Back to Journals » Patient Preference and Adherence » Volume 15
Are Older People Aware of Potential Risks Related to Benzodiazepines They are Taking and Has Anything Changed in Risk Awareness Over Ten Years?
Authors Celikkayalar E, Airaksinen M, Kivelä SL, Nieminen J, Kleme J, Puustinen J
Received 22 September 2020
Accepted for publication 9 December 2020
Published 28 January 2021 Volume 2021:15 Pages 141—147
DOI https://doi.org/10.2147/PPA.S280503
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ercan Celikkayalar,1 Marja Airaksinen,1 Sirkka-Liisa Kivelä,1,2 Jenni Nieminen,1 Jenni Kleme,1 Juha Puustinen1,3,4
1Clinical Pharmacy Group, Division of Pharmacology and Pharmacotherapy, Faculty of Pharmacy, University of Helsinki, Helsinki, Finland; 2Unit of Family Medicine, Department of Clinical Medicine, Faculty of Medicine, University of Turku, Turku, Finland; 3Social Security Center of Pori, Pori, Finland; 4Unit of Neurology, Satasairaala Central Hospital, Pori, Finland
Correspondence: Ercan Celikkayalar Email [email protected]
Purpose: The use of benzodiazepines and related drugs (BZD) is common among older adults although there is growing evidence of their harmful effects. This study investigated how well older people are aware of the potential risks related to the BZD they are taking and whether the risk awareness has changed in the years between 2004 and 2015.
Patients and Methods: The data were collected by interviewing BZD using home-dwelling patients aged ≥ 65 years with normal cognitive function (MMSE ≥ 20) who were admitted to the hospital within a 1 month study period in the years 2004 and 2015. Patients were asked whether they were aware of the ten main potential risks related to BZD use. A risk awareness score (range 0– 10) was assessed for each patient, each known potential risk yielding one point.
Results: The study included 37 patients in 2004 and 31 patients in 2015. In 2004, 6/37 patients (16%), while 16/31 patients (52%) in 2015 had risk awareness scores between 6 and 10. Awareness of dependence (p=0.047), interaction with alcohol (p=0.001), dizziness (p=0.002) and developing tolerance (p=0.002) had improved, while awareness of the other potential risks remained unchanged, muscle weakness being the least known (3/37 in 2004 and 4/31 in 2015 were aware of it as a potential risk). Regular BZD use had declined (p=0.043) but pro re nata (PRN; when required) BZD use had increased (p=0.003) between the years 2004 and 2015.
Conclusion: Older BZD users’ awareness of some potential risks related to BZD use (dependence, interaction with alcohol, dizziness and developing tolerance) had improved between 2004 and 2015, while awareness of other potential risks remained unchanged.
Keywords: benzodiazepines, risk awareness, potentially inappropriate medications, insomnia, aged, interview
Introduction
Benzodiazepines and related drugs (hereafter collectively BZD) are widely used, eg, for anxiety and insomnia.1–3 Their use is recommended to be avoided in older adults because of growing evidence on the harmful adverse effects of BZD.3,4 Major risks associated with BZD use include dependency (tolerance and withdrawal) and addiction (physical and mental reliance);5 cognitive decline;5,6 falls;5–7 fractures;5–8 and traffic accidents.5–9 Despite the risks, the BZD use is common especially in the age of ≥65 years in countries like the US and European countries, including Finland.10–12 The American Geriatrics Society suggests avoiding all BZD use at age ≥65 years.4 According to the Finnish National Current Care Guidelines (2020), treatment of acute insomnia with BZD should not exceed 2 weeks and chronic users of BZD should be encouraged to withdraw.3
A number of earlier studies have explored the patients’ perceptions and experiences of their BZD use.13–19 Some of these studies have reported patients’ experiences of the benefits and risks of their BZD medications.14,17–19 BZD users may usually think that their BZD medication is helpful and effective, however, at the same time they may underestimate or even may not be aware of the potential risks related to BZD.19–21 Age appears to be one of the major contributing factors to risk perception because older people have shown to have lower perceptions of risk.20 Previous studies also found that there is a concerning discordance between older BZD users and their physicians regarding the perceptions of risks and benefits of their BZD use.14,15
Better understanding of perceived risks about BZD use would help healthcare professionals to support their patients’ safe use of BZD. Although the recent studies have investigated the risk perceptions of BZD users,13–19 risk awareness of BZD users, ie, what they actually know about the potential risks, is not well understood. Therefore, the aim of this study was to explore how well older people are aware of potential risks related to the BZD they are taking and whether the risk awareness has changed between the years 2004 and 2015.
Patients and Methods
Study Design and Setting
This was a descriptive study based on personal patient interviews. We compared two cross-sectional data sets collected from the same hospital’s in-patients in one-month periods in the years 2004 and 2015. The same study protocols and practices were followed in both study periods. The study hospital was a mid-sized public primary care hospital in the City of Pori, Finland, with wards offering acute and rehabilitation specialist services in internal medicine, geriatrics, and neurology, with a total of 191 beds. The two acute wards with 28 beds each were selected for both study periods. Acutely ill patients were randomly directed to these wards.
Data Collection
Patients aged ≥65 years admitted to both wards with an acute illness during the study periods, between 1 June and 30 June 2004, and 1 May and 30 May 2015 were included in the study. Of all patients admitted to the wards, eligible patients using BZD for treatment of insomnia were interviewed after their cognitive function was assessed using the Mini-Mental State Examination (MMSE)22 on the first or second day after their hospitalization. Patients scoring ≥20 MMSE sum points were considered as eligible to be interviewed. This cut-off point based on the MMSE was used to increase the reliability of patients’ responses on the BZD use. Current regular and pro re nata (PRN; when required) medication use were reviewed by interviewing the patients during the first week after admission and from outpatient medical records. Only the baseline outpatient medical records were used; therefore, possible acute changes to medications after admission to the ward were not considered. BZD use for 3 months or longer within a year (12 months) was defined as regular use.
In both study periods, each consented eligible patient using BZD was interviewed personally on their awareness of ten main potential risks related to the use of BZD. The selection of potential risks was based on statutory package leaflets (PLs) that are in harmonized use within European Union countries.23 During the personal face-to-face interviews, the researcher asked whether the patients were aware of the following 10 potential risks related to BZD: 1) dependence, 2) interaction with alcohol, 3) withdrawal symptoms, 4) dizziness, 5) do not aid sleep in the long-term use, 6) reduced psychomotor performance and memory, 7) tolerance, 8) falls, 9) depression, and 10) muscle weakness. Patients’ awareness of potential risks related to the BZD use was scored by giving 1 point for each known adverse reaction, yielding a score range of 0–10.
Each eligible patient using BZD was also interviewed on their experiences of BZD withdrawal and their willingness to discontinue BZD therapy by asking whether they had withdrawal attempts; whether they had experienced BZD withdrawal symptoms and whether at the time of the interview they were willing to discontinue their BZD therapy. There was no specific time frame set for these questions, eg, for withdrawal attempts.
Statistical Analysis
The χ2 test or Fisher’s Exact test was used to test the differences in categorical variables. The significances of changes in all study patients and BZD users (with MMSE ≥20) were tested using the Wilcoxon signed-rank test. The differences of the mean sum scores, the mean ages and the mean number of medications and the changes of mean sum scores between study periods were tested using the two-sample t-test, one-way analysis of variance, the Mann–Whitney U-test or the Kruskal-Wallis test. A p-value <0.05 was considered statistically significant. Statistical analyses were performed using SAS System for Windows, version 9.1 (SAS Institute Inc., Cary, NC, USA).
Research Ethics
Both study periods were conducted with the approval of the Institutional Review Board of the Primary Care Hospital Services in the City of Pori, Finland. The study was carried out in accordance with the National Research Ethics Guidelines and Regulations,24 which are in line with the Declaration of Helsinki.25 Written informed consent was obtained from participating patients. The Regional Ethics Committee, Turku Clinical Research Centre (Turku CRC) was also consulted. According to the Turku CRC’s statement, additional approval from the Regional Ethics’ Committee was not required for this observational study. Turku CRC offers support and services for investigator-initiated clinical studies. Its services are available to investigators at the University of Turku and in the Hospital District of Southwest Finland, including Primary Care Hospital Services in the City of Pori. At the time of this study, according to the research ethics guidelines in Finland,24 Regional Research Ethics’ committee’s approval was required only for research in which patients are exposed to a clinical intervention other than the routine clinical practice based on current care guidelines. The Regional Ethics Committee (Turku CRC) stated that no such interventions were performed in this descriptive study.
Results
Characteristics of the Study Patients
The study sample in 2004 consisted of 188 patients, of which 164 were aged ≥65 years (Table 1). BZD users who scored eligible in MMSE were interviewed (n=37). In 2015, 166 patients were admitted, of which 105 were aged ≥65 years. BZD users who scored eligible in MMSE (n=31) were interviewed. Mean age of the BZD users did not differ between the study periods in 2004 and 2015 (80.3 ± 5.4 vs 80.2 ± 8.6, respectively). The female gender was more common in both study periods among BZD users (81% in both 2004 and 2015). The total number of medications in use had increased significantly among BZD users (p<0.001), also PRN use had increased (p<0.001). The regular use of at least one BZD among BZD users had declined (p<0.043), while PRN use had increased (p<0.003). The difference in concomitant use of BZD between the two study periods was not significant (Table 1).
 |
Table 1 Characteristics of the Study Patients (BZD Users: n=37 in 2004 and n=31 in 2015) |
Patients’ Awareness of Potential Risks Related to BZD Use
The patients’ awareness of potential risks related to BZD had increased between the study periods on dependence, interaction with alcohol, dizziness and developing tolerance (Figure 1). In 2004, dependence was the only potential risk that more than half of the patients (62%) were aware of, while in 2015 more than half of the patients were aware of dependence (84%), interaction with alcohol (77%), dizziness (68%), developing tolerance (58%) and withdrawal symptoms (55%). The awareness of other potential risks remained unchanged, muscle weakness being the least known potential risk in both study periods (8% vs 13% of the patients being aware of it as a potential risk, respectively).
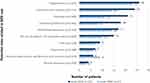 |
Figure 1 Patients’ awareness of potential risks related to the use of BZD in 2004 and 2015. |
The mean risk awareness score in 2004 and 2015 was 3.0 ± 2.6 vs 5.3 ± 2.9, respectively (p=0.001). In 2004, six out of 37 patients (16%), while in 2015, 16 out of 31 patients (52%) had higher than 6/10 risk awareness scores. The number of patients who were not aware of any of the ten potential risks (total score=0) was eight (22%) in 2004, while two patients (7%) were found with zero total scores in 2015 (Figure 2).
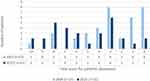 |
Figure 2 Total scores (0–10 points) for patients’ awareness of potential risks related to BZD use. Abbreviation: BZD, benzodiazepines and related drugs. |
BZD Withdrawal and Willingness to Discontinue BZD Therapy
Between study periods, no significant differences were found in patients with BZD withdrawal attempts, the patients who experienced BZD withdrawal symptoms or patients who were willing to discontinue BZD therapy (Table 2).
 |
Table 2 BZD Withdrawal Attempts and Willingness to Discontinue BZD Therapy |
Discussion
This study investigated the change in older patients’ awareness of the potential risks related to their BZD medications in 2004 and 2015. To our knowledge, this study is the first study to investigate directly the patients’ awareness of potential risks related to their BZD use based on personal interviews. We found that older patients’ awareness of potential risks related to their BZD use had increased; however, most patients were not aware of such potential risks as reduced psychomotor performance and memory, falls, depression, and muscle weakness. Awareness of the potential risk of dependence, interaction with alcohol, dizziness and developing tolerance had improved. We also found that overall BZD use had declined but PRN BZD use had increased. Despite the improvement in patients’ awareness, no significant change was found in the willingness to discontinue BZD therapy.
This study had the opportunity to compare findings in the same health-care organization between approximately 10 years to find out what has changed in the older patients’ awareness of potential risks of BZD use. The same study protocol and practices were followed in both study periods in order to facilitate the comparability of the results. Our study covered quite the same period as a national register-based study that observed a declining trend in BZD use during the years 2006 to 2014.12 Despite the observed decline, the long‐term use remained high, particularly in older adults. This overall high long-term BZD use may be due to the common use of few BZD drugs such as clonazepam and zolpidem: their use and long-term use had even increased in older adults.12 Another national register study found that more than one-third of the total potentially inappropriate medicines (PIM) use was associated with BZD in older adults in 2007.26 In that study temazepam was clearly the most commonly reimbursed PIM.
The authors of both above-mentioned national studies12,26 suggested several actions to be taken to influence the use and long-term use of BZD in older adults. These actions included training physicians and other healthcare providers in geriatric pharmacotherapy and psychotropic withdrawal, providing computerized decision-making support and alerting systems for physicians, and involving pharmacists in medication reviews.26 Researchers also suggested to monitor regularly national trends in PIM use,26 especially the duration of BZD use.12 Some of the recommended actions highlighted the need to enhance patient involvement: eg, the researchers noted that a considerable proportion of repeat prescriptions of BZD were prescribed without a face‐to‐face consultation.12 They suggested that not only the first prescription but also the first repeat prescription of a BZD should be carefully considered.12 For the long-term BZD users, BZD withdrawal interventions were suggested,12,26 considering BZD withdrawal requires strong commitment and motivation from both the patient and the health-care professionals.12,26–29
Given how common BZD use and long-term use are in older adults, surprisingly little user-centered research was found, eg, concerning awareness of potential risks, or communicating about the risks with BZD users.19–31 As the evidence on the BZD risks has been growing, reflecting eg, to leading PIM criteria,4,32 an interesting question is why this risk information is not shared with older BZD users to a greater extent than we found? It would be interesting to further investigate whether better risk awareness of BZD users may affect their willingness to discontinue long-term BZD use. Our small-scale study did not show this association. However, in our previous intervention study carried out in the same hospital as the present study, one-time counselling by a geriatrician on BZD use, including counselling on potential risks of these medicines, helped significantly to reduce the BZD use, these effects persisting for the total 12-month intervention period.27 More such intervention studies with BZD user-centered withdrawal practices are needed. On the other hand, more awareness should be created of non-pharmacological treatments for insomnia, which are currently emphasized as the primary forms of treatment in care guidelines.3,4 Also, awareness of prolonged-release melatonin as an option to reduce BZD use in the treatment of insomnia should be promoted.29,33 It is a non-sedative hypnotic which has demonstrated clinically relevant efficacy on quality of sleep with a good safety profile, without risks such as dependence and withdrawal effects.33–35
Our study indicates that patients were not aware of some of the important potential risks related to their BZD, such as reduced psychomotor performance and memory, falls, depression, and muscle weakness. These findings suggest that patient education and communication practices should be enhanced in order to improve patients’ awareness of the potential risks of BZD they take. Health-care professionals, including pharmacists, need to better recognize patients’ risk perceptions and use effective communication strategies to ensure better patient involvement when BZD use is considered as the best therapeutic choice in their condition.
The primary focus of our study was to explore patients’ risk awareness related to their BZD use. We developed a scoring system to evaluate the risk awareness and changes in it over time, based on personal interviews. We were able to generate comparable findings between two study periods with a time difference of 11 years. The main limitation of our study is the relatively small number of study participants derived from the local health-care organization. Further studies are needed with a larger number of patients. Future studies should also focus on older patients’ willingness to discontinue BZD therapy and how it is influenced by their awareness of potential risks these medicines pose them.
Conclusion
Older BZD users’ awareness of potential risks related to BZD use (dependence, interaction with alcohol, dizziness and developing tolerance) was improved between 2004 and 2015. However, most patients were not aware of such potential risks as reduced psychomotor performance and memory, falls, depression, and muscle weakness. BZD use had declined, but PRN BZD use increased. Despite the improvement in patients’ awareness, there was no significant change in their willingness to discontinue BZD therapy. Enhanced patient education and communication approaches with relevant assessment methods for risk awareness are needed.
Acknowledgments
We are immensely grateful to Dr. Anna-Liisa Koivisto, Chief Administrative Physician of the Primary Care Hospital Services in the City of Pori, Finland for supporting our work and this research. We would also like to extend our thanks to Mr. Teemu Kemppainen for his valuable work in assisting with the statistical analyses, and the study wards’ staff, nurses, physicians and patients for their most appreciated collaboration.
Disclosure
Author EC acknowledges funding from the Finnish Cultural Foundation in 2016. Juha Puustinen reports personal fees from Sanofi-Aventis and lecturer fees from Abbvie, Boehringer Ingelheim, Nutricia Medical, and Pharmac, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Roehrs T, Roth T. Insomnia pharmacotherapy. Neurotherapeutics. 2012;9(4):728–738. doi:10.1007/s13311-012-0148-3
2. Starcevic V. Benzodiazepines for anxiety disorders: maximising the benefits and minimising the risks. Adv Psychiatr Treat. 2012;18(4):250–258. doi:10.1192/apt.bp.110.008631
3. Insomnia. Current Care Guidelines. Working group set up by the Finnish Medical Society Duodecim and the Finnish Sleep Research Society. Helsinki: The Finnish Medical Society Duodecim 2015. Finnish. Available from: www.kaypahoito.fi/web/kh/suositukset/suositus?id=hoi50067.
4. By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. doi:10.1111/jgs.15767
5. Lader M. Benzodiazepine harm: how can it be reduced? Br J Clin Pharmacol. 2014;77(2):295–301. doi:10.1111/j.1365-2125.2012.04418.x
6. Crowe SF, Stranks EK. The residual medium and long-term cognitive effects of benzodiazepine use: an updated meta-analysis. Arch Clin Neuropsychol. 2018;33(7):901–911. doi:10.1093/arclin/acx120
7. Hartikainen S, Lönnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol a Biol Sci Med Sci. 2007;62(10):1172–1181. doi:10.1093/gerona/62.10.1172
8. Nurminen J, Puustinen J, Piirtola M, Vahlberg T, Kivelä SL. Psychotropic drugs and the risk of fractures in old age: a prospective population-based study. BMC Public Health. 2010;10(1):396. doi:10.1186/1471-2458-10-396
9. Smink B, Egberts A, Lusthof K, Uges D, de Gier J. The relationship between benzodiazepine use and traffic accidents: a systematic literature review. CNS Drugs. 2010;24(8):639–653. doi:10.2165/11533170-000000000-00000
10. Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiatry. 2015;72(2):136–142. doi:10.1001/jamapsychiatry.2014.1763
11. Huerta C, Abbing‐Karahagopian V, Requena G, et al. Exposure to benzodiazepines (anxiolytics, hypnotics and related drugs) in seven European electronic healthcare databases: a cross-national descriptive study from the PROTECT-EU Project. Pharmacoepidemiol Drug Saf. 2016;25(Suppl 1):56–65. doi:10.1002/pds.3825
12. Kurko T, Saastamoinen LK, Tuulio-Henriksson A, et al. Trends in the long-term use of benzodiazepine anxiolytics and hypnotics: a national register study for 2006 to 2014. Pharmacoepidemiol Drug Saf. 2018;27(6):674–682. doi:10.1002/pds.4551
13. Mah L, Upshur R. Long term benzodiazepine use for insomnia in patients over the age of 60: discordance of patient and physician perceptions. BMC Fam Pract. 2002;3(1):9. doi:10.1186/1471-2296-3-9
14. Iliffe S, Curran H, Collins R, Yuen Kee S, Fletcher S, Woods B. Attitudes to long-term use of benzodiazepine hypnotics by older people in general practice: findings from interviews with service users and providers. Aging Ment Health. 2004;8(3):242–248. doi:10.1080/13607860410001669778
15. Parr JM, Kavanagh DJ, Young RM, McCafferty K. Views of general practitioners and benzodiazepine users on benzodiazepines: a qualitative analysis. Soc Sci Med. 2006;62(5):1237–1249. doi:10.1016/j.socscimed.2005.07.016
16. Anthierens S, Habraken H, Petrovic M, Deveugele M, De Maeseneer J, Christiaens T. First benzodiazepine prescriptions: qualitative study of patients’ perspectives. Can Fam Physician. 2007;53(7):1200–1201.
17. Cook JM, Biyanova T, Masci C, Coyne JC. Older patient perspectives on long-term anxiolytic benzodiazepine use and discontinuation: a qualitative study. J Gen Intern Med. 2007;22(8):1094–1100. doi:10.1007/s11606-007-0205-5
18. Siriwardena AN, Qureshi MZ, Dyas JV, Middleton H, Orner R. Magic bullets for insomnia? Patients’ use and experiences of newer (Z drugs) versus older (benzodiazepine) hypnotics for sleep problems in primary care. Br J Gen Pract. 2008;58(551):417–422. doi:10.3399/bjgp08X299290
19. Sake F, Wong K, Bartlett D, Saini B. Benzodiazepine use risk: understanding patient specific risk perceptions and medication beliefs. Res Social Adm Pharm. 2019;15(11):1317–1325. doi:10.1016/j.sapharm.2018.12.007
20. Webster RK, Weinman J, Rubin GJ. People’s understanding of verbal risk descriptors in patient information leaflets: a cross-sectional national survey of 18- to 65-year-olds in England. Drug Saf. 2017;40(8):743–754. doi:10.1007/s40264-017-0542-1
21. Aronson JK. Risk perception in drug therapy. Br J Clin Pharmacol. 2006;62(2):135–137. doi:10.1111/j.1365-2125.2006.02739_1.x
22. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
23. European Commission. A guideline on summary of product characteristics; 2009. Available from: https://ec.europa.eu/health/sites/health/files/files/eudralex/vol-2/c/smpc_guideline_rev2_en.pdf.
24. Finnish Advisory Board on Research Integrity. Responsible conduct in research and procedures for handling allegations of misconduct in Finland. Available from: https://www.tenk.fi/en/tenk-guidelines.
25. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053.
26. Leikola S, Dimitrow M, Lyles A, Pitkälä K, Airaksinen M. Potentially inappropriate medication use among Finnish non-institutionalized people aged ≥65 years: a register-based, cross-sectional, national study. Drugs Aging. 2011;28(3):227–236. doi:10.2165/11586890-000000000-00000
27. Salonoja M, Salminen M, Aarnio P, Vahlberg T, Kivelä SL. One-time counselling decreases the use of benzodiazepines and related drugs among community-dwelling older persons. Age Ageing. 2010;39(3):313–319. doi:10.1093/ageing/afp255
28. Salonoja M, Salminen M, Vahlberg T, Aarnio P, Kivelä SL. Withdrawal of psychotropic drugs decreases the risk of falls requiring treatment. Arch Gerontol Geriatr. 2012;54(1):160–167. doi:10.1016/j.archger.2011.02.015
29. Lahteenmaki R, Puustinen J, Vahlberg T, et al. Melatonin for sedative withdrawal in older patients with primary insomnia: a randomized double-blind placebo-controlled trial. Br J Clin Pharmacol. 2014;77(6):975–985. doi:10.1111/bcp.12294
30. Sirdifield C, Chipchase SY, Owen S, Siriwardena AN. A systematic review and meta-synthesis of patients’ experiences and perceptions of seeking and using benzodiazepines and Z-drugs: towards safer prescribing. Patient. 2017;10(1):1–15. doi:10.1007/s40271-016-0182-z
31. Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized Trial. JAMA Intern Med. 2014;174(6):890–898. doi:10.1001/jamainternmed.2014.949
32. The Finnish Medicines Agency: Meds75+. Available from: http://www.fimea.fi/web/en/databases_and_registeries/medicines_information/database_of_medication_for_the_elderly.
33. Clay E, Falissard B, Moore N, Toumi M. Contribution of prolonged-release melatonin and anti-benzodiazepine campaigns to the reduction of benzodiazepine and Z-drugs consumption in nine European countries. Eur J Clin Pharmacol. 2013;69(4):1–10. doi:10.1007/s00228-012-1424-1
34. Wade A, Ford I, Crawford G, et al. Efficacy of prolonged release melatonin in insomnia patients aged 55–80 years: quality of sleep and next-day alertness outcomes. Curr Med Res Opin. 2007;23(10):2597–2605. doi:10.1185/030079907X233098
35. Wade A, Ford I, Crawford G, et al. Nightly treatment of primary insomnia with prolonged release melatonin for 6 months: a randomized placebo controlled trial on age and endogenous melatonin as predictors of efficacy and safety. BioMed Central Med. 2010:8. doi:10.1186/1741-7015-8-51.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
