Back to Journals » Infection and Drug Resistance » Volume 16
Antibacterial Mechanism of Patrinia scabiosaefolia Against Methicillin Resistant Staphylococcus epidermidis
Authors Liu X, An L, Zhou Y, Peng W, Huang C
Received 21 November 2022
Accepted for publication 19 January 2023
Published 10 March 2023 Volume 2023:16 Pages 1345—1355
DOI https://doi.org/10.2147/IDR.S398227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xin Liu,1 Lili An,2 Yonghui Zhou,1 Wei Peng,1 Cong Huang1
1College of Basic Medicine, Guizhou University of Traditional Chinese Medicine, Guiyang City, People’s Republic of China; 2Dermatology Department, the First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine, Guiyang City, People’s Republic of China
Correspondence: Xin Liu, College of Basic Medicine, Guizhou University of Traditional Chinese Medicine, Guiyang City, People’s Republic of China, Tel +8618886056643, Email [email protected]
Purpose: Staphylococcus epidermidis has become one of the most common causes of septicemia. Meanwhile, S. epidermidis has acquired resistance to many antibiotics. Among these, methicillin-resistant S. epidermidis (MRSE) were frequently isolated. Similar to methicillin resistant Staphylococcus aureus (MRSA), they also exhibited multi-resistance, which presented a danger to human health. Patrinia scabiosaefolia as traditional Chinese medicine had strong antibacterial activity against MRSE. However, the mechanism of P. scabiosaefolia against MRSE is not clear.
Methods: Here, the morphology of cell wall and cell membrane, production of β-lactamase and PBP2, energy metabolism, antioxidant system were systematically studied.
Results: The data showed that P. scabiosaefolia damaged the cell wall and membrane. In addition, β-lactamase, energy metabolism and antioxidant system were involved in mechanisms of P. scabiosaefolia against MRSE.
Conclusion: These observations provided new understanding of P. scabiosaefolia against MRSE to control MRSE infections.
Keywords: methicillin-resistantStaphylococcus epidermidis, Patrinia scabiosifolia, β-lactamase, energy metabolism, antioxidant system
Introduction
Staphylococcus epidermidis (S. epidermidis) is one of the major opportunistic pathogens associated with skin colonization.1 With the widespread use of indwelling medical devices and implanted foreign bodies, S. epidermidis has become a significant threat to medical device associated infections (MDAI), including catheter-related bloodstream and surgical site infections, infective endocarditis, and so on.2–5 Recently, several studies have reported that the distribution of S. epidermidis in human clinical samples were higher than infections caused by Staphylococcus aureus in Greece and India.6 Antibiotics have been used as the most commonly used first-line treatment for S. epidermidis. Yet, a number of European health care outbreaks associated with multidrug-resistant S. epidermidis have also been described, among which more than 60% were resistant to methicillin (methicillin-resistant S. epidermidis, MRSE). The MRSE showed a broad drug resistance spectrum including β-lactam, quinolone, macrolide, aminoglycosides, and so on.7 The emergence of MRSE infections emphasized the need for antimicrobial drug design to yield new treatments before the pathogens become resistant to the last-resort antibiotics.
Because of the safety and diversity, traditional Chinese medicine (TCM) has increased widespread interest in the search of alternative antibacterial agents.8 In our previous study, Patrinia scabiosaefolia (PS) possessed antibacterial against MRSE (MIC: 5 mg/mL).9 PS has a long application story in China, where it is also named “Bai Jiang Cao” recorded in the “Sheng Nong’ Herbal Classic”. Pharmacology researches showed that PS possessed good antibacterial activity in vitro.10 The studies demonstrated that the extracts of PS had significant antibacterial activity against S. aureus, Staphylococcus albus, typhoid bacillus,Streptococcus B, pneumococcus,Escherichia coli, dysentery bacillus, and Pseudomonas aeruginosa.10,11 However, the antibacterial mechanism of PS against MRSE is still unknown.
In the present work, we systematically studied the antibacterial mechanism of PS against MRSE. The results showed that PS is a promising antibacterial agent and can be used to control MRSE infections.
Materials and Methods
Strains and Culture Conditions
In this study, the bacterial strain S. epidermidis ATCC12228 was obtained from American Type Culture Collection. The methicillin-resistant S. epidermidis (MRSE) was previously induced under methicillin from S. epidermidis ATCC12228 and preserved in our lab. The MRSE was cultured at 37°C in Tryptic Soy Broth (TSB). The strain has been identified by routine laboratory methods and stored in 20% (v/v) glycerol at −80°C.
Antimicrobial Assessments
Preparation of P. scabiosaefolia Extracts
P. scabiosaefolia was purchased from Xi’an Yunyue Biotechnology Co., Ltd (20220106). Then P. scabiosaefolia was shade-dried, and then finely powdered. Next, 150 mL water was used to extract 30 g TMC for three times. Then the extracts were merged. The ointment was concentrated by rotary evaporator and dried by vacuum drying oven at 60°C. Finally, 3 g dry powder was received. Each acquired fractions are dissolved in distilled water for 80 mg/mL of final concentration and filtered through a 0.45 μm Millipore syringe filter.
Determination of the Antibacterial Capability of P. scabiosaefolia
Minimal bactericidal concentration (MBC) was evaluated as reported previously.12 Briefly, the minimal inhibitory concentration (MIC) of P. scabiosaefolia was determined. Then all the MIC wells were then used for coating on agar plates for colony counting. The concentration of no growth (<5 CFU/mL) was determined as MBC.
Fractional inhibitory concentration index (FIC) was calculated using the following formula: FIC index (FICI)=(FIC of methicillin)+(FIC of P. scabiosaefolia). Among these, FIC of methicillin was MIC of methicillin in combination/MIC of methicillin alone. Similarly, FIC of P. scabiosaefolia was MIC of P. scabiosaefolia in combination/(MIC of P. scabiosaefolia alone. The combined effects were defined as follows: synergistic: FICI ≤0.5; additive: 0.5 ≤FICI ≤1; and indifferent: 1 ≤FICI ≤4. The above assays were repeated three times.
Antimicrobial Mechanism
Effect of P. scabiosaefolia on Methicillin-resistant of S. epidermidis Membrane Integrity
Experiments were conducted by the technique of Ding et al.13 Loss of 260 nm absorbing material released from bacteria was measured to detect the effect of P. scabiosaefolia on MRSE membrane integrity.14 The MRSE was harvested at their logarithmic phase, washed and re-suspended in sterile physiological saline to 1×106 CFU/mL. Then, MIC of P. scabiosaefolia was mixed with the bacterial suspension. The mixtures were then incubated at 37°C for 0, 1, 2, 3, or 4 h. The mixtures were centrifuged at 9800 g for 2 min, and the supernatant was filtration using a 0.22 µm filter membrane. The filtrates were analyzed using a microplate reader at 260 nm.
Effect of P. scabiosaefolia on Microcosmic Morphology of Methicillin-resistant S. epidermidis
MRSE in their logarithmic phase were harvested and re-suspended in sterile physiological saline to 1×106 CFU/mL. Furthermore, the bacterial suspensions with and without MIC P. scabiosaefolia were incubated at 37°C for 4 h. Meanwhile, the bacterial suspensions with MIC vancomycin were as positive control. Then, according to Ding WY, the mixtures were examined by scanning electron microscopy (SEM) and transmission electron microscopy (TEM).13
Evaluation of the Inhibitory Production of P. scabiosaefolia on β-Lactamase
The inhibition of P. scabiosaefolia on β-lactamase production was measured as follows. The MRSE were harvested at their logarithmic phase, washed and re-suspended in sterile physiological saline to 1×106 CFU/mL. Then MIC P. scabiosaefolia were mixed with the bacterial suspensions. Meanwhile, the bacterial suspensions with tazobactam were as positive control. The mixtures were then incubated at 37°C for 4 h. Then, the mixture were centrifuged at 9800 g for 5 min at 4°C. Finally, the samples dealt with sonication were measured by ELISA Kit. Each treatment was repeated at least three times.
Evaluation of the Inhibitory Production of P. scabiosaefolia on PBP2a
The inhibition of P. scabiosaefolia on PBP2a production was measured as follow. The MRSE were harvested at their logarithmic phase, washed and re-suspended in sterile physiological saline to 1×106 CFU/mL. Then MIC P. scabiosaefolia were mixed with the bacterial suspensions. Meanwhile, the bacterial suspensions without P. scabiosaefolia were a negative control. The mixtures were then incubated at 37°C for 4 h. To this cultured broth, 10 mg/mL cefradine was added to induce PBP2a for 2 h. Then the mixtures were centrifuged at 9800 g for 5 min at 4°C. Finally, the samples dealt with sonication were measured by ELISA Kit. Each treatment was repeated at least three times.
Key Enzymes in Energy Metabolism Process Analysis
The MRSE in the logarithmic phase was washed and re-suspended in sterile physiological saline to 1×106 CFU/mL. Then MIC P. scabiosaefolia were mixed with the bacterial suspensions. The mixtures were then incubated at 37°C for 4 h. A negative control was also prepared, containing distilled water instead of P. scabiosaefolia. Next, the succinate dehydrogenase activity (SDH) and NADP-malate dehydrogenase activity (NADP-MDH) activity of MRSE with and without MIC P. scabiosaefolia were measured by using kits. Then the mixtures were centrifuged at 9800 g for 5 min at 4°C and the supernatant were removed. The cells were rinsed and suspended in physiological saline solution. Next, the samples dealt with sonication were centrifuged at 9800 g for 5 min at 4°C. Finally, the SDH and NADP-MDH activity in the supernatant were assayed according to directions of test kit from Nanjing Jiancheng Institute. Each treatment was repeated at least three times.
Antioxidant System Analysis
The MRSE in the logarithmic phase was washed and re-suspended in sterile physiological saline to 1×106 CFU/mL. Then MIC P. scabiosaefolia were mixed with the bacterial suspensions. The mixtures were then incubated at 37°C for 4 h. A negative control was also prepared, containing distilled water instead of P. scabiosaefolia.The mixtures were centrifuged 9800 g for 5 min at 4°C and and the supernatant were removed. The cells were rinsed and suspended in physiological saline solution. Next, the samples dealt with sonication were centrifuged 9800 g for 5 min at 4°C. Finally, The catalase (CAT) and superoxide dismutase (SOD) activities in the supernatant were estimated by using kits from Nanjing Jiancheng Institute. Each treatment was repeated at least three times.
Antibacterial Activity of P. scabiosaefolia Against Bloodstream
Establishment of Mouse Immunosuppressive Models
Male ec57bl/6j mice between six and eight-weeks-old were used in this study. 120 mg/kg cyclophosphamide (CP) treatment regimen was used to induce immunosuppressive model.15 Briefly, the mice were injected intraperitoneally with CP doses of 120 mg/kg of body weight for four days. Control mice were received phosphate-buffered saline (PBS). Then, thymus and spleen were isolated from the immunosuppressive and control mice. The thymus and spleen index were calculated. The above mouse experiments were approved by the University Committee on Use and Care of Animals at the Guizhou University of Traditional Chinese medicine and done as Laboratory Animal – Guideline for Ethical Review of Animal Welfare (GB/T 35892—2018).
Treatment of P. scabiosaefolia Against MRSE-induced Bloodstream Infection
The mice were randomly separated into four groups, including immunosuppressive group, bloodstream infection group, P. scabiosaefolia group and blank group. P. scabiosaefolia (8 g/kg) was administered by oral at seven days before infection in P. scabiosaefolia group. Then immunosuppression model was performed at three days before infection as the above method in immunosuppressive group, bloodstream infection group and P. scabiosilia group. Further, bloodstream infection were done in bloodstream infection group and P. scabiosilia group as follows. MRSE were cultured overnight at 37°C. Then, the bacteria were diluted into 1×108 cfu/mL. The immunosuppressed mice were injected with 0.1 mL of the bacterial suspension at above doses by tail vein. At 24 h post-infection, the blood of the mice in each group was obtained. These samples were serially diluted in PBS and plated on TSB agar plates for 24 h at 37°C. Finally, the number of clones were counted in order to evaluate the mouse BSI models.16 The above mouse experiment was approved by the University Committee on Use and Care of Animals at the Guizhou University of Traditional Chinese Medicine and done as Laboratory Animal – Guideline for Ethical Review of Animal Welfare (GB/T 35892—2018).
Statistical Analysis
Values were expressed as means ±SDs. The statistical differences among the different groups were compared by one-way ANOVA, significant means were separated using Tukey’s Honest significant difference and p <0.05.
Results and Discussion
Antimicrobial Assessments
Antimicrobial Activity of P. scabiosaefolia Against Methicillin-resistant S. epidermidis
More precise data on the antimicrobial properties were obtained through the determination MBC. Based on the above results, MIC of P. scabiosaefolia was determined as 5 mg/mL (Table 1). Since complete killing has occurred at 20 mg/mL, this concentration was determined as MBC (Table 2).
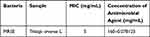 |
Table 1 MIC Value Against MRSE Isolates |
 |
Table 2 MBC Value Against MRSE Isolates |
In the current study, there is no standard of TCM against bacteria. In this study, literature about the antibacterial activity of TCM was consulted and the results indicated that the effective antibacterial activity of TCM crude extract was from 3.9 mg/mL to 125 mg/mL.17,18 Therefore, the results showed that P. scabiosaefolia may be a promising candidate for the treatment of MRSE infection.
Checkerboard Assays of P. scabiosaefolia and Methicillin
Beside antimicrobial activity of TCM, they may enhance the antibacterial effects of antibiotics in vitro.19 So, FICs of P. scabiosaefolia and methicillin in vitro were determined using the standard checkerboard methodology. The FIC index of P. scabiosaefolia and methicillin against MRSE was 0.75 by reducing MICs of methicillin from 64 μg/mL to 16 μg/mL (Table 3). According to the standard, the FIC index which is interpreted as 0.5 <FIC <1, stand for additive effect. So, the combination antibacterial of P. scabiosaefolia and methicillin against MRSE was an additive effect. It demonstrated that P. scabiosaefolia can improve the sensitivity of methicillin against MRSE.
 |
Table 3 The Effect of Combinations |
Antimicrobial Mechanism
Effect of P. scabiosaefolia on Methicillin-resistant S. epidermidis Membrane Integrity
The above results showed that P. scabiosaefolia was a strong antibacterial. However, the mechanism of P. scabiosaefolia against MRSE was not understood. We investigated the antibacterial effect of P. scabiosaefolia to evaluate its possible mechanism. The previous study reported that some antimicrobial agents cause gross membrane damage.20 So, in our study, membrane perturbation is involved in the antibacterial action. The intracellular components of cells are protected by cell membranes. Thus, the release of the intracellular components of bacterial cells can be used to monitor the membrane integrity.13 Thus, the detection of DNA and RNA from the protoplasm of bacterial cells represented whether the cell membrane has been destroyed.14 After treatment with P. scabiosaefolia at different times, the OD260 of filtrates of MRSE significantly changed during 4 h and the most remarkable increases occurred after 3-h treatment (Figure 1). The result suggested that P. scabiosaefolia damaged the cytoplasmic membrane, thereby causing the leakage of the DNA and RNA from the cells to kill MRSE. Interestingly, the absorbance at 4 h decreased. This was because of the release of RNA or DNA gradually degrading with the extension of time. Similar results were also reported as Staphylococcus xylosus and E. coli against CD-g-CS.21
 |
Figure 1 Release of intracellular components of methicillin-resistant S. epidermidis treated with MIC P. scabiosaefolia. Data were expressed as mean ±standard deviation (n=3). |
Effect of P. scabiosaefolia on Microcosmic Morphology of Methicillin-resistant S. epidermidis
The cell wall and cytoplasmic membrane play a very important role in protecting cells from external damage, and the integrity of the structure and morphology are vital to the normal functioning of cells.22 Therefore, the cell wall and cytoplasmic membrane of MRSE would be good target.
To understand the mode of action of P. scabiosaefolia, morphological changes of MRSE cells were observed using SEM. SEM images of MRSE included the untreated group (Figure 2A), positive-treated (vancomycin) group (Figure 2B), and P. scabiosaefolia-treated group (Figure 2C). Figure 2A showed that MRSE cells had smooth, rounded shapes and intact cell membranes. However, MRSE treated with vancomycin showed extracellular changes (Figure 2B). At the same time, Figure 2C showed that the outermost layer of the MRSE had disappeared and the cells had lost a lot of protection which can cause cell death. The results demonstrated that P. scabiosaefolia may have severe effects on the cell wall and cytoplasmic membrane. However, more detailed observations were still needed.
To further elucidate the effect of P. scabiosaefolia against MRSE membrane, the above groups were imaged with TEM. TEM allowed higher magnification and observation of intracellular structures of the cells. As shown in Figure 3A, MRSE cells without P. scabiosaefolia were normal and surrounded by cell membranes with a compact surface, which showed a well-defined cell membrane and a uniform cytoplasm region, without the release of intracellular components. However, most MRSE cells with P. scabiosaefolia (Figure 3C) appeared the lysis of cell wall, discontinuous cell membrane, and a few cells had dissolved. Meanwhile, the similar breakage also appeared in positive-treated (vancomycin) group (Figure 3B). In short, among the three samples, only the morphological structure of the bacteria in untreated group was relatively normal. In the P. scabiosaefolia and vancomycin groups, different degrees of necrosis were found.
So, the both images suggested that the antimicrobial mechanism of P. scabiosaefolia was related to wall and membrane disruption. Meanwhile, The similar results occurred in Aronia melanocarpa (Michx.), Chaenomeles superba Lindl. and Cornus mas L. leaf extracts against bacteria cells.23
Effect of P. scabiosaefolia on β-Lactamase and PBP2a
It is well known that the production of PBP2a and β-lactamase is attributed to β-lactam resistance.24 So, the antimicrobial mechanism of P. scabiosaefolia against MRSE may relate to them. In order to explore relationship of β-lactamase and P. scabiosaefolia, β-lactamase production was tested in MRSE untreated or treated with P. scabiosaefolia. Figure 4 showed that the positive control (tazobactam) reduced β-lactamase production. Since β-lactamase production was significantly reduced by MIC P. scabiosaefolia, compared to the untreated group. The results instructed that the antimicrobial mechanism of P. scabiosaefolia against MRSE was related to β-lactamase.
In addition, PBP2a production was also tested. In order to explore relationship between PBP2a and P. scabiosaefolia, PBP2a production was tested in MRSE untreated or treated with P. scabiosaefolia. Differently, Supplementary Figure 1 showed that PBP2a production was not reduced by MIC P. scabiosaefolia, compared to the untreated group. So, the results indicated that the antimicrobial mechanism of P. scabiosaefolia against MRSE was not related to PBP2a.
Effect of P. scabiosaefolia on Energy Metabolism Enzyme of MRSE
The TCA cycle is the vital pathway to provide energy for cell activity, which not only provides energy for organisms, but also serves as the hub for the transformation of three major substances (sugar, lipid, and protein).25 In TCA cycle, MDH can catalyze malic acid to form oxaloacetic acid, which is essential for cell growth. In addition, SDH is also a key enzyme in the TCA cycle and one of the key links between oxidative phosphorylation and electron transport. So, the activities of SDH and NADP-MDH were investigated. Compared with the control group, Figure 5A and B showed that the activities of SDH and NADP-MDH of MRSE under P. scabiosaefolia stress for 4 h significantly decreased. The above results were consistent with previous research reported by Chen et al, that the SDH enzyme activity of S. aureus was significantly suppressed under persimmon tannin.26 Therefore, the P. scabiosaefolia had a strong effect on the two key enzymes in energy metabolism.
Effect of P. scabiosaefolia on Antioxidant Enzyme System of MRSE
Defense mechanisms of cells including SOD, CAT and other antioxidant enzymes have the ability to counteract the killing effect of ROS, which is one of their mechanisms of antibacterial activity.27 To explore the impact of MRSE by P. scabiosaefolia, the activity of ROS related enzymes (SOD and CAT) were determined. As seen in Figure 6A and B, CAT and SOD treated with P. scabiosaefolia significantly reduced (p <0.05) when compared with control group. Thence, we believed that the P. scabiosaefolia had stronger effect on the two key enzymes in antioxidant enzyme system.
The production of ROS inevitably caused oxidative stress into bacteria death.28 On the contrary, antioxidant enzyme system can withstand the killing effect.29 The research demonstrated the plant extracts can decrease of SOD and CAT activities.23 Similarly, the activity of antioxidant enzyme system decrease in our study, demonstrating that P. scabiosaefolia can promote the effect of oxidative stress.
Effect of P. scabiosaefolia Against MRSE-induced Bloodstream Infection
In the above work, we found that P. scabiosaefolia had better antibacterial activity against MRSE in vitro. In order to further evaluate the antibacterial activity in vivo, the antimicrobial efficacy of P. scabiosaefolia treating MRSE-induced bloodstream infection was done. Because S. epidermidis is one of the major opportunistic pathogens, the immunosuppression model should be established. Supplementary Figure 2 showed that compared to blank group, the thymus and spleen index of immunosuppressive group, bloodstream infection group, and P. scabiosaefolia group significantly reduced. The results illustrated the immunosuppression model was successfully established. The MRSE-induced bloodstream infection model was established following the immunosuppression model. Based on the bloodstream infection model, the validity of P. scabiosaefolia was studied. The Figure 7 showed that after treatment of P. scabiosaefolia, the the number of clones of blood from P. scabiosaefolia group were significantly reduced, when compared with bloodstream infection group. The results illustrated P. scabiosaefolia had better antibacterial activity.
Conclusion
P. scabiosaefolia showed strong antimicrobial activity against MRSE in vitro and vivo. Furthermore, based on cell membrane integrity tests, SEM, TEM observation, enzyme activity determined that the antimicrobial mechanisms of P. scabiosaefolia were due to membrane disruption, β-lactamase reduction, inhibition of energy metabolism and antioxidant system. The findings of this study can help us understand the antimicrobial mechanism of P. scabiosaefolia, and may become a promising candidate for the treatment of MRSE infection.
Acknowledgments
We thank for financial support by the earmarked funding for the Science and Technology Foundation of Guizhou Province under Grant number Qianke He Foundation-ZK (2021) General 08, Young scientific and technological talents project of Gui Zhou Department of Education under Grant number Qianjiaohe KY (2022) 269, Doctor start-up fund of Guizhou University of Traditional Chinese Medicine under Grant number PhD start-up fund (2020] 22 and Gui Zhong Yi Ke Yuan Nei (2013) 22#.
Funding
The National Nature Science Foundation of China under Grant number 82260824. The Science and Technology Foundation of Guizhou Province under Grant number Qianke He Foundation-ZK (2021) General 08. The Young scientific and technological talents project of Gui Zhou Department of Education under Grant number Qianjiaohe KY (2022) 269. The Gui Zhong Yi Ke Yuan Nei (2013) 22#.
Disclosure
All authors declare no competing interests.
References
1. Xu Z, Cave R, Chen LQ, et al. Antibiotic resistance and molecular characteristics of methicillin-resistant Staphylococcus epidermidis recovered from hospital personnel in China. J Global Antimicrob Resist. 2020;22:195–201. doi:10.1016/j.jgar.2020.02.013
2. Watanabe S, Kawakami Y, Kimura H, Murakami S, Yamaguchi T. Association between daptomycin susceptibility and teicoplanin resistance in Staphylococcus epidermidis. Sci Rep. 2019;9(1). doi:10.1038/s41598-019-55149-z
3. Nguyen TH, Park M, Otto M. Host Response to Staphylococcus epidermidis Colonization and Infections. Front Cell Infect Microbiol. 2017;7:90. doi:10.3389/fcimb.2017.00090
4. Rice C, Lam AK, Foxley MA, Moen EL, Pusavat J, Wouters CL. Cationic Branched Polyethylenimine (BPEI) disables antibiotic resistance in methicillin-resistant Staphylococcus epidermidis (MRSE). ChemMedChem. 2018;13(20):2240–2248. doi:10.1002/cmdc.201800433
5. Yang M, Wang YW, Zhang YH, Li YJ, Li QF, Tan JT. Role of interleukin-33 in Staphylococcus epidermidis-induced septicemia. Front Immunol. 2020;11:534099. doi:10.3389/fimmu.2020.534099
6. Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27:870–926. doi:10.1128/CMR.00109-13
7. Ran FU, Fang-mei FU, Han-mei H, et al.Multi-drug resistance phenotype analysis of methicillin resistant Staplylococcus epidermidis and screening of antibacterial Chinese medicine. J Med Inform. 2022;35(3):1–8.
8. Paolo MG. Traditional phytotherapy in central Italy (Marche, Abruzzo, and Latium). Fitoterapia. 2005;76(1):1–25. doi:10.1016/j.fitote.2004.09.006
9. Liu X, An LL, Ren SJ, Zhou YH, Peng W. Comparative proteomic analysis reveals antibacterial mechanism of patrinia scabiosaefolia. against methicillin resistant Staphylococcus epidermidis. Infect Drug Resist. 2022;15:883–893. doi:10.2147/IDR.S350715
10. He XR, Luan F, Zhao ZF, Ning N, Li MX, Jin L. Chemical constituents and pharmacological effects of genus patrinia: a review. Curr Pharmacol Rep. 2020;6(6):1–35.
11. Chao T, Sun Z, Zhou K, Xu J. Studies on chemical constituents and sedation and antibacterial effect of Patrinia scabiosaefolia Fisch. J Trad Chin Vet Med. 2003;22(4):3–5.
12. Hashizume H, Takahashi Y, Masuda T, et al. In vivo efficacy of β-lactam/tripropeptin C in a mouse septicemia model and the mechanism of reverse β-lactam resistance in methicillin-resistant Staphylococcus aureus mediated by tripropeptin C. J Antibiot. 2017;71(1):79–85.
13. Ding WY, Zheng SD, Qin Y, Yu F, Bai JW, Cui WQ. Chitosan grafted with β-cyclodextrin: synthesis, characterization, antimicrobial activity, and role as absorbefacient and solubilizer. Front Chem. 2019;6. doi:10.3389/fchem.2018.00657
14. Devi KP, Nisha SA, Sakthivel R, Pandian SK. Eugenol (an essential oil of clove) acts as an antibacterial agent against Salmonella typhi by disrupting the cellular membrane. J Ethnopharmacol. 2010;130(1):107–115. doi:10.1016/j.jep.2010.04.025
15. Subashchandrabose S, Sara S, Valerie D, et al. Acinetobacter baumanniiGenes required for bacterial survival during bloodstream infection. Msphere. 2015;1(1). doi:10.1128/mSphere.00013-15
16. Chen X, Lou WY, Liu JX, Ding BS, Fan WM, Hong J. A novel antimicrobial polymer efficiently treats multidrug-resistant MRSA-induced bloodstream infection. Biosci Rep. 2019;39(10). doi:10.1042/BSR20192354
17. Zhou Y, Li FH, Guo JJ, Ren H, Wang QH, Chen XQ. Screening of antibacterial activity in vitro of 25 kinds of Chinese medicinal materials from guizhou. Chin J Ethnomed Ethnopharm. 2020;29(9):7.
18. Yi GJ. Study on the Pharmacodynamics and Mechanism of Anti-Drug-Resistant Pseudomonas Aeruginosa Biofilm of Qingrejiedu Traditional Chinese Medicine. Chengdu University; 2020.
19. Kırmusaoğlu S. Sensitizing of β-lactam resistance by tannic acid in methicillin-resistant S. aureus. World J Microbiol Biotechnol. 2019;35(4). doi:10.1007/s11274-019-2637-6
20. Chovanová R, MikuláOvá M, Vaverková Š. In vitro antibacterial and antibiotic resistance modifying effect of bioactive plant extracts on methicillin-resistant Staphylococcus epidermidis. Int J Microbiol. 2013;2013:1–7. doi:10.1155/2013/760969
21. Kpadonou D, Kpoviessi S, Bero J, et al. Chemical composition, in vitro antioxidant and antiparasitic properties of the essential oils of three plants used in traditional medicine in Benin. J Med Plant Res. 2019;13(6):384–395.
22. Wang R, Zhang Y, Jia Y, et al. Persimmon oligomeric proanthocyanidins exert antibacterial activity through damaging the cell membrane and disrupting the energy metabolism of Staphylococcus aureus. ACS Food Sci Technol. 2021;1(1):35–44. doi:10.1021/acsfoodscitech.0c00021
23. Efenberger-Szmechtyk M, Nowak A, Czyowska A, Niadowska M, Otlewska A, Yelewicz D. Antibacterial mechanisms of Aronia melanocarpa (Michx.), Chaenomeles superba Lindl. and Cornus mas L. leaf extracts. Food Chem. 2021;350:129218. doi:10.1016/j.foodchem.2021.129218
24. Tajima Y. Effects of tungstosilicate on strains of methicillin-resistant Staphylococcus aureus with unique resistant mechanisms. Microbiol Immunol. 2003;47(3):207–212. doi:10.1111/j.1348-0421.2003.tb03388.x
25. Mla B, Mf C, Ky A, et al. Transcriptomic and metabolomic analyses reveal antibacterial mechanism of astringent persimmon tannin against Methicillin-resistant Staphylococcus aureus isolated from pork - ScienceDirect. Food Chem. 2020;309:125692.
26. Chen J, Tang C, Zhang R, Ye S, Yang D. Metabolomics analysis to evaluate the antibacterial activity of the essential oil from the leaves of Cinnamomum camphora (Linn.) Presl. J Ethnopharmacol. 2020;253:112652. doi:10.1016/j.jep.2020.112652
27. Chai Z, Zhang F, Liu B, Chen X, Meng X. Antibacterial mechanism and preservation effect of curcumin-based photodynamic extends the shelf life of fresh-cut pears. LWT Food Sci Technol. 2021;142(23):110941. doi:10.1016/j.lwt.2021.110941
28. Chen Z, Chen Z, Gan Y, Li T, Kexin GU, Yin L. Antibacterial photodynamic gold nanoparticles for skin infection. ACS Appl Bio Mater. 2021;4(2):1461–1469. doi:10.1021/acsabm.0c01334
29. Kim J, Kim S, Lee K, Kim RH, Hwang KT. Antibacterial photodynamic inactivation of fagopyrin f from tartary buckwheat (Fagopyrum tataricum) flower against Streptococcus mutans and its biofilm. Int J Mol Sci. 2021;22(12):6205.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






