Back to Journals » Journal of Pain Research » Volume 13
Applying Serum Cytokine Levels to Predict Pain Severity in Cancer Patients
Authors Fazzari J, Sidhu J, Motkur S , Inman M, Buckley N, Clemons M, Vandermeer L, Singh G
Received 14 August 2019
Accepted for publication 20 January 2020
Published 7 February 2020 Volume 2020:13 Pages 313—321
DOI https://doi.org/10.2147/JPR.S227175
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Jennifer Fazzari,1 Jesse Sidhu,1 Shreya Motkur,1 Mark Inman,2 Norman Buckley,3 Mark Clemons,4,5 Lisa Vandermeer,5 Gurmit Singh1,3
1Department of Pathology & Molecular Medicine, McMaster University, Hamilton, Ontario, Canada; 2Department of Medicine, McMaster University, Hamilton, Ontario, Canada; 3Michael G. DeGroote Institute for Pain Research and Care, McMaster University, Hamilton, Ontario, Canada; 4Department of Medicine, Division of Medical Oncology, The Ottawa Hospital, Ottawa, Canada; 5Cancer Research Program, Ottawa Hospital Research Institute and University of Ottawa, Ottawa, Canada
Correspondence: Gurmit Singh
Department of Pathology & Molecular Medicine, McMaster University, 1280 Main Street West, Hamilton, ON, L8N 3Z5, Canada
Tel +1 905 525 9140 Ext 28144
Email [email protected]
Background and Aim: Cancers originating in the breast, lung and prostate often metastasize to the bone, frequently resulting in cancer-induced bone pain that can be challenging to manage despite conventional analgesic therapy. This exploratory study’s aim was to identify potential biomarkers associated with cancer-induced pain by examining a sample population of breast cancer patients undergoing bisphosphonate therapy.
Methods: A secondary analysis of the primary study was performed to quantify serum cytokine levels for correlation to pain scores. Cytokines with statistically significant correlations were then input into a stepwise regression analysis to generate a predictive equation for a patient’s pain severity. In an effort to find additional potential biomarkers, correlation analysis was performed between these factors and a more comprehensive panel of cytokines and chemokines from breast, lung, and prostate cancer patients.
Results: Statistical analysis identified nine cytokines (GM-CSF, IFNγ, IL-1β, IL-2, IL-4, IL-5, IL-12p70, IL-17A, and IL-23) that had significant negative correlations with pain scores and they could best predict pain severity through a predictive equation generated for this specific evaluation. After performing a correlation analysis between these factors and a larger panel of cytokines and chemokines, samples from breast, lung and prostate patients showed distinct correlation profiles, highlighting the clinical challenge of applying pain-associated cytokines related to more defined nociceptive states, such as arthritis, to a cancer pain state.
Conclusion: Exploratory analyses such as the ones presented here will be a beneficial tool to expand insights into potential cancer-specific nociceptive mechanisms and to develop novel therapeutics.
Keywords: biomarkers, cancer-induced pain, nociception, immune factors
Introduction
The bone is the common secondary site for some of the most prevalent cancers including breast, lung, and prostate. Patients with bone metastases, which are often associated with advanced disease, are living longer with this burden due to improved cancer therapeutics that prolong lifespan in cancer patients. Cancer-induced pain (CIP), which is commonly the most severe form of metastatic tumor development, is a multifaceted and heterogeneous pain state that exhibits characteristics of neuropathic and inflammatory pain. Currently, CIP is most commonly treated with radiotherapy, non-steroidal anti-inflammatories, opioids, and bone-targeting agents such as bisphosphonates and denosumab.1 These options unfortunately do not provide adequate analgesia in cancer patients, with 50% of the cancer patients having suboptimal pain control and deteriorating quality of life.2 This observation emphasizes the need to identify novel therapeutic targets that can provide adequate analgesia while helping to preserve a patient’s quality of life. Continued exploration of the cancer pain state, which may vary by type of the primary cancer as well as by subtype, is crucial for the development of novel therapeutics and the improvement of pain palliation in cancer patients.
Biomarker studies examining factors associated with pain development or analgesia have focused on analyzing factors that characterize non-cancer pain conditions such as inflammatory or neuropathic pain, which may have more well-defined nociceptive mechanisms. While cancer pain shares some features of inflammatory and neuropathic pain, it also includes unique characteristics that suggest that it be viewed as an independent pain state.3 Therefore, establishing biomarker profiles specifically associated with CIP may inform the application of disease-tailored analgesic agents. Several studies that have included CIP patients primarily focus on identifying markers that will predict an individual’s analgesic response to radiotherapy but limit their analysis to urinary markers of bone turnover and do not address the other modulatory factors that can propagate CIP.4–7
Recent research has indicated that cytokines play a key role in mediating cancer pain.8 Infiltrating pro-inflammatory immune cells found within tumors, as well as cancer cells themselves, release cytokines, which bind to and sensitize neighbouring nociceptors to painful stimuli and elicit a central pain response.8 Cancer is a systemic inflammatory state, and many of the symptoms experienced by cancer patients, including pain, can be attributed to the action of cytokines on the peripheral and central nervous systems.9 In healthy individuals, pro- and anti-inflammatory cytokines exist in equilibrium which is disrupted in the development of cancer, with patients showing both immuno-stimulatory and immunosuppressive profiles.10–12 In a cancer patient, cytokine levels may vary with disease stage, tumor subtype and chemotherapy/treatment.13 Given the heterogeneity of the disease itself and treatment regimens, it has proven difficult to associate a symptom such as pain, with any one specific biomarker.12
In an effort to further characterize this complex disease state and to generate new data for applying more tailored analgesic regimens, we reanalyzed samples from an existing clinical trial of breast cancer patients with bone metastases to quantify levels of circulating cytokines and growth factors in serum collected from cancer patients. This exploratory, secondary analysis was conducted using samples from a clinical trial, the TRIUMPH study, whose primary goal was to examine the efficacy of an altered bisphosphonate regimen for breast cancer patients with bone metastases in order to find a more optimal schedule for intravenous bisphosphonate administration.14,15 Serum samples and pain data were collected at 0, 12, 24, 36, and 48 weeks, corresponding to the timing of bisphosphonate administration. We then made further correlations between the specific factors that best represented changes in pain from the TRIUMPH study and a more comprehensive panel of 42 factors that included cytokines, chemokines, and growth factors. These compounds were analyzed in a set of 150 patient samples acquired from the Ontario Tumour Bank (OTB), including 50 samples each from late-stage breast, lung, or prostate cancer patients.
Methods
Sample Collection for Pain Model
Patient data and serum samples from 57 patients, provided by the TRIUMPH study were utilized for this secondary analysis.15 The aim of the TRIUMPH study was to determine whether switching from 3 to 4 weekly pamidronate treatments to 12 weekly treatments would be effective in treating patients with metastatic breast cancer. All eligible participants were female breast cancer patients with bone metastases who had a minimum of 3 months of 3–4 weekly intravenous pamidronate treatments in the past. In addition, participants were required to have serum C-telopeptide (CTx) levels of less than or equal to 600 ng/L, indicating their status as low-risk for skeletal-related events. Patients who consented to provide urine and serum samples for future research had their blood drawn after an overnight fast but before pamidronate treatment at baseline and weeks 12, 24, 36, and 48. Patients were also asked to complete the Brief Pain Inventory (BPI) and Functional Assessment of Cancer Therapy-Bone Pain (FACT-BP) to assess pain levels at baseline and weeks 12, 24, 36, and 48. The trial was approved by the Ontario Cancer Research Ethics Board, Toronto, Canada. Furthermore, the patient consent obtained for the trial was written informed consent and it was conducted in accordance with the Declaration of Helsinki.
Secondary Sample Accruement
The OTB established by the Ontario Institute of Cancer Research is a biobank of cancer-related biospecimens available to researchers undertaking translational research. Fifty plasma samples from banked breast, lung, and prostate cancer patients were obtained, with a special request for samples representing late-stage disease, if possible, in order to increase the likelihood that the sampled population had experienced a metastatic event to the bone. These patient samples were selected to better reflect the bone metastasis patients in the TRIUMPH pain model described above.
Biochemical Analysis
Serum samples were stored at −80°C until use. Prior to analysis of analyte concentrations, each sample was centrifuged at 14,000 rpm at 4°C for 10 mins. One hundred microliters of serum was transferred to 0.5 mL microtubes (Diamed Lab Supplies Inc., Mississauga, Ontario, Canada). The serum samples from the TRIUMPH study were sent to Eve Technologies for analysis utilizing the Human High Sensitivity T-Cell Discovery Array 14-plex (HDHSTC14). This panel included the following factors: GM-CSF, IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-13, IL-17A, IL-23, TNF-α (Table 1). The secondary plasma samples acquired from the OTB were analyzed for an array of 42 cytokines/chemokines (EGF, Eotaxin-1, FGF-2, Flt-3L, Fractalkine, G-CSF, GM-CSF, GRO(α), IFN-α2, IFN-γ, IL-1α, IL-1β, IL-1Ra, IL-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-12 (p40), IL-12 (p70), IL-13, IL-15, IL-17A, IL-18, IP-10, MCP-1, MCP-3, MDC, MIP-1α, MIP-1β, PDGF-AA, PDGF-AB/BB, RANTES, sCD40L, TGF-α, TNF-α, TNF-β, VEGF-A) in addition to TGF-β1, 2 and 3. Eve Technologies uses multiplex bead technology to analyze multiple analyte levels simultaneously. All samples were run twice and the average concentration was then used.
 |
Table 1 Correlation of Each Cytokine with Combined BPI Severity Scores |
Statistical Analyses
BPI pain severity ratings were acquired from the TRIUMPH study and a simple univariate linear regression was run between compiled BPI severity ratings with each corresponding cytokine measured. Statistically significant correlations (p<0.05) were input into a stepwise regression analysis to model which factors (from 1 to 9) would best predict pain scores. All possible models were calculated, and model averaging was used to generate the linear equation for pain prediction. Eight of the 9 cytokines identified in the above analysis were entered into a correlation matrix using the quantified levels of the 45 factors from the OTB patient plasma samples. Of these, all cytokines found to best predict pain were included, with the exception of IL-23. Data are reported in a heat map color-coded by correlation.
Results
Analysis of TRIUMPH Data
Both pain assessment methods (FACT-BP and BPI) indicated that all patients entered the study with low to moderate pain.15 Based on the primary results of the TRIUMPH study, BPI severity was the only pain measure that had prognostic value and was therefore used as the pain benchmark in developing the pain model used in the current investigation.15 Mean BPI severity scores were analyzed over five time points (baseline, 12, 24, 36, and 48 weeks). Pain scores appear to show a general upward trend over time; however, mean pain scores at each time point were not statistically different from one another. The mean baseline score was the lowest at 1.0202, while 48 weeks reflected the highest mean pain score of 1.95652.
Association Between Cytokine Concentrations and Pain Severity
In an exploratory analysis to examine whether any of the cytokines correlated with pain, BPI severity scores were combined independent of patient number and time point, and their matched cytokine concentrations were subjected to a bivariate correlation analysis to identify factors that have the strongest correlation with BPI pain severity. From this analysis, GM-CSF, IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-12p70, IL-17A, and IL-23 independently showed a significant correlation with BPI pain severity scores (Table 1). These factors were then run in a multivariate, stepwise regression model to identify which set of factors have the strongest predictive capacity of BPI severity. All possible fit models that included 1–9 of the significant (p<0.05) cytokines from the bivariate regression analysis were calculated (Table 2). An average of the models with 1 to 9 terms generated a formula (Equation 1) that provided a predicted pain score based on the concentrations of the above cytokines. Predicted pain scores were then correlated to report BPI severity pain scores from the TRIUMPH study using Equation 1, which is illustrated in Figure 1 depicting a correlation of R2=0.2.
 |
Table 2 Stepwise Regression Models |
 |
Figure 1 Pain score predicted using Equation 1 relative to the actual reported BPI severity score from the TRIUMPH study. |
Equation 1 represents the regression equation generated from an average of stepwise regression models:
1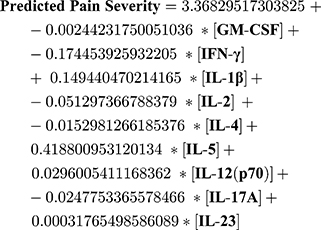
To expand the exploration of potential factors that could be measured in future studies focused on identifying biomarkers that define cancer pain, we conducted a correlation analysis of GM-CSF, IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-12(p70), and IL-17A with the second set of 45 factors to examine how these factors, which were the ones with the strongest predicative ability of BPI severity, correlated with additional factors in 3 cancer patient populations. Due to the heterogeneity of each cancer population, this data provided information on variations in cytokine and chemokine profiles and how they correlate with exploratory “pain predictive” cytokines. Figure 2 clearly depicts how patient samplings from breast, lung and prostate cancers exhibit markedly different correlation profiles compared to the identified factors.
Discussion
Biomarker analysis may be a promising approach to help predict pain severity and potentially provide a means to more objectively measure pain in patients. A recent study by Niculescu et al (2019) examined blood biomarkers and their association with pain in psychiatric patients using a whole-genome approach at the mRNA level.16 They identified a set of biomarkers with a predictive capacity for future pain and emergency department (ED) visits for pain. An interesting finding from this study includes the fact that future ED visits were better predicted by the biomarkers in independent cohorts compared to other clinical markers, such as the visual analogue scale (VAS), that are typically used.16 This shows the potential clinical value in using biomarkers to predict pain.
The current investigation represents an exploratory analysis using serum cytokine concentrations to predict a pain intensity rating in a sample population of metastatic breast cancer patients, providing a model for identifying cytokines that can best predict CIP severity. Although exhibiting properties of inflammatory and neuropathic pain, the study of cancer pain will benefit from this type of analysis in prospective studies with greater statistical power, as it is clear from this preliminary analysis that specific cytokine profiles can vary by cancer type. The differences between these cancer types shown here were in line with altered cytokine profiles identified in a comprehensive review by Lippitz (2013), which showed that cytokine fluctuations were present in some cancer types while being absent in others.11 It has also been shown that variations in subtypes of a single cancer type can vary a patient’s cytokine profile, with a general up-regulation in cytokine production as the disease progresses.13,17
In the current study, all of the cytokines that best correlated with the BPI pain severity scoring predicted a decrease in pain intensity when cytokine levels increased (Pearson r). The review by Lippitz (2013) can provide some information about this finding since they examined common patterns in tumor-induced immune activation and suppression that resulted in dysregulated immune responses of cancer patients.11 This observation highlights that dysfunctional feedback networks can potentially influence cytokine production, potentially changing their common functions in homeostasis, and even be associated with the development of a hypo-responsive state of immune cells in the tumor microenvironment.18 This may provide some insight into the negative association of some pro-inflammatory cytokines with pain in the model described here.
Knowledge of the roles of each cytokine used to generate the predictive equation for pain scores will improve the understanding of how these factors may inform future analyses. GM-CSF functions to drive differentiation and proliferation of stem cells into granulocytes and monocytes.19 Additionally, it is also often described in inflammatory and neuropathic pain as a pro-nociceptive cytokine.20 The IL-2 receptor has been shown to be expressed on peripheral nerves.21 Similarly, IL-2 is a pro-inflammatory cytokine that is well known for its role in the expansion and differentiation of effector T-cells.22 However, it is also involved in controlling the immune system by allowing the survival of T regulatory cells, which are important in preventing autoimmunity. Although this cytokine is considered to be pro-inflammatory, lower levels of IL-2 have been associated with cancer progression.11 In addition, in vivo studies have described anti-nociceptive effects associated with IL-2. Song et al (2000) found that the intraplantar injection of IL-2 in rats increased their threshold to pain.23 Similarly, intrathecal administration of the IL-2 gene (recombined in a pcDNA3 vector) to rats experiencing chronic neuropathic pain also demonstrated its anti-nociceptive effects.24 These findings could explain why a negative relationship between pain in cancer patients and IL-2 levels was observed in the present study.
Additional pro-inflammatory cytokines include TNF-α and IL-1β, they have both been associated with metastatic bone pain. Tumor cells secrete IL-1β into the microenvironment, where it binds to ion channels within neighbouring nociceptors, thereby sensitizing these pain receptors to further painful stimuli. Pain signals are then transferred to the brain, resulting in the pain perception. The release of TNF-α from tumor cells also plays a role in moderating bone metastasis pain by stimulating osteoclasts, which creates an acidic environment that may contribute to pain through acid-sensing nociceptors.25 IL-17A is another pro-inflammatory cytokine that is predominantly produced by a specific subtype of CD4+ T-cells.26 It has been linked to neuropathic pain induced by a spine ligation, stimulating the movement of astrocytes and other pro-inflammatory cytokines to the site of inflammation.27 Another pro-inflammatory cytokine is IL12(p70) which is involved in the proliferation of natural killer cells and T cells, and helps to enhance their cytotoxic activity. It was hypothesized to have been linked with pain development in cancer patients that were treated with IL-12 in a clinical trial and when it was injected in plantar tissue in rats, it had an algesic effect.28 In contrast to TNF-α, IL-1β and IL12(p70), IL-4 is an anti-inflammatory cytokine that is involved in the suppression of numerous pro-inflammatory cytokines, such as IL-1β and TNF-α.29 It has been shown to help mediate analgesic effects of exercising in mice that had neuropathic pain.30
Little information is available on the direct roles of IFN-γ, IL-23, and IL-5 in pain. IFN-γ plays an important role in the expression of the Major Histocompatibility Complex (MHC), which is a crucial part of the immune system, as it helps in the detection of antigens. Therefore, lower levels of IFN-γ production by immune cells have been associated with various types of cancer.11 In addition, IFN-γ is produced by immune cells, playing a key role in CD4+ Th1 cells, which are generally considered to be pro-inflammatory.31 Higher levels of IL-23 have been observed in patients with various cancers, including breast cancer. It is involved in the infiltration of cells from the innate immune system into tumors.11 In addition, this cytokine is involved in the “IL-23/IL-17 axis” of inflammation, inducing naive CD4+ T cells to differentiate into highly pathogenic helper T cells (Th17) that produce IL-17 and TNF-α, but not IFN-γ.32 IL-5 plays a crucial role in acquired and innate immunity as it is involved in the differentiation of B cells and in eosinophil activation.33 IL-5 has been implicated in inflammation involved in allergic diseases such as asthma, but its role in cancer and neuropathic pain is less studied.33
Although research on using cytokines as potential biomarkers for CIP is limited, there are several studies where cytokines were found to have a strong correlation with cancer pain. Starkweather et al (2013) analyzed 17 different inflammatory cytokines in serum samples from 32 patients with early stages of breast cancer, prior to chemotherapy.34 The study was conducted to examine whether cytokine levels could be associated with symptoms of cancer, including pain. It was found that patients with higher levels of pain had higher levels of c-reactive protein (CRP), interleukin-13 (IL-13), interleukin-7 (IL-7), pain interference, depression, and sleep disturbances.34 Another study conducted by Laird et al (2011) examined samples from patients with gastrointestinal, lung, and pancreatic cancer, reporting that CRP was positively correlated with CIP.35 These studies, together with the results presented here, will hopefully advance the utilization of cytokines as biomarkers for CIP.
Important limitations of this study include use of a relatively small population size to generate the predictive pain model. Several patient samples had to be omitted, as some of the cytokine levels were not within the detection limit of the assay, leading to a further reduction in sample size. Due to the limited sample size, subgroup analysis could not be carried out. Given that subgroup analysis was not possible, patients could not be separated into low and high pain score groups to compare their cytokine levels. It should also be noted that patients involved in the TRIUMPH study had relatively little pain and they were required to have low CTx levels for trial eligibility. They were also on a bisphosphonate regimen, and bisphosphonates are known to modulate inflammatory cytokine production and pain.36–38 Therefore, more datasets and populations of cancer patients experiencing CIP with their associated pain scores need to be examined to make further conclusions. Absence of the pain scores in the samples received from the OTB is another limitation in this study, as further correlation between cytokine levels and pain scores could not be examined. The lack of pain scores highlights the importance of having pain as a regular measure for cancer populations and that this information should become a standard part of tumor registries and biobanks, so future studies of cancer-related pain can be completed. Furthermore, the cytokines used to generate the predictive equation were derived from female breast cancer patients, and will therefore need to be evaluated in males. It is known that there are sex differences in the immune system, and sex differences in pain.39,40 Although statistically significant, the degree of correlation in the exploratory analysis is weak, so definite conclusions cannot be drawn, but it does give some insight into the potential use of cytokines as biomarkers for CIP.
Conclusion
The current investigation provides an interesting exploratory tool to examine the complex relationship between pain and immune factors that play a role in CIP, especially in light of the heterogeneous nature of this complex disease. Unique analyses such as the ones described here are therefore important in investigating the mechanisms of CIP as well as identifying potential biomarkers that can be used to classify this distinctive pain state in patients. Biomarkers with predictive abilities can be beneficial as health-care moves toward more personalized treatment regimens and may help in monitoring the progression of pain in cancer patients.
Acknowledgments
We would like to acknowledge Atefeh Noori and Dr. Vahid Ashoorion for their assistance with data analysis and statistics. This work was supported by the Canadian Institutes of Health Research (CIHR) Strategy for Patient-Oriented Research (SPOR) grant.
Author Contributions
All of the authors made substantial contributions to the conception and design, data acquisition or data analysis and interpretation. They also helped draft the manuscript or revise it critically. In addition, all authors have approved the final version to be published. Lastly, all authors agree to be accountable for all aspects of the work and ensure any questions regarding accuracy or integrity be addressed appropriately.
Disclosure
The authors declare that they have no competing interests.
References
1. Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997;69(1–2):1–18. doi:10.1016/s0304-3959(96)03267-8
2. Christo PJ, Mazloomdoost D. Cancer pain and analgesia. Ann N Y Acad Sci. 2008;1138:278–298. doi:10.1196/annals.1414.033
3. Falk S, Dickenson AH. Pain and nociception: mechanisms of cancer-induced bone pain. J Clin Oncol off J Am Soc Clin Oncol. 2014;32(16):1647–1654. doi:10.1200/JCO.2013.51.7219
4. Chow E, Hird A, Zhang L, et al. Change in urinary markers of osteoclast activity following palliative radiotherapy for bone metastases. Clin Oncol. 2009;21(4):336–342. doi:10.1016/j.clon.2009.01.013
5. Chow E, Deangelis C, Chen BE, et al. Effect of re-irradiation for painful bone metastases on urinary markers of osteoclast activity (NCIC CTG SC.20U). Radiother Oncol. 2015;115(1):141–148. doi:10.1016/j.radonc.2015.02.025
6. Gardner K, Laird BJA, Fallon MT, Sande TA. A systematic review examining clinical markers and biomarkers of analgesic response to radiotherapy for cancer-induced bone pain. Crit Rev Oncol Hematol. 2019;133:33–44. doi:10.1016/j.critrevonc.2018.10.008
7. Hoskin PJ, Stratford MR, Folkes LK, Regan J, Yarnold JR. Effect of local radiotherapy for bone pain on urinary markers of osteoclast activity. Lancet (London, England). 2000;355(9213):1428–1429. doi:10.1016/s0140-6736(00)02144-9
8. Vendrell I, Macedo D, Alho I, Dionísio MR, Costa L. Treatment of cancer pain by targeting cytokines. Mediators Inflamm. 2015;2015:1–11. doi:10.1155/2015/984570
9. Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919–2925. doi:10.1002/cncr.11382
10. Lippitz BE, Harris RA. Cytokine patterns in cancer patients: a review of the correlation between interleukin 6 and prognosis. Oncoimmunology. 2016;5(5):e1093722. doi:10.1080/2162402X.2015.1093722
11. Lippitz BE. Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol. 2013;14(6):e218–e228. doi:10.1016/S1470-2045(12)70582-X
12. Ø P, Laird B, Aass N, et al. The relationship between pro-inflammatory cytokines and pain, appetite and fatigue in patients with advanced cancer. PLoS One. 2017;12(5):e0177620. doi:10.1371/journal.pone.0177620
13. Panis C, Pavanelli WR. Cytokines as mediators of pain-related process in breast cancer. Mediators Inflamm. 2015;2015:1–6. doi:10.1155/2015/129034
14. Kuchuk I, Beaumont JL, Clemons M, Amir E, Addison CL, Cella D. Effects of de-escalated bisphosphonate therapy on the functional assessment of cancer therapy-bone pain, brief pain inventory and bone biomarkers. J Bone Oncol. 2013;2(4):154–157. doi:10.1016/j.jbo.2013.07.004
15. Addison CL, Bouganim N, Hilton J, et al. A Phase II, multicentre trial evaluating the efficacy of de-escalated bisphosphonate therapy in metastatic breast cancer patients at low-risk of skeletal-related events. Breast Cancer Res Treat. 2014;144(3):615–624. doi:10.1007/s10549-014-2906-x
16. Niculescu AB, Le-Niculescu H, Levey DF, et al. Towards precision medicine for pain: diagnostic biomarkers and repurposed drugs. Mol Psychiatry. 2019;24(4):501–522. doi:10.1038/s41380-018-0345-5
17. Panis C, Victorino VJ, Herrera ACSA, et al. Differential oxidative status and immune characterization of the early and advanced stages of human breast cancer. Breast Cancer Res Treat. 2012;133(3):881–888. doi:10.1007/s10549-011-1851-1
18. Jiang Y, Li Y, Zhu B. T-cell exhaustion in the tumor microenvironment. Cell Death Dis. 2015;6(6):e1792. doi:10.1038/cddis.2015.162
19. Nicol LSC, Thornton P, Hatcher JP, et al. Central inhibition of granulocyte-macrophage colony-stimulating factor is analgesic in experimental neuropathic pain. Pain. 2018;159(3):550–559. doi:10.1097/j.pain.0000000000001130
20. Hamilton JA. Colony-stimulating factors in inflammation and autoimmunity. Nat Rev Immunol. 2008;8(7):533–544. doi:10.1038/nri2356
21. Schweizerhof M, Stösser S, Kurejova M, et al. Hematopoietic colony–stimulating factors mediate tumor-nerve interactions and bone cancer pain. Nat Med. 2009;15(7):802–807. doi:10.1038/nm.1976
22. Abbas AK, Trotta E, Simeonov RD, Marson A, Bluestone JA. Revisiting IL-2: biology and therapeutic prospects. Sci Immunol. 2018;3(25):eaat1482. doi:10.1126/sciimmunol.aat1482
23. Song P, Zhao ZQ, Liu XY. Expression of IL-2 receptor in dorsal root ganglion neurons and peripheral antinociception. Neuroreport. 2000;11(7):1433–1436. doi:10.1097/00001756-200005150-00016
24. Yao M-Z, Gu J-F, Wang J-H, et al. Interleukin-2 gene therapy of chronic neuropathic pain. Neuroscience. 2002;112(2):409–416. doi:10.1016/S0306-4522(02)00078-7
25. Aielli F, Ponzetti M, Rucci N. Bone metastasis pain, from the bench to the bedside. Int J Mol Sci. 2019;20:2. doi:10.3390/ijms20020280
26. de Oliveira CMB, Sakata RK, Issy AM, Gerola LR, Salomão R. Cytokines and pain. Rev Bras Anestesiol. 2011;61(2):
27. Sun C, Zhang J, Chen L, et al. IL-17 contributed to the neuropathic pain following peripheral nerve injury by promoting astrocyte proliferation and secretion of proinflammatory cytokines. Mol Med Rep. 2017;15(1):89–96. doi:10.3892/mmr.2016.6018
28. Chen I-F, Khan J, Noma N, et al. Anti-nociceptive effect of IL-12p40 in a rat model of neuropathic pain. Cytokine. 2013;62(3):401–406. doi:10.1016/J.CYTO.2013.03.021
29. Hao S, Mata M, Glorioso JC, Fink DJ. HSV-mediated expression of interleukin-4 in dorsal root ganglion neurons reduces neuropathic pain. Mol Pain. 2006;2:
30. Bobinski F, Teixeira JM, Sluka KA, Santos ARS. Interleukin-4 mediates the analgesia produced by low-intensity exercise in mice with neuropathic pain. Pain. 2018;159(3):437–450. doi:10.1097/j.pain.0000000000001109
31. Castro F, Cardoso AP, Gonçalves RM, Serre K, Oliveira MJ. Interferon-gamma at the crossroads of tumor immune surveillance or evasion. Front Immunol. 2018;9:847. doi:10.3389/fimmu.2018.00847
32. Iwakura Y, Ishigame H. The IL-23/IL-17 axis in inflammation. J Clin Invest. 2006;116(5):1218–1222. doi:10.1172/JCI28508
33. Kouro T, Takatsu K. IL-5- and eosinophil-mediated inflammation: from discovery to therapy. Int Immunol. 2009;21(12):1303–1309. doi:10.1093/intimm/dxp102
34. Starkweather AR, Lyon DE, Schubert CM. Pain and inflammation in women with early-stage breast cancer prior to induction of chemotherapy. Biol Res Nurs. 2013;15(2):234–241. doi:10.1177/1099800411425857
35. Laird BJA, Scott AC, Colvin LA, et al. Cancer pain and its relationship to systemic inflammation: an exploratory study. Pain. 2011;152(2):460–463. doi:10.1016/j.pain.2010.10.035
36. Coleman RE. Impact of bone-targeted treatments on skeletal morbidity and survival in breast cancer. Oncology (Williston Park). 2016;30(8):695–702.
37. Ferretti G, Fabi A, Carlini P, et al. Zoledronic-acid-induced circulating level modifications of angiogenic factors, metalloproteinases and proinflammatory cytokines in metastatic breast cancer patients. Oncology. 2005;69(1):35–43. doi:10.1159/000087286
38. Hendriks LEL, Hermans BCM, van den Beuken-van Everdingen MHJ, Hochstenbag MMH, Dingemans A-MC. Effect of bisphosphonates, denosumab, and radioisotopes on bone pain and quality of life in patients with non-small cell lung cancer and bone metastases: a systematic review. J Thorac Oncol off Publ Int Assoc Study Lung Cancer. 2016;11(2):155–173. doi:10.1016/j.jtho.2015.10.001
39. Sorge RE, Totsch SK. Sex differences in pain. J Neurosci Res. 2017;95(6):1271–1281. doi:10.1002/jnr.23841
40. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638. doi:10.1038/nri.2016.90
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

