Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Application of SHEL Model in the Management of Respiratory Tract Exposure in Fangcang Shelter Hospitals for COVID-19
Authors Wu X, Wang X, Guo H, Zhang L, Wu G
Received 29 September 2022
Accepted for publication 24 February 2023
Published 27 March 2023 Volume 2023:16 Pages 819—826
DOI https://doi.org/10.2147/JMDH.S391737
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Xiulian Wu, Xin Wang, Huimin Guo, Lili Zhang, Guangjiang Wu
Department of Nursing, Beijing Youan Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Xin Wang, Department of Nursing, Beijing Youan Hospital, Capital Medical University, No. 8, You an Men Outer Street, Fengtai District, Beijing, 100069, People’s Republic of China, Tel +86-13521101275, Email [email protected]
Objective: To explore the application effect of the (software factors, hardware factors, environmental factors, parties and other factors, SHEL) model in respiratory tract exposure protection of staff in temporary COVID-19 hospitals.
Methods: 207 Staff members working in the isolation units of Fangcang shelter hospitals between 20 May 2022 and 5 June 2022 were selected as research subjects. The SHEL model was used to protect and manage the respiratory exposure of the isolation unit staff to the novel coronavirus. The incidence of respiratory exposure among the staff in the isolation units was compared before the SHEL model’s implementation (20 May 2022– 28 May 2022) and afterwards the SHEL model’s implementation (29 May 2022– 5 June 2022).
Results: Before the implementation of the SHEL model, a total of nine cases (4.35%) from 207 workers had respiratory exposure. Occurrence location: six cases in the isolation room (one-out room, level-one protection zone) and three cases in the drop-off area for patients outside the ward. After implementation, a total of two cases (0.97%) of respiratory tract exposure occurred among the 207 staff members; both occurred in the unprotected zone (two-out room, level-two protection zone), and the difference was statistically significant before and after the implementation (P < 0.05).
Conclusion: New coronary pneumonia Fangcang shelter hospitals should use the SHEL model to manage the respiratory exposure of their isolation unit staff to reduce the respiratory exposure risk to staff in isolation units.
Keywords: SHEL model, new coronavirus, makeshift hospital, respiratory tract exposure, protection management
Introduction
Pneumonia caused by the new coronavirus (referred to as new coronary pneumonia) spreads rapidly, is highly contagious, and the population is generally susceptible.1 As at 8 October 2020, the outbreak of COVID-19 (the disease caused by SARS-CoV-2) in Wuhan, Hubei Province, China, had infected over 36.5 million individuals and claimed over one million lives worldwide. The novel virus spread rapidly across China and was transmitted to 213 other countries/territories across the globe.2
The epidemic has brought huge challenges to the health system. Close contact with patients greatly increases the occupational exposure risk of medical staff.3 Occupational exposure to respiratory pathogens4 refers to the accidental inhalation of droplets of secretions containing various respiratory pathogens, as well as direct or indirect contact with respiratory secretions, blood-contaminated skin, mucous membranes or shared objects that may be infected by pathogens. COVID-19 is spread mainly through respiratory droplets and close contact. It is transmitted by aerosols in a relatively closed environment and can also cause infection after contact with virus-contaminated items.5 Therefore, reducing the risk of respiratory exposure of staff is particularly important for the prevention and control of nosocomial infection of new coronary pneumonia.
A Fangcang shelter hospital is a medical shelter as a carrier and functions as a provider of a complete set of treatment platforms that can be deployed quickly with comprehensive integration of medical and technical support functions. It has multiple functions, such as centralised isolation, treatment and clinical testing, and it serves as the main treatment facility for patients with COVID-19.6–8 The working area is divided into clean areas (ie any area that is not contaminated by pathogenic microorganisms/viruses, such as changing rooms, duty rooms, pantries and storerooms), potentially contaminated areas (ie areas that are likely to be contaminated by pathogenic microorganisms/viruses, such as medical offices, treatment rooms, laboratories, inner corridors and discharge rooms), contaminated areas (ie areas contaminated by pathogenic microorganisms/viruses or with direct or indirect patient contact, such as wards, toilets and bathrooms; articles in a polluted area are not allowed to leave without disinfection), staff access channels and patient access channels according to the principle of ‘three areas and two channels’.9
The staff in an isolation unit are composed of medical and nursing teams from multiple hospitals and third-party property personnel. The medical and nursing teams are responsible for the admission and treatment of patients, the nucleic acid testing of patients and health monitoring. The third-party property personnel are responsible for the distribution of patients’ meals, the disposal of rubbish and the disinfection of the environment. Due to the rapid development of the epidemic, the staffing team is assembled quickly from multiple members, the management is not perfect, and the risk awareness and protection effectiveness in terms of respiratory exposure may be insufficient. As the ambient temperature rises, the isolation unit workers often work in the open air, resulting in a sharp increase in the body’s oxygen consumption, further increasing the risk of respiratory exposure.
Fangcang shelter hospitals were located in Xiaotangshan, Beijing, China. There were three isolation units in total. Before applying the new management mode, relevant personnel were trained (new management rules and practices) in the early stage; then, infection control specialists in each isolation unit guided and corrected errors through observation and monitoring.
The SHEL (software factors, hardware factors, environmental factors, parties and other factors) management model, also known as the SHEL accident analysis method, has been widely used in hospital management. This model considers that medical errors are not only related to the ability and awareness of patients and medical workers but also to the clinical environment and hospital management and are affected by other multiple factors.10 Some studies have reported that the application of the SHEL management model has a positive significance in reducing the occurrence of occupational exposure among nursing staff, and the model can improve the quality of nosocomial infection management.11–13 However, the exact extent of the impact is unclear. Therefore, we applied the SHEL model to the management of respiratory exposure among isolation unit workers to further study the specific impact of the SHEL model on respiratory tract exposure protection of staff in makeshift hospitals for COVID-19.
Research Subjects and Methods
Research Subjects
Consecutive staff members working in the Xiaotangshan Fangcai shelter hospitals from 20 May 2022 to 5 June 2022 were screened for their eligibility if they worked in the contaminated area of the isolation unit. Exclusion criteria: ① those who were moved out for centralised isolation and observation at the end of the study period; ② those who had terminated work in the isolation unit in advance due to personal reasons, such as physical conditions; ③ those who worked in clean areas and potentially contaminated areas. A total of 207 cases were included. The number of people working in each isolation unit was 69. A total of 207 people in the Xiaotangshan Fangcai shelter hospitals were divided into three units, and about 10 people were excluded from early training.
Research Methods
Establishment of Infection Control Management Team in Square-Cabin Hospitals
To improve the infection prevention and control level in square-cabin hospitals, a square-cabin hospital infection control management group was established. A square-cabin hospital is a complete set of mobile medical platforms that can be deployed rapidly, with a medical shelter as the provider and the comprehensive integration of medical treatment and medical technology support functions. Infection control teams are the medical staff responsible for the development of nosocomial infection monitoring plans, the implementation of countermeasures and measures and the supervision of related work. The members include the headquarters’ infection control team (one team leader and four team members) and the isolation unit infection control team (three infection control team leaders and 18 infection control specialists) to implement the hierarchical management of staff in the contaminated area of the isolation unit (see Figure 1).
 |
Figure 1 Diagram of sensory control level of Xiaotangshan Fangcai Hospital. |
Application of the SHEL Model
From 29 May 2022, the SHEL model was applied to manage the respiratory exposure protection of new coronavirus pneumonia for workers in contaminated areas. The management group discussed each part of the SHEL model, formulated improvement plans and organised implementation evaluations.14 (see Table 1)
 |
Table 1 Summary of SHEL Model Related to Prevention and Control of Work-Related Respiratory Exposures in Xiaotangshan Fangcai Hospital |
(1) S: ① Improvement and training of systems and procedures. The infection control management team of the headquarters formulated various infection control systems, procedures, plans and distributed them to each isolation unit to clarify the emergency plan for respiratory exposure and its reporting. Systems and processing procedures used a combination of methods for training.15 ② Online infection control regular meetings exchange and guidance: Regular online meetings were arranged every day, and the infection control commissioner reported the problems found in video surveillance and proposed rectification suggestions. The reasons for exposure in the first nine cases of personnel respiratory exposure were analysed and summarised. Targeted guidance on how to quickly exit contaminated areas and remove protective equipment when masks were wet in hot weather and there was shortness of breath, as well as guidance on evacuating to areas with low exposure risk when respiratory tract exposure was unavoidable, improved the coping ability of staff. ③ Assessment and training of basic operations. The headquarters’ induction control team conducted an online assessment on the wearing and removal of protection by the isolation unit staff on a daily basis. If the protection was found to be unqualified, it was reported immediately to the infection control specialist in the isolation unit; training and assessment were conducted again to enable the assessment to be passed. After that, the contaminated area could be entered for work, and the assessment data were uploaded to the infection control team of the headquarters for future reference. ④ Psychological support: Psychologists were regularly invited to conduct collective and individual psychological counselling16 to ensure the psychological state of the isolation unit staff remained stable.
(2) H: ① Cooling measures. The isolation unit was equipped with a single-use or reusable cooling vest, which was fitted with an antiperspirant hairband to reduce the risk of damp masks; the directions for using the cooling vest were issued by the infection control management team. ② Keeping communications open. The staff in the isolation unit were equipped with a call station and a public mobile phone. In case of an emergency, they could contact the infection control specialist in the unit promptly. ③ Dual-video monitoring. The infection control specialists of each unit and the infection control team of the headquarters formed a working mode of dual-video monitoring, with a 24-hour duty system. A WeChat group was established for feedback on infection control problems in the isolation unit to find and rectify problems in a timely manner. The infection control specialist in the unit was the first-level video surveillance personnel with responsibility for the video supervision of the process of donning and removing protective equipment by the unit’s staff and the related work of infection control in the unit. Problems were recorded for each shift, and they were summarised and fed back to the headquarters every day. The infection control team of the headquarters was the second-level video surveillance team, responsible for the video supervision of all isolation units, discovering omissions and errors promptly and issuing the “Inspection and Supervision Form” to notify the isolation unit for rectification. After the rectification of problems in each unit, the Inspection and Supervision Form was completed. The rectification part of the problem were feedback to the headquarters’ infection control team on the second day.
(3) E: ① Scientific shift arrangement and adjustment of working hours in contaminated areas. From 29 May 2022, the working hours of staff in contaminated areas in the isolation unit were reduced, the workload was reduced, the work content was reasonably arranged, and work was avoided in high-temperature periods. ② Set up restrooms in contaminated areas. Each isolation unit was set up with restrooms in contaminated areas. The interior was equipped with cooling facilities, such as air conditioners and ice buckets. Staff could enter the restrooms to rest.17 ③ Respiratory exposure risk prevention. Staff entering contaminated areas wore protective equipment and were supervised by the infection control specialist of the unit. They could enter only after passing the COVID test. When leaving the polluted area, the infection control specialist of the unit and the infection control team of the headquarters both supervised to detect the risk of respiratory exposure promptly. ④ Clear divisions. The staff of the isolation unit made clear divisions and posted walking route signs to prevent re-entry or mistaken entry into the clean area. The positions of the staff in each isolation unit were fixed, the removal or replacement of positions needed to be reported to the headquarters’ infection control team, and personnel in different department could not be crossed. The isolation unit items could not be mixed.
(4) L: The infection control specialists of each isolation unit and the infection control team of the headquarters clearly defined the exposure reporting and processing procedures. The dual-monitoring working mode supervised whether the donning and removal of protective equipment were standardised, and errors were corrected promptly through a video intercom to reduce the risk of respiratory exposure. According to the respiratory exposure reporting system, the exposed person reported to the infection control specialist of the isolation unit, who reported to the headquarters’ infection control team by phone within 10 minutes. After respiratory tract exposure was confirmed, the infection control team filled in the “Notice of Respiratory Exposure Isolation”, conducted centralised isolation for 10 days and performed daily health monitoring and nucleic acid testing. After the centralised isolation was completed, it was continued at home for seven days, and a return to work was made only after the risk of respiratory exposure had passed.
Comparison of evaluation indicators before the implementation of the SHEL model (20 May 2022–28 May 2022) and afterwards the implementation (29 May 2022–5 June 2022).
The status of respiratory exposure of staff in the isolation unit of Fangcang shelter hospitals was recorded, including the incidence, location and reporting route of respiratory exposure. The reporting methods of respiratory exposure included the following: exposed individuals were reported to the infection control specialist → the infection control specialist of the isolation unit discovered the exposure situation → the infection control team at the headquarters discovered the exposure situation.
Statistical Methods
SPSS 26.0 statistical software was used for data analysis. Enumeration data were expressed by the number of cases (n) and percentage (%), and the χ2 test was used for comparisons between groups, with P < 0.05 considered statistically significant.
Results
Composition of Research Subjects
The 207 study subjects consisted of medical staff in the isolation unit and third-party property staff. Among them were 27 doctors, accounting for 13.07%; 96 nurses, accounting for 46.38%; and 84 third-party personnel, accounting for 40.58% (see Table 2 for details).
 |
Table 2 Distribution of Staff in the Isolation Ward of Xiaotangshan Fangcai Hospital (n=207) |
The Occurrence of Respiratory Tract Exposure Before and After the Implementation of the SHEL Management Model
Before implementing the SHEL model to manage the isolation unit of Xiaotangshan Fangcai Hospital, a total of nine cases (4.35%) out of 207 staff members had respiratory tract exposure, including six cases in the isolation room (one-out room: The medical personnel in the one-out room removed protective face screens or goggles, disposable isolation clothing, shoe covers and outer gloves) and three cases in the drop-off area outside the ward. After the implementation, a total of two cases (0.97%) of respiratory tract exposure occurred among the 207 staff members, both of which occurred in the deprotection room (two-out room: The medical staff removed medical protective clothing, inner gloves and boot covers, medical protective masks and disposable hats).
Comparison of respiratory tract exposure detection methods: Three cases of exposed individuals were reported to the infection control specialist before the implementation of the SHEL model. One case of exposure was found by the infection control specialist of the isolation unit, and five cases of exposure were found by the induction control team of the headquarters. After the implementation, both cases were reported by the isolation unit infection control specialist. The incidence rate before and after the implementation was compared, and the difference was statistically significant (P < 0.05) (see Table 3 for details).
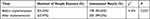 |
Table 3 Occurrence of Respiratory Tract Exposure Before and After the Implementation of SHEL Model Management (n=207) |
Discussion
The SHEL model has a good effect on the safety management of respiratory exposure prevention in isolation unit staff.
Studies have shown that the SHEL model has been applied to nursing safety management,18 emergency safety management, surgical patient prevention and control of postoperative infection, and good results have been achieved in improving nurses’ safety cognition, nursing service quality and patient satisfaction.19–21 The comparison between before and after the management of respiratory tract exposure in the isolation unit of a Fangcang shelter hospital using the SHEL model showed that the number of people with respiratory tract exposure after its implementation of the SHEL model decreased from nine cases before implementation to two cases afterwards the implementation, with the number significantly reduced. This was similar to the research results of Guo et al.22 Using the SHEL model to manage the occupational exposure of nurses to the new coronavirus, the number of occupational exposures was reduced from 11 cases before the implementation to 3 cases afterwards the implementation. In that study, the area where respiratory tract exposure occurred changed from the high-risk isolation room (one-off room) and the patient drop-off area to the low-risk deprotection room (two-off room). The risk decreased significantly, indicating that the SHEL management model is suitable for preventing respiratory exposure.
The implementation of the SHEL model helped to improve the safety awareness of various types of staff in the isolation units of Fangcang shelter hospitals for respiratory exposure.22 Since isolation unit personnel are composed of medical staff and third-party property personnel, although they have undergone preliminary training and assessment, some staff still have a lack of awareness of the risk of respiratory exposure to COVID-19. After the implementation of the SHEL model, through online teaching and lectures, the reasons for exposure in the nine cases of respiratory exposure were analysed, and the division of the isolation unit area was explained. The regional division of the risk level of respiratory exposure, the concept of clean areas in the isolation unit and the division of the semi-contaminated area of the contaminated area effectively reduced the occurrence of re-entry, retrogradation (walk against the directions), cross-regional contamination and other phenomena. Through the statistics on the reporting methods of respiratory tract exposure before and after the application of the SHEL model, three cases were reported by individuals before implementation, one case was discovered and reported by the infection control commissioner, and five cases were reported to the infection control commissioner of the isolation unit by the induction control team of the headquarters. Two cases were exposed after the implementation. All were identified and reported by the isolation unit infection control specialist, indicating that the application of the SHEL model improved the safety awareness of the staff and reduced the occurrence of respiratory exposure, with the application of software and hardware measures achieving good results.
The application of the SHEL model systematically improved the infection control management level in Fangcang shelter hospitals. The incidence of respiratory tract exposure before and after the implementation of the SHEL model decreased from 4.35% to 0.97%; the difference was statistically significant (P < 0.05), and there was an obvious reduction in the risk of the exposure location. A study by Li Hongmei came to a similar conclusion: After applying the SHEL model during the COVID-19 epidemic, the occupational exposure rate of front-line nurses in hospitals decreased compared with before its implementation.23 Furthermore, Peng et al also confirmed that the application of the SHEL management model in the department of radiology during the COVID-19 epidemic improved individual coping ability and department team cohesion, improved the comprehensive quality of department nosocomial infection management and contributed to the prevention and control of COVID-19 in the department of radiology.24
During the implementation of the SHEL model, through the training system process, the analysis of respiratory exposure cases, daily online regular meetings and psychological support improved the management level of the software element. Hardware facilities were improved through the application of various cooling measures, communication facilities and dual monitoring equipment. The clinical environmental element was improved by clarifying divisions, placing process signs on the walls, scientifically arranging shifts and setting up rest areas. Clarifying the responsibilities of the infection management team and infection control specialists and providing training and guidance for each staff member improved the infection control awareness and exposure risk handling capabilities of staffs.
Therefore, the application of the SHEL management model comprehensively improved infection management and the level of control in Fangcang shelter hospitals.
The limitations of this study were that the study period was short and the sample size was small; therefore, further research and exploration will be carried out by extending the study time and expanding the sample size.
Summary
To sum up, the application of the SHEL model comprehensively improved the infection control management level in Fangcang shelter hospitals, helped reduce the risk of respiratory exposure by various staff and was an important guarantee for Fangcang shelter hospitals in completing treatment tasks.
Data Sharing Statement
The data underlying this article will be shared at reasonable request to the corresponding author.
Ethics Approval and Consent to Participate
This study has been approved by the Ethics Committee of Beijing You’an Hospital Affiliated to Capital Medical University. Written informed consent was obtained from all participants.
Funding
This study did not receive any funding in any form.
Disclosure
All authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Song P, Zhao L, Li X, et al. Interpretation of the Traditional Chinese Medicine portion of the diagnosis and treatment protocol for Corona virus disease 2019 (Trial Version 7). J Tradit Chin Med. 2020;40(3):497–508.
2. Sharma A, Farouk IA, Lal SK. COVID-19: a Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses. 2021;13(2):202. doi:10.3390/v13020202
3. Cao Q, Cui FH, Han Y, Su JZ. Analysis of risk factors for occupational exposure to novel coronavirus in 27 medical workers. PLA J Prev Med. 2020;38(8):100–101.
4. Xiuni G. Terms and definitions of occupational exposure to respiratory pathogens in emergency department. Chin J Nurs. 2017;7(52):20–24.
5. National Health Commission of China. Diagnosis and treatment plan for novel coronavirus pneumonia (trial ninth edition). Int J Epidemiol Infect Dis. 2022;49(02):73–80.
6. Martin-Gill C, Doyle TJ, Yealy DM. In-Flight Medical Emergencies: a Review. JAMA. 2018;320(24):2580–2590. doi:10.1001/jama.2018.19842
7. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi:10.1016/S0140-6736(20)30744-3
8. Shang L, Xu J, Cao B. Fangcang shelter hospitals in COVID-19 pandemic: the practice and its significance. Clin Microbiol Infect. 2020;26(8):976–978. doi:10.1016/j.cmi.2020.04.038
9. Fang D, Pan S, Li Z, et al. Large-scale public venues as medical emergency sites in disasters: lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob Health. 2020;5(6):e002815. doi:10.1136/bmjgh-2020-002815
10. Glavin RJ. Human performance limitations (communication, stress, prospective memory and fatigue). Best Pract Res Clin Anaesthesiol. 2011;25(2):193–206. doi:10.1016/j.bpa.2011.01.004
11. Li L, Min Y, Bai DM, Zhou B, Shan SJ. Application of hospital infection management based on SHEL model in digestive endoscopy center. Hosp Infect Manag. 2022;2(15):286–290.
12. Lu ZH, Wang Y, Guo XB, Yang XK. Research progress on cause analysis models of adverse nursing events. J Nurs. 2019;34(21):107–110.
13. Mo HP, Wang X, Zhou Y, et al. Discussion on occupational exposure protection measures of medical staff under the background of mechanical ventilation in patients with respiratory infectious diseases. Chin Nurs Manag. 2021;9(21):1387–1391.
14. Tang T, Xu SS, Liu Q. Application of check list management based on SHEL model in the prevention and management of adverse events of new coronavirus nucleic acid specimen collection. J Nurs. 2021;28(14):55–59.
15. Wang YW, Huang X, Zeng LM, et al. Occupational exposure monitoring of medical staff related to the treatment of new coronary pneumonia. Chin J Infect Control. 2020;12(19):1082–1087.
16. Lu J, Zhao M, Wu Q, et al. Mental health needs of the COVID-19 patients and staff in the Fangcang shelter hospital: a qualitative research in Wuhan, China. Glob Ment Health. 2021;9(8):e33. doi:10.1017/gmh.2021.23
17. Shen B, Chen L, Zhang L, et al. Wuchang Fangcang Shelter Hospital: practices, Experiences, and Lessons Learned in Controlling COVID-19. SN Compr Clin Med. 2020;2(8):1029–1034. doi:10.1007/s42399-020-00382-1
18. Shi XX, Chen HJ, Zhou X, Hu HL, Gao HM. Application progress of SHEL model in nursing safety management. Chin Nurs Manag. 2020;6(20):897–900.
19. Yu X, Li C, Gao X, Liu F, Lin P. Influence of the medication environment on the unsafe medication behaviour of nurses: a path analysis. J Clin Nurs. 2018;27(15–16):29993–30000. doi:10.1111/jocn.14485
20. Marcilly R, Leroy N, Luyckx M, Pelayo S, Riccioli C, Beuscart-Zéphir MC. Medication Related Computerized Decision Support System (CDSS): make it a Clinicians’Partner! Stud Health Technol Inform. 2011;1(166):84–94.
21. De Korne DF, Van Wijngaarden JD, Van Dyck C, Hiddema UF, Klazinga NS. Evaluation of aviation-based safety team training in a hospital in The Netherlands. J Health Organ Manag. 2014;28(6):731–753. doi:10.1108/JHOM-01-2013-0008
22. Guo XL, Lu CJ, Wang Y, et al. Application of SHEL model in nurses’ occupational exposure protection during the novel coronavirus pneumonia epidemic. Nurs Res. 2020;34(6):943–944.
23. Li HM. Observation on the application of the SHEL model in the occupational exposure protection management of front-line nurses in the fever clinic of our hospital during the epidemic of COVID-19. Med Theory Pract. 2021;34(15):2737–2738.
24. Peng Y, Deng JL, Zhou J, Zhang XF, Jin XR. Application of SHEL model management in the prevention and control of radiology department during the novel coronavirus pneumonia epidemic. Mod Med Health. 2021;37(08):1423–1427.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
