Back to Journals » Journal of Multidisciplinary Healthcare » Volume 11
Anxiety and depression predicted quality of life among patients with heart failure
Authors AbuRuz ME
Received 7 April 2018
Accepted for publication 15 May 2018
Published 30 July 2018 Volume 2018:11 Pages 367—373
DOI https://doi.org/10.2147/JMDH.S170327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mohannad Eid AbuRuz
Clinical Nursing Department, College of Nursing, Applied Science Private University, Amman, Jordan
Purpose: Anxiety and depression are prevalent among patients with heart failure. However, their effect on the quality of life (QoL) is not well investigated in developing countries. Therefore, the purpose of this study was to test the effect of anxiety and depression on QoL among Jordanian patients with heart failure.
Patients and methods: Two hundred patients with a confirmed diagnosis of heart failure from 1 governmental and 1 private hospital in Amman, Jordan, were recruited between March and August, 2017. A descriptive, cross-sectional design was used. Anxiety and depression were measured using the Arabic version of the Hospital Anxiety and Depression Scale. QoL was measured using the Arabic version of the Short Form-36.
Results: Patients reported poor QoL in both physical component summary (M ± SD; 35.8±9.6) and mental component summary (M ± SD; 41.5±11.3). Prevalence rates for anxiety and depression were 62% and 65%, respectively. In stepwise regression analysis, anxiety and depression were independent predictors for poor QoL in both summaries, p<0.001.
Conclusion: Patients with heart failure have poor QoL and high anxiety and high depression prevalence rates. Inclusion of routine assessment and management of anxiety and depression in heart failure protocols is highly recommended.
Keywords: anxiety, depression, heart failure, quality of life, Jordan
Introduction
For many decades, cardiovascular disease (CVD) has been the number one killer worldwide.1 Globally, 80% of CVD deaths take place in low- and middle-income countries. Heart failure (HF) is one of the most common CVDs, since 26 million adults worldwide are living with HF.2 Projections show that the prevalence of HF is increasing. For instance, it is estimated that the prevalence will increase in US by 46% from 2012 to 2030, resulting in >8 million people ≥18 years of age suffering from HF.3
In developing countries, HF is a critical health problem similar to the developed countries.4 In Jordan, a developing Arabic country, the extrapolated prevalence of HF is 99,021 cases. Based on an estimated small population of 5.61 million, the incidence is 8,251 cases annually.5 On the other hand, highly populated Arabic countries (ie, Egypt, Sudan, and Saudi Arabia) have extrapolated prevalences of 1,343,248, 690,849, and 455,222 cases, respectively.5
Acute exacerbation of HF is the most common reason for HF admissions to the hospitals.6,7 HF affects cardiovascular, neurological, and endocrine functions, resulting in dangerous outcomes. Dyspnea, pitting edema, fluid retention, pulmonary edema, fatigue, sleep disturbance, and loss of energy are common signs and symptoms in patients with HF.8–10 These symptoms influence patients’ ability to perform activities of daily living, socialization, functional status, and their quality of life (QoL).8–11 Therefore, different studies have been conducted to test the effect of HF on QoL. Mostly, authors have concluded that patients with HF have poor QoL even with conventional treatment.2,9,11–13
Many sociodemographic, physiological, and psychological factors have been shown to affect the QoL in patients with HF. These factors include but are not limited to age, gender, marital status, social support, education, and culture.4,9,11 Left ventricular ejection fraction (LVEF), New York Heart Association classification (NYHA class), time since HF diagnosis, other comorbidities, insomnia, anxiety, and depression were also considered as predictors of QoL.14,15
Anxiety and depression are common among patients with HF.7,8,12 The prevalence rates of anxiety and depression in patients with HF are 4–5 times more than that in the general population.7,8,12 The prevalence rate of anxiety in patients with HF ranged between 11% and 70%,7,8,12,13,16,17 and the prevalence rate for depression ranged between 9% and 96.1%.2,7,8,12,13,17 The difference in the prevalence rates among studies is due to different assessment methods, the definition and categorization of anxiety and depression, and the severity of the cases included in each study.13,18 Moreover, some signs and symptoms of HF (ie, insomnia, fatigue, and loss of appetite) are shared with depression and anxiety.13,19
Poor QoL is one of the most important characteristics of HF.20,21 Most studies showed that anxiety and depression were associated with poor QoL in patients with HF.2,6,7,13,17,22–25 However, other studies did not show this relationship.13,26–28 Some researchers concluded that these factors have equal or even more negative consequences than traditional risk factors such as diabetes mellitus (DM), hypertension (HTN), smoking, and hypercholestermia.29,30 For these reasons, HF management guidelines recommended routine assessment of depression and anxiety in patients with HF.31,32 However, these recommendations are not transferred into practice.20 For example, in a study6 checking the effect of anxiety and depression on QoL for patients with HF and hypertension, the authors found that anxiety and depression were rarely detected or correctly treated by physicians. Moreover, only 2 patients (0.01%) of the sample had previous contact with psychiatric clinics.6
Most of the previous studies assessing the effect of HF on QoL and the effect of anxiety and depression on QoL in patients with HF were performed in developed countries. In developing countries, there are some studies testing the effect of HF on QoL.9,11 However, studies assessing the effect of anxiety and depression on QoL in patients with HF are lacking. Therefore, the purpose of this study was to analyze the effect of anxiety and depression on QoL for patients diagnosed with HF in Jordan.
Materials and methods
Research hypotheses
1) Anxiety scores will be an independent predictor of QoL (physical component summary [PCS] and mental component summary [MCS]), in patients with HF after controlling for sociodemographic and clinical variables, 2) Depression scores will be an independent predictor of QoL (PCS and MCS) in patients with HF after controlling for sociodemographic and clinical variables.
Design, sample, and setting
A descriptive, cross-sectional correlational design was used. A convenience sampling technique was used to recruit patients between March and August, 2017. Patients who met the following inclusion criteria were recruited from 1 governmental and 1 private hospital in Amman, Jordan: 1) a confirmed diagnosis of HF by a cardiologist, 2) 18 years or older, 3) able to read and write Arabic, 4) signed an informed consent, 5) not on antianxiety or antidepressant medications, and 6) free from any chronic disease that might affect QoL (ie, cancer, chronic kidney disease, and liver failure). Sample size was calculated using an online a priori Sample Size Calculator for Multiple Regression.33 The assumptions were as follows: medium effect size of 0.15, a power of 0.9, 10 predictors, and an α of 0.01. Based on these assumptions, the necessary sample size to achieve the desired power was 192 participants. Two hundred and seventy five participants were screened according to the inclusion and exclusion criteria. Among them, 25 did not meet the criteria, 30 did not agree to participate, and 20 had missing data. All of them (75 participants) were excluded from the sample. Therefore, the final sample consisted of 200 participants; 100 from each hospital.
Ethical considerations
The principal investigator presented the study to the Institutional Review Board (IRB) committee at the Applied Science Private University, Amman, Jordan. The Dean of the college then issued the IRB approval letter based on the committee recommendation; (IRB#: Faculty 021). Then, the principal investigator submitted this letter to the medical directors of the selected hospitals where data collection took place. Prior to data collection, medical directors accepted the IRB approval letter from the university, and the study was approved by the hospital boards.
Procedure
Patients who met the inclusion criteria during their visit to the outpatient clinic were contacted by research assistants. Purpose, risks, and benefits of the study were informed to participants verbally and in written form. Patients who agreed to participate after this explanation were asked to sign an informed consent. Patients were asked to fill the Hospital Anxiety and Depression Scale (HADS), Short Form 36, and their sociodemographic characteristics in a quiet place at the hospital. Research assistants obtained patients’ LVEF, NYHA class, and information about other comorbidities from patients’ medical records.
Measurement of variables
QoL
This was measured using the Arabic version of the Short Form 36. This tool consisted of 36 multiple response questions with 8 domains, namely, physical functioning (10 items), role physical functioning (4 items), role emotional functioning (3 items), vitality (4 items), mental health (5 items), social functioning (2 items), body pain (2 items), and general health (5 items).34 Scores for each domain ranged from 0 to 100. Higher scores indicated better QoL in each domain. Two major summaries can be calculated: PCS, which is composed of physical functioning, role physical functioning, body pain, and general health, and MCS, which is composed of role emotional functioning, vitality, mental health, and social functioning. In this study, these 2 summaries will be reported as reported by recent studies.9,11 Patients were considered to have poor QoL in these subscales if their scores were below 47.9,11 The psychometric properties of the Arabic version showed that the minimum Cronbach’s α for general health was 0.71, and the highest was for physical functioning, at 0.94.9,11,35
Anxiety and depression
This was measured by the Arabic version of the HADS. This instrument assesses anxiety and depression without investigating somatic symptoms. It is composed of 14 items, 7 for anxiety and 7 for depression. The participants rated their levels on a 0–3 scoring system, with a range of 0–21 for each subscale. Higher scores indicate higher symptoms frequency and severity. Scores were classified as follows: 0–7, normal; 8–10, mild; 11–14, moderate; and 15–21, severe anxiety/depression.36 Previous studies36–40 showed the following coefficients regarding the psychometric properties of the Arabic version of the HADS: the Cronbach’s α for anxiety and depression subscales were 0.78 and 0.87, respectively.36–40
Sociodemographic and clinical characteristic
These data were collected either by administering a questionnaire or by medical records review. The following sociodemographic and clinical data were collected: age, gender, level of education, marital status, job status, NYHA class, LVEF, history of HTN, DM, and time since HF diagnosis. For clarification, NYHA class is described as follows: class I, no limitation of physical activity; class II, slight limitation of physical activity; class III, marked limitation of physical activity; and class IV, unable to perform physical activity without symptoms of cardiac insufficiency.6
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences for Windows 21.0 (IBM Corporation, Armonk, NY, USA). Statistical significance was determined at p-value of <0.05. Participants’ demographic and clinical characteristics were described by (mean ± standard deviation or frequency and percentages). To identify if anxiety and depression scores were independent predictors of QoL (PCS and MCS), a series of bivariate correlations were conducted to test for associations between the 2 summary subscales and demographic variables (ie, age, gender, marital status, job status, and anxiety/depression scores) and clinical variables (LVEF, NYHA class, time since HF diagnosis, history of HTN, and DM). Pearson’s r was used for interval measures, and Spearman ρ was used for ordinal measures. Next, stepwise regression was used to check the effect on the QoL. Two regression models were carried out, 1 for PCS and 1 for MCS. Each model consisted of 3 blocks. The first block contained age, gender, marital status, and job status, while the second block contained LVEF, NYHA class, time since HF diagnosis, history of HTN, and DM. The last block contained anxiety and depression scores.
Results
The sample of this study consisted of 123 men and 77 women with a mean age of 53.4±14.5 years. Sociodemographic and clinical characteristics of the sample are presented in Table 1. Approximately three-quarters of the sample were married; more than half of the sample was working. More than a third of the sample (35%) were educated to a Baccalaureate level (BS). Based on the HADS criteria, the sample was moderately anxious and depressed. The prevalence rates of anxiety and depression were 62% and 65%, respectively.
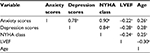
Table 2 shows the correlations between (PCS, MCS), demographic, and clinical variables. All variables had a negative correlation with PCS and MCS except for LVEF and job status. This meant that patients with higher LVEF and patients who were working had better QoL. Table 3 shows the results of regression analyses for predictors of PCS and MCS. Age, LVEF, NYHA class, and anxiety and depression scores were independent predictors for both PCS and MCS. In addition, job status was an independent predictor for MCS. Job status and LVEF were the only positive predictors in the 2 models. The PCS model explained 49% of the variance and MCS model explained 44% of the variance. Table 4 shows the correlation between anxiety scores, depression scores, NYHA class, LVEF, and age. Anxiety and depression increased with age, NYHA class, and low LVEF. NYHA class increased with age, and lower LVEF.
Discussion
The purpose of this study was to assess the effect of anxiety and depression on QoL for patients with HF in a developing country. The results showed that patients with HF have poor QoL in both PCS and MCS. In addition, the results showed that anxiety and depression are prevalent among patients with HF. Anxiety scores, depression scores, age, LVEF, and NYHA class were predictors for PCS. Anxiety scores, depression scores, age, LVEF, NYHA class, and job status were predictors for MCS. The results of this study are consistent with previous studies in regard to poor QoL in patients with HF.8,9,11 In addition, it is consistent with studies showing that anxiety and depression are associated with poor QoL in patients with HF.2,6,7,13,17,22–25
Anxiety and depression affect QoL in patients with HF through different potential mechanisms. Physiologically, anxiety and depression stimulates the sympathetic nervous system, reduces heart rate variability, impairs platelet functioning, motivates inflammatory process, and leads to hypercholestermia.6,41–45 Behaviorally, anxious and depressed patients will neglect their self-care and dietary regimen and fail to follow the prescribed medications.30,46,47 Moreover, there is a reciprocal relationship between negative emotions (anxiety and depression) and QoL (PCS and MCS). Deterioration of health status in patients with HF; acute exacerbations, made them realize the risk of death which led to anxiety and depression.17,48
Previous studies which did not show a significant relation between anxiety and depression and QoL have several limitations including the fact that 1) anxiety and depression measures included confounding somatic symptoms such as fatigue and shortness of breath23,24,49,50, 2) anxiety and depression symptoms were mixed together while measuring anxiety,17 3) PCS in previous studies concentrated on general activities of daily living and did not evaluate items precisely for HF,17 4) samples included a large number of patients with no signs and symptoms of HF or a large number of patients with mild HF categories. For example, 85% of the patients included in a study on anxiety and HF were NYHA class I and II.13
Age was an independent predictor for poor QoL in both PCS and MCS. Previous studies argue that the prevalence of HF increases with age.2,3 The results of current study showed that anxiety scores, depression scores, NYHA class increases with age, and LVEF decreases with age. All these factors lead to a decline in physical and mental capabilities in patients with HF, thus contributing to poor QoL.2,26,51–53 The mean age of the participants of this study was approximately the same as in previous studies on QoL done in Jordan and Saudi Arabia.9,11 In this study and the 2 previous studies,9,11 older age was a contributing factor to poor QoL in patients with HF.
Another predictor for poor QoL in this study was the severity of the disease. The severity of HF in this study was measured by high NYHA class and lower levels of LVEF. This result is in line with previous studies about LVEF9,11 and NYHA class.2,9,11,54 In this study, patients with high NYHA class and lower levels of LVEF had higher levels of anxiety and depression, which further explain the results of poor QoL. Moreover, patients with severe HF usually have higher rates of admission to the hospitals. Despite the fact that we did not measure this variable in the present study; previous studies demonstrated that patients with severe HF have been hospitalized more than patients with mild and moderate HF. This could have made them more anxious and depressed and thus reduced their QoL.2
Job status was one of the predictors for QoL in this study. Previous studies showed that unemployed patients with HF have higher levels of anxiety and depression than employed patients.2,54 This might explain why we have a positive relation between job status and QoL. The current study has consistent results with the previous studies in regard to this issue. Approximately half of the patients in this study were unemployed or retired. This group has higher levels of anxiety and depression compared to the employed group, which explains the prediction of poor QoL. Moreover, previous studies showed that HF patients with high annual salary reported lower levels of depression and anxiety and higher levels of security.2,54 Unemployed/retired patients will have lower levels of income and therefore lower level of security and less socialization, which have an important effect on their QoL.2,54
Previous studies showed that social support and socialization have a crucial role in improving QoL in patients with HF.9,11,17,55 Most of the times, depression and anxiety usually occur due to poor social support and isolation rather than medical causes.13,19 HF patients with high levels of anxiety and depression may develop somatic pain and other disabilities.6 Therefore, they might view suicide as a realistic solution for their situation.6 Based on all these results, it is highly recommended that patients with HF be screened and treated for anxiety and depression.
Conclusion
This study assessed the effect of anxiety and depression on QoL in patients with HF in a developing country. The results of this study give further support to previous conclusions that patients with HF have poor QoL. In addition, it was concluded that anxiety and depression were predictors of poor QoL in patients with HF. Inclusion of routine assessment and management of anxiety and depression in HF protocols is highly recommended.
Study limitations
The major limitations of this study were the use of the cross-sectional design and the convenience sampling technique. Patients were recruited only from 1 major city (Amman). Moreover, anxiety and depression was measured at 1 time point, and this could possibly be a transient episode.
Disclosure
The author reports no conflicts of interest in this work.
References
Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. | ||
Aggelopoulou Z, Fotos NV, Chatziefstratiou AA, Giakoumidakis K, Elefsiniotis I, Brokalaki H. The level of anxiety, depression and quality of life among patients with heart failure in Greece. Appl Nurs Res. 2017;34:52–56. | ||
Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. | ||
Pelegrino VM, Dantas RAS, Clark AM. Health-related quality of life determinants in outpatients with heart failure. Rev Latino-Am Enfermagem. 2011;19(3):451–457. | ||
Right Diagnosis, Health Grades Inc. Statistics by Country for Congestive Heart Failure. 2017. Available from: http://www.rightdiagnosis.com/c/congestive_heart_failure/stats-country.htm. Accessed October 28, 2017. | ||
Serafini G, Pompili M, Innamorati M, et al. The impact of anxiety, depression, and suicidality on quality of life and functional status of patients with congestive heart failure and hypertension: an observational cross-sectional study. Prim Care Companion J Clin Psychiatry. 2010;12(6):pii: PCC.09m00916. | ||
Uchmanowicz I, Gobbens RJ. The relationship between frailty, anxiety and depression, and health-related quality of life in elderly patients with heart failure. Clin Interv Aging. 2015;10:1595–1600. | ||
Eisele M, Blozik E, Stork S, Trader JM, Herrmann-Lingen C, Scherer M. Recognition of depression and anxiety and their association with quality of life, hospitalization and mortality in primary care patients with heart failure – study protocol of a longitudinal observation study. BMC Fam Pract. 2013;14:180. | ||
AbuRuz ME, Alaloul F, Saifan A, Masa’deh R, Abusalem S. Quality of life for Saudi patients with heart failure: a cross-sectional correlational study. Glob J Health Sci. 2015;8(3):49–58. | ||
Hunt SA; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2005;46(6):e1–e82. | ||
Alaloul F, AbuRuz ME, Moser DK, Hall LA, Al-Sadi A. Factors associated with quality of life in Arab patients with heart failure. Scand J Caring Sci. 2017;31(1):104–111. | ||
Isaksen K, Munk PS, Giske R, Larsen AI. Effects of aerobic interval training on measures of anxiety, depression and quality of life in patients with ischaemic heart failure and an implantable cardioverter defibrillator: A prospective non-randomized trial. J Rehabil Med. 2016;48(3):300–306. | ||
Tsuchihashi-Makaya M, Kato N, Chishaki A, Takeshita A, Tsutsui H. Anxiety and poor social support are independently associated with adverse outcomes in patients with mild heart failure. Circ J. 2009;73(2):280–287. | ||
Chung ML, Moser DK, Lennie TA, Frazier SK. Perceived social support predicted quality of life in patients with heart failure, but the effect is mediated by depressive symptoms. Qual Life Res. 2012;22(7):1555–1563. | ||
Son YJ, Song Y, Nam S, Shin WY, Lee SJ, Jin DK. Factors associated with health-related quality of life in elderly Korean patients with heart failure. J Cardiovasc Nurs. 2012;27(6):528–538. | ||
Olafiranye O, Jean-Louis G, Zizi F, Nunes J, Vincent M. Anxiety and cardiovascular risk: review of epidemiological and clinical evidence. Mind Brain. 2011;2(1):32–37. | ||
Shen BJ, Eisenberg SA, Maeda U, et al. Depression and anxiety predict decline in physical health functioning in patients with heart failure. Ann Behav Med. 2011;41(3):373–382. | ||
Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail. 2005;11(6):455–463. | ||
MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Arch Intern Med. 2002;162(5):509–516. | ||
Moser DK, Dracup K, Evangelista LS, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung. 2010;39(5):378–385. | ||
Calvert MJ, Freemantle N, Cleland JG. The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. Eur J Heart Fail. 2005;7(2):243–251. | ||
Rumsfeld JS, Havranek E, Masoudi FA, et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42(10):1811–1817. | ||
Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007;13(8):643–648. | ||
Faller H, Stork S, Schuler M, et al. Depression and disease severity as predictors of health-related quality of life in patients with chronic heart failure – a structural equation modeling approach. J Card Fail. 2009;15(4):286–292.e2. | ||
Chung ML, Moser DK, Lennie TA, Rayens MK. The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: testing dyadic dynamics using Actor-Partner Interdependence Model. J Psychosom Res. 2009;67(1):29–35. | ||
Cully JA, Phillips LL, Kunik ME, Stanley MA, Deswal A. Predicting quality of life in veterans with heart failure: the role of disease severity, depression, and comorbid anxiety. Behav Med. 2010;36(2):70–76. | ||
Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. J Psychosom Res. 2001;51(3):521–527. | ||
Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110(22):3452–3456. | ||
Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111(3):271–277. | ||
Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–651. | ||
Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119(14):e391–e479. | ||
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–1852. | ||
Free Statistics Calculators. A-priori Sample Size Calculator for Multiple Regression. Available from: http://www.danielsoper.com/statcalc/calculator.aspx?id=1. Accessed October 13, 2017. | ||
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. | ||
Coons SJ, Alabdulmohsin SA, Draugalis JR, Hays RD. Reliability of an Arabic version of the RAND-36 Health Survey and its equivalence to the US-English version. Med Care. 1998;36(3):428–432. | ||
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. | ||
el-Rufaie OE, Absood GH. Retesting the validity of the Arabic version of the Hospital Anxiety and Depression (HAD) scale in primary health care. Soc Psychiatry Psychiatr Epidemiol. 1995;30(1):26–31. | ||
el-Rufaie OE, Albar AA, Al-Dabal BK. Identifying anxiety and depressive disorders among primary care patients: a pilot study. Acta Psychiatr Scand. 1988;77(3):280–282. | ||
el-Rufaie OE, Absood G. Validity study of the Hospital Anxiety and Depression Scale among a group of Saudi patients. Br J Psychiatry. 1987;151:687–688. | ||
Malasi TH, Mirza IA, el-Islam MF. Validation of the Hospital Anxiety and Depression Scale in Arab patients. Acta Psychiatr Scand. 1991;84(4):323–326. | ||
Serebruany VL, Glassman AH, Malinin AI, et al. Enhanced platelet/endothelial activation in depressed patients with acute coronary syndromes: evidence from recent clinical trials. Blood Coagul Fibrinolysis. 2003;14(6):563–567. | ||
Otte C, Marmar CR, Pipkin SS, Moos R, Browner WS, Whooley MA. Depression and 24-hour urinary cortisol in medical outpatients with coronary heart disease: The Heart and Soul Study. Biol Psychiatry. 2004;56(4):241–247. | ||
Otte C, Neylan TC, Pipkin SS, Browner WS, Whooley MA. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: findings from the Heart and Soul Study. Am J Psychiatry. 2005;162(11):2139–2145. | ||
Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379–2388. | ||
Shang YX, Ding WQ, Qiu HY, Zhu FP, Yan SZ, Wang XL. Association of depression with inflammation in hospitalized patients of myocardial infarction. Pak J Med Sci. 2014;30(4):692–697. | ||
Johnson TJ, Basu S, Pisani BA, et al. Depression predicts repeated heart failure hospitalizations. J Card Fail. 2012;18(3):246–252. | ||
Cholowski K, Cantwell R. Predictors of medication compliance among older heart failure patients. Int J Older People Nurs. 2007;2(4):250–262. | ||
Berry C, McMurray J. A review of quality-of-life evaluations in patients with congestive heart failure. Pharmacoeconomics. 1999;16(3):247–271. | ||
Gottlieb SS, Khatta M, Friedmann E, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43(9):1542–1549. | ||
Muller-Tasch T, Peters-Klimm F, Schellberg D, et al. Depression is a major determinant of quality of life in patients with chronic systolic heart failure in general practice. J Card Fail. 2007;13(10):818–824. | ||
Heo S, Moser DK, Riegel B, Hall LA, Christman N. Testing a published model of health-related quality of life in heart failure. J Card Fail. 2005;11(5):372–379. | ||
Gottlieb SS, Kop WJ, Ellis SJ, et al. Relation of depression to severity of illness in heart failure (from heart failure and a controlled trial investigating outcomes of exercise training [HF-ACTION]). Am J Cardiol. 2009;103(9):1285–1289. | ||
Piazza JR, Charles ST, Almeida DM. Living with chronic health conditions: age differences in affective well-being. J Gerontol B Psychol Sci Soc Sci. 2007;62(6):P313–P321. | ||
Chu SH, Lee WH, Yoo JS, et al. Factors affecting quality of life in Korean patients with chronic heart failure. Jpn J Nurs Sci. 2014;11(1):54–64. | ||
Bennett SJ, Perkins SM, Lane KA, Deer M, Brater DC, Murray MD. Social support and health-related quality of life in chronic heart failure patients. Qual Life Res. 2001;10(8):671–682. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.