Back to Journals » Open Access Emergency Medicine » Volume 11
Are serial hematocrit measurements sensitive enough to predict intra-abdominal injuries in blunt abdominal trauma?
Authors Mosaddegh R, Ashayeri N, Rezai M, Masoumi G , Vaziri S, Mohammadi F, Givzadeh H, Noohi N
Received 16 July 2018
Accepted for publication 23 October 2018
Published 7 January 2019 Volume 2019:11 Pages 9—13
DOI https://doi.org/10.2147/OAEM.S180398
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Reza Mosaddegh,1 Neda Ashayeri,2 Mahdi Rezai,1 Gholamreza Masoumi,3 Samira Vaziri,1 Fatemeh Mohammadi,4 Hamed Givzadeh,5 Nasrin Noohi1
1Emergency Medicine Management Research Center, Iran University of Medical Sciences, Tehran, Iran; 2Department of Pediatric Hematology and Oncology, Ali Asghar Children’s Hospital, Iran University of Medical Sciences, Tehran, Iran; 3Trauma and Injury Research Center, Iran University of Medical Sciences, Tehran, Iran; 4Research and Development Center of Firoozgar Hospital, Iran University of Medical Sciences, Tehran, Iran; 5Orthopedic Research Center, Guilan University of Medical Sciences, Rasht, Iran
Objective: Routine serial hematocrit measurements are a component of the trauma evaluation for patients without serious injury identified on initial evaluation. We sought to determine whether serial hematocrit testing was useful in predicting the probable injuries in blunt abdominal trauma.
Materials and method: We performed a prospective study of trauma patients admitted in our observation unit over a 12-month period. Patients routinely underwent serial hematocrit testing in 6-hour intervals (two hematocrit levels). We compared trauma patients with a hematocrit drop of 5 and 10 points or more to those without a significant hematocrit drop.
Results: Five hundred forty-two isolated blunt abdominal trauma patients were admitted to observation unit, and 468 patients (86.35%) had serial hematocrit during their 6-hour stay. Of these patients, 36.11% had a hematocrit drop of 5 or more and 12.61% a drop of 10 or more. Of patients with the hematocrit drop >10, 50.8% have had diagnostic manifestations of intra-abdominal injury in both ultrasonographic and computed tomography scanning (P<0.001). There was no significant correlation between hematocrit drop >5 and positive imaging.
Conclusion: Although serial hematocrit testing may be useful in specific situations, routine use of serial hematocrit testing in trauma patients at a level I trauma center’s observation unit did not significantly aid in the prediction of occult injuries.
Keywords: Blunt abdominal trauma, serial hematocrit, ultrasonography, computed tomography
Introduction
Trauma is the first leading cause of mortality all over the world and most of the victims are among people aged 14–44 years.1 In 2015, WHO reported that accidents were responsible for 8.1% of deaths in Iran.2 Also, surveys have shown that abdominoplevic trauma is a main cause of morbidity and mortality in trauma patients.3 Patients are referred to emergency department because abdominal trauma may have vague symptoms and signs, and estimating of the severity of injury through abdominal examination is difficult and is not reliably possible.4–6
The benefit of serial hematocrit measurement for diagnosis of intra-abdominal injuries has been assessed in some studies and it can be used as a screening tool in trauma patients.7,8 Zehtabchi et al found that a change in hematocrit of >5 points in 4 hours predicted serious injury.7 Another study that was performed in patients with penetrating trauma stated that a hematocrit change of 6.5 points at 15 minutes predicts significant injury.8
The aim of the present study was to evaluate whether serial hematocrit testing could precisely predict intra-abdominal injuries in blunt abdominal trauma patients.
Materials and methods
Design and ethics
This prospective study was performed on patients admitted to emergency department of Firoozgar University Hospital from May 1, 2014 to April 31, 2016. Firoozgar Hospital is a teaching hospital located at downtown of Tehran, Iran, as a level I trauma center. The ethics committee of Iran University of Medical Sciences approved the study.
Participants
We enrolled patients referred to emergency department with blunt trauma after obtaining written informed consent form from all patients. This study was conducted in accordance with the Declaration of Helsinki. All types of trauma such as motor vehicle collision, falling from height, and fighting were included the study. Exclusion criteria were patient death before completion of evaluations, penetrating abdominal trauma, necessity for blood transfusion in the first 6 hours of admission, abnormal electrocardiogram, abnormal head computed tomography (CT) scan, Glasgow Coma Scale score <14, injuries resulting in immediate transferring to operation room before 6 hours.
Process and assessment
In our emergency department the trauma patients are managed according to advanced Trauma Life Support instructions and algorithms. The primary and secondary surveys were done by emergency medicine residents supervised by emergency medicine attendings. The focused assessment with sonography for trauma (FAST exam) and chest radiography were done as an adjunct to primary survey. General surgeon, neurosurgeon, and orthopedic surgeon visited the patients if needed.
In our emergency department, the trauma patients are allocated to subacute and acute area according to severity of trauma and observed by emergency medicine residents. Other ancillary tests such as supplementary radiographies and laboratory tests are pursued in those areas. As part of the observation, especially surgeons, checked hematocrit levels every 6 hours to aid in the detection of occult hemorrhagic injuries that may not have been identified in the initial trauma assessment by FAST exam and CT scanning. Physicians might order spiral abdominopelvic CT scans with intravenous contrast for some trauma patients who had indication according to trauma guidelines or their judgments.
Post graduate year 3 emergency medicine residents reviewed all diagnostic and therapeutic processes of admitted trauma patients. They recorded patient characteristics, injuries, hematocrit levels, length of stay, results of FAST exam and spiral abdominopelvic CT scanning. Also the adverse outcomes including instability of vital signs, advanced airway management (intubation), death, and whether these patients were discharged from the hospital or admitted to an inpatient ward were also recorded. Significant intra-abdominal injury was defined as any injury detected during observation period that required operative repair or hospitalization in an inpatient ward.
Patients were considered to have a hematocrit drop of 5 points or more if any of the hematocrit levels after the initial hematocrit level (which was drawn on patient’s ED admission) was 5 points or more lower. We used a hematocrit decrease of 5 points or more based on the previous study that established this threshold as a predictor of intra-abdominal injury.7 We also considered a hematocrit drop of 10 or more to assess whether the diagnostic values changed or not.
We also followed up patients to identify outcome 30 days after trauma. The hematocrit drop and its relationship with the results of ultrasound and CT scans were assessed to determine the diagnostic values (sensitivity and specificity) of these drops.
Statistics
All statistical analyses were performed using SPSS 16.0 (SPSS Inc. Chicago, IL, USA). Quantitative descriptive data were reported using mean with 95% CI. To determine the diagnostic value of hematocrit drop in trauma patients, indicators of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive and negative likelihood ratio were calculated. The level of significance was considered <5%.
Results
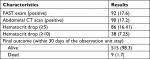
During the study period, 617 patients were admitted to the observation unit, and 524 patients (85%) had at least two hematocrits results between their initial evaluation and their observation unit stays. The observation unit trauma protocol called for hematocrit levels to be drawn every 6 hours. All the patients observed in this unit suffered from isolated sustained blunt trauma. The most common specific mechanism was motor vehicle accident (331/524, 63.2%). Of the patients, 79.2% were male, and average age was 32.3 years (median age, 24 years; Table 1).
  | Table 1 Data of patients |
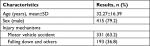
All patients had received primary and secondary trauma surveys, including FAST exam and CT scanning per the trauma team discretion. All the trauma patients had a FAST Exam (initially and serial according to the severity of injury and order of attending physician), and of these, 92 patients (17.6%) had positive FAST (free fluid in abdomen or pelvis cavity). One hundred seventy-five patients (32.29%) had a CT scan of the abdomen and pelvis performed before admission to the observation unit and of these 90 patients (17.2%) had a positive scanning and showed intra-abdominal or pelvis injuries or hematoma (Table 2).
The average changes in hematocrit were a decrease of 3.64% (median, 3% decrease).
Of the 524 patients, 86 (16.41%) had a hematocrit drop of 5 points or more during their observation unit stay. The hematocrit drop of 10 points or more was seen in 38 patients (7.25%). Comparison between patients with a significant hematocrit drop (≥5% and ≥10%) and those without are listed in Table 2.
Thirty-three (38.4%) of patients with a hematocrit drop of 5% or more had an abnormal FAST exam vs 59 (13.5%) of patients without a significant hematocrit drop (P=0.324; OR =1.27; 95% CI, 0.792–2.039). In patients with a hematocrit drop of 10 points or more, 30 (78.9%) patients had an abnormal FAST vs 62 (12.7%) of patients without a significant hematocrit drop (P<0.001; OR =6.72; 95% CI, 3.779–11.964).
Thirty-three (38.4%) of patients with a hematocrit drop of 5% or more had abnormal CT scans vs 57 (13.0%) of patients without a significant hematocrit drop (P=0.263; OR =1.325; 95% CI, 0.824–2.130). In patients with a hematocrit drop of 10% or more, 30 (78.9% ) patients had abnormal CT scans vs 60 (12.3%) patients without a significant hematocrit drop (P<0.001; OR =6.983; 95% CI, 3.918–12.446; Table 3).
In our study, trauma patients who had intra-abdominal injuries seen in CT scan images were admitted to intensive care units (ICUs) or sent for laparotomy. Thus, we can conclude that an Hct drop of 10% or more was associated with ICU care or laparotomy (P<0.001).
This study showed that a hematocrit drop of 5% or more has 35.87% sensitivity, 69.45% specificity, 20% PPV, and 83.56% NPV for abnormal FAST. The sensitivity and specificity for abnormal abdominopelvic CT scanning were 36.67% and 69.58%, respectively, and PPV and NPV for abnormal abdominopelvic CT scanning were 20.0% and 84.12%, respectively (Table 4).
According to the results of this study, the hematocrit drop of 10% or more had 32.61% sensitivity, 93.29% specificity, 50.85% PPV, and 86.67% NPV for abnormal FAST exam, whereas, the sensitivity, specificity, PPV, and NPV for abnormal abdominopelvic CT scanning were 33.33%, 93.32%, 50.85%, and 87.10%, respectively (Table 4).
We used analysis of ROC curves to test the diagnostic performance of drop in hematocrit in predicting abnormal FAST examination and CT scanning in the study subjects. In this analysis, the area under the ROC curve was significantly different (P<0.001) from the unity line. Patient records were reviewed for 30 days after the observation unit visit. Only nine of these cases (1.7%) have died during stay in observation unit or the admitting service within 30-day follow-up. Eight of them (89%) suffered from intra-abdominal injuries (free fluid in FAST exam and CT scan images) and admitted to ICUs or operation room. We compared the hematocrit drop after 6 hours in survivors and nonsurvivors and found that there was no significant differences between the two groups (−3% vs –3.64%, P=0.642; Table 2).
Discussion
Currently, physical examination and imaging studies such as extended FAST and CT in trauma patients apply to determine the severity of injuries and blood loss, but in certain cases the diagnosis can be challenging.
Recently, bedside ultrasound in the initial assessment of trauma patients plays a significant role,9–11 and it’s sensitivity and specificity for the presence of intra-abdominal fluid in patients suffering from trauma is acceptable (75%–93.8% and 97%–100%, respectively).3,6 However, serial ultrasound examination may be needed in some situations11,12 and of course ultrasound is an operator-dependent modality.
Serial hematocrit measurements are one of current screening tests as part of the trauma assessment. The aim of serial hematocrit testing is to detect occult, and may be serious intra-abdominal injuries. However, dilution of blood due to infusion of intravenous fluids may decrease the diagnostic value of dropped hematocrit (DHct). Thus, we designed this study to test the diagnostic performance of DHct in a population of trauma patients. The operating characteristics of an efficient screening test require a high sensitivity and a low likelihood ratio of a negative test. These qualities will allow a negative screening test to strongly rule out patients for the disease in question.
In the present study, there was no significant difference between the normal and abnormal FAST examinations and CT scanning for DHct-6 h >5 points. The sensitivity of DHct-6 h >5 points in predicting normal FAST examination and CT scanning was low. Meanwhile there was a significant difference between the positive and negative FAST examinations and CT scanning for DHct-6 h >10%. Using a cutoff for DHct-6 h of 10% could not improve the sensitivity. Likelihood ratios using DHct-6 h of >10% had a higher +LR and a lower –LR in detecting positive FAST examination and CT scanning.
Previous studies have assessed DHct within 1 hour after blood loss.8,13–14 Paradis et al8 reported a sensitivity of 20% and 27% for DHct 15 and 30 minutes after ED arrival, respectively. Kass et al14 reported a sensitivity of >90% for DHct, 30 minutes following phlebotomy of 500 mL in healthy individuals. We chose 6-hour intervals to measure DHct. According to our analysis, DHct-6 h >5 points, and DHct-6 h >10 points showed low sensitivity in predicting abnormal FAST examination and CT scanning.
While the DHct proved to have a relatively low sensitivity, their specificity especially in DHct-6 h >10 points was quite high. These findings indicate that DHct could be a powerful test for ruling in abnormal FAST examination and CT scanning which could be indicative of major injury. A similarly high specificity was also found by Paradis et al.7
In summary, we showed that a drop in Hct greater than 5 and especially 10 points after 6 hours has a high specificity (>93%) and a high likelihood ratio for a positive test (4.7). A trauma patient who drops his/her Hct more than 5 or 10 points in 6 hours, compared with the one without a similar drop, has much higher odds of having major injury.
The low sensitivity and likelihood ratio of a negative test for the drop in hematocrit greater than 5 or 10 points indicates that these tests cannot be used to reliably rule out abnormal FAST examination and CT scanning which could be indicative of major injury. Trauma patients with DHct <5 or 10 points have approximately the same odds of having positive FAST examination and CT scanning.
There are several limitations to our study. The study analyzed a special section of trauma patients and our data represent only a portion of our hospital’s total trauma admissions. We excluded the severely injured patients with multiple organ involvement or unstable patients who received blood transfusion in order to more accurately study the effect of hemorrhage on hematocrit measurement. This exclusion, although inevitable, resulted in the elimination of a significant number of patients with major injury. Similarly, only the data of patients who stayed in the ED for 6 hours were analyzed; patients who were transferred to other units, such as the operating room, were not included in this analysis.
Conclusion
At a level I trauma center, in which patients receive a trauma evaluation and diagnostic testing before admission to the observation unit, the use of routine serial hematocrit testing as a screening tool during observation rarely provides additional diagnostic information. But in hospitals where emergency physicians or surgeons do not have access to CT scan machine, monitoring Hct changes can be helpful. We conclude that a drop in Hct of more than 10% during the first 6 hours is suggestive of positive imaging relative to major trauma (high specificity and +LR). However, the drop of Hct less than these degrees cannot be used to rule out abnormal imaging or major injury (low sensitivity and –LR).
Acknowledgments
The authors wish to thank all staff of Emergency Medicine Management Research Center for their kind help in all steps of this study. This study was supported by Iran University of Medical Sciences, Tehran, Iran.
Disclosure
The authors report no conflicts of interest in this work.
References
Center for Disease Control and Prevention. National Vital Statistics System. Atlanta, GA: National Center for Health Statistics; 2004. | ||
WHO. World Health Statistics 2015. Geneva: World Health Organization; 2015. | ||
Miniño AM, Heron MP, Murphy SL, Kochanek KD, Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep. 2007;55(19):1–119. | ||
Perez FG, O’Malley KF, Ross SE. Evaluation of the abdomen in intoxicated patients: is computed tomography scan or peritoneal lavage always indicated? Ann Emerg Med. 1991;20(5):500–502. | ||
Poletti PA, Mirvis SE, Shanmuganathan K, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;57(5):1072–1081. | ||
Rodriguez A, Dupriest RW, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457–459. | ||
Zehtabchi S, Sinert R, Goldman M, Kapitanyan R, Ballas J. Diagnostic performance of serial haematocrit measurements in identifying major injury in adult trauma patients. Injury. 2006;37(1):46–52. | ||
Paradis NA, Balter S, Davison CM, Simon G, Rose M. Hematocrit as a predictor of significant injury after penetrating trauma. Am J Emerg Med. 1997;15(3):224–228. | ||
Porter RS, Nester BA, Dalsey WC, et al. Use of ultrasound to determine need for laparotomy in trauma patients. Ann Emerg Med. 1997;29(3):323–330. | ||
Hoffmann R, Nerlich M, Muggia-Sullam M, et al. Blunt abdominal trauma in cases of multiple trauma evaluated by ultrasonography: a prospective analysis of 291 patients. J Trauma. 1992;32(4):452–458. | ||
Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879–885. | ||
Healey MA, Simons RK, Winchell RJ, et al. A prospective evaluation of abdominal ultrasound in blunt trauma: is it useful? J Trauma. 1996;40(6):875–885. | ||
Greenfield RH, Bessen HA, Henneman PL. Effect of crystalloid infusion on hematocrit and intravascular volume in healthy, nonbleeding subjects. Ann Emerg Med. 1989;18(1):51–55. | ||
Kass LE, Tien IY, Ushkow BS, Snyder HS. Prospective crossover study of the effect of phlebotomy and intravenous crystalloid on hematocrit. Acad Emerg Med. 1997;4(3):198–201. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.