Back to Journals » International Journal of General Medicine » Volume 14
Antithyroid Peroxidase Antibodies and Histopathological Outcomes in Egyptian Patients Subjected to Total Thyroidectomy for Non-Malignant Nodular Goiter
Authors Rabiee A, Salman M , Tourky M , Ameen M, Hussein A, Salman A , Labib S, Soliman AAZA, Shaaban HE , GabAllah G, Abouelregal T
Received 1 May 2021
Accepted for publication 24 May 2021
Published 10 June 2021 Volume 2021:14 Pages 2421—2425
DOI https://doi.org/10.2147/IJGM.S318398
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ahmed Rabiee,1 Mohamed Salman,2 Mohamed Tourky,3 Mahmoud Ameen,2 Ahmed Hussein,2 Ahmed Salman,1 Safa Labib,1 Ahmed Abdulkader Zaki Ali Soliman,4 Hossam El-Din Shaaban,5 Ghada GabAllah,6 Tarek Abouelregal1
1Internal Medicine Department, Kasralainy School of Medicine, Cairo University, Cairo, Egypt; 2General Surgery Department, Kasralainy School of Medicine, Cairo University, Cairo, Egypt; 3Great Western Hospital, NHS Foundation Trust, Swindon, UK; 4Lancashire Teaching Hospital, NHS Foundation, Preston, UK; 5Gastroenterology and Hepatology, National Hepatology and Tropical Medicine Research Institute, Cairo, Egypt; 6Medical Biochemistry Department, Faculty of Medicine, Menoufia University, Menoufia, Egypt
Correspondence: Mohamed Salman
General Surgery Department, Kasralainy School of Medicine, Cairo University, Cairo, Egypt
Email [email protected]
Mohamed Tourky
Great Western Hospital, NHS Foundation Trust, Marlborough Road, Swindon, SN3 6BB, UK
Email [email protected]
Objective: The study aimed to assess antithyroid antibodies in patients with benign thyroid masses and the effect of total thyroidectomy on the antibodies titers.
Patients and Methods: This is a retrospective work of 112 cases managed with total thyroidectomy with positive antithyroid peroxidase antibodies (TPO-Ab), anti-thyroglobulin antibodies (Tg-Ab), or both. All patients were euthyroid before surgery. Thyroid function tests and thyroid antibodies levels were measured before and 6 and 12 months after surgery.
Results: Histopathological evaluation revealed Hashimoto thyroiditis (47.3%), colloid nodules (22.3%), and lymphocytic thyroiditis (30.4%). All patients were TPO-Ab positive, while 96 patients (85.7%) were Tg-Ab positive before surgery. There was no considerable change in TPO-Ab and Tg-Ab after surgery (p = 0.817, and p=0.560, respectively). Also, there was no significant difference between the three histopathological diagnoses in the levels of TPO-Ab (p = 0.086) or Tg-Ab (p = 0.673).
Conclusion: Antithyroid antibodies are not valuable markers for diagnosis or prognosis of benign thyroid diseases subjected to total thyroidectomy. We do not recommend their use beyond supporting evidence of the possibility of the autoimmune nature of the illness if other criteria are confirmed.
Keywords: antithyroid antibodies, total thyroidectomy
Introduction
Thyroid peroxidase (TPO) is the critical thyroid enzyme for iodination and coupling of tyrosine residues in thyroglobulin to synthesize thyroid hormone.1 Anti-TPO antibodies are found in 90–95% of autoimmune thyroid diseases (AITD) patients and 10–15% of non-AITD patients.2 Anti-TPO antibodies in euthyroid individuals have no blocking TPO activity or interference with the blocking activity of anti-TPO antibodies from AITD patients.3 In contrast, anti-TPO antibodies from AITD patients can damage thyrocytes and inhibit enzymatic activity.4 Thyroglobulin (Tg) is a large glycoprotein containing three molecules of T4 and only 0.3 molecules of T3. Antibodies against Tg can be induced by significant destruction of the thyroid gland.5 Anti-TPO antibodies are more common than anti-Tg antibodies and more indicative of thyroid disease.6
Antithyroid antibodies are considered a sensitive marker of autoimmune thyroid diseases.7 However, these antibodies can be detected in 5% to 27% of the general population.8
The study aimed to assess the relation between thyroid autoantibodies and histopathological findings and the effect of total thyroidectomy on the auto-antibodies titers in patients with benign thyroid masses.
Patients and Methods
This prospective study included 112 patients managed with total thyroidectomy in Kasralainy Hospital, Cairo University between May 2016 and 2018. All methods were carried out in accordance with the declaration of Helsinki.
The study protocol was approved by the Institutional Review Board of Cairo University Hospitals. Informed consent was obtained from all subjects included in the study.
All patients presented to the endocrine and metabolism outpatient clinic complaining of nodular thyroid swelling that was proved to be non-malignant. Patients who were thyrotoxic or on thyroxine, on antithyroid drugs, steroids, or immunosuppressive drugs were excluded.
All included patients have positive anti-TPO ab with or without positive anti-TG ab.
All patients are euthyroid before surgery. In the department of surgery, all patients were subjected to total thyroidectomy after proper pre-operative preparation. Thyroidectomy was done for cosmetic purposes, to alleviate pressure symptoms, or for suspected malignancy. Operations were done using a standard transverse neck incision. Dissection was done, taking care not to injure parathyroid glands or recurrent laryngeal nerve. Suction drain insertion was performed when indicated.
Weight-based L-thyroxin(1.4–1.6 microgram/kg) is prescribed to all patients postoperatively with dose adjustment based on target TSH level.
All patients were subjected to throughout history taking, general and local examination. Laboratory assessment included TSH, freeT4, T3, antithyroid peroxidase (TPO-Ab), and anti-thyroglobulin (Tg-Ab). All patients were assessed with ultrasonography of the neck region.
Anti-TPO-Ab levels > 40 IU/mL were considered TPO-Ab-positive, and those with Tg-Ab levels >20 IU/mLwere considered Tg-Ab-positive9
Antibody-negative patients were excluded from the study.
Some patients (n=55) (solitary, isthmic, or dominant nodules with suspicious criteria) had fine-needle aspiration cytology (FNAC) of the thyroid nodule.
Thyroidectomy specimens were subjected to histopathological examination using H and E stains. Both FNAC and postoperative samples are examined at Kasralainy pathology department.
Postoperatively, laboratory assessment was repeated after 6 and 12 months. Investigations included TSH, freeT4, T3, TPO-Ab, and Tg-Ab. Patients with TPO-Ab levels > 40 IU/mL were considered TPO-Ab-positive, and those with Tg-Ab levels >20 IU/mL were considered Tg-Ab-positive.9
Statistical Methods
Statistical analysis was done using IBM© SPSS© Statistics version 22 (IBM© Corp., Armonk, NY, USA). Numerical data were expressed as mean and standard deviation or median and range as appropriate. Qualitative data were expressed as frequency and percentage. A Chi-square test was used to examine the relationship between qualitative variables. For quantitative data, a comparison between two groups was made using an independent sample t-test or Mann–Whitney test. Comparison between 3 groups was made using ANOVA test or Kruskal–Wallis test followed by the appropriate post-hoc test. Comparison of repeated measures was made using Friedman test followed by Wilcoxon signed-ranks test. A p-value < 0.05 was considered significant.
Results
The age of the patients ranged from 24 to 52 years, with a mean of 37.2±6.8 years. The male-to-female ratio was 1:3.7. The results of FNAC and postoperative histopathological examination are shown in Table 1. FNAC was acellular in 5 cases. In the remaining 50 patients, FNAC ultimately agreed with surgical specimen examination to diagnose colloid nodules. The main difference was in detecting lymphocytic infiltration in 40% of patients with colloid nodules (Table 2). Ultrasound examination revealed solitary thyroid nodule (STN) in 48 patients (42.85%), multinodular goiters (MNG) in 64 (57.15%).
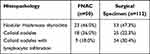 |
Table 1 Histopathological Findings of FNAC and Examination of Surgical Specimens |
 |
Table 2 Relation Between FNAC Diagnosis and Surgical Specimen Examination in 50 Patients |
Table 3 shows the baseline thyroid function tests and antithyroid antibodies. All patients were TPO-Ab positive, while 96 patients were Tg-Ab positive (85.7%). Compared to baseline readings, there was no significant change of TSH after surgery. On the other hand, free T4 increased significantly 12 months after surgery compared to baseline (p < 0.001). There was no significant change in T4 after six months compared to baseline (p = 0.145). Free T3 increased significantly six months after surgery compared to baseline (p = 0.009). By 12 months after surgery, free T3 returned near the baseline reading (p = 1.000). There was no significant change in the two autoantibodies after surgery (Table 4).
 |
Table 3 Baseline Thyroid Function Tests and Levels of Antithyroid Antibodies |
 |
Table 4 Baseline Thyroid Function Tests and Levels of Antithyroid Antibodies |
As shown in Table 5, there was no significant difference between the three histopathological diagnoses in the levels of TPO (p = 0.086) or TGO (p = 0.673). Postoperative hypocalcemia was observed in 3 patients, while unilateral recurrent laryngeal nerve injury occurred in 2 patients.
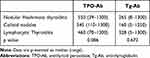 |
Table 5 Baseline Levels of Antithyroid Antibodies in Different Histopathological Diagnoses |
Discussion
The results of this study demonstrated that the levels of TPO-Ab and Tg-Ab were relatively high in the majority of the studied group with no significant differences between the three diagnoses (Nodular Hashimoto thyroiditis, colloid nodules, and lymphocytic thyroiditis). One year after total thyroidectomy, there was no substantial change in the levels of both TPO-Ab and Tg-Ab. Therefore, the two autoantibodies did not have a diagnostic or prognostic significance in the current series of benign nodular thyroid diseases.
Increased levels of antithyroid antibodies were linked to the diagnosis of autoimmune thyroid diseases (AITD).1 It is also detected in 10–15% of non-AITD patients.2 Hashimoto thyroiditis is usually defined as the presence of serum thyroid autoantibodies which are correlated with intraglandular lymphocytic infiltrate.3 The presence of thyroid antibodies in serum was correlated well with lymphocytic infiltration.4,5 Also, a good correlation was found between the level of antibodies and the severity of thyroiditis histologically.6
However, thyroid antibodies have been detected in population surveys and patients with extrathyroid diseases. TPO-Abs were detected in 6.8% and Tg-Ab in 2% of a sample of 2799 people in the Whickham study in the UK.7 Data from the National Health and Nutrition Examination Survey from the USA showed TPO-Ab in 13% and Tg-Ab in 11.5% of the examined sample of 17,353 people.8 A more recent population study in Tehran reported TPOAb positivity in 12.8% of their model, with a higher prevalence among women.9 This variation may be attributed to genetic and environmental factors as iodine intake or the type of antibody assays used in different studies.10 TPO-Abs are frequently detected in pregnant women.11,12 TPO-Ab positivity is related to adverse pregnancy outcome as miscarriage, premature delivery and low birth weight.13–16
In patients with autoimmune thyroid disease, Tg-Ab and TPO-Abs appear to increase due to thyroid inflammation. This is evidenced by their polyclonality and their failure to induce disease when transferred to animal models.3 In animal models, thyroid antibodies develop spontaneously without a definite stimulus.17 In humans, it is not clear how these antibodies are induced. However, epidemiological studies revealed valuable observations. Previous studies demonstrated that thyroid antibodies are not common in children. Female gender and puberty are strongly associated with thyroid antibody development.18,19 The autoantibodies showed a tendency to increase with age.20 It was shown that 21% of women of the Whickham cohort coveted to thyroid antibody positivity around the age of menopause.21 Increased titers were associated with increasing age.22
The two critical findings of the current study were increased antithyroid antibodies irrespective of the nature of the disease and the non-significant effect of surgery on the antibody levels. These results indicate a lack of diagnostic value of TPO-Ab and Tg-Ab for differentiating AITD and non-AITD in this series. Colloid nodule with no evidence of thyroid inflammation was the diagnosis of 38% of cases in this series. In these patients, TPO-Ab and Tg-Ab were as high as in cases of Hashimoto and lymphocytic thyroiditis. The two antibodies were not valid as markers of the effect of surgery, as no significant change was associated with surgery. It is not uncommon in clinical practice to ask frequently for these markers. Some physicians may think that these antibodies values may add or change their management plan.
According to our results, this practice of overusing these ancillary investigations is not so beneficial and may distract the physicians and constitute a financial burden over the health system without a tangible impact on the treatment of patients.
Based on these findings and the literature evidence of the presence of antithyroid antibodies in healthy people, we can conclude that antithyroid antibodies are not valuable markers for diagnosis or prognosis of benign nodular thyroid diseases subjected to total thyroidectomy. We do not recommend their use in nodular goiter beyond being and supportive evidence of the possibility of autoimmune nature of the illness if other criteria are confirmed.
Acknowledgment
Published as preprint Research Square, doi: 10.21203/rs.3.rs-79479/v1 (https://creativecommons.org/licenses/by/4.0/). No significant changes have been made since preprint.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mondal S, Raja K, Schweizer U, Mugesh G. Chemistry and biology in the biosynthesis and action of thyroid hormones. Angew Chem Int Ed Engl. 2016;55:7606–7630.
2. de Carvalho GA, Perez CLS, Ward LS. The clinical use of thyroid function tests. Arq Bras Endocrinol Metabol. 2013;57:193–204. doi:10.1590/s0004-27302013000300005
3. Kohno Y, Yamaguchi F, Saito K, Niimi H, Nishikawa T, Hosoya T. Anti-thyroid peroxidase antibodies in sera from healthy subjects and from patients with chronic thyroiditis: differences in the ability to inhibit thyroid peroxidase activities. Clin Exp Immunol. 1991;85:459–463. doi:10.1111/j.1365-2249.1991.tb05749.x
4. McLachlan SM, Rapoport B. Autoimmune response to the thyroid in humans: thyroid peroxidase--the common autoantigenic denominator. Int Rev Immunol. 2000;19:587–618. doi:10.3109/08830180009088514
5. Fröhlich E, Wahl R. Thyroid autoimmunity: role of anti-thyroid antibodies in thyroid and extra-thyroidal diseases. Front Immunol. 2017;8:521. doi:10.3389/fimmu.2017.00521
6. Balucan FS, Morshed SA, Davies TF. Thyroid autoantibodies in pregnancy: their role, regulation and clinical relevance. J Thyroid Res. 2013;2013:182472.
7. Iddah MA, Macharia BN. Autoimmune thyroid disorders. ISRN Endocrinol. 2013;2013:509764. doi:10.1155/2013/509764
8. Melmed S, editor. Williams Textbook of Endocrinology.
9. Gardner DG, Greenspan FS, editors. Greenspan’s Basic & Clinical Endocrinology. Vol. 9. New York: McGraw Hill Medical; 2011.
10. Roth C, Scortea M, Stubbe P, et al. Autoimmune thyreoiditis in childhood – epidemiology, clinical and laboratory findings in 61 patients. Exp Clin Endocrinol Diabetes. 2009;105(Suppl S 04):66–69. doi:10.1055/s-0029-1211937
11. Lindberg B, Svensson J, Ericsson U-B, Nilsson P, Svenonius E, Ivarsson S-A. Comparison of some different methods for analysis of thyroid autoantibodies: importance of thyroglobulin autoantibodies. Thyroid. 2001;11(3):265–269. doi:10.1089/105072501750159697
12. Arai T, Kurashima C, Utsuyama M, Sawabe M, Ito H. Measurement of anti-thyroglobulin and antithyroid peroxidase antibodies using highly sensitive radioimmunoassay: an effective method for detecting asymptomatic focal lymphocytic thyroiditis in the elderly. Endocr J. 2000;47:575–582. doi:10.1507/endocrj.47.575
13. Tunbridge WM, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol. 1977;7:481–493. doi:10.1111/j.1365-2265.1977.tb01340.x
14. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T4, and thyroid antibodies in the United States Population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489–499. doi:10.1210/jcem.87.2.8182
15. Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The prevalence, incidence and natural course of positive antithyroperoxidase antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283. doi:10.1371/journal.pone.0169283
16. Pedersen IB, Knudsen N, Jørgensen T, Perrild H, Ovesen L, Laurberg P. Thyroid peroxidase and thyroglobulin autoantibodies in a large survey of populations with mild and moderate iodine deficiency. Clin Endocrinol (Oxf). 2003;58(1):36–42. doi:10.1046/j.1365-2265.2003.01633.x
17. La’ulu SL, Roberts WL. Second-trimester reference intervals for thyroid tests: the role of ethnicity. Clin Chem. 2007;53(9):1658–1664. doi:10.1373/clinchem.2007.089680
18. Yang X, Meng Y, Zhang Y, et al. Thyroid function reference ranges during pregnancy in a large Chinese population and comparison with current guidelines. Chin Med J. 2019;132(5):505–511. doi:10.1097/CM9.0000000000000051
19. Han L, Zheng W, Zhai Y, et al. Reference intervals of trimester-specific thyroid stimulating hormone and free thyroxine in Chinese women established by experimental and statistical methods. J Clin Lab Anal. 2018;32(4):e22344. doi:10.1002/jcla.22344
20. Korevaar TIM, Schalekamp-Timmermans S, de Rijke YB, et al. Hypothyroxinemia and TPO-antibody positivity are risk factors for premature delivery: the generation R study. J Clin Endocrinol Metab. 2013;98(11):4382–4390. doi:10.1210/jc.2013-2855
21. Chen L-M, Zhang Q, Si G-X, et al. Associations between thyroid autoantibody status and abnormal pregnancy outcomes in euthyroid women. Endocrine. 2015;48(3):924–928. doi:10.1007/s12020-014-0420-x
22. Han Y, Mao L-J, Ge X, et al. Impact of maternal thyroid autoantibodies positivity on the risk of early term birth: Ma’anshan Birth Cohort Study. Endocrine. 2018;60(2):329–338. doi:10.1007/s12020-018-1576-6
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
