensions. The levels were categorized as good, moderate, and poor/low patient-safety culture, with scores of ≥75%, 50%–70%, and <50%, respectively.29 Composite-level scores were computed by summation of the item within the composite scale and dividing by the number of items. Scores of negatively worded items were reversed to ensure that higher scores always reflected more positive responses. The Likert-type scale was converted to a 100-point scale (1=0, 2=25, 3=50, 4=75, and 5=100).
A linear regression model was fitted to identify factors associated with patient-safety culture. Patient-safety culture was regressed against sociodemographic and individual factors. Before fitting the linear regression model, assumptions were checked: linearity was checked through scatterplots, normality by plotting histograms and P–P plots, homoscedasticity with scatterplots of standardized residuals against standardized predicted values, and autocorrelations using the Durbin–Watson test. The value of the Durbin–Watson statistic for these data was 1.61, within the acceptable range of 1.5–2.5. The multicollinearity assumption was checked through the variance inflation factor, which was <10 for each independent variable. Accordingly, all assumptions were satisfied. Bivariate linear regression analysis was performed and variables with p<0.25 exported to the multivariate linear regression analysis. Significance was declared at 95% CI and p<0.05, and unstandardized β-coefficients were used for interpretation.
Ethical Considerations
Ethical clearance was obtained from the Institutional Review Board of the Institute of Health, Jimma University, and from the Oromia Regional Health Bureau Ethical Review Committee. A letter of support was obtained from the East Wollega Zone Health Department. These letters were delivered to the chief executive officer of each hospital. The purpose and importance of the study was explained to the participants. Data were collected after written informed consent had been obtained, and confidentiality of information was maintained by omitting their names and personal identifiers.
Results
Characteristics of Study Participants
Of the 421 questionnaires distributed to different departments/units in the five public hospitals, 388 were fully completed and returned, giving a response rate of 92.2%. Of the 388 respondents, 238 (61.3%) were males and more than half (212, 54.6%) ≤29 years old, and 251 (64.7%) were from referral/specialized hospitals. In terms of professional category, 171 (44.1%) were nurses, followed by physicians (64, 16.5%), and about a third of participants worked in medicine, surgery, and laboratory units. A majority (79.6%) of respondents had ≤5 years of work experience. Of the 388 study participants, 313 (80.7%) had direct interaction or contact with patients, and 244 (62.9%) had not received any training on patient safety (Table 1).
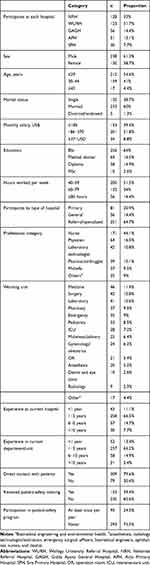 |
Table 1 Sociodemographic and individual characteristics of study participants (n=388) |
Level of Patient-Safety Culture
The overall level of patient-safety culture was 49.2% (95% CI 47.6%–50.9%). The highest average positive percentage response was 77.9% for teamwork within hospital units. The lowest average positive percentage scores that may require potential improvements were nonpunitive responses to errors, staffing, handoffs, and transitions (Table 2).
 |
Table 2 Patient safety–culture dimensions: average positive-response scores (n=388) |
Predictors of Patient-Safety Culture
After variables had been computed and assumptions checked, bivariate analysis on the linear regression model was done for each independent variable with the dependent variable, and those with p<0.25 were selected for further analysis. Accordingly, 19 variables — age ≥45, monthly salary (≤US$185 and $186–$370), type of hospital (primary and general), profession (nurse, midwifery, laboratory, and others), working unit (medicine, pediatrics, delivery, emergency, laboratory, and others), experience of 1–5 years at the current hospital, and education (general practitioner, BSc, and diploma) — were selected as candidates for multiple linear regression (Table 3).
 |
Table 3 Bivariate analysis of predictors of patient-safety culture among health-care providers (n=388) |
Multivariate Linear Regression Analysis to Identify Predictors of Patient-Safety Culture
Multivariate analysis showed that scores of respondents whose age was ≥45 years, had worked 1–5 years in the current hospital, worked in a general hospital, and worked in primary hospital found to be significantly higher (Table 4).
 |
Table 4 Predictors of patient-safety culture among health-care workers (n=388) |
Discussion
The percentage of positive responses among the health workers in our study was low — 49.2% (95% CI 47.6%–50.9%). This showed that the hospitals had poor/low patient-safety culture, and areas with the most potential for improvement need urgent action. This finding is similar to earlier ones, which ranged from 46% in Ethiopia to 48% in India.26,27,30 However, our finding was much lower than those reported from Taiwan (64%),31 Saudi Arabia (61%),32 Lebanon (61.5%),33 the US (62%),34 Sri Lanka (62.7%),35 and China (65%).36 Although infrastructural and economic differences among settings could explain part of these differences, the role of management and organizational commitment, leadership, and relationships among hospital staff should have played a role.
In this study, teamwork within hospital units was the only area of strength, with an average positive-response rate of nearly 80%. Similar findings have been reported for this dimension from different countries.26,31,32,33,36 This shows that staff are supporting one another, treat one another with respect, work together as a team, and doing things to improve patient safety. This is an opportunity health managers could grab to enhance patient-safety culture in their health-care organization. On the other hand, the area with the most potential for improvement in this study was nonpunitive response to error. Others have also reported findings as low as or even lower than ours from different countries for this dimension.27,32,33,37 This implies that a punitive approach and managerial inaction to promote patient safety is common to different countries, though better patient-safety culture for this dimension has been reported from the Netherlands (66%)1 and China (60%).13 This wide gap between health systems implies that it is possible to establish event-reporting systems that are blame-free but enhance accountability. Health-care workers in settings similar to our study area feel that their mistakes are held against them and worry that mistakes they make are kept in their personnel file. This discourages workers from reporting critical incidents that could be used for future learning and improvement of patient safety.
Another potential for improvement in this study area was staffing (32%). Most respondents felt that staff allocation was not adequate to handle patient safety–related workload. Health workers from other countries have also reported the same feeling.26,27,30,32,33,38,39 However, our finding was lower than those of the Netherlands (59%)25 and US (54%).34 Looking at this difference, one may easily assume that this difference relates to number and mix of health professionals in a country. While that may well be true, the role of style of leadership and priority-setting in staff allocation in the health-care organization are also important drivers.
Hospital handoffs and transition (36.2%) was another area of potential for improvement in this study. This is slightly comparable with studies conducted in India (43%),30 the Netherlands (42%),25 and Ethiopia (41%, 33%).26,27 This result shows that important patient-care information might not be well transferred across hospital units, often lost during shift changes, and problems often occur in the exchange of information across hospital units. Earlier studies have reported much worse scores in this regard. Results as high as 60%–74.5% have been recorded in studies from Sri Lanka,35 Iran,40 and Saudi Arabia.32 This difference might be related to lack of teamwork across units and lack of handoff and clear transition procedures within these hospitals.
Management support for patient safety was the next area of potential for improvement in this study. Previous similar studies from Palestine38 and Ethiopia26,27 have also implied that hospital managers did not provide a work climate that promoted patient safety and that patient safety was not a priority in their facility, while findings from other settings, including Sri Lanka,35 Saudi Arabia,41 and China,42 indicated that patient safety can become a top priority of health facilities in different contexts. This implies that whether a setting is resource-constrained or has surplus supplies, the orientation of the managers toward patient safety is a key issue.
It is also interesting to see other potential areas for improvement. Supervisor expectations and actions, overall perceptions of patient safety, communication openness, feedback, and communication about errors were areas that need improvement. This means managers do not consider staff suggestions for improving patient safety, do not praise staff for following patient-safety procedures, may overlook patient-safety problems, and that procedures and systems are not good at preventing errors. As such, staff will not speak up freely if they see something that may negatively affect a patient and not feel free to question those with more authority. It also means staff are not informed about errors that happen, are not given feedback about changes implemented, and will not be able to discuss ways to prevent errors. Generally, the results of this study highlight deficiencies in many patient safety–culture components and indicate that there are areas of for potential improvement requiring urgent attention.
According to this study, for every unit increase in scores of respondents at the current hospital (1–5 years), the patient safety–culture score improved by 5.559 (β=5.559, 95% CI, 2.075–9.042) when compared to those of with experience of l<1 year. This finding is again in line with a study conducted in Tunisia.43 This suggests that more experience in clinical care renders better orientation in ensuring patient safety. Therefore, medical schools should actively motivate their trainees and trainers in the importance of patient safety in any clinical care exposure, even during preservice training programs. Similarly, we found that each unit increase in scores of respondents aged ≥45 years increased patient safety–culture scores by 13.642 compared with those aged ≤29 years (β=13.642, 95% CI 5.324–21.959). This finding agrees with the study conducted in Riyadh.44
In our study, participants working in primary and general hospitals showed higher patient safety–culture scores (β=6.408, 95% CI 2.192–10.624 and β=11.988, 95% CI 7.233–16.743) compared to referral or specialized hospitals, respectively. The studies conducted in Riyadh44 and Tunisia43 support this finding. This implies that larger organizations are more hierarchical and bureaucratic implementation of quality initiatives challenging, which also affects employees’ attachment to these organizations and consequently their performance. Evidence from international literature links small hospital capacity (<100 beds) to increased formal organizational leadership in relation to patient-safety events. This is due to the fact that in small hospitals (where the economic burden of safety programs may be large), formal leadership is closer to the front lines and has a greater impact on patient safety than in larger hospitals.45
Our study used widely validated data-collection tools tested in different settings. However, there were limitations. First, since we asked the health workers to evaluate their own culture, there is a possibility of social-desirability bias potentially inflating positive responses. We used negatively worded items to minimize such a possibility. Furthermore, our study did not include verification of findings through document review and/or key informant interviews, which could have improved the strength of conclusions from this study.
Conclusion
This study showed that patient-safety culture and average percentage of positive scores on patient safety–culture components in East Wollega Zone public hospitals were lower than the Agency for Healthcare Research and Quality benchmark. Teamwork within hospital units was the only area of strength, and most of the patient safety–culture dimensions were areas for potential improvement. Improving the existing situation would require paying attention to thoseareas for potential improvement we have reported here. Particular emphasis should be put on the importance of the establishment of blameless event-reporting systems, risk free hospital handoffs and transitions, and appropriate staffing and management support to patient-safety initiatives. Mechanisms to retain experienced professionals within each type of hospital should be considered.
Data-Sharing Statement
Data are available from the principal investigator and corresponding author upon reasonable request.
Acknowledgment
We would like to thank Jimma University for funding the study. Our appreciation also goes to all study participants for their kind cooperation.
Author Contributions
All authors contributed to conception and design of the study, acquisition of data, data analysis and interpretation, funding acquisition, and drafting and revising the manuscript, gave final approval for submission and the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no financial or other competing interests.
References
1. WHO. Patient safety. 2014. Available from: http://www.who.int/patientsafety/en/. Accessed June 24, 2020.
2. Achakzai H. Assessing Patient Safety Culture In Public Hospitals Under The Essential Package of Hospital Services (EPHS) in Afghanistan. 2014.
3. Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC (US): National Academy Press; 2001.
4. Retrived W. 2014. http://www.ahrq.gov/professionals/quality patient safety/patient safety culture/hospital/user guide/hospcult1.html. Accessed June 24, 2020.
5. Mc Charthy N, Blumenthal D. Stories from the sharp end: case studies in safety improvement. Milbank Quart. 2006;84(1):165–200. doi:10.1111/j.1468-0009.2006.00442.x
6. Marlene DM. Improving Patient Safety: Safety Culture and Patient Safety Ethics. 87. Denmark ISBN: Risø NLISD; 2006:550–35205.
7. WHO. World alliance for patient safety. Summary Evidence Patient Safety. 2008. Available from: https://apps.who.int/iris/handle/10665/43874. Accessed July 26, 2020.
8. Gillian R, Mary S. Measuring the safety culture in a hospital setting. J New Zealand Med Assoc. 2010;123:1314.
9. Helmreich RL, Merritt AC. Culture at Work in Aviation and Medicine. Burlington,US: Routledge; 2001.
10. Guide Us. AHRQ hospital survey on patient safety culture. Agency Healthcare Res Qual. 2016. Available from: http://www.ahrq.gov/. Accessed July 26, 2020.
11. Martin WF. Is your hospital safe? Disruptive behavior and workplace bullying. Hosp Top. 2008;86:21–28. doi:10.3200/HTPS.86.3.21-28
12. El-Jardali F, Dimassi H, Jamal D, et al. Predictors and outcomes of patient safety culture in hospital. BMC Health Serv Res. 2011;24:45. doi:10.1186/1472-6963-11-45
13. Hellings JE, Schrooten W, Klazinga N, Vleugels A. Challenging patient safety culture: survey results. Int J Health Care Qual Assur. 2007;20(7):620–632. doi:10.1108/09526860710822752
14. Institute of Medicine; Board on Health Care Services; Committee on Data Standards for Patient Safety. Patient Safety, Achieving a New Standard for Care. Aspden P, Corrigan JM, Wolcott J, Erickson SM, editors. Washington, DC: The National Academies Press; 2004.
15. World Health Organization. African Partnerships for Patient Safety. Geneva; 2009.
16. Adams RE, Boscarino JA. A community survey of medical errors in New York. Int J Qual Health Care. 2004;16:353–362. doi:10.1093/intqhc/mzh063
17. WHO. WHO Patient Safety Research. Geneva: World Health Organization; 2009.
18. News TM. Hand hygiene initiative aims to decrease healthcare associated infection in developing countries. Med News. 2007;21:35.
19. WHO. Patient Safety in Developing and Transitional Countries: New Insights From Africa and the Eastern Mediterranean. 2011:16–20.
20. Medical News. Hand hygiene initiative aims to decrease healthcare associated infection in developing countries. Med News. 2007;21:35.
21. Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Joint Com- Mission J Qual Patient Safety. 2007;33:467–476. doi:10.1016/S1553-7250(07)33050-X
22. Powell S, Bailey D, Ndili N, Ente C. Patient safety in Africa: a culture shift? BMJ. 2011. Available from: https://www.psqh.com/analysis/patient-safety-in-africa-a-culture-shift/ Accessed July 26, 2020.
23. WHO R. Patient Safety in African Health Services: Issues and Solutions. Yaounde: Republic of Cameroon; 2008.
24. Assefa T, Woldie M, Ololo S, Woldemichael K. Patient safety practices and medical errors: perception of health care providers at Jimma University Specialized Hospital, Southwest Ethiopia. Open Journal of Preventive Medicine. 2012;2:162–170.
25. Wagner C, Smits M, Sorra J, Huang CC. Assessing patient safety culture in hospitals across countries. Int J Qual Health Care. 2013;25(3):213–221. doi:10.1093/intqhc/mzt024
26. Wami SD, Demssie AF, Wassie MM, Ah, ed AN. Patient safety culture and associated factors: A quantitative and qualitative study of healthcare workers’ view in Jimma zone Hospitals, Southwest Ethiopia. BMC Health Serv Res. 2016;16:495. doi:10.1186/s12913-016-1757-z
27. Alemayehu B, Mekonnen, Andrew J, et al. Hospital survey on patient safety culture in Ethiopian public hospitals: a cross sectional study. Safety in Health. 2017;3:11. doi:10.1186/s40886-017-0062-9
28. Sorra JS, Nieva V. Hospital survey on patient safety culture. Agency Health Care Res Qual. 2004;04-0041.
29. Sorra JS, Dyer N. Multi-level psychometric properties of the AHRQ Hospital survey on patient safety culture. BMC Health Serv Res. 2010;10:199. doi:10.1186/1472-6963-10-199
30. Rao MTD, Srinivas P. A study to assess patient safety culture amongst a category of hospital staff of a teaching hospital. IOSR J Dent Med Sci. 2014;13:3.
31. Chen I-C, Li H-H. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv Res. 2010;10(1):152. doi:10.1186/1472-6963-10-152
32. Alahmadi HA. Assessment of patient safety culture in Saudi Arabian hospitals. Qual Saf Health Care. 2010;19(5):e17.
33. El-Jardali F, Jaafar M, Dimassi H, Jamal D, Hamdan R. The current state of patient safety culture in Lebanese hospitals: a study at baseline. Int J Qual Health Care. 2010;22(5):386–395. doi:10.1093/intqhc/mzq047
34. Famolaro TYN, Burns W, Flashner E, Liu H. Prepared by Westat, Rockville, MD hospital survey on patient safety culture 2016 user comparative database report. Agency Health Care Res Qual. 2016;
35. Amarapathy M, Sridharan S, Perera R, Handa Y. Factors affecting patient safety culture in a tertiary care hospital in Sri Lanka. International Journal of Scientific & Technology Research. 2013;2(3):173–180.
36. Nie YL, Mao X, Cui H, He S, Li J, Zhang M. Hospital survey on patient safety culture in China. BMC Health Serv Res. 2013;13:228. doi:10.1186/1472-6963-13-228
37. Aboul-Fotouh AM, Ismail NA, Ez Elarab HS, Wassif GO. Assessment of patient safety culture among healthcare providers at a teaching hospital in Cairo, Egypt. East Mediterr Health J. 2012;18(4):372–377. doi:10.26719/2012.18.4.372
38. Hamdan MSA. Assessment of patient safety culture in Palestinian public hospitals. Int J Qual Health Care. 2013;25(2):167–175. doi:10.1093/intqhc/mzt007
39. Fujita S, Seto K, Ito S, Wu Y, Huang C-C Hasegawa T. The characteristics of patient safety culture in Japan, Taiwan and the United States. BMC Health Serv Res. 2013;13(1):20. doi:10.1186/1472-6963-13-20
40. Mohammadreza AST, Omid B. Measuring safety culture and setting priorities for action at an Iranian hospital. Al Ameen J Med Sci. 2010;3(3):237–245.
41. Alahmadi HA. Assessment of patient safety culture in Saudi Arabian hospitals. QSHC BMJ. 2010;19(5):e17. doi:10.1136/qshc.2009.033258
42. Nie Y, Mao X, Cui H, He S, Li J, Zhang M. Hospital survey on patient safety culture in China. BMC Health Serv Res. 2013;13:228. doi:10.1186/1472-6963-13-228
43. Rejeb MB, Chebil D, Merzougui L, et al. Patient safety culture in a tunisian teaching tertiary care hospital. Arch Nurs Pract Care. 2017;3(1):077–083.
44. El-Jardali F, Sheikh F, Garcia NA, et al. Patient safety culture in a large teaching hospital in Riyadh: baseline assessment, comparative analysis and opportu nities for improvement. BMC Health Serv Res. 2014;14:122.
45. Ginsburg LR, Chuan YT, Berta WB. The relationship between organizational leadership for safety and learning from patient safety events. Health Ser v Res. 2010;45(3):607–663. doi:10.1111/j.1475-6773.2010.01102.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
