Back to Journals » Risk Management and Healthcare Policy » Volume 14
Applying “Stages of Readiness to Change” Model to Dentists’ Decisions to Participate in Medicaid: An Exploratory Study
Authors Kateeb E , McKernan SC, Askelson N, Momany E, Damiano P
Received 4 May 2021
Accepted for publication 20 July 2021
Published 11 August 2021 Volume 2021:14 Pages 3311—3322
DOI https://doi.org/10.2147/RMHP.S318357
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mihajlo Jakovljevic
Elham Kateeb,1,2 Susan C McKernan,2,3 Natoshia Askelson,2,4 Elizabeth Momany,2 Peter Damiano2,3
1Oral Health Research and Promotion Unit, Al-Quds University, Jerusalem, Palestine; 2Public Policy Center, University of Iowa, Iowa City, Iowa, USA; 3Department of Preventive and Community Dentistry, College of Dentistry, University of Iowa, Iowa City, Iowa, USA; 4Department of Community and Behavioral Health, College of Public Health, University of Iowa, Iowa City, Iowa, USA
Correspondence: Elham Kateeb Email [email protected]; [email protected]
Background: The Stages of Readiness to Change (SOC) behavioral model describes behavior change as a process and distinguishes individuals based on their current behavior and readiness to change that behavior. SOC can be used to improve dentists’ participation in a state public dental benefit program (Medicaid) by targeting them at different SOC with interventions, strategies, and tools tailored to those stages. Therefore, this study assessed the usefulness of using SOC to describe dentists’ attitudes towards and participation in Medicaid. Dentists’ participation in Medicaid is of interest to policymakers, and this study demonstrates a method to identify potential opportunities for intervention.
Methods: A modified SOC algorithm used data from a periodic survey of Iowa Dentists to categorize dentists (N=514) into: 1) pre-contemplation, 2) considering participation (SOC contemplation and preparation), 3) acting (SOC action and maintenance), and 4) risk of relapse (at risk for discontinuing participation). The four SOC stages were compared using ANOVA and post hoc Tukey’s test among: practice characteristics, Dentists Altruism scale, Attitude about Program Administration scale, Attitude about Medicaid patients scale and Perception of Importance of Medicaid Problems scale.
Results: Among survey respondents, 36% were categorized as pre-contemplation, 6% were considering Medicaid participation, 12% were acting as Medicaid providers with minimal risk of relapse, and 46% were participating and at risk of discontinuing. Dentists’ attitudes towards program administration, Medicaid patients, and access to care varied across the SOC cycle.
Conclusion: Nearly, 46% dentists in this analysis were identified as at risk of discontinuing participation – a much larger proportion than dentists considering Medicaid participation. Categorizing dentists using this approach has important implications for programmatic interventions. For example, policymakers targeting our study population could focus their efforts on reducing the likelihood of dentists dropping out of the program, with less emphasis targeting dentists in the precontemplation stage.
Keywords: dentists, surveys and questionnaires, transtheoretical model, stages of change, Medicaid
Introduction
Finding effective ways to encourage healthcare providers (HCP) to change their behavior towards a particular decision or belief they embrace is a major challenge.1 Behavioral theories that attempted to understand mechanisms of HCP’s behavior change, for example, social cognitive theories that emphasize the importance of individual attitude to change intention processes,2 or other economic theories that promote financial incentives to change behavior,3,4 did not succeed in explaining healthcare providers’ (HCP) behavior or proposing a valid framework to achieve the desired change.
Different theories typically focus on different problems in behavior change process; therefore, they are potentially complementary. Nonetheless, using a combination of theories to understand behavior or to promote a behavior change related to decision making remains an exception rather than the rule.5 Few significant cross-theoretical frameworks have been proposed that are intended to facilitate the understanding of a health behavior change while integrating different theories that attempts to address change from different perspectives. The Stages of Readiness to Change (SOC)6 is one of the few examples that identifies the complementary nature of theories explaining health behaviors and introduces the concept of SOC that provides a framework that permits such integration.7
One of the areas that the SOC framework can be applied is dentists’ participation in Medicaid program. Although the factors related to dentists’ participation in Medicaid have been investigated in many studies since the early 1980s,8–14 no approach to date has been effective in increasing participation beyond its current levels. One reason is that participating in Medicaid is a challenging task requiring complex changes in clinical routines, better collaboration among practices, changes in patients’ behavior, or changes in the organization of care.6
The other reason could be that no studies have used theoretical models to describe or explain providers’ intentions related to participation in Medicaid. Simply classifying providers into those who participate in Medicaid and those who do not oversimplifies the decision-making continuum and neglects the distinction between non-participants who are considering change and non-participants who are not considering change. On the other side, using a reductive classification ignores the difference between participants who are satisfied in their participation and those who are thinking of soon quitting the program. Although Medicaid marketing campaigns may target all those providers indiscriminately, their success is not guaranteed until they target the providers at different Stages of Readiness to Change with interventions, strategies, and tools tailored to those stages.6
Our previous work15 investigating factors related to dentists’ decisions to accept new Medicaid patients in their practice used an innovative approach to elicit hidden drivers. Results from that study showed that patients’ punctuality in showing up for appointments and the ease of Medicaid claims processing were as important as reimbursement rates. However, to use these results effectively in promoting the participation in Medicaid, we need a behavioral model that offers theoretical assumptions about the steps that professionals and organizations in healthcare must take to achieve the intended changes.
The SOC posits that behavioral change is a process, and individuals can be distinguished throughout the process based on their intentions to change. Among healthcare providers, the SOC individuals differ according to the professionals’ and teams’ awareness of and motivation to perform a specific behavior. Each stage is governed by different factors and requires different strategies and theories for change. Thus, identifying different stages of readiness to change will naturally lead better design of different interventions and strategies to change behavior.6
In the SOC, pre-action stages include Pre-contemplation during which the individual does not intend to adopt the criteria behavior in the near future; Contemplation, during which the individual is intending to adopt the criteria behavior within the near future, and Preparation, when the individual is actively considering adoption of the criteria behavior in the immediate future.7 Action stages include Action, during which the individual has adopted the behavior change in the recent past but the changes are not well established, and the Maintenance stage, during which the individual has adopted the criteria behavior and is working to sustain the change.16
The SOC model suggests that people are thought to progress through the five stages at varying rates, often moving back and forth along the continuum several times before attaining the goal of maintenance. Relapse is an event that terminates the action or maintenance phases prompting a cyclic movement back through the initial stages (all 5 stages). To address the risk of relapse that may occur at any point in the previous stages, a study that assessed readiness to adhere to antiviral therapy added the “Risk of relapse” stage to the previous five stages.20
This study came to identify dentists’ different SOC to participate in Medicaid at a state level, (Pre-contemplation, Contemplation, Preparation, Action, Maintenance, and Risk of relapse)
The specific objectives of this study were:
- Categorizing primary care dentists in the State of Iowa into the six stages of SOC, Precontemplation, Contemplation, Preparation, Action, Maintenance and Risk of relapse.
- Comparing dentists’ practice characteristics among the different stages of SOC.
- Comparing dentists’ Altruism scale among the different stages of SOC.
- Comparing dentists’ attitude about Program administration and Medicaid patients among the different stages of SOC.
- Comparing dentists perception of the importance of Medicaid problems among the different stages of SOC.
- Proposing different interventions to move dentists from one stage to another among the different stages of SOC to maximize Medicaid participation.
Identifying the stage/stages that the majority of dentists belong to will help in designing interventions that target the largest percentage of providers at a state level. SOC can be used as a template on which to map, organize, and synthesize a variety of disparate theories of persuasion and behavior change and embody specific methods for discrete communication campaign interventions.6
In addition, if providers are evenly distributed over more than one segment, this segmentation will help policy makers decide where to invest their limited resources, in those on the margin of change or most likely to change, or those who are not considering change at all in the foreseen future.
Recent studies in exercise17 and diabetes care18 have found that tailored interventions based on SOC are more effective than traditional approaches that focus on the premise that individuals are always ready to change. Among healthcare providers, tailoring strategies to an individual provider’s readiness to change has been proposed to enhance the efficiency of guideline implementation and counseling activities.19,20
Methods
Data for the current analysis was extracted from a mail survey (Appendix 1) to all primary care dentists (general dentists GDs and pediatric dentists PDs) engaged in private practice in the state of Iowa in 2013 (n=1101).21 Dentists’ mailing addresses were obtained from the Iowa Dentist Tracking System, which maintains information about all licensed dentists in the state.22 The survey was modified from a previous version developed by the University of Iowa Public Policy Center and College of Dentistry.23 The new version was pretested for format and content validity with members of the Dental Safety Net in Iowa (DSNI) Project’s national advisory committee, which included representatives from organized dentistry, academic experts, dental safety net providers and government agencies (https://ppc.uiowa.edu/health/study/dental-safety-net-iowa-dsni-project). Members received iterative versions of the survey and provided feedback via cognitive interviews. The University of Iowa Institutional Review Board (IRB) approved the protocol for this project, including the survey questionnaire.
Dentists demographic data such as dentists’ age and sex were obtained from the Iowa Dentist Tracking System. The current survey collected data about dentists’ practices such as, dentists’ practice arrangements (for example, solo versus group practice) and perceived workload during the previous 12 months.
A series of survey questions were used to build composite variables that measured,1) altruistic attitudes among dentists, 2) attitudes about Medicaid program administration, 3) attitudes about Medicaid enrollees and 4) perception of Medicaid program’s problems.21 Dentists were asked to indicate, on a 4-point scale, the degree to which they disagreed or agreed with each statement (1: strongly disagree, 4: strongly agree). These statements were adapted from a previous survey provided to dental students24 that in turn was modeled on a study of attitudes toward social responsibility among medical students.25 Higher scores in the four scales indicated more altruistic attitudes, more positive attitudes toward the Medicaid patient population, more positive attitudes about Medicaid administration and greater importance of the impact of Medicaid’s problems on decision to participate in the program. More information about the previous scales and their validity can be found in our previous published work.21
The SOC Algorithm Development
A SOC algorithm (Figure 1) was developed to assess, where possible, willingness of dentists to accept new Medicaid children patients and to assess SOC stages of change. A total of 6 stages that include the 5 stages of SOC26 (pre-contemplation, contemplation, preparation, action, and maintenance) and the “ Relapse Risk”16,20 were assigned for primary dental care providers’ (general dentists and pediatric dentists) participation in Medicaid.
 |
Figure 1 Stage of change (SOC) algorithm. |
To quantify current Medicaid participation, this question was asked: “Do you currently accept new Medicaid patients?”. Three possible answers were provided: 1)“None”, indicating no participation, 2) “Yes, some new”, indicating limited participation (LP), and 3) “Yes, all new”, indicating full participation (FP).
To assess the dentists’ readiness to participate, maintain, or quit Medicaid, a staging algorithm was used (Figure 1). This method is considered the simplest way for assessing SOC stages. In this format, providers are presented with a series of 4–5 questions and assigned to discrete stages based on their responses.27 For that purpose, the following questions were asked: “Do you currently accept new Medicaid patients?”, “Are you seriously thinking about starting to accept all new or some new Medicaid patients in the next year?”, “Are you planning to accept all new or some new Medicaid patients in the next 6 months?”, “About how long have you been accepting some new Medicaid patients in your practice?”, “How certain are you that you will continue accepting all/some new Medicaid patients on a regular basis in the next year?”.
Action, Maintenance, and Relapse risk stages were presented for limited (LP) and full (FP) participants. Dentists in the “Action” stage were not assessed for relapse, because it is premature for them to evaluate this experience. Answers to the algorithm questions were measured by “Yes/ No” nominal variable. Figure 1.
The SOC algorithm used in this study was adapted from previous studies28 and went through pre-testing before implementation by cognitive Interviewing and pilot testing. Cognitive interviewing is a technique commonly used to pre-test survey instruments developed by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC), the Bureau of Labor Statistics, and the Census Bureau.29 Cognitive interviews were conducted by the project’s national advisory committee. Experts were interviewed while filling out and after completing the test instrument to ascertain potential problems encountered with terminology, ambiguous information, or question format. We used both concurrent and retrospective “think aloud” interviews, as well as probes, to determine how the participants arrive at their answers. The interviews were conducted using previously published techniques.29 Cognitive interview guidelines do not specify the number of interviews that are needed for pre-testing, but it has been recommend that no more than 12–15 to be conducted on one version of an instrument.29 Feedback may become redundant after only five interviews.30 The final algorithm was also be tested in a small group of private dentists (15 dentists from a neighboring state) during a pilot test prior to the study.
Statistical Analysis
Means and frequencies were performed on the provider and practice characteristics data. Data about general characteristics of Iowa primary care dentists obtained from the Iowa Dentists tracking system31 was used to detect any response bias in our sample. Descriptive statistics were generated to summarize the proportion of subjects in pre-contemplation, contemplation, preparation, action, maintenance, and risk of relapse stages for willingness to accept new Medicaid children. For analysis consideration, participants in (FL) and (PT) were combined together and the six SOC were combined into 4 main stages, Pre-contemplation, Considering, Acting, and At Risk (Figure 2).
 |
Figure 2 Stages of readiness to change framework. |
The four stages of SOC (Dependent variables): “Pre-contemplation”, “Considering, “Acting” and “At Risk” were compared using ANOVA and Post hoc Tukey’s test among practice characteristics (% of Medicaid reimbursement and % of Medicaid participation) and the 4 composite scales of Dentists Altruism, Attitude about Program Administration, Attitude about Medicaid Patients and Perception of Importance of Medicaid Problems Scale. A significance level of 0.05 for all hypothesis tests. All Bivariable analysis was conducted by using statistical software (SPSS Statistics, version 21; IBM). Missing responses were treated as missing values in analysis. Patterns of missing responses to attitudinal statements were examined among dentists on the basis of Medicaid participation; tests here did not reveal any statistically significant evidence of response bias on the basis of age or sex (P > 0.05).
Results
Of the 1101 eligible primary care dentists, 651 completed and returned the original survey (response rate of 59%). Survey respondents were comparable with the overall population of general dentists in age and sex. However, survey respondents were significantly more likely to be solo practitioners (65% versus 53% of all general dentists; P < 0.001). In the current analysis, only dentists who were primarily responsible for making the decision whether their dental practice would accept Title 19 patients (N=514) were included.
Sample Characteristics
Eighty-one percent of the sample were males and 59% were older than 50 years (Age Mean= 51 ±11.5) and 64% were solo practitioners. Eighty percent practiced in Metropolitan areas and 14% in rural/small towns. Fifty-seven percent had comfortable workload and 24% were too busy and overworked. Fifty-four percent had a personal gross product more than $500,000, with an average of $34,500 reimbursed from Medicaid in year 2011 (Min=0, Max=500,000). An average of 10% of practices’ current patients were Title 19 (Min=0, Max=90%). More information about sample demographic and practice characteristics can be found in Table 1.
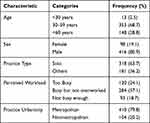 |
Table 1 Demographic and Practice Characteristics of Dentists in the Study Sample |
The current sample scored on a scale from 1 to 4 an average of 2.68 ±0.53 on Dentist Altruism scale, 2.47±0.58 on Attitudes about Medicaid Patients scale, 2.04 ±0.67 on Attitudes about Medicaid Administration scale and 3.1± 0.47 on Perceptions of Problems with the Medicaid program.
Stages of Readiness to Change (SOC)
Five hundred dentists completed the SOC algorithm. According to the algorithm proposed in this study, 12% of our sample (n=59) were in the “Acting” stage, and 46% (n=230) were in the “At risk” stage. Dentists in both stages, “Acting” and “At risk”, are already Medicaid participants (289 out of 500). “Pre-considering” stage included 36% (n=182) of our sample and 6% (n=29) were in the ”Considering” stage. This shows that 211 dentists in our sample were not Medicaid participants. Distribution of dentists in the four SOC are shown in Figure 3.
 |
Figure 3 Dentists in different stages of readiness to change. |
Practice characteristics were compared among the four SOC. Among program participants, dentists in “Acting Stage” had more reimbursement money from Medicaid (M= $84,000 ±10,000) in the past year than dentists in “At risk” stage (M=52,000 ±7000); F= 22.7, p < 0.0001. In addition, dentists in “Acting” stage had more % of current Title 19 patients (M=21% ± 23) than dentists in “At risk” stage (M=13% ± 12), F=30, p < 0.0001.
Dentists in “Pre-considering “ stage scored significantly lower scores on Dentists Altruism scale than “Considering”, “Acting” and “At risk”. As expected, dentists in “Acting” stage had the highest score on this scale; however, this difference was statistically significant with dentists in “Pre-considering” stage only. Data about Altruism scale in the four SOC can be found in Table 2
 |
Table 2 Mean Values of Dentists Altruism Scale in the Different SOC |
Attitude about Medicaid administration was most positive in the “Acting” stage and differed significantly than other stages. The lowest scores were among dentists in “Pre-considering” stage but not statistically significant than in “Considering” stage. Dentists in “At risk stage” scored significantly higher than dentists in “ Pre-considering “ stage but similar to the scores of dentists in “Considering” stage. Attitude about Medicaid administration scale is shown in Table 3. Scores on dentists’ attitude towards Medicaid patients were not significantly different between SOC (Table 4).
 |
Table 3 Mean Values of Dentists’ Attitude Towards Program Administration Scale in the Different SOC |
 |
Table 4 Mean Values of Dentists’ Attitude About Medicaid Patients Scale in the Different SOC |
Perception of the importance of Medicaid problems its influence on dentists’ decision to accept new Medicaid patients was the least in the “Acting” stage and the most in “Pre-considering” and “Considering” stages. Table 5 show the scores of the perception of the importance of Medicaid problems scale.
 |
Table 5 Mean Values of Dentists’ Perception of Importance of Medicaid s Scale in the Different SOC |
Discussion
This article suggests an innovative application of a well-known methodology that is used historically to explain human decision-making process on dentists’ decision to accept Medicaid patients. The use of SOC as the theoretical framework in this study was unique and the first of its kind in dental literature.
The strength of this model, which cannot easily be achieved by other traditional surveying tools is its ability to: 1) distinguish between Medicaid non-participating dentists who are considering future Medicaid participation (behavior change) and those who are not thinking at all about this step, and 2) distinguish between current Medicaid dentists who are satisfied with the program and dentists who are facing challenges and considering quitting the program. This distinction is important because it can help match the most appropriate intervention to each stage of readiness to change. The SOC framework suggests that not only is the nature of the intervention important, but an individual’s stage of readiness, or receptiveness, is also crucial to its success.
Most of the SOC literature has focused on changing behavior among patients.16,17 However, this framework offers utility to understand and change health professionals’ behavior.18,19
Evidence from previous research that used SOC as a framework for behavior change can be adapted to dentists and target different stages of their readiness to participate in Medicaid (Figure 4), some examples are:
- Precontemplation Stage: In our study, 36% of dentists were in the “Pre-contemplation” stage. This means that more than one-third of our sample were not even considering Medicaid participation. According to the literature on the SOC model, this population can benefit from interventions that target processes such as consciousness-raising and self-reevaluation32 to motivate dentists in these early stages.
- Considering Stage: 6% of our sample were in the “Considering” stage. Dentists at this stage could be targeted by interventions that modify the practice environment, management, and administration. Theses intervention can have the potential to initiate the desired change and motivates dentists to start accepting new Medicaid patients. These interventions should target dentists and office staff together to produce an environment conducive to change.32,33 Training staff on the Medicaid program administration and paperwork could also facilitate this change.32,33
- Acting Stage: 12% of our sample were in the “Acting” stage. Those dentists are already motivated, thus they can benefit from strategies that focus on resources support to sustain their engagement.32–34
- At Risk: Nearly half of the dentists in our study were identified as being at risk of discontinuing Medicaid participation. Interventions that address dentists’ challenges and provide them with tools to overcome these issues will be required here. These dentists had the lowest scores in the “Attitude towards Medicaid Patients” scale, which suggests that patients’ behavior is a challenge for those dentists to maintain their commitment to this population. A previous study by our authors that used conjoint analysis to understand factors related to dentists’ decision to accept Medicaid patients found that patients who did not show to their to their appointments regularly or did not comply with oral hygiene instructions significantly decreased dentists’ willingness to accept new Medicaid patients.15 Strategies to improve appointment-keeping behaviors include care coordination care, including social services like transportation or childcare. Finally, at risk dentists reported fewer Medicaid patients in their practice, suggesting less experience with this population. As a result, dentists may be not well-prepared to provide care to Medicaid enrollees in comparison to dentists in the Acting stage.
 |
Figure 4 Interventions that help dentists to move between different SOC to maximize Medicaid participation. |
In summary, almost half of this sample were at risk of quitting Medicaid and more than one-third are not considering participation. The data used in the current analysis was collected in 2013. Since then, large scale changes to the Medicaid program in Iowa have taken place. Thus, estimates of Medicaid participation described in this article likely have changed.
One significant change that occurred in Iowa state since data collection for this study was the Iowa Health and Wellness Plan in 2014, which is an expansion plan of the Medicaid program to include adult benefits and more incentives for healthy behaviors.35 Although, dentists’ participation in the new version did not differ significantly than the older version as cited by a 2019 study,35 predictors to participation in the two programs varied based on the different structure and administration of the two versions.
It would be interesting to longitudinally assess the pattern of Medicaid participation in its two versions and the impact of policy changes on participation stages by comparing our findings with more recent data from this population. However, our main goal was to assess the feasibility of applying the SOC framework to explain dentists’ attitudes and behaviors, not to quantify their participation in the program.
This study is the first of its kind to apply SOC model to dentists’ decision-making process. Categorizing dentists using SOC has important implications for programmatic interventions. For example, policymakers targeting our study population could focus their efforts on reducing the likelihood of dentists dropping out of the program, with less emphasis targeting dentists in the precontemplation stage.
In conclusion, information gleaned from this study can be used in interventions to improve dentists’ participation in the Medicaid program. The SOC model, used as the conceptual framework for this study, theorizes that interventions to change behavior cannot be applied universally. Dentists first need to be screened to identify readiness to change. Then, appropriate interventions to target behavior change can be proposed. For example, a large percentage of income among our dentists in the “Acting“ stage came from Medicaid patients. Thus, competitive reimbursement rates and customary charges on a key set of services can be tempting to sustain their participation.32–34 However, periodic reimbursement rate review and updates, along with simplification of administrative requirements, and care coordination services for beneficiaries would be more effective in retaining dentists who are at risk.32–34 Direct outreach to dentists to build participation can be a good way to introduce the program benefits for dentists who are pre-contemplative.34
Abbreviations
SOC, stages of change; HCP, healthcare providers; NCHS, National Center for Health Statistics; CDC, Centers for Disease Control and Prevention; FP, full participation; LP, limited participation; GP, general dentists; PD, pediatric dentists.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available because it belongs strictly to the University of Iowa Public Policy Center, but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Prior to data collection, an ethics approval from the University of Iowa Institutional Review Board (ID# 2012-07782) was obtained. Dentists’ participation was voluntary and confidential. Informed consent forms were collected from all participants in this study. This study has been conducted in full accordance with the World Medical Association Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was supported by the Zamalah Fellowship Program, an academic development program for higher edication in Palestine, and an Innovation Fund for Oral Health award to the University of Iowa Public Policy Center from the DentaQuest Foundation. Neither funder had a role in the design, collection, analysis, or interpretation of data or in writing the manuscrip
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50. doi:10.1186/1748-5908-7-50
2. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
3. Laffont JJ, Martimort D. The theory of incentives: the principal-agent model. Princeton University Press; 2002. JSTOR. Available from: www.jstor.org/stable/j.ctv7h0rwr.
4. Becker GS. The Economic Approach to Human Behavior. Chicago: University of Chicago Press; 1976.
5. Westat Inc. The CDC health communication program database.
6. Slater M. Integrating application of media effects, persuasion, and behavior change theories to communication campaigns: a stages-of-change framework. Health Commun. 1999;11:335–354. doi:10.1207/S15327027HC1104_2
7. Arthur AB, Kopec JA, Klinkhoff AV, et al. Readiness to manage arthritis: a pilot study using a stages-of-change measure for arthritis rehabilitation. Rehabil Nurs. 2009;34(2):64–84. doi:10.1002/j.2048-7940.2009.tb00250.x
8. Hughes RJ, Damiano PC, Kanellis MJ, Kuthy R, Slayton R. Dentists’ participation and children’s use of services in the Indiana dental Medicaid program and SCHIP: assessing the impact of increased fees and administrative changes. J Am Dent Assoc. 2005;136(4):517–523. doi:10.14219/jada.archive.2005.0209
9. Milgrom P, Riedy C. Survey of Medicaid child dental services in Washington state: preparation for a marketing program. J Am Dent Assoc. 1998;129(6):753–763. doi:10.14219/jada.archive.1998.0318
10. Im JL, Phillips C, Lee J, Beane R. The north carolina Medicaid program: participation and perceptions among practicing orthodontists. Am J Orthod Dentofacial Orthop. 2007;132(2):
11. Al Agili DE, Pass MA, Bronstein JM, Lockwood SA. Medicaid participation by private dentists in Alabama. Pediatr Dent. 2007;29(4):293–302.
12. Shulman JD, Ezemobi EO, Sutherland JN, Barsley R. Louisiana dentists’ attitudes toward the dental Medicaid program. Pediatr Dent. 2001;23(5):395–400.
13. Blackwelder A, Shulman JD. Texas dentists’ attitudes toward the dental Medicaid program. Pediatr Dent. 2007;29(1):40–46.
14. Damiano PC, Brown ER, Johnson JD, Scheetz JP. Factors affecting dentist participation in a state Medicaid program. J Dent Educ. 1990;54(11):638–643. doi:10.1002/j.0022-0337.1990.54.11.tb02476.x
15. Kateeb ET, McKernan SC, Gaeth GJ, Kuthy RA, Adrianse NB, Damiano PC. Predicting dentists’ decisions: a choice-based conjoint analysis of Medicaid participation. J Public Health Dent. 2016;76(3):171–178. doi:10.1111/jphd.12126
16. Highstein GR, Willey C, Mundy LM. Development of Stage of Readiness and decisional balance instruments: tools to enhance clinical decision-making for adherence to antiretroviral therapy. AIDS Behav. 2006;10(5):563–573. doi:10.1007/s10461-005-9043-9
17. Jones H, Edwards L, Vallis TM, et al. Changes in diabetes self-care behaviors make a difference in glycemic control: the diabetes stages of change (DiSC) study. Diabetes Care. 2003;26(3):732–737. doi:10.2337/diacare.26.3.732
18. DiClemente CC, Carbonari JP, Velasquez MM. Alcoholism Treatment Mismatching from a Process of Change Perspective. In: Watson RR, editor. Alcohol Abuse Treatment. Drug and Alcohol Abuse Reviews. Vol. 3. Totowa, NJ: Humana Press; 1992. doi:10.1007/978-1-4612-0363-6_5
19. Main DS, Cohen SJ, DiClemente CC. Measuring physician readiness to change cancer screening: preliminary results. Am J Prev Med. 1995;11(1):54–58. doi:10.1016/S0749-3797(18)30501-4
20. Goldstein MG, DePue JD, Monroe AD, et al. A population-based survey of physician smoking cessation counseling practices. Prev Med. 1998;27(5 Pt 1):720–729. doi:10.1006/pmed.1998.0350
21. McKernan SC, Reynolds JC, Momany ET, et al. The relationship between altruistic attitudes and dentists’ Medicaid participation. J Am Dent Assoc. 2015;146(1):34–41.e3. PMID: 25569496. doi:10.1016/j.adaj.2014.11.014
22. Kuthy RA, McKernan SC, Hand JS, Johnsen DC. Dentist workforce trends in a primarily rural state: iowa: 1997–2007. J Am Dent Assoc. 2009;140(12):1527–1534. doi:10.14219/jada.archive.2009.0105
23. Damiano PC, Kanellis MJ, Willard JC, Momany ET. A Report on the Iowa Title XIX Dental Program.; 1996. Available from: https://ppc.uiowa.edu/publications/report-iowa-title-xix-dental-program. Accessed July 12, 2021.
24. Brown LJ, Wall TP, Lazar V. Trends in untreated caries in primary teeth of children 2 to 10 years old. J Am Dent Assoc. 2000;131(1):93–100. doi:10.14219/jada.archive.2000.0027
25. Brown LJ, Wall TP, Lazar V. Trends in caries among adults 18 to 45 years old. J Am Dent Assoc. 2002;133(7):827–834. doi:10.14219/jada.archive.2002.0296
26. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi:10.1037//0003-066x.47.9.1102
27. Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13(1):39–46. doi:10.1037//0278-6133.13.1.39
28. Weinstein ND, Lyon JE, Sandman PM, Cuite CL. Experimental evidence for stages of health behavior change: the precaution adoption process model applied to home radon testing. Health Psychol. 1998;17(5):445–453. doi:10.1037//0278-6133.17.5.445
29. Willis GB; National Center for Health Statistics (U.S.). Cognitive Interviewing and Questionnaire Design: A Training Manual. Hyattsville, MD: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 1994.
30. Mobley AR. Evaluation of Behavioral Theory and Integrated Internet/Telephone Technologies to Support Military Obesity and Weight Management Programs. College Park: University of Maryland; 2006.
31. Iowa dentist tracking system ui carver college of medicine office of statewide clinical education programs. Iowa Health Professional Tracking Center; 2010.
32. Cohen SJ, Halvorson HW, Gosselink CA. Changing physician behavior to improve disease prevention. Prev Med. 1994;23(3):284–291. doi:10.1006/pmed.1994.1040
33. Wendy J. Frosh, Founder and principal of Healthcare Management Strategies. Missouri Foundation for Health (Spring 2017). Available from: https://mffh.org/wpcontent/uploads/2017/04/Policy-Strategies-to-Enhance-Dentists-Participation-in-Medicaid.pdf.
34. Bezner J, Lloyd LK, Crixell SH, Burke TJ. The health care provider’s role in supporting positive health behavior change: developing an effective and supportive communication approach. Med Res Arch. 2017;5(9). ISSN 2375–1924. Available form: https://esmed.org/MRA/mra/article/view/1523. Accessed August 04, 2021.
35. Reynolds JC, McKernan SC, Damiano PC, Kuthy RA. A tale of two public dental benefit programs: iowa dentist participation in traditional Medicaid versus a Medicaid expansion program. BMC Oral Health. 2019;19(1):89. doi:10.1186/s12903-019-0771-z
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
