Back to Journals » Drug Design, Development and Therapy » Volume 12
Anticancer activity of the intraperitoneal-delivered DFP-10825, the cationic liposome-conjugated RNAi molecule targeting thymidylate synthase, on peritoneal disseminated ovarian cancer xenograft model
Authors Iizuka K, Jin C, Eshima K, Hong MH, Eshima K , Fukushima M
Received 9 November 2017
Accepted for publication 4 January 2018
Published 29 March 2018 Volume 2018:12 Pages 673—683
DOI https://doi.org/10.2147/DDDT.S156635
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Video abstract presented by Kenzo Iizuka.
Views: 889
Kenzo Iizuka, Cheng Jin, Kokoro Eshima, Mei Hua Hong, Kiyoshi Eshima, Masakazu Fukushima
Division of Research and Development, Delta-Fly Pharma Inc., Tokushima, Japan
Introduction: Peritoneal disseminated ovarian cancer is one of the most difficult cancers to treat with conventional anti-cancer drugs and the treatment options are very limited, although an intraperitoneal (ip) paclitaxel has shown some clinical benefit. Therefore, treatment of peritoneal disseminated ovarian cancer is a highly unmet medical need and it is urgent to develop a new ip delivered drug regulating the fast DNA synthesis.
Methods: We developed a unique RNAi molecule consisting of shRNA against the thymidylate synthase (TS) and a cationic liposome (DFP-10825) and tested its antitumor activity and PK profile in peritoneally disseminated human ovarian cancer ascites models by the luciferase gene-transfected SCID mice. DFP-10825 alone, paclitaxel alone or combination with DFP-10825 and paclitaxel were administered in an ip route to the tumor-bearing mice. The TS expression level was measured by conventional RT-PCR. The anti-tumor activity and host survival benefit by DFP-10825 treatment on tumor-bearing mice were observed as resulting from the specific TS mRNA knock-down in tumors.
Results: DFP-10825 alone significantly suppressed the growth of SKOV3-luc tumore ascites cells and further extended the survival time of these tumor-bearing mice. Combination with the ip paclitaxel augmented the antitumor efficacy of DFP-10825 and significantly prolonged the survival time in the tumor-bearing mice. Short-hairpin RNA for TS (TS shRNA) levels derived from DFP-10825 in the ascetic fluid were maintained at a nM range across 24 hours but not detected in the plasma, suggesting that TS shRNA is relatively stable in the peritoneal cavity, to be able to exert its anti-tumor activity, but not in blood stream, indicating little or no systemic effect.
Conclusion: Collectively, the ip delivery of DFP-10825, TS shRNA conjugated with cationic liposome, shows a favorable antitumor activity without systemic adverse events via the stable localization of TS shRNA for a sufficient time and concentration in the peritoneal cavity of the peritoneally disseminated human ovarian cancer-bearing mice.
Keywords: DFP-10825, thymidylate synthase, short-hairpin RNA, cationic liposome, ip delivery, intraperitoneal dissemination, ovarian cancer
Introduction
Peritoneal carcinomatosis (PC), caused by advanced abdominal malignancies, such as those of the ovarian and gastrointestinal (gastric and pancreatic) tracts, has an extremely poor prognosis in the world. Therefore, the development of specific intraperitoneal (ip) drugs using newly emerging cytotoxic and molecular targeted compounds, or new drug delivery systems is an urgent unmet need and essential to improve the efficacy, without severe side effects, of the ip therapy in patients.1 In ovarian cancer, the recurrence rate in advanced stage III–IV patients is estimated over 85% and their long-term prognosis is very poor.2,3 Therefore, control of recurrent ovarian cancer in the abdominal cavity is thought to be one of the best ways of increasing survival rate in ovarian cancer. At present, ip chemotherapy with paclitaxel plus cisplatin in addition to intravenous paclitaxel and cisplatin has attained the most prolonged median survival time (MST) in patients with PC.4,5 However, the problem with the therapy is substantially toxicity which bone marrow suppression associated with severe leukopenia and thrombocytopenia in the ip chemotherapy group, and it is recommended to add a reduction of the toxicity from just ip injection since it could be due to the combination of iv administration. Accordingly, such an ip approach with taxane and platinum drugs has not yet become routine practice.6 To improve the outcome in patients with peritoneal disseminated ovarian cancer, new drugs with low toxicity focused on the ip administration are being developed from a viewpoint of inhibition of target molecules in disseminated ovarian cancer.7–10
Regarding the rapidly growing ovarian cancer cells, there are several pieces of evidence showing that thymidylate synthase (TS), an important rate-limiting enzyme in tumoral DNA biosynthesis, is highly expressed in both original and metastatic (peritoneal) ovarian carcinomas.11–14 The TS expression level (in both protein and gene expression levels) in tumor has been suggested as the key determinant for the efficacy, and the insensitive and resistant for TS-targeting drugs including 5-FU and pemetrexed was innervated by a status of the high and elevated levels of TS expression which target the regulation of post-transcription of TYMS expression. Therefore, a monotherapy to control the TYMS expression and/or combination with antagonists of TS would be a better approach for the antitumor activity.
In 2011, Kadota et al reported that when intratumorally administered, TS-inhibiting vector downregulated the expression of TS mRNA and resultantly overcame the resistance to 5-FU in human colon cancers.15 Based on this evidence, Abu Lila et al tried to develop a liposome-based drug delivery system containing RNAi for TS instead of adenovirus vector and evaluated the efficacy of PEG-coated RNAi-liposome by intravenous administration in human colorectal cancer cells, and also malignant pleural mesothelioma cells, in vitro and in vivo.16,17
Because of instability of the bare RNAi molecule or its conjugate with liposome in the blood stream following an intravenous injection, and the requirement of rigorous controlling for particle size of RNAi-liposome (up to 100 nm), local administration of the RNAi-liposome is rather favorable for locally advanced malignant tumors. Abu Lila et al showed that the downregulation of TS by RNAi molecules enhanced the antitumor activity of pemetrexed, the TS inhibitor, in an orthotopic mesothelioma model in mice.18 We are interested in evaluating the antitumor activity of the ip injection of short-hairpin RNA for TS (TS shRNA) conjugated with liposome further in peritoneal disseminated human ovarian cancer; the more common and unmet medical need.
The present study describes the pharmacology and pharmacokinetic/pharmacodynamic profile of DFP-10825, the TS shRNA-cationic liposome (lipoplex), in a peritoneal disseminated human ovarian cancer (SKOV3-luc) xenograft in mice.
Materials and methods
Materials
TS shRNA (Figure 1) for clinical use by scaling-up synthesis was obtained from Nitto-Denko Avecia Biotechnology Inc. (Milford, MA, USA). Paclitaxel was purchased from Wako Pure Chemical Inc. (Tokyo, Japan). Dioleoylphosphatidylcholine (DOPC) and dioleoylphosphatidylethanolamine (DOPE), and O,O′-ditetradecanoyl-N-(α-trimethyl ammonioacetyl) diethanolamine chloride (DC-6-14), for preparation of cationic liposome (called lipoplex) were obtained from NOF Inc. (Tokyo, Japan) and Nippon Fine Chemicals Inc. (Hyogo, Japan), respectively. All other chemicals and biological products of analytical grade were commercially available.
Tumor cells
Human ovarian cancer SKOV3 cells were purchased from DS Pharma Biomedical Co. (Osaka, Japan) and maintained in vitro as a monolayer culture in a Roswell Park Memorial Institute (RPMI)-1640 medium supplemented with heat-inactivated fetal calf serum containing penicillin (100 U/mL), streptomycin (100 μg/mL) and L-glutamine (2 mM). SKOV3 cells expressing firefly luciferase (SKOV3-luc cells) were generated by stable transfection with the firefly luciferase gene (pGL3 basic plasmid; Promega, Madison, WI, USA) in our laboratory and maintained in the same medium until used in in vivo experiments.
Preparation of cationic liposome (lipoplex)
Cationic liposome composed of DOPE:DOPC:DC-16-4 (3: 2: 5 molar ratio) was prepared by the method of Abu Lila et al as described previously.18 This lipoplex was not constructed as a PEG modification.
Preparation of TS shRNA-lipoplex (DFP-10825)
For the preparation of TS shRNA/cationic liposome complex (TS shRNA-lipoplex, DFP-10825, Figure 1), TS shRNA and cationic liposome were mixed at a molar ratio of 2,000/1 (lipid:shRNA =2,000:1), and the mixture was vigorously vortexed for 10 min at room temperature to form TS shRNA-lipoplex (DFP-10825). The free TS shRNA in the formulation (TS shRNA-lipoplex, DFP-10825) of 2.0 mg/kg (as shRNA) was checked by agarose gel electrophoresis. As TS-shRNA remained stable in the formulation, no free TS-shRNA was detected up to day 3 after preparation (Figure 1). The mean diameter and zeta potential of the DFP-10825 was 395±32 nm and 31±2 mV (n=3), respectively, as determined with an NICOMP 370 HPL submicron particle analyzer (Particle Sizing System, Santa Barbara, CA, USA). The concentration of phospholipids was confirmed by colorimetric assay.19 The absence of free (un-bound) TS shRNA in prepared DFP-10825 was evaluated by electrophoresis performed on 2% agarose gel.
Animals and in vivo intraperitoneal orthotopic implantation model
Six- to 8-week-old male SOD/SCID mice were purchased from CLEA Japan IncHFK Animal Technology Co, Ltd. (Beijing, People’s Republic of China) and were fed with a sterilized diet and autoclaved water ad libitum. Mice were kept in laminar units throughout the experiments.
The care and treatment of the animals were in accordance with the guidelines issued by the Science and International Affairs Bureau of the Japanese Ministry of Education, Science, Culture and Sports. The experimental protocol was performed after approval from the Institutional Animal Ethical Committee in Delta-Fly Pharma, Inc., (Tokushima, Japan).
Groups of 8–10 SCID mice were used. Intraperitoneally disseminated SKOV3-luc human ovarian cancer models were prepared by ip injection of cultured SKOV3-luc cells (5–10×106 cells/mouse) into mice, and bioluminescence signals in the tumor-transfected mice were visualized using an in vivo imaging system (IVIS, Xenogen, CA, USA). The fluorescence images were acquired using an exposure time of 1/8 second.
Therapeutic efficacy of DFP-10825 in an intraperitoneal disseminated SKOV3-luc cancer model
On day 7 of the peritoneal implantation of SKOV3-luc tumor cells, DFP-10825 (0.5–2 mg/kg as TS shRNA) was administered to the ip cavity in a schedule of every 3rd day (q3d) for two or four doses. In a combination experiment, paclitaxel at a dose of 15 mg/kg was intraperitoneally administered to the tumor-bearing mice in the same way already described in addition to the DFP-10825 treatment. Tumor bioluminescence imaging (BLI) were checked once a week and body weight twice a week. Antitumor activity of DFP-10825, paclitaxel or their combination was evaluated based on the mean BLI value in the vehicle control and drug-treated groups as follows:
|
Survival time of all animals was followed up and the MST was calculated for each group. Increase in life span (ILS) was calculated by formula: (MST of treatment group/MST of the control group − 1) ×100%, and was expressed as the percentage of increase over the life span of the control animals.
Determination of TS expression levels (TS mRNAs) in SKOV3-luc human ovarian cancer peritoneal disseminated model
TYMS expression (TS mRNA) in ovarian tumor ascites cells and disseminated solid tumors was determined by real-time quantitative RT-PCR as described by Kadota et al15 and Fujiwara et al.20 Briefly, peritoneal ascetic tumor cells and disseminated tumors were collected from SKOV3-luc-bearing mice and their total RNAs were extracted using RNAiso plus (TAKARA Bio Inc, Shiga, Japan). In this procedure, RNaseZap RNase decontamination solution was used throughout to remove possible RNase contamination on benchtop and instruments. First-strand cDNA synthesis was performed with 5–10 μg of total RNA using a cDNA synthesis kit (Amersham Bioscience, Piscataway, NJ, USA). To quantitatively measure the TYMS expression, TaqMan real-time quantitative PCR was performed with the ABI PRISM 7700 sequence detection system (Applied Biosystems, Foster City, CA, USA). The primers and probes for TS were from Taqman gene expression assay mix (assay ID Hs00426586_m1, lot# 1312626; PCR product size 250 rxns; Thermo Fisher Scientific, Waltham, MA, USA). Each sample was run in triplicate. The comparative threshold cycle method (Applied Biosystems) was used to calculate the gene expression in each sample relative to the value observed in control (no drug) tumor cells using 18S rRNA (Taqman gene expression assay kit, ID: Hs99999901_s1 18S, size 250 rxns; Thermo Fisher Scientific) as a control for the normalization among samples. RNA samples isolated from three mice were evaluated.
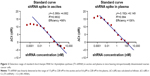
Determination of TS shRNA by stem-loop RT-PCR
After ip administration of DFP-10825 (TS shRNA-lipoplex), ascetic fluids and blood samples were isolated from SKOV3-luc-bearing mice, and 100 μL of the 2x denaturing solution and 200 μL of acid phenol-chloroform were added to 100 μL of each isolated sample solution. After vortexing for 60 sec and subsequent centrifugation at 10,000× g for 5 min, aliquots (about 100 μL) of aqueous phase were added to 100% ethanol (125 μL), mixed well, moved to the filter cartridge and then centrifuged at 10,000× g. The filter cartridge was washed with the mRNA wash solution (700 μL) and then centrifuged. This procedure was repeated three times and subsequently RNA solution from the washed filter cartridge was extracted with nuclease-free water (100 μL) and kept at −80°C until use in the reverse transcription reaction. For TS shRNA, 3 μL of stem-loop RT primer (GTCGTATCCAGTGCAGGGTCCGAGGTATTCGCACTGGATACGACAAAGTAA, HB1404288132; Thermo Fisher Scientific) was added to 5 μL of isolated RNA solution, and incubated at 85°C for 5 min and at 60°C for 5 min to denature the RNA. For 18S rRNA as a reference standard, 3 μL of random 9 mers (12.5 μmol/L) was added to the RNA solution (5 μL) and treated in the same way. After that, real-time RT-PCR for TS shRNA and 18S rRNA was performed using TaqMan gene expression kits from Thermo Fisher Scientific, respectively. The TaqMan gene expression kit contains 10 μL Master Mix, 4 μM probe, each 4 μM forward and reverse primer and RT reaction mixture for TS shRNA, and 10 μL Master Mix, small RNA assay for 18S rRNA (20X), nuclease-free water and RT reaction mixture for 18S rRNA. The quantitative PCR was performed with Stratagene MX3005P PCR System (50°C for 2 min and 95°C for 10 min in 1 cycle and then 95°C for 15 sec and 60°C for 60 sec in 40 cycles). To analyze the data obtained, the threshold was calculated by MXpro software automatically using the default setting Export Ct value to Excel. Data of each sample were normalized by using the following formula: ΔCt = average Ct (TS shRNA) − average Ct (18S rRNA). Levels of TS shRNA in ascites and blood samples were calculated on the standard curve. By this stem-loop RT-PCR method, TS shRNA was linearly detected at the range of from 15 pM to 228 nM in the ascites and at the range of from 0.6 pM to 228 nM in the blood, respectively, as shown in Figure 2.
Statistical analysis
The differences between the mean BLI values for comparing groups were analyzed for significance using the one-way analysis of variance (ANOVA). P<0.05 was considered statistically significant. The differences between MSTs for comparing groups were analyzed for significance using Wilcoxon test. P<0.05 was considered statistically significant.
Results
Dose dependent tumor growth inhibition by DFP-10825 in peritoneal SKOV3-luc tumor-bearing ascites xenografts in mice
After SKOV3-luc ovarian cancer cells were intraperitoneally inoculated into mice, DFP-10825 of 0.5, 1 or 2 mg as TS shRNA/kg was intraperitoneally administered q3d for four doses from 7 days after the inoculation, and the tumor growth level was monitored in the BLI in each group when it reached ~50 photons ×107. As presented in Figure 3, DFP-10825 at the range of 0.5–1 mg/kg inhibited dose dependently the growth of ascetic tumor, measured as the BLI signal throughout the treatment period, from days 7 to 18. The TGI by DFP-10825 at 1 mg/kg reached a plateau, since the next dose (2 mg/kg), and the highest dose tested in the model, did not result in further augmented efficacy. The tumor wet weight was measured at the end of the experiment, and the consistency of the BLI signals and the tumor wet weight were confirmed (data not included). To assess the tolerability or toxicity for the ip delivery of DFP-10825, body weight was measured in parallel in this model and no body weight change with DFP-10825 treatment was observed compared to that in the vehicle control group. These data indicate that DFP-10825 as monotherapy against the TS RNA expression is an effective approach for peritoneal disseminated ovarian cancer without any change in body weight for the host. A typical BLI signal in SKOV3-luc-bearing mice is shown in Figure 4.
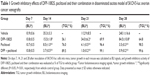
Antitumor effect of DFP-10825, paclitaxel and their combination on SKOV3-luc tumor ascites model
From day 7 after SKOV3-luc cells were inoculated into the ip cavity of mice, DFP-10825 (1 mg/kg as TS shRNA), paclitaxel (15 mg/kg) and their combination were intraperitoneally administered q3d ×2 times. BLI signals in tumor-bearing mice of each group during the therapeutic periods (days 7–28) are illustrated in Figure 4. BLI signals in drug-treated mice were found to visually decrease compared with those in the vehicle control group. As shown in Figure 5, the treatment with combination of DFP-10825 (as TS shRNA) and paclitaxel resulted in significant TGI, and decreased luciferase-derived BLI signals in mice (in particular, the additive effect was shown better in a log scale). Based on monitored BLI signals in each mouse of each group, antitumor activity (% of TGI) of DFP-10825, paclitaxel and their combination was calculated and is presented in Table 1. DFP-10825 (1 mg/kg as TS shRNA) resulted in significant (P<0.05) TGI with 56%, 70% and 65% on days 14, 21 and 28, respectively. In this tumor model, ip paclitaxel also showed excellent antitumor activity with TGI of 76%, 96% and 98% on days 14, 21 and 28, respectively. Due to the potent antitumor activity of paclitaxel alone, addition of DFP-10825 to paclitaxel only resulted in a little augmentation of antitumor activity with about 89%, 99% and 100% of TGI on days 14, 21 and 28, respectively.
  | Figure 5 Growth inhibitory effect and body weight change of DFP-10825, paclitaxel and their combination on intraperitoneal disseminated SKOV3-luc tumor xenografts in mice. |
No body weight change in DFP-10825 groups compared to that of the control group was evident. Interestingly, no body weight change in the combination treatment was observed either (slightly increased body weights, around 5%, over the end of the treatment period). Accordingly, in this SKOV3-luc model, it was strongly suggested that DFP-10825, paclitaxel and their combination could be a new therapy option for patients with peritoneal disseminated human ovarian cancer and well tolerated for both single and combination therapies.
Life-prolonging effect in SKOV3-luc-bearing mice by the treatment with DFP-10825, paclitaxel and their combination
After the drug treatments, survival time in mice (n=10) was monitored for 100 days after the tumor implantation. As shown in Table 2, the MST for vehicle control, DFP-10825, paclitaxel and DFP-10825 plus paclitaxel groups was 29, 34, 62 and 83 days, respectively, and ILS in DFP-10825, paclitaxel and their combination groups was 17.2% (P=0.007), 113.8% (P<0.01) and 186.2% (P<0.01), respectively. It is worth pointing out that the combination treatment with DFP-10825 and paclitaxel showed an additive effect in parallel with that of the inhibition of tumor growth (Figures 4 and 5). This further supports the notion that the combination therapy can be a better option as it completely controls the TS activity at both transcriptional and protein levels.
TS shRNA levels in ascites and blood for post-intraperitoneal injection of DFP-10825 in SKOV3-luc tumor-bearing ascites mice
The ip delivered DFP-10825 sufficiently inhibited the growth of intraperitoneally disseminated SKOV3-luc cells in mice and resultantly prolonged the survival of the tumor-bearing mice. To confirm the specificity and PK profile of DFP-10825 (TS shRNA) in peritoneal disseminated tumor cells with ascites, it is important to detect TS shRNA level in the peritoneal ascites and bloodstream of mice post-injection of DFP-10825. After administration of DFP-10825 (1 mg/kg as TS shRNA), TS shRNA contents in ascites and blood of the tumor-bearing mice (n=3) were measured at 2, 4, 8 and 24 hours, as shown in Figure 6. Throughout 24 hours after the administration, the level of TS shRNA could be detected in the ascetic fluids, and TS shRNA concentration in ascites samples was 4.26±1.00, 3.85±0.78, 1.79±0.51 and 0.68±0.24 nM at 2, 4, 8 and 24 hours post-dosing, respectively. The concentration of ascites at pre-dosing was 2.23±0.54 mL and after 24 hours from the shRNA dosing was 0.61±0.49 mL. By striking contrast, 0.005±0.002 nM of TS shRNA was detected in the bloodstream only at 2 hours post-dosing. These results indicate that TS shRNA after the local delivery of DFP-10825 reached a sufficient concentration to control the TS mRNA expression and maintained at a nM range in the ascites up to 8 hours, without meaningful detection of it in the bloodstream. This supports the effectiveness and desirable PK profile for the local delivery system of DFP-10825 and further contributes to the specific activity via the downregulation of TS mRNA expression that results in the inhibition of ovarian cancer ascites cell growth while having few adverse events in accordance with the very limited systemic distribution.
Inhibition of TYMS expression in SKOV3-luc tumor ascites cells after ip administration of DFP-10825
To demonstrate mode of action of the specificity for the antitumor activity of DFP-10825 in SKOV3-luc tumor ascites cells, the expression of TS mRNA in tumor cells with ascites was investigated at 24 hours after treatment with DFP-10825. As presented in Figure 7, DFP-10825 significantly (P<0.05) downregulated the expression of TS mRNA, while paclitaxel did not affect the expression. The suppression of TS mRNA expression (P<0.1) in the combination therapy appears to be due to the action of DFP-10825. Accordingly, it is suggested that the ip administration of DFP-10825 inhibits the growth of disseminated ovarian cancer ascites cells in the peritoneal cavity via downregulation of the TS mRNA expression.
Discussion
Ovarian cancer is the most lethal malignancy in the field of gynecology, and peritoneal dissemination is the most frequent type of metastasis of such a type of advanced cancer, which results in a poor prognosis, with a 5-year survival rate of <25%.21 In addition to systemic chemotherapy including taxane and platinum drugs, ip chemotherapy with cytotoxic drugs for the peritoneal carcinomas of ovarian cancer suggested promising clinical effects.22 Furthermore, a combination of systemic and ip chemotherapy administration of paclitaxel and cisplatin (CDDP) confers a significant survival benefit upon patients with optimally debulked ovarian cancer compared with systemic administration alone.6 Armstrong et al4 reported that the median survival was prolonged from 49.7 months for systemic paclitaxel + CDDP arm to 65.6 months for a combination of systemic and ip paclitaxel + CDDP regimen. However, there was substantially more toxicity in the combination regimen including severe leukopenia, thrombocytopenia and pain. Accordingly, new agents or novel therapeutic methods focused on disseminated ascetic tumors existing in the peritoneal cavity are urgently needed to further improve the survival rate in a better tolerated fashion for the limited therapeutic options to peritoneal disseminated ovarian cancer patients.
We attempted to apply the TYMS-targeted specific RNAi molecule,15 one of the important rate-limiting enzymes of DNA biosynthesis in rapidly growing tumor cells, to treat peritoneal disseminated ascites tumor cells. For this, TS shRNA (Figure 1) was conjugated with cationic liposome17,18 (lipoplex, named as DFP-10825) and intraperitoneally injected to disseminated SKOV3-luc human ovarian cancer xenograft model in mice. As presented in Figures 1 and 2, DFP-10825 in the range of 0.5–2 mg/kg as the TS shRNA content strongly inhibited the growth of SKOV3-luc ascites cancer cells in the peritoneal cavity of mice. The same as other malignant cancers such as gastric, colorectal, pancreatic and non-small cell lung cancer, TS expression in ovarian cancer is one of prognostic factors,11–14 and therefore its regulation would lead to improved outcome of a therapy for ovarian cancer. Our data clearly show that regulation of TYMS (TS RNA) by TS shRNA molecule including DFP-10825 not only inhibited the tumor growth but also improved patient’s outcome. To further confirm the pharmacokinetic/pharmacodynamics of such antitumor activity of DFP-10825 as TS shRNA upon peritoneal disseminated SKOV3-luc ovarian cancer cells, we investigated the concentration of TS shRNA in the ascites and bloodstream of mice following the ip administration of DFP-10825 on day 28 after inoculation of SKOV3-luc ascites cancer cells. As shown in Figure 6, when 1 mg/kg of TS shRNA was injected, TS shRNA level was found to be sustainable in the range of a single digit nM in the ascites for a long time (over 24 hours), but not in the bloodstream. This level of TS shRNA is indeed sufficient for downregulation of TYMS expression consistent with the in vitro inhibition (IC50, 2.5 nM) of tumor cell viability reported by Abu Lila et al.16 Also, we demonstrated that a single dose of 1 mg/kg TS shRNA significantly (P<0.05) downregulated the expression of TS mRNA in SKOV3-lu ascites cancer cells in the peritoneal cavity in an in vivo system, as shown in Figure 7.
In clinical practice, the intraperitoneally dosing paclitaxel in combination with a systemic delivery of chemotherapeutic agents, including paclitaxel, has been frequently used for the treatment of peritoneal disseminated ovarian cancer patients. Therefore, we evaluated a potential combination opportunity of DFP-10825 with paclitaxel on the anticancer activity and side effects in the same SKOV3-luc tumor model. As presented in Figures 4 and 5, the combination of DFP-10825 with paclitaxel significantly enhanced the antitumor activity in the disseminated SKOV3-luc tumors compared to that of a single agent of DFP-10825 or paclitaxel. In parallel, the survival rate in the SKOV3-luc tumor-bearing ascites mice was significantly (P<0.01) prolonged to 186% from 17.2% for DFP-10825 alone and 113.8% for paclitaxel alone. However, the host body weight change in the combination was neglectable. Accordingly, the ip administration of DFP-10825 in combination with local delivery of paclitaxel would provide a new ideal therapeutic option for treating peritoneal disseminated ovarian cancer patients who are sensitive or resistant to paclitaxel.
Recently, several nucleic acid-based drugs have been designed and developed for the treatment of cancers. These are mainly miRNAs or siRNAs that were coated (or conjugated) with cationic lipid, neutral lipid emulsion and amphoteric liposome,23 and are being extensively investigated in preclinical and clinical stages. For example, Let-7b and miR-34 both suspended in a neutral lipid emulsion, miR-29b conjugated with liposomes and miR-200c coated with an amphoteric liposome have been intravenously administered and evaluated in non-small cell lung cancer preclinical models and patients with non-small cell lung cancer.24–26 As a unique therapeutic delivery, miR-16-based mimic miRNA (named as TargomiRs) loaded to targeted bacterial mini cells has been delivered intravenously to cancer patients.27,28 Different from RNAi molecules, synthetic antisense-oligonucleotide targeting ribonucleotide reductase R2, a key enzyme in DNA synthesis, has also been investigated pre-clinically29 and clinically30,31 by the method of intravenous infusion for a long-term effect.
In general, nucleic acid-based molecules such as siRNA and miRNA are well known to be unstable in the bloodstream due to the rapid hydrolysis by nucleases, and therefore surfactants such as polyethylene glycol are attached to siRNA and miRNA conjugated with lipids to exhibit their sustained stability in the bloodstream. When pegylated DFP-10825 (TS shRNA-cationic liposome) was systemically administered, it sensitized malignant pleural mesothelioma xenografts.17 However, it is desirable to deliver such agents locally to be able to concentrate enough agent, as well as avoid any adverse events from the systemic delivery system. The peritoneal delivery of DFP-10825 for peritoneal disseminated ovarian tumor, is a good example of desired therapeutic outcomes with a wide therapeutic index, and this successful formulation for the delivery system which may be maintained with an effective concentration for a long period will pave a new path to further treatment options in patients with ovarian cancer. In addition, the delivery system can be extended to other PC like peritoneal disseminated human gastrointestinal (gastric and pancreatic) cancers and our preliminary data with the antitumor activity of ip delivered DFP-10825 in luciferase gene-transfected human gastric and pancreatic cancer xenograft models further confirmed such promising potential (a separate manuscript is being prepared and will be presented in detail later). We are planning to carry out a clinical trial of the ip DFP-10825 for patients with peritoneal disseminated ovarian cancer and also other cancers in the near future.
Conclusion
As a new approach to downregulate or inhibit the growth of peritoneal disseminated human ovarian cancer xenograft model, DFP-10825, the RNAi molecule for the TYMS (TS shRNA) conjugated with cationic liposome, was developed and administered intraperitoneally to the SKOV3-luc tumor-bearing ascites mice. DFP-10825 showed a dose-dependent antitumor activity in the range of 0.5–2 mg/kg as TS shRNA and significantly prolonged the survival rate of the tumor-bearing mice. Furthermore, co-intraperitoneal administration of DFP-10825 and paclitaxel further enhanced the antitumor activity over the efficacy of paclitaxel alone in this tumor model. When intraperitoneally administered, TS shRNA level in ascites but not in the bloodstream was stably maintained in the range of a single digit nM over several hours and subsequently did downregulate the expression of TS mRNA in the disseminated SKOV3-luc tumor-bearing ascites mice. The present study strongly suggests that the ip delivery of DFP-10825 would provide a new opportunity for improving the outcome of patients with peritoneal disseminated ovarian cancer.
Acknowledgment
The authors thank Dr Tatsuhiro Ishida, Professor of Tokushima University, for his detailed technical support of the liposome technology and Dr Chen-Long Huang (Kitano Hospital, Kyoto, Japan) and Dr Hiromi Wada, the emeritus professor of Kyoto University, for their helpful suggestion of the clinical application of this drug. The preliminary data of this paper was presented at the 12th France-Japan Drug Delivery Systems Symposium as a conference talk with interim findings, and the poster’s abstract was published in “Poster Abstracts” in the Annual Meeting 2017 of American Association for Cancer Research: Hyperlink with DOI: 10.1158/1538-7445.AM2017-5097 Published July 2017.
Disclosure
All authors are employees of Delta-Fly Pharma Inc. The authors report no other conflicts of interest in this work.
References
Kitayama J. Intraperitoneal chemotherapy against peritoneal carcinomatosis: current status and future perspective. Surg Oncol. 2014;23(2):99–106. | ||
Ozols RF, Bundy BN, Greer BE, et al; Gynecologic Oncology Group. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a gynecologic oncology group study. J Clin Oncol. 2003;21(17):3194–3200. | ||
McGuire WP, Hoskins WJ, Brady MF, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med. 1996;334(1):1–6. | ||
Armstrong DK, Bundy B, Wenzel L, et al; Gynecologic Oncology Group. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354(1):34–43. | ||
Jaaback K, Johnson N, Lawrie TA. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Syst Rev. 2011;(11):CD005340. | ||
Trimble EL, Alvarez RD. Intraperitoneal chemotherapy and the NCI clinical announcement. Gynecol Oncol. 2006;103(2 Suppl 1):S18–S19. | ||
Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25(33):5165–5171. | ||
Cannistra SA, Matulonis UA, Penson RT, et al. Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol. 2007;25(33):5180–5186. | ||
Banerjee S, Kaye SB, Ashworth A. Making the best of PARP inhibitors in ovarian cancer. Nat Rev Clin Oncol. 2010;7(9):508–519. | ||
Ledermann J, Harter P, Gourley C, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012;366(15):1382–1392. | ||
Suzuki M, Ohwada M, Tamada T, Tsuru S. Thymidylate synthase activity as a prognostic factor in ovarian cancer. Oncology. 1994;51(4):334–338. | ||
Look KY, Moore DH, Sutton GP, Prajda N, Abonyi M, Weber G. Increased thymidine kinase and thymidylate synthase activities in human epithelial ovarian carcinoma. Anticancer Res. 1997;17(4A):2353–2356. | ||
Fujiwaki R, Hata K, Nakayama K, Fukumoto M, Miyazaki K. Thymidylate synthase expression in epithelial ovarian cancer: relationship with thymidine phosphorylase expression and prognosis. Oncology. 2000;59(2):152–157. | ||
Wang C, Weng Y, Wang H, Shi Y, Ma D. Relationship between the expression of thymidylate synthase, thymidine phosphorylase and dihydropyrimidine dehydrogenase and survival in epithelial ovarian cancer. J Huazhong Univ Sci Technolog Med Sci. 2010;30(4):494–499. | ||
Kadota K, Huang CL, Liu D, Yokomise H, Haba R, Wada H. Combined therapy with a thymidylate synthase-inhibiting vector and S-1 has effective antitumor activity against 5-FU-resistant tumors. Int J Oncol. 2011;38(2):355–363. | ||
Abu Lila AS, Moriyoshi N, Fukushima M, et al. Metronomic S-1 dosing and thymidylate synthase silencing have synergistic antitumor efficacy in a colorectal cancer xenograft model. Cancer Lett. 2017;400:223–231. | ||
Abu Lila AS, Fukushima M, Huang CL, Wada H, Ishida T. Systemically administered RNAi molecule sensitizes malignant pleural mesotheliomal cells to pemetrexed therapy. Mol Pharm. 2016;13(11):3955–3963. | ||
Abu Lila AS, Kato C, Fukushima M, Huang CL, Wada H, Ishida T. Downregulation of thymidylate synthase by RNAi molecules enhances the antitumor effect of pemetrexed in an orthotopic malignant mesothelioma xenograft mouse model. Int J Oncol. 2016;48(4):1399–1407. | ||
Bartlett GR. Colorimetric assay methods for free and phosphorylated glyceric acids. J Biol Chem. 1959;234(3):469–471. | ||
Fujiwara H, Terashima M, Irinoda T, et al. Quantitative measurement of thymidylate synthase and dihydropyrimidine dehydrogenase mRNA level in gastric cancer by real-time RT-PCR. Jpn J Cancer Res. 2002;93(12):1342–1350. | ||
Ozols RF. Treatment goals in ovarian cancer. Int J Gynecol Cancer. 2005;15(Suppl 1):3–11. | ||
Markman M. Intraperitoneal antineoplastic agents for tumors principally confined to the peritoneal cavity. Cancer Treat Rev. 1986;13(4):219–242. | ||
Fortunato O, Boeri M, Verri C, Moro M, Sozzi G. Therapeutic use of microRNAs in lung cancer. Biomed Res Int. 2014;2014:756975. | ||
Trang P, Wiggins JF, Daige CL, et al. Systemic delivery of tumor suppressor microRNA mimics using a neutral lipid emulsion inhibits lung tumors in mice. Mol Ther. 2011;19(6):1116–1122. | ||
Wu Y, Crawford M, Mao Y, et al. Therapeutic delivery of microRNA-29b by cationic lipoplexes for lung cancer. Mol Ther Nucleic Acids. 2013;2:e84. | ||
Cortez MA, Valdecanas D, Zhang X, et al. Therapeutic delivery of miR-200c enhances rediosensitivity in lung cancer. Mol Ther. 2014;22(8):1494–1503. | ||
Reid G, Kao SC, Pavlakis N, et al. Clinical development of TargomiRs, a miRNA mimic-based treatment for patients with recurrent thoracic cancer. Epigenomics. 2016;8(8):1079–1085. | ||
van Zandwijk N, Pavlakis N, Kao SC, et al. Safety and activity of microRNA-loaded minicells in patients with recurrent malignant pleural mesothelioma: a first-in-man, phase 1, open-label, dose-escalation study. Lancet Oncol. 2017;18(10):1386–1396. | ||
Lee Y, Vassilakos A, Feng N, et al. GTI-2040, an antisense agent targeting the small subunit component (R2) of human ribonucleotide reductase, shows potent antitumor activity against a variety of tumors. Cancer Res. 2003;63(11):2802–2811. | ||
Klisovic RB, Blum W, Wei X, et al. Phase I study of GTI-2040, an antisense to ribonucleotide reductase, in combination with high-dose cytarabine in patients with acute myeloid leukemia. Clin Cancer Res. 2008;14(12):3889–3895. | ||
Sridhar SS, Canil CM, Chi KN, et al. A phase II study of the antisense oligonucleotide GTI-2040 plus docetaxel and prednisone as first-line treatment in castration-resistant prostate cancer. Cancer Chemother Pharmacol. 2011;67(4):927–933. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.