Back to Journals » Journal of Hepatocellular Carcinoma » Volume 9
Antiviral Treatments Eliminate the Adverse Impacts of High Baseline HBV Loads on the Survival of HBV-Related HCC Patients
Authors Hu Z , Sun X, Mei J , Hu Z, Yang Z, Hou J, Fu Y , Wang X , Chen M
Received 18 February 2022
Accepted for publication 4 April 2022
Published 19 April 2022 Volume 2022:9 Pages 315—325
DOI https://doi.org/10.2147/JHC.S363123
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Laura A. Dawson
Zili Hu,1,2,* Xuqi Sun,3,* Jie Mei,1,2,* Zhiwen Hu,1,2 Ziliang Yang,1,2 Jingyu Hou,1,2 Yizhen Fu,1,2 Xiaohui Wang,4 Minshan Chen1,2
1Department of Liver Surgery, Sun Yat-Sen University Cancer Center, Guangzhou, 510060, People’s Republic of China; 2Collaborative Innovation Center for Cancer Medicine, State Key Laboratory of Oncology in South China, Sun Yat-Sen University Cancer Center, Guangzhou, Guangdong, 510060, People’s Republic of China; 3Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310003, People’s Republic of China; 4Department of Hepatobiliary Surgery, Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Changsha, 410005, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Minshan Chen, Department of Liver Surgery, Sun Yat-sen University Cancer Center, Dongfeng Road East 651, Guangzhou, Guangdong, 510060, People’s Republic of China, Tel +86-20-87343117, Email [email protected] Xiaohui Wang, Department of Hepatobiliary Surgery, Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Jiefang Road West 61, Changsha, Hunan, 410005, People’s Republic of China, Tel +86-073183928052, Email [email protected]
Background: In consideration of no standard exclusion criteria for hepatitis B virus (HBV) loads in hepatocellular carcinoma (HCC)-related clinical trials, this study aimed to investigate the prevalence of HBV-related exclusion criteria among current clinical trials and evaluate whether antiviral treatments could eliminate the adverse effects from high HBV loads for HCC patients.
Methods: This is a retrospective study including 772 HCC clinical trials on ClinicalTrials.gov and 1784 HCC patients receiving antiviral treatment. The Kaplan–Meier (K-M) method was used to compare the progression-free survival (PFS) and overall survival (OS) between different groups, and Cox regression analyses were performed to validate possible risk factors on PFS and overall survival OS.
Results: Among 772 clinical trials, 58.3% did not adopt baseline HBV loads as exclusion criteria, 18.0% was 2000 IU/mL, and 10.5% was receiving antiviral therapy. We observed baseline HBV loads had no significant impact on PFS (p = 0.491, 0.155, 0.119, 0.788, 0.280, 0.683 respectively) and OS (p = 0.478, 0.741, 0.263, 0.039, 0.999, 0.581 respectively) in all patients or each treatment group including hepatectomy, radiofrequency ablation, interventional therapy, targeted drugs and anti-programmed cell death immunotherapy, except for the OS of interventional therapy group, where patients with high HBV loads had higher BCLC stage, serum AFP level and ALBI grade (p = 0.009, 0.015 and 0.003, respectively).
Conclusion: Antiviral treatments could eliminate the adverse impacts of high HBV loads on the survival of HCC patients. Simplified eligibility criteria can be adopted for HCC patients with HBV infection where regular antiviral therapy should be enough.
Keywords: hepatocellular carcinoma, hepatitis B virus loads, antiviral treatment, exclusion criteria, clinical trials
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancy and ranks as the third leading cause of cancer-related mortality.1 Although curative treatments achieve promising survival in patients with early-stage HCC, the prognosis remains dismal among those at advanced stage.2 Clinical trials can help solve this dilemma by identifying effective therapies for patients with advanced HCC such as lenvatinib by the REFLECT trial and atezolizumab plus bevacizumab by the IMbrave150 trial.3,4 However, clinical trials are currently in crisis due to low patient accrual rates, which impede the completion of trials.5,6 Obstacles to patient enrollment can extend trial duration and limit the generalizability of trials, and complex eligibility criteria are a major barrier to patient accrual.7,8
Approximately 54% HCC patients are infected with hepatitis B virus (HBV), the proportion of which reaches to 70–80% in endemic region.9 However, clinical trials usually exclude HCC patients with high baseline HBV loads. For instance, HCC patients with HBV loads >100IU/mL were excluded from CheckMate 040, and they were consistently omitted from KEYNOTE-224.10,11 Eligibility criteria from previous protocols are reflexively applied to clinical trials with similar study populations without scientific justification.12 The reflexive exclusion of HCC patients with HBV infection from trials is presumably for the concerns that high baseline HBV loads can adversely affect or interfere with clinical outcomes.13 All HBsAg-positive HCC patients are recommended to accept NAs therapy.14,15 With effective antiviral drugs such as entecavir and tenofovir, however, few studies have explored whether antiviral treatments could reverse the adverse impact of high baseline HBV loads on clinical outcomes, which can potentially expand the enrollment of clinical trials.
This study aimed to investigate the prevalence of HBV-related exclusion criteria among current clinical trials and to evaluate whether antiviral treatments could eliminate the adverse effects from high HBV loads for HCC patients, which assisted to identify reasonable inclusion criteria for HCC patients and improve the accrual rates of clinical trials.
Materials and Methods
Clinical Trials Selection
To investigate the prevalence of requirements of baseline HBV loads among HCC clinical trials, we reviewed HCC clinical trials on ClinicalTrials.gov. Trials with “withdrawn status” were excluded considering that their protocols might be unreasonable. We also excluded trials lacking necessary information or enrolling other tumors except for HCC. Finally, 772 HCC clinical trials were included for analysis. Detailed description of trials enrollment is shown in Figure 1.
 |
Figure 1 Flow diagram of HCC clinical trials enrollment on ClinicalTrials.gov. |
Patient Selection
We retrospectively reviewed the clinical data on consecutive HCC patients in Sun Yat-sen University Cancer Center from January 2011 to December 2020. The inclusion criteria of patients were as following: 1) age at diagnosis ≥18 years old; 2) clinically or pathologically diagnosed as HCC according to ESMO guidelines and 3) with positive hepatitis B virus surface antigen (HBsAg). Patients were excluded when meeting any of the following criteria: 1) without pretreatment baseline HBV DNA tests; 2) coinfected with other hepatitis viruses such as hepatitis C virus; 3) only receiving best supportive care; 4) incomplete clinical data; 5) initiating antiviral treatments more than one week after initial anti-HCC therapy or 6) receiving other antiviral drugs except for entecavir or tenofovir. Eventually, a total of 1784 HCC patients were included for analysis in this study. The treatment modalities can be classified into hepatectomy, radiofrequency ablation (RFA), interventional therapy, targeted drugs and anti-programmed cell death (PD) immunotherapy. Serum HBV loads was measured by real-time viral polymerase chain reaction with a lower detection limit of 30 IU/mL.
Statistical Analysis
The demographic and clinical characteristics were compared between HCC patients with baseline HBV loads <2000 IU/mL and those with baseline HBV loads ≥2000 IU/mL. Two-sample independent t-test was adopted to compare age at diagnosis with a normal distribution. Chi-square test was performed to compare categorical characteristics between the two groups. The Kaplan–Meier (K-M) method was used to compare the progression-free survival (PFS) and overall survival (OS) between groups with high and low baseline HBV loads. The PFS was defined as the period from initial treatments to the first progression or death. The OS was measured from the time of initial treatments to the date of death or last follow-up. Cox regression model was adopted to identify significant factors for the PFS and OS including age at diagnosis, gender, Barcelona Clinic Liver Cancer (BCLC) stage, serum alpha-fetoprotein (AFP) level, albumin-bilirubin (ALBI) grade, treatment modalities and antiviral drugs. The analyses were performed using IBM SPSS, version 25.0. The survival curves were plotted with R software version 3.3.2. A two-tailed P value <0.05 was statistically significant.
Results
Characteristics of Included Trials and HBV Exclusion Criteria
They included 772 clinical trials enrolling a total of 98,340 patients. The characteristics and relevant HBV loads exclusion criteria are summarized in Table 1. Among these trials, 58.3% (450/772) did not adopt baseline HBV loads as exclusion criteria. The criteria of HBV infection varied among protocols of the rest trials. The most common cutoff value of exclusion criteria for HBV loads was 2000 IU/mL (18.0%, 139/772). Receiving antiviral therapy was the secondary most common inclusion criteria for patients with HBV-related HCC (10.5%, 81/772). The other common cutoff values of HBV loads for exclusion criteria were 100 IU/mL, 500 IU/mL and 0 IU/mL. The association between clinical trial characteristics and HBV-related exclusion criteria is shown in Supplementary Table 1. Overall, HBV-related exclusion criteria were more common in Phase I/II trials and trials for systemic treatments. Besides, modern trials excluded HCC patients with high HBV loads more often. The proportion of exclusion criteria for HBV loads increased with the stage of HCC.
 |
Table 1 Characteristics of HCC Clinical Trials and Their HBV Loads Related Exclusion Criteria |
Patient Characteristics
The clinical characteristics of 1784 HCC patients are presented in Table 2. No significant association was found between baseline HBV loads and age or gender. Patients with baseline HBV loads ≥2000 IU/mL had more advanced HCC than those with baseline HBV loads <2000 IU/mL. Serum AFP level had a similar trend. The liver function was slightly worse in the group with high HBV loads. The use of type of antiviral drugs was similar between groups with high and low baseline HBV loads. To specifically evaluate the impact of HBV loads on survival, patients were further classified into subgroups according to their initial treatment modalities. Among the whole cohort, 870 patients received hepatectomy, 109 patients received RFA, 424 patients were treated with interventional therapy including transarterial chemoembolization (TACE) and hepatic arterial infusion chemotherapy (HAIC), 187 patients were treated with targeted drugs and 194 patients received anti-PD-1 immunotherapy.
 |
Table 2 Baseline Demographic and Clinical Characteristics of HCC Patients with Different Baseline HBV Loads |
Impact of Baseline HBV Loads on the Survival of HCC Patients
The median follow-up time was 43.03 months. During the follow-up, 53.5% (955/1784) suffered from disease progression, and 27.2% (487/1784) of patients died. No significant difference was found in PFS between patients with baseline HBV loads <2000 IU/mL and those with baseline HBV loads ≥2000 IU/mL (p = 0.491). The survival curves are shown in Figure 2A. Similar trends were detected when the cutoff values were set at 500 IU/mL, 100 IU/mL and 0 IU/mL (p = 0.296, 0.463 and 0.521 respectively). In multivariate analysis, BCLC stage, serum AFP level, ALBI grade and treatment modalities were significantly associated with PFS. Detailed data are listed in Table 3. Baseline HBV loads had no significant impact on PFS (p = 0.491; hazard ratio (HR), 1.05; 95% confidence interval (CI), 0.92–1.19).
 |
Table 3 Univariate and Multivariate Analyses for Prognostic Factors of PFS and OS |
 |
Figure 2 Kaplan–Meier curves of progression-free survival in all HCC patients (A) or different treatment group (B–F). |
The OS was also similar between HCC patients with HBV loads <2000 IU/mL and those with HBV loads ≥2000 IU/mL (p = 0.478) (Figure 3A). Similarly, the OS did not differ significantly between groups with low and high baseline HBV loads when the cutoff values were sat at 500 IU/mL, 100 IU/mL and 0 IU/mL (p = 0.539, 0.842 and 0.898 respectively). In univariate analysis, BCLC stage was significantly correlated with OS (p < 0.001). Serum AFP had negative association with OS (p < 0.001). Similarly, patients with higher ALBI grade had worse survival (p < 0.001). Treatment modalities were also associated with OS significantly (p < 0.001). Patients receiving tenofovir had longer OS than those receiving entecavir (p < 0.001). The above factors remained significant in the multivariate analysis (Table 3). However, no significant association was detected between baseline HBV loads and OS (p = 0.478; HR, 1.07; 95% CI, 0.89–1.27).
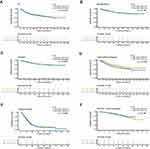 |
Figure 3 Kaplan–Meier curves of overall survival in all HCC patients (A) or different treatment group (B–F). |
Impact of Baseline HBV Loads Classified by Treatment Modality
To specifically evaluate the prognostic impact of HBV in each treatment modality, we further compared the survival between patients with low and high baseline HBV loads in each subgroup classified by treatments. There was no significant association between PFS and baseline HBV loads in each treatment group. The survival curves are shown in Figure 2B–F. In terms of OS, patients with high baseline HBV loads had similar survival compared to those with low HBV loads in all subgroups except for the group receiving interventional therapy (Figure 3B–F). In group with intervention treatment, patients with high HBV loads had higher BCLC stage, serum AFP level and ALBI grade (p = 0.009, 0.015 and 0.003, respectively). After multivariate analyses, baseline HBV loads did not correlate with OS significantly in HCC patients receiving interventional therapy (p = 0.317; HR, 1.20; 95% CI, 0.84–1.70).
Discussion/Conclusion
In this study, we reviewed clinical trials for HCC and found that 41.7% trials adopted baseline HBV loads as exclusion criteria. To validate the validity of this criterion, we compared the prognosis of HCC patients who received antiviral treatments but had different baseline HBV loads and found that antiviral treatments could eliminate the adverse impact of high HBV loads on the survival of HCC patients. These findings could assist in increasing patient enrollment and improving the efficiency and generalizability of clinical trials.
In recent years, the first-line treatments of HCC have been updated by the results from clinical trials such as lenvatinib from the REFLECT trial and atezolizumab plus bevacizumab from the IMbrave150 trial.3,4 Anti-PD-1 immunotherapy has changed the landscape of treatments for unresectable HCC, and oncologists are exploring how to improve the survival of HCC patients by the combination of immunotherapy and other treatment modalities, which are mainly based on clinical trials.16 Clinical trials improve the management of patients and prove the feasibility of new treatments. However, only 2–4% cancer patients are recruited in trials, and half of National Cancer Institute-sponsored trials are completed.17,18 Low accrual rates can prolong the duration of enrollment, which increases the risk of termination of trials.18 Barriers to enrollment involve clinician, patient and trial factors, among which strict eligibility criteria is a major obstacle. Strict inclusion criteria may compromise the generalizability of clinical trials and prevent potential beneficiaries from accessing new therapies.19 Despite proposals for simplified and rational criteria, eligibility criteria have become more complex and stringent over time. Our results showed that the proportion of HBV-related exclusion criteria had been increasing over years. Excluding HCC patients with high baseline HBV loads may be due to the long-held belief that high HBV loads can cause adverse impacts on the survival. However, few studies have evaluated the rationality of this criterion. Considering the high prevalence of HBV in HCC patients, this eligibility criterion can severely limit accrual rates.
Currently, the criteria of HBV infection varied among clinical trials. Different cutoff values were set for exclusion criteria, while some trials only required patients to receive antiviral therapy. To our knowledge, no research has been conducted to explore which is the most appropriate criterion. For clinical trials, exclusion criteria should not only exclude factors that can potentially affect clinical outcomes but guarantee enrolling eligible patients as much as possible. This study showed that both PFS and OS were similar between HCC patients with low and high baseline HBV loads when they received antiviral treatments. If HCC patients with high baseline HBV loads are excluded from clinical trials due to perceived risks that HBV may have negative impacts on the survival of patients, our results may alleviate this concern.
Investigators may concern that high baseline HBV loads can adversely affect the prognosis of HCC patients since previous studies have reported that HCC patients with high HBV loads had worse survival than those with low HBV loads in different treatment modalities such as hepatectomy, TACE, sorafenib and so on.20–22 However, these studies did not further analyze whether antiviral treatments could eliminate the adverse effects of high HBV loads. Till now, the validity of this concern has barely been validated. Takafumi et al have reported that chronic viral hepatitis does not significantly compromise the efficiency of anticancer agents or adversely affect the survival in Phase I clinical trials.23 They also found that there was no significant difference in the rates of hepatitis virus reactivation and adverse events between patients with negative and positive hepatitis virus. Besides, the efficiency and feasibility of nivolumab was similar in patients with and without viral hepatitis in CheckMate 040.10 We specifically compared the survival of HCC patients with low and high HBV loads when they were treated with antiviral drugs in reported studies. With antiviral treatments, the prognosis was comparable between patients with HBV loads <2000 IU/mL and those with HBV loads ≥2000 IU/mL after undergoing hepatectomy for early-stage HBV-related HCC.24 For HCC patients receiving sorafenib, antiviral treatments could eliminate the adverse impacts of high HBV loads on survival.25 Peter et al found that antiviral therapy can provide benefits for HCC patients in terms of survival, liver function and adverse events.26 Similarly, HCC patients receiving TACE or anti-PD-1 immunotherapy can also benefit from antiviral therapy.27 According to above findings, it can be inferred that antiviral drugs can eliminate the adverse effects of high HBV loads on the survival of HCC patients. Thus, receiving antiviral treatment is necessary for patients with HBV-related HCC in clinical trials. However, baseline HBV DNA levels may not be reasonable exclusion criteria, which can decrease accrual rates of trials.
This study has several limitations except for its retrospective nature. First, this study focused on the impacts of HBV loads on survival outcomes but did not further evaluate whether the rates of HBV reactivation and adverse events differed among HCC patients with different viral loads. It has been reported that HBV reactivation had no significant association with OS in HCC receiving HAIC with antiviral treatments.28 Nucleoside analogs can inhibit hepatitis activity and reverse liver function, which improves patients’ tolerance to anticancer therapy and survival.29 Second, HBV loads were only measured at baseline, while the changes in viral loads were not regularly monitored. Whether the decline of HBV loads affects clinical outcomes needs further exploration. The purpose of this study focused on expanding clinical trial enrollment by evaluating whether baseline HBV loads could affect the survival of HCC patients with antiviral treatments. Third, proper eligibility criteria remain to be explored for HCC patients with hepatitis C virus infection.
In conclusion, antiviral treatments could eliminate the adverse impacts of high baseline HBV loads on the survival of HCC patients. Simplified eligibility criteria can be adopted for HCC patients with HBV infection where regular antiviral therapy should be enough. Strict criteria for baseline HBV loads may compromise the efficiency and generalizability.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted according to the ethical guidelines of the 1975 Declaration of Helsinki. This research was approved by the institutional review board of Sun Yat-sen University Cancer Center. The study used retrospective anonymous clinical data that were obtained after each patient agreed to treatment.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Vogel A, Cervantes A, Chau I, et al. Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(5):871–873. doi:10.1093/annonc/mdy510
3. Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi:10.1056/NEJMoa1915745
4. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–1173. doi:10.1016/S0140-6736(18)30207-1
5. Lara PN, Higdon R, Lim N, et al. Prospective evaluation of cancer clinical trial accrual patterns: identifying potential barriers to enrollment. J Clin Oncol. 2001;19(6):1728–1733. doi:10.1200/JCO.2001.19.6.1728
6. Scoggins JF, Ramsey SD. A national cancer clinical trials system for the 21st century: reinvigorating the NCI Cooperative Group Program. J Natl Cancer Inst. 2010;102(17):1371. doi:10.1093/jnci/djq291
7. Filion M, Forget G, Brochu O, et al. Eligibility criteria in randomized Phase II and III adjuvant and neoadjuvant breast cancer trials: not a significant barrier to enrollment. Clin Trials. 2012;9(5):652–659. doi:10.1177/1740774512456453
8. Lemieux J, Goodwin PJ, Pritchard KI, et al. Identification of cancer care and protocol characteristics associated with recruitment in breast cancer clinical trials. J Clin Oncol. 2008;26(27):4458–4465. doi:10.1200/JCO.2007.15.3726
9. Akinyemiju T, Abera S, Ahmed M, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol. 2017;3(12):1683–1691. doi:10.1001/jamaoncol.2017.3055
10. El-Khoueiry AB, Sangro B, Yau T, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, Phase 1/2 dose escalation and expansion trial. Lancet. 2017;389(10088):2492–2502. doi:10.1016/S0140-6736(17)31046-2
11. Zhu AX, Finn RS, Edeline J, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label Phase 2 trial. Lancet Oncol. 2018;19(7):940–952. doi:10.1016/S1470-2045(18)30351-6
12. Kim ES, Bernstein D, Hilsenbeck SG, et al. Modernizing Eligibility Criteria for Molecularly Driven Trials. J Clin Oncol. 2015;33(25):2815–2820. doi:10.1200/JCO.2015.62.1854
13. Ohkubo K, Kato Y, Ichikawa T, et al. Viral load is a significant prognostic factor for hepatitis B virus-associated hepatocellular carcinoma. Cancer. 2002;94(10):2663–2668. doi:10.1002/cncr.10557
14. Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380. doi:10.1002/hep.29086
15. Vogel A, Cervantes A, Chau I, et al. Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:238–255. doi:10.1093/annonc/mdy308
16. Pinter M, Jain RK, Duda DG. The current landscape of immune checkpoint blockade in hepatocellular carcinoma: a review. JAMA Oncol. 2021;7(1):113–123. doi:10.1001/jamaoncol.2020.3381
17. Howerton MW, Gibbons MC, Baffi CR, et al. Provider roles in the recruitment of underrepresented populations to cancer clinical trials. Cancer. 2007;109(3):465–476. doi:10.1002/cncr.22436
18. Ding CY, Peng L, Lin YX, Yu LH, Wang DL, Kang DZ. Elevated lactate dehydrogenase level predicts postoperative pneumonia in patients with aneurysmal subarachnoid hemorrhage. World Neurosurg. 2019;129:e821–e30. doi:10.1016/j.wneu.2019.06.041
19. Zhou H, Huang Y, Qiu Z, et al. Impact of prior cancer history on the overall survival of patients newly diagnosed with cancer: a pan-cancer analysis of the SEER database. Int J Cancer. 2018;143(7):1569–1577. doi:10.1002/ijc.31543
20. Yang T, Lu JH, Zhai J, et al. High viral load is associated with poor overall and recurrence-free survival of hepatitis B virus-related hepatocellular carcinoma after curative resection: a prospective cohort study. Eur J Surg Oncol. 2012;38(8):683–691. doi:10.1016/j.ejso.2012.04.010
21. Yu SJ, Lee JH, Jang ES, et al. Hepatocellular carcinoma: high hepatitis B viral load and mortality in patients treated with transarterial chemoembolization. Radiology. 2013;267(2):638–647. doi:10.1148/radiol.13121498
22. Yang Y, Wen F, Li J, et al. A high baseline HBV load and antiviral therapy affect the survival of patients with advanced HBV-related HCC treated with sorafenib. Liver Int. 2015;35(9):2147–2154. doi:10.1111/liv.12805
23. Koyama T, Kondo S, Shimizu T, et al. Impact of hepatitis virus on the feasibility and efficacy of anticancer agents in patients with hepatocellular carcinoma in phase I clinical trials. Front Oncol. 2019;9:301. doi:10.3389/fonc.2019.00301
24. Ge Z, Ma J, Qiao B, Wang Y, Zhang H, Gou W. Impact of tenofovir antiviral treatment on survival of chronic hepatitis B related hepatocellular carcinoma after hepatectomy in Chinese individuals from Qingdao municipality. Medicine (Baltimore). 2020;99(32):e21454. doi:10.1097/MD.0000000000021454
25. Xu L, Gao H, Huang J, et al. Antiviral therapy in the improvement of survival of patients with hepatitis B virus-related hepatocellular carcinoma treated with sorafenib. J Gastroenterol Hepatol. 2015;30(6):1032–1039. doi:10.1111/jgh.12910
26. Galle PR, Kudo M, Llovet JM, et al. Ramucirumab in patients with previously treated advanced hepatocellular carcinoma: impact of liver disease aetiology. Liver Int. 2021;41(11):2759–2767. doi:10.1111/liv.14994
27. Xu X, Huang P, Tian H, et al. Role of lamivudine with transarterial chemoembolization in the survival of patients with hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29(6):1273–1278. doi:10.1111/jgh.12554
28. Liu S, Lai J, Lyu N, et al. Effects of antiviral therapy on HBV reactivation and survival in hepatocellular carcinoma patients undergoing hepatic artery infusion chemotherapy. Front Oncol. 2020;10:582504. doi:10.3389/fonc.2020.582504
29. Zhong JH. Nucleos(t)ide analogue therapy for HBV-related HCC after hepatic resection: clinical benefits and unanswered questions. Tumour Biol. 2014;35(12):12779–12784. doi:10.1007/s13277-014-2881-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
