Back to Journals » Risk Management and Healthcare Policy » Volume 15
Application of the Plan–Do–Check–Act Cycle in Shortening the Decision to Delivery Interval Time
Authors Lu MN, Zhang BL, Dai QH, Fu XH
Received 14 February 2022
Accepted for publication 10 June 2022
Published 6 July 2022 Volume 2022:15 Pages 1315—1323
DOI https://doi.org/10.2147/RMHP.S362420
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Kyriakos Souliotis
Ming-Na Lu, Bai-Lei Zhang, Qiao-Hong Dai, Xian-Hu Fu
Department of Obstetrics and Gynecology, Ningbo Women and Children’s Hospital, Ningbo, 315012, People’s Republic of China
Correspondence: Qiao-Hong Dai, Department of Obstetrics and Gynecology, Ningbo Women and Children’s Hospital, Ningbo, 315012, People’s Republic of China, Tel +86 13858220557, Email [email protected]
Objective: To discuss the application value of the plan–do–check–act (PDCA) cycle in shortening the decision to delivery interval (DDI) time.
Methods: A total of 106 DDI cases from the Ningbo Women and Children’s Hospital (China) from January 2019 to December 2020 were selected as the subjects of this study. The causes for the prolongation of DDI were analyzed and protocols were developed. Through continuous summaries and improvement, a standardized process was established to direct clinical application, ie, the PDCA cycle.
Results: The DDI was shortened from 14.26 min in 2019 to 12.18 min in 2020 and the neonatal asphyxia rate significantly decreased from 34.69% in 2019 to 12.50% in 2020 (P < 0.05).
Conclusion: The PDCA cycle management mode effectively shortened the DDI time and reduced the neonatal asphyxia rate, without increasing adverse maternal outcomes.
Keywords: PDCA cycle, emergency C-delivery, DDI, neonatal, asphyxia
Introduction
For acutely and critically ill pregnant women, performing a Cesarean (C)-delivery for the rapid termination of a pregnancy is an effective approach when it comes to saving the lives of both the mother and the fetus and improving the maternal and infant prognosis. The American College of Obstetricians and Gynecologists (ACOG, 1989) suggests that an emergency C-delivery and the decision to delivery interval (DDI) time should not exceed 30 minutes.1 In an exceptional emergency, when conducting an immediate C-delivery to save the lives of the mother and the fetus, the DDI should be equal to or less than 5 minutes.2 Shortening the DDI time has always been a major concern in the obstetrics department of our hospital. It is, however, difficult for conventional management methods to achieve success in this regard because DDI time involves numerous links.
In recent years, some studies have proposed applying the Plan-Do-Check-Act (PDCA) cycle management in various types of surgical management, where it plays a positive role in the nursing management of the diagnosis and treatment of various diseases.3,4 The PDCA cycle, also known as the Daiming cycle, is an effective way to solve problems and implement solutions.5 Four consecutive stages characterize it: (I) Plan: find, describe, and dissect problems; (II) Do: study and discuss effective countermeasures; (III) Check: test the specific implementation effect of protocols
and analyze whether there are methods and measures for improvement; (IV) Act: specifically apply the scheme to clinical practice. Therefore, the purpose of this experiment is to study whether good results can be obtained by applying PDCA cycle to shorten DDI time.
Materials and Methods
General Materials
A retrospective study method was adopted for the current research. A total of 106 DDI cases were selected from our hospital from January 2019 to December 2020 as the study subjects. Cause analysis, causal factor analysis, and root cause analysis were conducted for the prolongation of DDI time. Additionally, relevant protocols were developed. Through continued summaries and improvement implementation, a standardized process was established to direct the clinical practice. This study was conducted in accordance with the declaration of Helsinki and approved by the Ethics Committee of Ningbo Women and Children’s Hospital. Written informed consent was obtained from all participants.
Study Methods
Planning
In 2019, our hospital had an average DDI time of 14.40 minutes, a neonatal asphyxia rate of 34%, a DDI of more than 30 minutes for 4% of the selected cases, and a 5-minute C-delivery rate of only 8.33% in the delivery room. Through investigation and authentication, brainstorming discussions were conducted to analyze the factors impacting DDI time; a process study on DDI prolongation cases was also again conducted. The subsequently derived causes were made into a fishbone diagram (Figure 1).
 |
Figure 1 Fishbone diagram of cause. |
Through a demonstration via Plato analysis, three aspects were identified as major causes, ie, a defective process, a lack of first-aid experience, and poor cooperation among departments (as shown in Figure 2).
 |
Figure 2 Proportions of causes. |
We set a target to shorten the emergency DDI time to within 30 minutes and the DDI in the delivery room to within 5 minutes. Improvement measures were developed for the major causes. Multi-disciplinary cooperation was carried out among the obstetrics emergency department, the obstetrics ward, the delivery room, the anesthesiology department, the operating room, the neonatology department, the laboratory department, the blood transfusion department, the B-ultrasound room, and the fetal heart-rate monitoring room. The different team members worked together on the development of countermeasures for the causes shown in Figure 1, monthly continuous monitoring, and towards the continued improvement of quality.
Do
Process Improvement
Simplifying the Surgical Process
As conventional surgical steps before the delivery of a newborn can take a long time to complete, the routine surgical disinfection was replaced by directly applying disinfectant within the disinfection area. After disinfection was complete, the assistants washed their hands and directly spread surgical drapes and covered the incision site with surgical film. The operating rooms were equipped with simplified DDI operation kits that included disposable scalpels, curved forceps, a wire retractor, as well as gauze, to rapidly begin the operation for delivery of the newborn.
Improving DDI Time First-Aid Processes at Different Start Places
Processes are improved separately at different DDI starting places, including in the emergency area, in non-emergency areas, in the ultrasound department, the delivery room, the fetal heart-rate monitoring room, and in the ward.
Establishing a Special DDI Team and Standardizing Its Working Processes
A 24-hour duty system and a system of personal responsibility were adopted. The DDI specialists were assigned and equipped with mobile phones. Special operating rooms and surgical patient elevators were set out. In the case of an emergency, if the surgeon and operating room nurses were not in position after the arrival of a patient in the operating room, the outpatient obstetrician or the emergency obstetrician and maternity assistants would immediately wash their hands, perform disinfection and spread the surgical drapes, and then begin the procedure. They would be substituted once the surgeon and operating room nurses were in position or after the delivery of the newborn if necessary. If an emergency C-delivery indication was reported in the delivery process, the most senior doctor or the second-line duty doctor in the delivery room would provide the relevant instructions. The medical care personnel in the delivery room were required to instantly transfer the pregnant woman to an operating room of the delivery room and concurrently complete preoperative preparation and inspection. If necessary, a C-delivery would be performed by the physician in the delivery room, who may be replaced following the arrival of the surgeon of the relevant inpatient area or the surgeon on a night shift in the operating room, provided that the mother and the newborn were safe. The anesthesiology department and the perinatal department would be contacted to immediately rush to the operating room of the delivery room.
Continued enhancement of first-aid experience.
Establishing a Critically-Ill Pregnant and Postpartum Patient Emergency Treatment Team
To further enhance disease assessment and emergency treatment, senior doctors with clinical first-aid experience and command capabilities were selected from the obstetrics department as the frontline doctors for the emergency treatment of pregnant women and to organize other personnel in the creation of an emergency treatment team. The second-line obstetrician on duty on the same day served as the second-line doctor for the emergency treatment of pregnant women and also as the general director of emergency treatment.
Carrying Out a Variety of Training
To improve the clinical first-aid capabilities of obstetricians, we continually carry out a variety of training in the form of, eg, obstetrical safety meetings, discussions on intractable and critical cases in obstetrics, discussions on neonatal asphyxia cases, teaching emergency C-delivery processes, emergency obstetrician training and assessment, informing on various updated obstetrics guidelines, theoretical training and assessment about fundamental theories, knowledge and the skills of obstetrics, neonatal resuscitation training, and electric defibrillation and assessment.
Following the start of the DDI time for each case, a quality control form must be completed, summarized, and analyzed. The first contact doctor was responsible for whole-process tracking and for completing the form by recording the time taken to complete each process, the intraoperative conditions, and fetal prognosis. The department head was responsible for corresponding checks, giving appropriate advice, and delivering rectification requirements if needed. The general department head was responsible for creating the relevant reviews. Finally, the DDI special team held regular discussions, created summaries, and filed the relevant data.
Further improvement of cooperation among departments.
The Continued Improvement of Processes in Other Departments
An emergency C-delivery requires multi-disciplinary team cooperation involving the anesthesiology, obstetrics, and neonatology departments, operating room nurses, and obstetric nurses. We aim to implement continuous improvements in the relevant processes related to medical technology, blood transfusion, and laboratory departments, as well as in the operating rooms. All the departments are in close contact with one another via specialized first-aid personnel and telephones. Team members are well-trained and cooperate well.
Conducting Periodic Multi-Department First-Aid Drills
Emergency treatment drills are organized in turn in the obstetrics department, operating room, delivery room, and perinatal department on a quarterly basis. An emergency C-delivery drill is carried out once a month in the delivery room. An emergency C-delivery DDI drill is carried out once every quarter in the emergency and B-ultrasound areas.
Strengthening Critical Value Management
To avoid a delay in the start of DDI time caused by the failure to assign a doctor to whom the B-ultrasound room reports critical values, potential critical values must be reported to the doctor ordering the test or using a DDI-related phone line.
Check
We carried out monthly monitoring and statistical work, created summaries and evaluations regularly, and refined the cause analysis and improvement measures. We classified the start places further into two categories as follows: 1) The start of DDI procedures in the outpatient and emergency departments and wards; 2) the start of DDI procedures in the delivery room.
Statistical Methods
All data were incorporated into the SPSS Statistics 22.0 software for statistical analysis. The measurement data were expressed as ( ), and two independent sample t-tests were performed. The enumeration data were expressed as a percentage (%), and a comparison was made by chi-square test or using Fisher’s exact probability method; P < 0.05 indicated a statistically significant difference.
), and two independent sample t-tests were performed. The enumeration data were expressed as a percentage (%), and a comparison was made by chi-square test or using Fisher’s exact probability method; P < 0.05 indicated a statistically significant difference.
Comparison of the DDI Time and Neonatal Asphyxia Rate
The DDI time was shorter in 2020 (12.18 min) than in 2019 (14.40 min); the neonatal asphyxia rate significantly decreased from 34.00% to 12.50%, indicating a statistically significant difference (P < 0.05). No severe neonatal asphyxia or a DDI > 30 min was reported in the DDI cases of 2020 (see Table 1).
 |
Table 1 DDI and Neonatal Asphyxia Rate |
A Comparison of Emergency C-Delivery Initiated in the Delivery Room
The operating room of an emergency C-delivery is in the delivery room; therefore, an emergency C-delivery that is initiated in the delivery room has an obvious advantage in terms of the DDI time.
The number of cases with a DDI duration below 5 min was 2 (8.72%) in 2019, and there were 6 cases (23.53%) in 2020, indicating that shortcomings remained. Compared with 2019, 2020 saw an obvious reduction in the DDI duration and the time from the start of the DDI process to the start of an operation; this indicated a statistical significance (P < 0.05). There was also a decrease in the time from the start of an operation to the delivery of a newborn, the mean value of mild neonatal asphyxia, and the mean value of severe neonatal asphyxia; however, no statistical significance was indicated for these aspects. The 5-minute C-delivery rate increased but the average DDI duration was 8.47 min (still above 5 min), indicating that continual improvement remained necessary (see Table 2).
 |
Table 2 Comparison of DDI Started in Delivery Room in 2019 and 2020 |
Act
All links with performing a C-delivery were optimized and DDI-related processes were established and continually improved to effectively shorten the DDI time for an emergency C-delivery.
Multi-disciplinary collaboration was strengthened in an ongoing manner to effect a continuous decrease in DDI time in our hospital. As the DDI was shortened, the neonatal asphyxia rate decreased continually and the incidence of adverse maternal outcomes did not increase, thereby ensuring the safety of the mother and the newborn.
Results
Comparison of the DDI Time and the Neonatal Asphyxia Rate
The PDCA cycle management enabled the DDI to be shorter in 2020 (12.18 min) than in 2019 (14.40 min). The neonatal asphyxia rate significantly decreased from 34.00% to 12.50% (P < 0.05).
Surgical Indication
The main surgical indications of DDI cases in 2020 were fetal distress and placental abruption, accounting for 92.86%. Placental abruption is the main surgical indication of emergency C-delivery initiated in the emergency and ward, and fetal distress is the main indication of those initiated in the delivery room (see Figures 3 and 4).
 |
Figure 3 Indications of C-delivery with DDI start in outpatient and emergency departments and wards. |
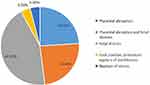 |
Figure 4 Indications of C-delivery with DDI start in the delivery room. |
Discussion
The DDI Process and Its Indications
The DDI process originated in 1988. According to a survey in the United States at the time, almost all hospitals were capable of performing emergency C-delivery within 30 minutes.6 This rule was subsequently adopted by the ACOG and the American Academy of Pediatrics.1,7 However, DDIs are not always the same; eg, in Germany, it is suggested that the DDI time be shortened to 20 min.8 The Findberg Hospital in the US proposed the concept of a 5-minute emergency C-delivery in the delivery room in 2013. The 5-minute C-delivery was introduced in China by the “No Pain Labor & Delivery – Global Health Initiative” project group. It is required when the maternal and fetal conditions suddenly become adverse in anodyne labor and are paramount for saving maternal and fetal lives.2 In this study, following improvements, no cases with a DDI of more than 30 minutes were recorded in 2020 but there was an increase in the proportion of 5-minute C-delivery. A shorter DDI time contributed to an obvious decrease in the neonatal asphyxia rate.
Lucas et al conducted a study with obstetricians and anesthetists in 2000, in which C-delivery were classified into four grades according to their degree of urgency. Among them, Category 1 represented an immediate threat to the life of the mother or the fetus. Category 2 represented a maternal or fetal compromise that was not immediately life-threatening.9 The DDI was required to be within 30 minutes for Category 1 and within 75 minutes for Category 2. The perinatal outcomes of an emergency C-delivery, particularly a Category 1 C-delivery, were worse than those for an elective C-delivery.10 This was mainly related to the disease. Fetal distress has always been a primary indicator of category 1 and 2 C-delivery.10 In this study, the main surgical indication was also fetal distress. Other indications included those posing an immediate threat to the lives of mothers and fetuses, eg, severe placental abruption, umbilical cord prolapse, uterine rupture, massive bleeding from the placenta previa, and bleeding due to rupture of the vasa previa.11,12
A perimortem C-delivery, which is also a type of emergency C-delivery, is performed mainly to save the life of the pregnant woman. It should be started within 4 minutes after sudden cardiac arrest and delivery of the newborn should be finished within 5 min. Performing a C-delivery for a woman suffering sudden cardiac arrest can effectively improve the hemodynamic state; as such, the DDI time should preferably be shorter.13
The Significance of DDI
The DDI is an effective method for saving the lives of high-risk perinatal infants and improving early neonatal outcomes.14 A study conducted by Lv et al showed that, compared to the control group, the 5-minute C-delivery group had a lower proportion of newborn infants with an Apgar score below 7 at 1 min and higher umbilical artery pH values.15 The DDI management protocol has bearing on the improvement of early neonatal outcomes.14 A study conducted by Wong et al found that an emergency C-delivery delivery was essential in the case of umbilical cord prolapse accompanied by fetal bradycardia because the bradycardia-to-delivery interval was significantly correlated with the umbilical artery pH value.16 In the case of perinatal hypoxia, oxytocia cannot systematically prevent the occurrence of ischemic encephalopathy; however, a shorter DDI time can reduce the incidence of newborn infants.
Inconsistent and even opposing conclusions have nonetheless been proposed. For example, a DDI below 30 minutes was not always associated with good neonatal outcomes.10 A study conducted by Brandt et al suggested that the duration of DDI time had no impact on the incidence of adverse neonatal outcomes.17 Another study indicated that the Apgar scores of newborn infants after an immediate C-delivery were lower than those in the control group and that the operation had specific adverse impacts on the newborn infants.14 However, such results may be associated with specific classifications of “C-delivery” or caused by specific diseases. These results may also be obtained if intrauterine fetal resuscitation had been performed concurrently with active preparation for a C-delivery after fetal distress was discovered. Moreover, the maternal anxiety arising from the decision to perform an emergency C-delivery may lead to an increase in the catecholamine concentration and, accordingly, the reduction of placental perfusion, causing transient acidosis of the newborn infant.10
The bulk of existing literature suggests that the DDI time does not cause an increase in maternal complications. For example, the comparison of postpartum hemorrhage, adjacent organ damage, blood transfusion, endometritis, pelvic abscess, transfer to the intensive care unit after an operation, incision infection and postoperative pyrexia incidence, perioperative bleeding, and length of stay suggested that the differences were of no statistical significance.14,15 However, oxytocia may increase the maternal risks,10 eg, increased blood loss and high hospitalization costs.14
How to Shorten the DDI Time
The main factors influencing the DDI time include the level of practice of obstetricians, the optimization of clinical procedures, multi-disciplinary team collaboration (including obstetrics, anesthesiology, nursing, and perinatal departments), anesthesia speed and method, as well as operating room conditions. In addition, the physical condition of the pregnant woman is also an influencing factor. For example, an obese pregnant woman and a scarred uterus will lead to the prolongation of DDI time.18 Understanding the impacts of DDI time can help to accelerate the DDI reduction process.17 Measures such as continuous training and optimization can be implemented to shorten the DDI time for an emergency C-delivery. The unnecessary delay of an operation may occur if the obstetrician and the anesthetist disagree about aspects of the operation; therefore, a unified judgment criterion and good multi-disciplinary communication are required. Based on the study conducted by Le Mitouard et al, in the case of an emergency, a color-code protocol may be adopted, with orange representing the delivery of the fetus within 30 min and red representing delivery within 15 min. This method can shorten the DDI without influencing neonatal outcomes.19 To shorten the DDI time, methods such as establishing the operating room within the delivery room and implementing attention-grabbing labels in the emergency operating room have also been adopted in some hospitals. The DDI time can be minimized by strengthening the training related to the emergency C-delivery process. Periodic simulated training is an important management mode in obstetrics for improving maternal and fetal outcomes and reducing the complications arising from an emergency C-delivery.20,21
Many quality issues have occurred due to dangerous factors within weak links. In the PDCA cycle, scientific procedures are adopted, various management techniques and methods are comprehensively utilized, continual improvement is made through process optimization, and the anti-risk capability of the system has been enhanced, thereby contributing to the radical improvement of service, treatment, and hospital management levels. It is a scientific and standard management method for effectively discovering the root causes of problems, establishing targeted treatment measures, effectively evaluating their execution, and providing continuous feedback. The PDCA cycle advocates the notion of continual improvement, team-based operation, and data-guided decision-making to continually improve specific programs and processes.
The limitations of this study are as follows: Although the DDI time in this study has decreased, the proportion of 5-minute C-delivery has increased. However, the relationship between the two is not clarified in this paper. We will study it in later experiments. In addition, the DDI team may have different DDI time results due to the different level of doctors, which cannot be ruled out.
In this paper, multiple measures, including simplifying the surgical process, simplifying the operation, improving the first-aid process, and standardizing the working processes of a special DDI team, were presented, and the PDCA cycle was applied. These methods can effectively shorten the DDI time and reduce the neonatal asphyxia rate without increasing maternal complications, and are, accordingly, worth disseminating.
Funding
This study was supported by Zhejiang medical and health science and technology project (No.2022ky337), which “Study on the mechanism of negative regulation of FGFR1 by cervical derived secretion trf-gly-gcc-010 to promote the repair of endometrium and induce the occurrence of placenta previa”.
Disclosure
The authors report no conflicts of interest in this work.
References
1. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. Number 5, July 1999 (replaces practice bulletin number 2, October 1998). Clinical management guidelines for obstetrician-gynecologists. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 1999;66(2):197–204.
2. Lipman S, Cohen S, Einav S, et al., Society for Obstetric Anesthesia and Perinatology. The Society for Obstetric Anesthesia and Perinatology consensus statement on the management of cardiac arrest in pregnancy. Anesth Analg. 2014;118(5):1003–1016. doi:10.1213/ANE.0000000000000171
3. Ueda A, Saito T, Ueda M, et al. Introduction and PDCAManagement of a liaison-clinical pathway with cancer patients after a curative operation. Gan To Kagaku Ryoho. 2015;42:1197–1201.
4. Leitmann A, Reinert S, Weise H. Surgical suture course for dental students with the Peyton-4-step approach versus the PDCA cycle using video assisted self-monitoring. BMC Oral Health. 2020;20:365. doi:10.1186/s12903-020-01309-x
5. Meehan CD, Silvestri A, Street ED. Improving blood glucose monitoring in a hospital setting using the PDCA approach. Plan, do, check, act cycle. J Nurs Care Qual. 1993;7:56–63. doi:10.1097/00001786-199307000-00010
6. ACOG. American College of Obstetricians and Gynaecologists Standards for Obstetric Services.
7. American Academy of Pediatrics, American College of Obstetrician s and Gynecologists. Guidelines for Perinatal Care.
8. Hillemanns P, Hepp H, Rebhan H, Knitza R. Emergency cesarean section– organization and decision-delivery time. Geburtshilfe Frauenheilkd. 1996;56(8):423–430. doi:10.1055/s-2007-1023258
9. Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: a new classification. J R Soc Med. 2000;93(7):346–350. doi:10.1177/014107680009300703
10. Anuradha G, Nirupama V, George S. An audit of the decision to delivery interval in emergency caesarean section and its effect on neonatal outcome. Int J Reprod Contracept Obstet Gynecol. 2020;9(10):4202–4207. doi:10.18203/2320-1770.ijrcog20204314
11. Suwal A, Shrivastava VR, Giri A. Maternal and fetal outcome in elective versus emergency cesarean section. JNMA J Nepal Med Assoc. 2013;52(192):563–566.
12. Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ. 2004;328(7441):665. doi:10.1136/bmj.38031.775845.7C
13. Jeejeebhoy FM, Zelop CM, Windrim R, et al. Management of cardiac arrest in pregnancy: a systematic review. Resuscitation. 2011;82:801–809. doi:10.1016/j.resuscitation.2011.01.028
14. Weiner E, Bar J, Fainstein N, et al. The effect of a program to shorten the decision-to-delivery interval for emergent cesarean section on maternal and neonatal outcome. Am J Obstet Gynecol. 2014;210(3):
15. Lv HR, Zhou XY. Clinical effect of 5-minute cesarean section in delivery room. Chin J Fam Planning Gynecotokol. 2018;10(12):50–52.
16. Wong L, Tse WT, Lai CY, et al. Bradycardia-to-delivery interval and fetal outcomes in umbilical cord prolapse. Acta Obstet Gynecol Scand. 2021;100(1):170–177. doi:10.1111/aogs.13985
17. Brandt JA, Morgenstern B, Thangarajah F, et al. Evaluating the decision-to-delivery interval in emergency cesarean sections and its impact on neonatal outcome. In vivo. 2020;34(6):3341–3347. doi:10.21873/invivo.12172
18. Wang Q, Zhang GZ, Wan M, et al. Analysis of the influencing factors of the operation time in urgent cesarean section. J Bengbu Med Coll. 2019;44(02):215–218.
19. Le Mitouard M, Gaucher L, Huissoud C, et al. Decision-delivery intervals: impact of a colour code protocol for emergency caesareans. Eur J Obstet Gynecol Reprod Biol. 2020;246:29–34. doi:10.1016/j.ejogrb.2019.12.027
20. Ju XQ, Wang Y, Zhong Y, et al. Value of rapid response team 5 min emergency cesarean section in reducing decision-to-delivery interval. J Clin Med Pract. 2019;14:64–67.
21. Hu R, Li XT. Establishment and practice of emergency cesare an delivery procedure. Chin J Pract Gynecol Obstet. 2019;35(9):993–996.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
