Back to Journals » Vascular Health and Risk Management » Volume 14
Anxiety and depression in patients with pulmonary hypertension: impact and management challenges
Authors Bussotti M, Sommaruga M
Received 21 April 2018
Accepted for publication 15 August 2018
Published 8 November 2018 Volume 2018:14 Pages 349—360
DOI https://doi.org/10.2147/VHRM.S147173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Maurizio Bussotti,1 Marinella Sommaruga2
1Cardiorespiratory Rehabilitation Unit, Istituti Clinici Scientifici Maugeri, IRCCS, Scientific Institute of Milan, Milan, Italy; 2Psychology Unit, Istituti Clinici Scientifici Maugeri, IRCCS, Scientific Institute of Milan, Milan, Italy
Background: Anxiety and depression are frequent disorders in patients with pulmonary arterial hypertension (PAH), but despite this only less than one-fourth of them is treated. Our aim was to review the studies regarding the prevalence and the impact of anxiety and depression and to propose management challenges.
Methods: A literature review regarding 1) anxiety and depression studies in PAH patients and caregivers, 2) psychological interventions, 3) slow breathing approach, and 4) pharmacological approach was performed, based on evidence of effectiveness through a search of the most well-known databases (Cochrane Library, Medline, PsychINFO [2004–2018]).
Results: The prevalence of mental disorders in PAH patients lies between 7.5% and 53% for depression and 19% and 51% for anxiety and panic disorders. The latest guidelines of the European Society of Cardiology recommend a psychological support with a class of recommendation I and a level of evidence c. The analysis of psychological intervention shows that at present there is no evidence of specific psychological interventions in these patients. However, treatment approaches based on other chronic illnesses are suggested, especially based on relaxation training, slow breathing, and cognitive behavioral therapy. Finally, data concerning the use of antidepressant drugs are conflicting.
Conclusion: Firstly, our data demonstrate a common underestimation of mental disorders by health professionals and secondly, the need of implementing appropriate methods of screening for mental disorders in PAH patients. However, the paucity of large observational studies in this area requires the attention of researchers. The evidence about optimal approaches for managing anxiety and depression in PAH also remains unclear and largely speculative. The challenge is the introduction of routine psychological intervention, as suggested by the European Society of Cardiology and already applied in other chronic disease.
Keywords: pulmonary arterial hypertension, anxiety, depression, psychological distress, rehabilitation, psychological intervention
Introduction
When talking about pulmonary hypertension (PH), we actually refer to a wide spectrum of cardiorespiratory pathologies, all characterized by an increased pulmonary artery mean pressure over 25 mmHg.1
The classification reported by the international guidelines divides the various forms into five groups.
The most frequent cases of pulmonary PH are secondary to the left heart’s diseases or to pulmonary pathologies,2 but currently, Group I, the so-called pulmonary arterial hypertension (PAH), is attracting the majority of researchers’ attention. PAH is a rare disease, with a prevalence and incidence of 15 cases per million of the adult population and 5–10 cases per million per year, respectively.
This group includes those forms characterized by a primary involvement of the pulmonary circulation. Many of these cases are based on genetic transmission. Some forms are associated with congenital heart disease, while some others are secondary to connective diseases or HIV infection-related or drug-induced; the remaining, those without any genetic substrate or known triggering factor, are defined as idiopathic.2
The aspects differentiating this group from the other four groups are the occurrence at an earlier age, a greater prevalence in women (although it must be recognized that female predominance concerns the younger age groups), a worse prognosis, and the lack of response to conventional therapies for heart and respiratory failure.3
The first registry created in 1981 (the US National Institutes of Health registry) reported a mean age of 36 years among patients with idiopathic PAH. On the contrary, the most recent registries have reported the first diagnosis between 50 and 65 years.4
Numerous substances have been identified as possible or certain triggers for the development of PAH, based on the strength of the evidence about their link and possible causal effect with PAH itself.3
Among these, the selective serotonine-reuptake inhibitors (SSRIs) with anorexic action had a prominent role, before their withdrawal from marketing.
Numerous registries have studied PAH prognosis. In US Registry (dating back to 1981–1988 and concluded before the marketing of PAH-specific therapies), the median survival after diagnosis of IPAH was 2.8 years, with survival rates of 68%, 48%, and 34% at 1, 3, and 5 years, respectively.4
Over a 4-year period (between 2006 and 2009), the REVEAL Registry enrolled consecutively 2,039 PAH patients.5 Its analysis shows that in newly diagnosed patients, survival rates at 1, 3 and 5 years were 86.3%, 69.3%, and 61.2%, respectively.6
Indeed, despite the progress in PAH-specific therapies and patients support strategies, the prognosis does not remain so positive.7,8
The characteristic pathophysiological features of this disease are an increased pulmonary ventilation/perfusion mismatching that may cause hypoxemia and low cardiac output, which explain the reduced tolerance to physical exertion, the dyspnea, and the easy fatigability of these patients.1
The more the clinical condition of these patients is advanced, the more they will struggle to be autonomous in normal daily activities, in their work environment, and in their mobility.
It is therefore understandable to find a good correlation between functional indices in the literature, such as peak oxygen uptake (peakVO2), measured using cardiopulmonary exercise test (CPET) and 6MWD, long-term need of oxygen therapy, right heart failure, and quality of life (QoL) indices.9
Patients affected by PAH have to continuously deal with many challenges. On average, these patients are young, well-educated, and with access to the Internet or other media.
Unfortunately, the first information they find is the heavy prognosis of this disease and the statement that there is no cure.10
Other challenges for them are the uncertainty related to the delay in arriving at a correct diagnosis, the impact of the diagnosis, the rapid progression of symptoms, the impact of therapies, the loss of abilities, feelings of anxiety or depression, of being alone, and of being misunderstood by others.10
In recent years, pharmaceutical research has made new and effective drugs available, but they can be very expensive and often have heavy side effects. In more clinically advanced patients, it could also be necessary to undertake very heavy therapeutic pathways, that is, by pumps that allow the continuous infusion of prostanoid drugs by parenteral route. Such administration through tunneled catheters or intradermal needles is a daily challenge for patients and their caregivers. Some of these continuous infusion drugs can never be stopped, otherwise there could be lethal clinical consequences. The patients must therefore always have a sufficient supply of such drugs, some of which must also be stored in particular ways.10
Patients often refuse to take these drugs, which are thought to be usually reserved to the more advanced PAH stages, as if it was an irreversible step beyond a point of no return.11
In many cases, the patients must also perform oxygen therapy that further limits their ability to move and travel due to the need of carrying oxygen containers.
In selected PAH patients, it may be necessary to undergo complex cardiac surgery, or lung or heart-lung transplant.3
Finally, it should be remembered that in women of childbearing age, a possible pregnancy correlates with a risk of fetal death of about 50% and an increase in maternal mortality of up to 30%. Therefore, pregnancy is not recommended and contraception counseling should be given to these patients.12
This generates negative ideas about their desire to have a family and to have an intimate relationship.10 It also causes anxiety in patients and caregivers.
The primary research question of this review was to point out the prevalence and the impact of anxiety and depression on PAH and to propose management challenges.
Methods
The criteria used to elaborate this review were based on:
- Consultation of the latest international guidelines and consensus statements produced by the major scientific societies
- Identification of a reference bibliography based on evidence of effectiveness through a search of the most well-known databases (Cochrane Library, Medline, PsychINFO [2004–2018]), using the following keywords: anxiety, depression, stress, distress, psychological intervention, psycho-pharmacological intervention, caregivers.
Results
Prevalence of psychological symptoms
Analysis of the Registry to Evaluate Early and Long-term PAH Disease Management (REVEAL Registry) has shown that depression is a frequent occurrence in patients with PAH, with a significantly higher prevalence than the general population (25% vs 6.7%, respectively).5
The review shows that early studies have investigated the presence of mental disorders such as anxiety, depression, panic, and cognitive impairment.11,13,14 The prevalence of mental disorders in PAH patients lies between 7.5% and 53% for depression and 19% and 51% for anxiety and panic disorders, and the studies are summarized in Table 1.
Both panic disorder and panic attacks were significantly more prevalent in patients with PH than in either patients with inflammatory rheumatic diseases or primary care patients (control groups).11 The functional impairment influenced the presence of mental disorders (from 17.7% in WHO class I to 61.9% in WHO class IV).9 White et al studied the cognitive function and found cognitive impairment (verbal learning, verbal memory, and executive function) in 58% of PAH patients.14
Wryobeck et al, in addition to the impact of anxiety and depression on PAH patients, underlined the importance of the psychosocial aspects of PAH, such as adaptation to chronic illness, coping related factors, and social factors.15 The author suggested that for the PAH patient it is not the decrease in functioning that affects emotional well-being, but the impact of that change on the patient’s ability to engage in activity that provides meaning and allows them to fulfill roles that they view as important.15
Clinical importance of psychologic symptoms
The study of Mc Collister et al showed that only 45% of PAH patients had “no-to-minimal depressive symptoms” and that depressive symptoms were associated with worse physical functioning, as assessed by the 6MWD and functional class.16
Other more recent studies outlined the prevalence of anxiety and depression disorders and their association with QoL, clinical parameters, and survival in patients with PAH.17–22
The prospective study of Harzeim et al found that QoL impairment significantly correlated with the severity of depression and anxiety.17 In the study of Vanhoof et al, depression symptoms were found in one-third of patients, while anxiety and stress showed a prevalence of 48% and 27.6%, respectively.18 The authors showed that the presence of stress (difficulties relaxing, nervous arousal, being easily upset or agitated, being irritable or over-reactive, and being impatient) cannot be underestimated and need appropriate screening and psychological/psychotherapeutic and/or pharmacological treatment.18
Also, the results of the study of Somaini et al indicate that over one-third of PAH patients suffer from depression and/or anxiety, with a higher prevalence in incident compared to prevalent patients. Anxiety and depression correlate with the QoL, but not with baseline hemodynamics, age, or gender.19
Pfeuffer et al suggest an important difference in the prevalence of anxiety, depression, and perception of health-related quality of life (HRQoL) between chronic thromboembolic pulmonary hypertension (CTEPH) and PAH patients, with higher scores in CTEPH cohorts.20
Harzheim et al confirmed a little difference in anxiety and depression prevalence between PAH (22.5%) and CTEPH (25%) patients, but we must outline that the cohorts analyzed by Harzheim were younger than patients studied by Pfeuffer.17,20
A qualitative study was performed by Muntingh et al to explore mental problems, distress, and the need for support of PAH patients, identifying some issues, such as feeling misunderstood and handling of worries and emotions.21 For example, for female patients of childbearing age, the inability to have children due to the disease is particularly challenging. Also, unfamiliarity with a rare disease such as PAH and the healthy appearance of patients were specific aspects, which led to misunderstandings between PAH patients and their social environment.21 The results from the survey highlight the need of specialized support, especially for young, anxious, and depressed people.
Finally, a more recent study explored QoL, anxiety, depression, and coping strategies in 55 PAH patients and found high anxiety and depression, coping focused on medical information strategies, and poor QoL.22
Other studies focused their attention on the sleep disturbances, that are also not so infrequent in PAH, and on their correlation with worse PAH symptoms, psychological states, and HRQoL.23,24
These studies permit only limited conclusions because they were not specifically designed to better understand the emotional and social well-being of PAH patients, and the results were applicable only to patients willing and able to participate in controlled trials; these patients may have had better social support and coping skills.
Another problem, which still exists, is that there is no uniformity in QoL measures used or how anxiety and depression were operationalized.
The relation between anxiety, depression, and PH severity and QoL is summarized in Table 2.
Impact on caregivers
There are not many studies that have investigated psychological problems and burden in the family caregivers of PAH patients.
A recent review indicates that caregivers experience daily challenges creating uncertainty in terms of coping with the worsening of disease.25 Physicians should be aware of the caregivers’ problems that can cause significant burden. Caregiver’s burden is a multidimensional phenomenon affecting care-givers physically, emotionally, and socially.25
Limited research exists focusing on the broader impact of PAH on the lives of caregivers.
Hwang et al studied 35 patients with PAH and their caregivers and found the presence of depression in 14% of them and low social support.26 Lower levels of social support were significantly associated with more severe depressive symptoms in caregivers, and more than 85% of them were involved in disease managing.26
In a European survey, PAH patients’ perspectives on their situation and the health care provided to them were examined.10 The most reported symptoms were frustration, irritation, low self-esteem, feeling misunderstood and worthless, together with a fear for the future and isolation from their social environment. A high percentage of caregivers indicated that PAH had a profound effect on day-to-day life, often resulting in exhaustion because of the additional tasks and responsibilities.10
A recent Chinese survey suggests the important impact of PAH on the family, especially stress caused by the financial burden imposed by PAH and its treatment.27
These studies underline that caregivers of patients with PAH play a significant role in patients’ medical care and self-management, yet they lack sufficient emotional support or information to meet the demands of caregiving. These findings underscore the importance of supporting family caregivers of patients with PAH.
Treatment approaches
Löwe et al firstly indicated that only 24.1% of the patients with PAH with mental disorders received psychopharmacological or psychological/psychotherapeutic treatment,11 and Harzeim affirmed that only 8% of the patients with mental disorders received psychopharmacological treatment, suggesting a screening for mental disorder in PAH patients in clinical practice.17
The 2015 guidelines of European Society of Cardiology (ESC) and European Respiratory Society (ERS) affirm that “psychosocial support should be offered to patients with PAH” (level I-C recommendation.).3
Our review of anxiety and depression enables us to highlight the association between anxiety and depression, the presence of distress in patients and family, so the referral of patients diagnosed with PAH to a psychiatrist and/or psychologist should be considered when appropriate.3
In addition, health care professionals should ensure that patients are aware of the existence of patient support organizations, which can be a good source of emotional support, and how to contact them.28
Encouraging patients and their families to join patient support groups can have positive effects on coping, confidence, and outlook and provide practical assistance.
In a recent review, authors underline that other non-pharmacological interventions may serve an important purpose in providing the emotional support that has been shown to be fundamental to the well-being of patients with PAH and their families.29 In fact, recently, the adequate provision of psychosocial support has undergone close scrutiny by professional organizations.
The ESC/ERS guidelines state that “multidisciplinary teams should be involved in the delivery of psychosocial support, so that the psychological, social, financial, emotional, and spiritual needs of patients can be managed effectively”.3
Ultimately, in attempting to delineate and reduce the burden of PAH on the patient, it is important to understand that physician and patient expectations from disease management are likely to differ.30
The complexity of this disease and its management is described in Figure 1.
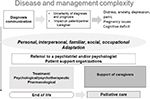  | Figure 1 Complexity of PAH disease and its management. Abbreviation: PAH, pulmonary arterial hypertension. |
Psychological intervention
To our knowledge, there are only few studies of psychological interventions in PAH.
At our institute, we conducted a study on 15 patients with PAH in WHO classes II and III.31 The primary end point was to evaluate the effect of training in an outpatient setting on oxygen consumption (VO2). The program consisted of aerobic training, respiratory exercises, and psychological intervention. Patients were checked before, 1 month after, and at the end of the rehabilitative intervention. Psychological variables (anxiety, depression, and QoL) were assessed by Hospital Anxiety Depression Inventory (HADS) and EuroQoL-5D before and after completion of treatment, while functional capacity was evaluated by spirometry, 6MWD, and CPET.
QoL improved significantly with large effect sizes in both the EQ-5D and the EQVAS. The level of anxiety and depression decreased significantly (P<0.01) with large effect sizes, with the patients’ level of anxiety passed below the threshold based on HADS norms.31
This is the first study that includes a structured psychological intervention in the multidisciplinary intervention. The aim of psychological intervention was: 1) to assess and to manage emotional issues (anxiety, depression, and panic attacks especially); 2) to enhance knowledge, awareness, and acceptance of the illness; and 3) to allow personal, interpersonal, family, social, and occupational adaptation to the disease.31
Cognitive–behavioral sessions (4–10 per patient), aimed to recognize the impact of behavioral and/or thinking patterns on feeling states and encouraging alternative cognitive and/or behavioral coping skills to reduce the severity of target symptoms and problems, were performed.
The themes covered were: 1) education on health and awareness both of symptoms and emotional reactions associated with them (it is important, in fact, that the patient learns to discriminate between symptom perception and its emotional consequences, ie, dyspnea and fear); 2) modification of inappropriate behavior connected to the illness and the management of symptoms; 3) psychological aspect on anxiety focused on symptoms; and 4) coping with uncertainty and adjusting to life.31
The patients also learned progressive muscle relaxation (PMR, 4–10 sessions), focusing attention onto particular muscle groups and understanding the differences between tensing and relaxing the muscles. In addition, individual respiratory relaxation sessions (Slow Breathing Relaxation Awareness [SBRA], 4–10 sessions), aimed to reduce the respiratory rate from 15 to 6 breaths-per minute through perception and awareness, were performed by both the psychologist and the physiotherapist.31
This study indicates that health psychology could offer a promising adjunct to medical treatment to symptomatic PAH patients.
Two other studies added relaxation techniques to multidisciplinary interventions.32,33 Relaxation techniques have been shown as an effective therapy for anxiety and depression, providing patients with self-maintenance coping skills to reduce anxiety symptoms.34,35 PMR is a systematic technique used to achieve a deep state of relaxation and has been shown to improve HRQoL in a variety of medical and psychiatric illnesses.36
Li et al conducted a controlled trial (130 patients randomized into a PMR group and a control group) to study the effects of PMR on anxiety, depression, and QoL in PAH patients.33 The PMR group received hospital-based group and in-home PMR practice, while the control group received hospital-based mild group stretching and balance exercises. After 12 weeks of intervention, the PMR group showed significant improvement in anxiety, depression, and QOL. The control group showed no significant improvement in any of the variables.33
In conclusion, the paucity of the studies does not permit us to affirm the evidence of the efficacy of specific psychological interventions amongst these patients.
Current guidelines for anxiety and depression in the general population recommend the combination of drugs and psychotherapy, mainly cognitive behavioral therapy (CBT), for moderate to severe depression while psychotherapy can be a valuable first step for mild depression and anxiety.37 The basic principal of CBT is a focused and structured collaborative environment to assist patients in solving problems and dysfunctional thinking. It is a collaborative effort between patients and clinicians to apply valuable strategies that can help patients to gain control.37
Possible approaches based on other chronic illnesses could therefore be suggested. In fact, CBT strategies have been used in cardiovascular diseases,38 and in COPD.39 However, there is a paucity of data regarding CBT in the PAH cohort.
Firstly, a good practice intervention, as indicated in a recent position paper regarding psychological activities in cardiovascular prevention and rehabilitation, could be suggested (Figure 2). It is recommended to structure all of the psychological activity within the multidisciplinary intervention and in synergy with the team.38
  | Figure 2 PAH psychological assessment and intervention. Abbreviation: PAH, pulmonary arterial hypertension. |
It is very important to assess the possible presence of psychopathological aspects in the medical history and to consider referring the patient to local community services. Further research should be recommended.
Slow breathing
Slow breathing is the pivot in yoga practices. Because of positive anecdotal evidence concerning yoga and meditative breathing, several studies have focused on determining the effectiveness of a variety of yoga slow-breathing techniques on the reduction of the sympathetic nervous system activity and blood pressure.40,41
The central respiratory neural network is anatomically and physiologically linked to autonomic outflow to the rest of the body. Respiratory sinus arrhythmia, for example, is modulated via changes in parasympathetic cardiac vagal outflow, causing an increase in vagal tone during expiration and a withdrawal during inhalation, controlled by pulmonary stretch afferents and the Hering-Breuer reflex.42
The changes of heart rate during the different phases of breathing may have a positive influence on lung gas exchange via a more efficient ventilation/perfusion matching. Controlled breathing has been shown to be beneficial in COPD, heart failure, and high altitude hypoxia that are characterized by a gas exchange impairment.43–46 These studies demonstrated that slow and controlled breathing can improve vagal activity and concomitantly reduce sympathoexcitation, with a favorable effect on symptoms and prognostic variables. Furthermore, controlled breathing can have a favorable psychological effect.43
In one of our previous studies conducted on PAH patients in our clinic’s outpatient service, we showed that slow breathing, together with a psychological intervention, may significantly decrease the level of anxiety and depression.31
In a recent study conducted in Philadelphia, slow breathing was applied to PAH patients, demonstrating favorable effects on sleep disturbances and depressive symptoms, together with decreased levels of IL-6,47 effect that in other studies has been shown to translate into a better survival and into ameliorating fatigue, anxiety, and depression.48,49
Slow breathing can be conducted in many ways. Some patients can manage themselves with yoga methods or self-paced breathing (ie, by using a metronome). A guide voice, mindfulness methods,50 or respiratory relaxation sessions (SBRA)31 can also be used. Finally, in a device-guided breathing protocol, patients may use a device, ResperateTM, that progressively slows down breathing acts through musical tones emitted by headphones and a sensor attached to the chest and able to detect respiratory movements.51
Pharmacological approach
Finally, the question remains whether it is appropriate to treat these patients pharmacologically. Doubt concerns the etiopathogenic role of serotonin as a factor favoring the onset or progression of PAH, and the possible favorable effect of SSRI drugs.
The hypothesis of serotonin on the genesis of PAH has been sustained in recent decades following the numerous cases of PAH related to the intake of anorectic agents such as aminorex fumarate and fenfluramine.52
In fact, serotonin promotes the proliferation of fibroblasts and smooth muscle cells of the pulmonary vessels, the vasoconstriction of these same vessels, and the genesis of microthrombosis in situ. These effects of serotonin are mediated by the interactions between the serotonin itself, its transporter (SERT), and its receptors. In the laboratory, the SERT plays a key role in the pathogenesis of experimental PAH, while the pharmacological blockade of SERT appears to be a protective factor.52
Preliminary studies have shown a possible positive effect of SSRIs on PAH. On the contrary, the use of SSRIs in pregnant women was found to be a risk factor for the development of persistent PH of the newborn, suggesting the suspicion that exposure to SSRIs could be harmful to the human lung vascular system under development.52
Indeed, other authors further underline the likely unfavorable action of SSRIs in PAH because, causing the increase of the serotonin concentration at the extracellular level and the consequent stimulation of the 5-HT1B receptor, they tend to increase the contractility of the pulmonary vessels.52
In fact, the use of antidepressants has been associated with a non-causal but significantly increased risk of PAH.
A recent Canadian study, based on the UK Clinical Practice Research Datalink Exam and the Hospital Episodes Statistics repository in the period between January 1, 1988 and September 30, 2011, reported a positive association between the use of SSRIs and PAH.53
In this study, incident cases of PAH were identified (195 patients with an incidence of 3.84/million per year) and matched to all controls to estimate the influence of the use of antidepressants on the risk of PAH.53
The use of any antidepressant in the 18-month period prior to diagnosis was associated with an increased risk of PAH (in 67% of cases). The rate of PAH was similar between the various classes of antidepressants, both with SSRIs and non-SSRI antidepressants. The consistency of this risk among all antidepressants and the absence of a dose–response relationship suggest a non-causal association.53
In another study, the authors examined the population of the REVEAL Registry matching patients reporting new SSRIs use to non-SSRI users.54 The analysis showed that in the REVEAL population, incident SSRI users, but not prevalent users, had an increased mortality and a greater risk of clinical worsening. But, at enrollment, SSRI users had worse New York Heart Association functional class and a tendency to walk a shorter distance at the 6MWD compared to patients without depression. As in other cardiovascular diseases, also in PAH the depression appears to be a well-defined risk factor related to physical inactivity.54 The authors point out how they could not correct the results for all the potential confounders, as depression and obesity.
In any case, this study was not able to verify any possible effect of SSRIs on depression and on the evolution of patients with PAH, suggesting the authors that a high incidence of depression (probably also underestimated) may have neutralized the favorable effects of SSRIs.54
Finally, it is noteworthy that we did not find any studies on the use of benzodiazepine in PAH, although their use is very frequent in patients with PAH for the treatment of anxiety and sleep disorders.
Conclusion
PAH is often characterized by a long-lasting latent period before it is clearly manifested and diagnosed so that patients end up inevitably experiencing high levels of stress and anxiety before the diagnosis has been made in a certain way.
Patients often apply positive strategies to cope with the anxiety due to the knowledge of the disease. However, in many cases, PAH has a devastating impact on patients and their families, producing responses of anxiety, depression, and panic attacks. These disorders are very frequent in PAH population, particularly in the early phases of the disease, when the uncertainty of diagnosis and prognosis are at the highest level. The frequency and intensity of these disorders correlate with the intensity of symptoms and the functional impairment experienced by the patients.
Unfortunately, physical limitation, easy fatigability, incapacity to make efforts even of minimum intensity, in addition to dependence on complex therapies, determine a social isolation and work difficulties with economic repercussions.
In fact, in addition to the impact of anxiety, depression, and coping related factors, there are also social factors. Social interactions are important for gaining and maintaining social acceptance, but for many individuals with a PAH diagnosis, physical limitations can lead to increased social isolation.
The real impact of these problems is underestimated due to the poor habit of testing patients from a psychological point of view and the lack of standardization in the assessment processes (no uniformity in anxiety and depression measures used or how anxiety and depression were operationalized).
The need for a psychiatric and/or psychological support and counseling in order to improve mental symptoms would also be beneficial in patients with PAH.
Also, nurse counseling and regular attendance of peer group sessions are available in centers with specific expertise in the treatment of PAH. This determines favorable effects on the mood of the patients.
Patients who have long been diagnosed and followed in a reference center have a lower frequency of psychological disorders than patients who have recently been diagnosed with PAH; this further demonstrates the positive effect of psychosocial support.
The research regarding the pharmacological treatment of anxiety and depression in PAH is not exhaustive. Studies that definitely demonstrate the efficacy or negative effects of antidepressant drugs on the progression of PAH are lacking.
Our hope and the purpose of works like this are to spread the culture on PH not only from the pathophysiological and pharmacological point of view, but also on the psychological and social aspects that the disease itself determines.
Regular screening to provide social and emotional support to patients with PAH and their families would be desirable, with an appropriate program of psychological/psychotherapeutic and/or pharmacological treatment.
Disclosure
The authors report no conflicts of interest in this work.
References
Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D42–D50. | ||
Simonneau G, Galiè N, Rubin LJ, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004;43(12):S5–S12. | ||
Galié N, Humbert M, Vachiery JL, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. The task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Endorsed by: Association for Paedriatic and Congenital Cardiology (AEPC), International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. 2015;37:67–119. | ||
D’Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;1;115(5):343–349. | ||
Badesch DB, Raskob GE, Elliott CG, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137:376–387. | ||
Barst RJ, Chung L, Zamanian RT, Turner M, Mcgoon MD. Functional class improvement and 3-year survival outcomes in patients with pulmonary arterial hypertension in the REVEAL Registry. Chest. 2013;144(1):160–168. | ||
Mclaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002;106:1477–1482. | ||
Sitbon O, McLaughlin VV, Badesch DB, et al. Survival in patients with class III idiopathic pulmonary arterial hypertension treated with first line oral bosentan compared with an historical cohort of patients started on intravenous epoprostenol. Thorax. 2005;60:1025–1030. | ||
Halank M, Einsle F, Lehman S, et al. Exercise capacity affects quality of life in patients with pulmonary hypertension. Lung. 2013;191(4):337–343. | ||
Guillevin L, Armstrong I, Aldrighetti R, et al. Understanding the impact of pulmonary arterial hypertension on patients’ and carers’ lives. Eur Respir Rev. 2013;22(130):535–542. | ||
Löwe B, Gräfe K, Ufer C, et al. Anxiety and depression in patients with pulmonary hypertension. Psychosom Med. 2004;66(6):831–836. | ||
Olsson KM, Channick R. Pregnancy in pulmonary arterial hypertension. Eur Respir Rev. 2016;25(142):431–437. | ||
Shafazand S, Goldstein MK, Doyle RL, Hlatky MA, Gould MK. Health-related quality of life in patients with pulmonary arterial hypertension. Chest. 2004;126(5):1452–1459. | ||
White J, Hopkins RO, Glissmeyer EW, Kitterman N, Elliott CG, Cognitive ECG. Cognitive, emotional, and quality of life outcomes in patients with pulmonary arterial hypertension. Respir Res. 2006;7(1):55. | ||
Wryobeck JM, Lippo G, Mclaughlin V, Riba M, Rubenfire M. Psychosocial aspects of pulmonary hypertension: a review. Psychosomatics. 2007;48(6):467–475. | ||
Mccollister DH, Beutz M, Mclaughlin V, et al. Depressive symptoms in pulmonary arterial hypertension: prevalence and association with functional status. Psychosomatics. 2010;51(4):339–339. | ||
Harzheim D, Klose H, Pinado FP, et al. Anxiety and depression disorders in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Respir Res. 2013;14(1):104. | ||
M M Vanhoof J, Delcroix M, Vandevelde E, et al. Emotional symptoms and quality of life in patients with pulmonary arterial hypertension. J Heart Lung Transplant. 2014;33(8):800–808. | ||
Somaini G, Hasler ED, Saxer S, et al. Prevalence of Anxiety and Depression in Pulmonary Hypertension and Changes during Therapy. Respiration. 2016;91(5):359–366. | ||
Pfeuffer E, Krannich H, Halank M, et al. Anxiety, Depression, and Health-Related QOL in Patients Diagnosed with PAH or CTEPH. Lung. 2017;195(6):759–768. | ||
Muntingh ADT, Gerritsen S, Batelaan NM, Bogaard HJ. Pathways to experiencing mental problems and need for mental support in patients with pulmonary arterial hypertension. Pulm Circ. 2017;7(3):609–616. | ||
Halimi L, Marin G, Molinari N, et al. Impact of psychological factors on the health-related quality of life of patients treated for pulmonary arterial hypertension. J Psychosom Res. 2018;105:45–51. | ||
Batal O, Khatib OF, Bair N, Aboussouan LS, Minai OA. Sleep quality, depression, and quality of life in patients with pulmonary hypertension. Lung. 2011;189(2):141–149. | ||
Matura LA, Mcdonough A, Hanlon AL, Carroll DL, Riegel B, Disturbance S. Sleep disturbance, symptoms, psychological distress, and health-related quality of life in pulmonary arterial hypertension. Eur J Cardiovasc Nurs. 2015;14(5):423–430. | ||
Verma S, Sayal A, Vijayan VK, Rizvi SM, Talwar A. Caregiver’s burden in pulmonary arterial hypertension: a clinical review. J Exerc Rehabil. 2016;12(5):386–392. | ||
Hwang B, Howie-Esquivel J, Fleischmann KE, Stotts NA, Dracup K. Family caregiving in pulmonary arterial hypertension. Heart Lung. 2012;41(1):26–34. | ||
Zhai Z, Zhou X, Zhang S, et al. The impact and financial burden of pulmonary arterial hypertension on patients and caregivers: results from a national survey. Medicine. 2017;96(39):e6783. | ||
European Pulmonary Hypertension Association (PHA). The impact of pulmonary arterial hypertension (PAH) on the lives of patients and carers: results from an international survey. International-PAH-patient-and-Carer-Survey-Report-FINAL1.pdf [updated: September 2012]. Available from: www.phaeurope.org/wp-content/uploads/. Accessed June 29, 2015. | ||
Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev. 2015;24(138):621–629. | ||
Howard LS, Ferrari P, Mehta S. Physicians’ and patients’ expectations of therapies for pulmonary arterial hypertension: where do they meet? Eur Respir Rev. 2014;23(134):458–468. | ||
Bussotti M, Gremigni P, Pedretti RFE, et al. Effects of an outpatient service rehabilitation programme in patients affected by pulmonary arterial hypertension: an observational study. Cardiovasc Hematol Disord Drug Targets. 2017;17(1):3–10. | ||
Mereles D, Ehlken N, Kreuscher S, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. 2006;114(14):1482–1489. | ||
Li Y, Wang R, Tang J, et al. Progressive muscle relaxation improves anxiety and depression of pulmonary arterial hypertension patients. Evid Based Complement Alternat Med. 2015;792895. | ||
Barrows KA, Jacobs BP. Mind-body medicine. An introduction and review of the literature. Med Clin North Am. 2002;86(1):11–31. | ||
Weiss M, Nordlie JW, Siegel EP. Mindfulness-based stress reduction as an adjunct to outpatient psychotherapy. Psychother Psychosom. 2005;74(2):108–112. | ||
Dehdari T, Heidarnia A, Ramezankhani A, Sadeghian S, Ghofranipour F. Effects of progressive muscular relaxation training on quality of life in anxious patients after coronary artery bypass graft surgery. Ind J Med Res. 2009;129(5):603–608. | ||
Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry. 2011;23(4):318–327. | ||
Sommaruga M, Angelino E, della Porta P, et al. Best practice in psychological activities in cardiovascular prevention and rehabilitation: Position Paper. Monaldi Arch Chest Dis. 2018;88(2):966. | ||
Tselebis A, Pachi A, Ilias I, et al. Strategies to improve anxiety and depression in patients with COPD: a mental health perspective. Neuropsychiatr Dis Treat. 2016;12:297–328. | ||
Pal GK, Velkumary SM. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120(2):115–121. | ||
Bhavanani AB, Madanmohan, Sanjay Z, Basavaraddi IV. Immediate cardiovascular effects of pranava pranayama in hypertensive patients.. 2012;56(3):273–278. | ||
Yasuma F, Hayano J. Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm? Chest. 2004;125(2):683–690. | ||
Raupach T, Bahr F, Herrmann P, et al. Slow breathing reduces sympathoexcitation in COPD. Eur Respir J. 2008;32(2):387–392. | ||
Valenza MC, Valenza-Peña G, Torres-Sánchez I, González-Jiménez E, Conde-Valero A, Valenza-Demet G. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: a randomized clinical Trial. Respir Care. 2014;59(2):209–215. | ||
Bernardi L, Porta C, Spicuzza L, Bellwon J, Spadacini G, Frey AW. Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation. 2002;105(2):143–145. | ||
Bilo G, Revera M, Bussotti M, et al. Effects of slow deep breathing at high altitude on oxygen saturation, pulmonary and systemic hemodynamics. PLoS One. 2012;7(11):e49074. | ||
Matura LA, Fargo J, Fritz JS, et al. Slow-paced respiration therapy to treat symptoms in pulmonary arterial hypertension. Heart Lung. 2017;46(1):7–13. | ||
Soon E, Holmes AM, Treacy CM, et al. Elevated Levels of Inflammatory Cytokines Predict Survival in Idiopathic and Familial Pulmonary Arterial Hypertension. Circulation. 2010;122(9):920–927. | ||
Matura LA, Ventetuolo CE, Palevsky HI, et al. Interleukin-6 and tumor necrosis factor-α are associated with quality of life-related symptoms in pulmonary arterial hypertension. Ann Am Thorac Soc. 2015;12(3):370–375. | ||
Tulloh RMR, Garratt V, Tagney J, et al. A pilot randomised controlled trial investigating a mindfulness-based stress reduction (MBSR) intervention in individuals with pulmonary arterial hypertension (PAH): the PATHWAYS study. Pilot Feasibility Stud. 2018;4(1):78. | ||
Cernes R, Zimlichman R. RESPeRATE: the role of paced breathing in hypertension treatment. J Am Soc Hypertens. 2015;9(1):38–47. | ||
Maclean MMR. The serotonin hypothesis in pulmonary hypertension revisited: targets for novel therapies (2017 Grover Conference Series. Pulm Circ. 2018;8(2):2045894018759125. | ||
Fox BD, Azoulay L, dell’aniello S, et al. The use of antidepressants and the risk of idiopathic pulmonary arterial hypertension. Can J Cardiol. 2014;30(12):1633–1639. | ||
Sadoughi A, Roberts KE, Preston IR, et al. Use of selective serotonin reuptake inhibitors and outcomes in pulmonary arterial hypertension. Chest. 2013;144(2):531–541. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


