Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Are pulmonologists well aware of planning safe air travel for patients with COPD? The SAFCOP study
Authors Ergan B , Arıkan H , Akgün M
Received 2 April 2019
Accepted for publication 1 August 2019
Published 22 August 2019 Volume 2019:14 Pages 1895—1900
DOI https://doi.org/10.2147/COPD.S210854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Begüm Ergan,1 Hüseyin Arıkan,2 Metin Akgün3
1Dokuz Eylul University, School of Medicine, Department of Pulmonary and Critical Care, Izmir, Turkey; 2Department of Internal Medicine, Yuzuncu Yil University, Dursun Odabas Health Center, Van, Turkey; 3Ataturk University, School of Medicine, Department of Pulmonary Diseases, Erzurum, Turkey
Correspondence: Begüm Ergan
Dokuz Eylul University School of Medicine, Department of Pulmonary and Critical Care, Izmir 35340, Turkey
Tel +90 232 412 3801
Email [email protected]
Background: Patients with respiratory diseases are more prone to health risks of air travel.
Purpose: The aim of this study was to investigate the current knowledge and attitudes of Turkish pulmonary physicians for air travel in patients with chronic obstructive pulmonary disease (COPD).
Participants and methods: A questionnaire was developed and administered either by congress mobile phone application or by e-mail. A total of 242 physicians participated in the study (75 by mobile phone application and 167 through the e-mail).
Results: Among participants, only 30.6% reported that they usually inform COPD patients about possible risks of air travel in their routine practice. A preflight assessment was performed by 61.2% of them and a fit to fly report was prepared by 34.3%. The most common methods/tests used for preflight assessment were reported as oxygen saturation with pulse oximetry, arterial blood gas analysis, and pulmonary function tests (51.2%, 50.8%, and 49.6%, respectively). When the participants were asked to plan safe air travel in two clinical case scenarios, only 16.2% were able to answer both cases correctly.
Conclusion: This study shows that a standard approach for preflight assessment in patients with COPD is lacking and an active initiative is needed to increase awareness and education for fit to fly concept for COPD among pulmonologists.
Keywords: pulmonologist, chronic obstructive pulmonary disease, air travel, hypoxemia, preflight assessment
Introduction
Air travel is one of the most preferred options for traveling throughout the world. It has been reported that a total of 4 billion passengers traveled by air in 2017.1 Although travel by air is considered to be relatively safe in healthy people, some specific populations may be prone to health risks during flight.2,3 A medical emergency occurs per 604 flights.4 Respiratory problems comprise approximately 12% of all in-flight emergencies, and are reported as the third most frequent cause of medical diversions.4 Most of those in-flight emergencies, around 65%, are associated with a pre-existing medical condition, of which 21% are respiratory problems.5
Hypobaric hypoxemia due to cabin altitude may cause health risks in patients with respiratory problems who have a limited cardiopulmonary reserve.6 Compared to healthy individuals, passengers with moderate-to-severe chronic obstructive pulmonary disease (COPD) have higher risk of experiencing significant hypoxemia during air travel.7,8 It was reported that around 25% of COPD patients experience hypoxemia-related symptoms during flight.9 Moreover, the medical risk of flying does not stop upon arrival to the destination. Another problem usually unnoticed is the need for health care utilization after flying. It was observed that unscheduled health care use in patients with respiratory problems is up to 20% within the first month after a flight.9
Therefore, it is crucial to inform and assess individuals who have high risk and fitness to fly concept should be integrated into the comprehensive management of COPD. It was previously reported that among respiratory problems, COPD is the most common disease for preflight evaluation.9 However, awareness and practices for fitness to fly among physicians and countries differ widely.10 The aim of this study was to investigate the current knowledge and attitudes of Turkish pulmonary physicians for a safe air travel in patients with COPD.
Methods
The Safe Air travel For COPD (SAFCOP) study was approved by the ethics committee of Marmara University (approval no.: 09.2018.283). A questionnaire was developed by the authors (BE; HA; MA) to understand the level of knowledge and current practice of pulmonologists for air travel in patients with COPD. The questionnaire consisted of 3 parts: the first part was for the demographics of the survey participants (age, gender, medical school graduation year, active practice duration in pulmonology field, number of patients/week), the second part dedicated to understand the current practice methods for preflight evaluation and the last part consisted of management of two case scenarios with different disease severities according to previous recommendations.6,7
The SAFCOP study was supported by the Turkish Thoracic Society (TTS). To reach as many participants as possible, the authors applied two-step approach. In the first step, the questionnaire was adapted to the mobile phone application of TTS Annual Congress and accessed during the congress. After downloading the congress application to their phones, congress participants were invited and asked to fill the questionnaire. The questionnaire was available throughout the congress, which was held between 11 and 15 April 2018. A reminder note was sent through the application on the second day of the congress. In the second step, an invitation for the questionnaire was sent to pulmonologists via an e-mail group of TTS two times in May 2018. Because of the nature of a survey study, informed consent was waived and all participants deemed to give consent after completing and sending back the questionnaire voluntarily. All data were recorded online.
Statistical methods
In this survey study, descriptive statistics were used to display patient characteristics. Numbers and percentages were used when applicable. Group differences were analyzed using chi-square test for categorical variables. A two-tailed P<0.05 was considered statistically significant. Statistical analysis was performed with SPSS (Statistical Package for the Social Sciences Version 20; IBM Corporation, Armonk, NY, USA) program.
Results
A total of 242 physicians participated in the study. During TTS 2018 congress, 851 registered participants downloaded the congress application to their mobile phones. Of them, 75 filled the questionnaire form through mobile phone application during the congress. In the second step, 167 participants filled the questionnaire through mail invitation. The total response rate was 8.8% for congress application and 11% (167/1504) for the mail.
Most of the participants were pulmonologist (98.3%). The most common workplaces were either in a university hospital (43.8%) or training and research hospital (30.6%) (Table 1). It was observed that all participants take care of COPD patients in their routine practice. The average number of COPD patients evaluated per week was reported as <20 patients in 31.4%, between 20 and 40 patients in 28.5% and more than 40 patients in 40.1% (Table 2). The estimated percentage of patients with moderate to severe COPD was reported as more than 50% of all COPD patients by 40.1% of participants.
 |
Table 1 Demographics of survey participants |
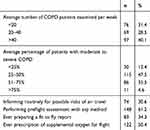 |
Table 2 Clinical practices of participants |
Among study participants, 74 (30.6%) reported that they usually inform patients about possible risks of air travel in their routine practice (Table 2). A preflight assessment was performed by 61.2% of them. A fit to fly report was prepared by 34.3% of all study participants and 50.4% declared that they have previously asked to prescribe supplemental oxygen for air travel.
The most common methods/tests used for preflight evaluation were reported as oxygen saturation with pulse oximetry, arterial blood gas (ABG) analysis, and pulmonary function tests (51.2%, 50.8%, and 49.6%, respectively; Figure 1). When the participants were asked about which tests they would prefer to use as the first-line method for preflight assessment, oxygen saturation with pulse oximetry and ABG analysis were the most commonly preferred tests (44.9% and 29.3%, respectively). Only one participant preferred hypoxic challenge test (HCT).
In the third part of the questionnaire, the participants were asked to plan safe air travel in two different clinical case scenarios (Box 1). The rate of correct answer was 24.8% for the first case scenario and 70.2% in the second. Only 16.2% answered both questions correctly. Participants who answered correctly to both case scenarios were not different than the ones who could not in terms of demographic characteristics (age, career status, working place) and experience for air travel (previous preparation of fit to fly report and prescription of supplemental oxygen).
 |
Box 1 Clinical case scenarios |
Discussion
The present survey study has two important results: First, although the percentage of COPD patients who should be informed for possible risks of air travel is relatively high, it was reported that only one-third of the pulmonologists routinely inform patients about potential risks of air travel. Second, a standard approach for preflight assessment is lacking and there is huge variability for the methods used among pulmonologists.
The airplane cabin altitude pressure is maintained at approximately 5000–8000 feet with cabin pressurization of approximately 520–570 mm Hg. As barometric pressure decreases, partial inspiratory oxygen pressure decreases and results in a drop in arterial oxygen tension to the equivalent of breathing 15.1% oxygen at sea level.11 Respiratory patients who are at risk may not tolerate this decline. Disease severity and presence of resting hypoxemia, flight duration, exercise taken at altitude such as walking on the aisle and presence of other comorbidities may influence the response to high altitude induced (hypobaric) hypoxemia.6,12 Moreover, with developing technology, the characteristics of air travel are also changing. Ultra-long-haul flights which are up to 20 hours and longer are increasing. Longer journeys are expected to increase the possible risk of in-flight medical incidents and physiological disturbances associated with hypoxemia. Therefore, COPD patients, particularly who have moderate to severe disease, should be informed for possible risks and preflight assessment should be considered in case needed.
The survey participants reported that about half of patients had moderate to severe COPD in their routine practice and only one-third of them inform patients about risks of air travel. On the other hand, more participants, about 60%, performed preflight assessment and half of them prescribed supplemental oxygen previously. The results show that preflight assessment is a relatively common condition in pulmonology clinics, yet systematic information for air travel did not become a part of routine practice. This discordance may be explained by preflight assessment and oxygen supplementation is usually considered only when it is requested either by the patient him/herself or by the airline company.
We have observed that oxygen saturation with pulse oximetry, ABG analysis, and pulmonary function tests are the most preferred tests for preflight assessment. However, several studies have shown that pulmonary function (forced expiratory volume in 1 s – FEV1), the partial pressure of oxygen and oxygen saturation may not predict inflight hypoxemia and therefore, the actual risk of flying.6,13–15 The ideal test for preflight evaluation is HCT but it is complex and expensive.11,16 In respiratory diseases, British Thoracic Society (BTS) recommends HCT when sea level oxygen saturation is <95%.6 This means that a lot of patients need to be assessed by HCT, which is not widely available. Edvardsen et al proposed that an algorithm that may be helpful for discriminating patients needing a referral to HCT.17 Oxygen saturation with pulse oximetry was measured in a group of patients with COPD at rest and during six-minute walk test (6MWT) and the results were compared with oxygen tension and saturation obtained during HCT. They proposed that extended preflight assessment with HCT might be limited to patients with either the combination of resting saturation >95% and severe exercise desaturation (<84%) and to patients with oxygen saturation between 92% and 95% without severe exercise desaturation (≥84%). It was shown that by adding 6MWT to assessment, the number of patients needing a referral to HCT was markedly reduced. However, new studies are needed to confirm these results. There may be some limitations of HCT as well. In a survey study, it was observed that about half of the patients with moderate to severe COPD had respiratory symptoms but there was no relationship between respiratory symptoms during air travel and the degree of hypoxemia during HCT.14
In the present study, HCT was not preferred by all participants except one. This result can be explained by two reasons: First, the test is currently unavailable in Turkey because it is not reimbursed by insurance systems. For that reason, we believe that, as a first step, respiratory societies should first focus on the reimbursement problem. Second, the pulmonologists may not be familiar to systematic preflight evaluation and therefore HCT. Hence, as a second step, in order to change the clinical practice nationwide, educational initiatives to increase knowledge for preflight evaluation among not only pulmonologists but also family physicians should be considered. Moreover, implementation of specific criteria and algorithms for identification of patients needing referral to preflight assessment is a requisite.
The wide range of the preferred tests for preflight evaluation is concordant with previous reports.9 One interesting finding of the present study was discordant correct answer rates to clinical case scenarios. It was observed that most of the pulmonologists answered correctly in a patient with chronic respiratory failure, whereas only 25% answered correctly the need for preflight evaluation in a high-risk patient. Several aviation authorities define high-risk patient populations, but they do not address disease specific preflight assessment methods.2,3,18 The most recent national guideline for the preflight assessment in stable pulmonary diseases is published by BTS but still, there is a lack of consistency in recommendations for COPD.6,17,19 Developing practical recommendations for comprehensive assessment and management of high-risk COPD patients is essential.
In this study, we have tried a new approach for surveying. Recently, mobile phone applications are being utilized more often for the electronic transfer of information during congresses. Although it seems a reasonable approach for a survey study because of its ease of use, the number of participants who filled the survey from an application remained low in the present study. Low response rate might be due to a couple of reasons such as low utilization of the congress application, a relatively new technique for participants and uninterest to the survey. Mobile phone application for survey studies is a promising tool and needs further testing.
There are some limitations of the study. First, the response rate was relatively low, and the survey was performed in Turkey, therefore, the results cannot be generalized. The study results are for COPD patients and we could not have a chance to understand the management of other respiratory diseases such as interstitial lung disease, kyphoscoliosis. Because of the study design (survey study), there is always a concern of recall bias. Finally, but most important, selection bias may have been occurred, as only physicians who have previously dealt with preflight assessment might have responded to the survey. On the other hand, the study has several strengths. It is one of the limited number of studies addressing the potential problem. The present study also shows that urgent intervention is needed to increase awareness and education for fit to fly concept among pulmonologists. Moreover, we believe that national and international guidelines for COPD and other respiratory diseases should refer to air travel, its potential risks, and management strategies.
Conclusion
Air travel is an essential activity of daily life. However, it may bring some health risks for passengers with limited cardiopulmonary reserve. From a physiologic point of view, every COPD patient with moderate and severe disease has increased risk of an adverse event during air travel and information of patients about fit to fly concept and preflight assessment is a requisite. Health care personnel taking care of these patients should be able to predefine and prevent possible risks. The current study suggests that an active initiative is needed to increase awareness and education for fit to fly concept among pulmonologists in Turkey. To ensure “safe” air travel for COPD patients as much as possible, we need to develop more effective strategies for education of health care professionals, patients, and caregivers.
Acknowledgments
We would like to thank Turkish Thoracic Society for support and permission to use congress application. We also would like to thank sincerely all our colleagues who have participated in the study. The SAFCOP study was supported by the Turkish Thoracic Society.
Disclosure
The authors report no conflicts of interests in this work.
References
1. The World Bank. Air transport, passangers carried. Available from: https://data.worldbank.org/indicator/IS.AIR.PSGR.
2. International Air Transport Association. Medical Manual.
3. International Civil Aviation Organization. Manual of Civil Aviation Medicine,
4. Peterson D, Martin-Gill C, Guyete FX, et al. Outcomes of medical emergencies on commercial airline flights. N Eng J Med. 2013;368:2075–2083.
5. Querishi A, Porter KM. Emergencies in the air. Emerg Med J. 2005;22:658–659. doi:10.1136/emj.2004.017236
6. Ahmedzai S, Balfour-Lynn IM, Bewick T, et al. Managing passangers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2011;66:i1–30.
7. Ergan B, Akgun M, Pacilli AMG, Nava S. Should I stay or should I go? COPD and air travel. Eur Respir Rev. 2018;27:180030.
8. Edvardsen A, Akero A, Hardie JA, et al. High prevalence of respiratory smptoms during air travel in patients with COPD. Respir Med. 2011;105:50–56.
9. Coker RK, Shiner RJ, Patridge MR. Is air travel safe for those with lung disease? Eur Respir J. 2007;30:1057–1063.
10. Coker RK, Patridge MR. Assessing the risk of hypoxia in flight: the need for more rational guidelines. Eur Respir J. 2000;15:128–130. doi:10.1183/09031936.00.15112800
11. Tzani P, Pisi G, Aiello M, Olivieri D, Chetta A. Flying with respiratory disease. Respiration. 2010;80:161–170.
12. Akero A, Christensen CC, Edvardsen A, Skjonsberg OH. Hypoxaemia in chronic obstructive pulmonary disease patients during a commercial flight. Eur Respir J. 2005;25:725–730.
13. Akero A, Christensen CC, Edvardsen A, Ryg SOH. Pulse oximetry in the preflight evaluation of patients with chronic obstructive pulmonary disease. Aviat Space Environ Med. 2008;79:518–524.
14. Edvardsen A, Ryg M, Akero A, Christensen CC, Skjonsberg OH. COPD and air travel: does hypoxia-altitude simulation testing predict in-flight respiratory symptoms? Eur Respir J. 2013;42:1216–1223.
15. Christensen CC, Ryg M, Refvem OK, Skjonsberg OH. Development of severe hypoxaemia in chronic obstructive pulmonary disease patients at 2,438m (8000ft) altitude. Eur Respir J. 2000;15:635–639.
16. Kelly PT, Swanney MP, Seccombe LM, et al. Air travel hypoxemia vs the hypoxia inhalation test in pasangers with COPD. Chest. 2008;133:920–926.
17. Edvardsen A, Akero A, Christensen CC, Ryg M, Skjonsberg OH. Air travel and chronic obstructive pulmonary disease: a new algorithm for pre-flight evaluation. Thorax. 2012;67:964–969.
18. Civil Aviation Authority. Available from: https://www.caa.co.uk/Passengers/Before-you-fly/Am-I-fit-to-fly-/.
19. Global Initiative for Chronic Obstructive Lung Disease. 2019 Global strategy for the diagnosis, management and prevention of COPD. Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

