Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Anti-Inflammatory Treatment Efficacy in Major Depressive Disorder: A Systematic Review of Meta-Analyses
Authors Simon MS , Arteaga-Henríquez G, Fouad Algendy A, Siepmann T, Illigens BMW
Received 5 August 2022
Accepted for publication 13 December 2022
Published 5 January 2023 Volume 2023:19 Pages 1—25
DOI https://doi.org/10.2147/NDT.S385117
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Maria S Simon,1,2 Gara Arteaga-Henríquez,3,4 Ahmed Fouad Algendy,1,5 Timo Siepmann,1,6 Ben MW Illigens1,7
1Division of Health Care Sciences, Dresden International University, Dresden, Saxony, Germany; 2Department of Psychiatry and Psychotherapy, University Hospital, Ludwig-Maximilians-University, Munich, Bavaria, Germany; 3Department of Psychiatry, Hospital Universitari Vall d’Hebron, Vall d’Hebron Research Institute (VHIR), Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain; 4Biomedical Network Research Centre on Mental Health (CIBERSAM), Madrid, Spain; 5Clinical Pharmacy, Geriatric Department, Rumailah Hospital, Hamad Medical Corporation, Doha, Qatar; 6Department of Neurology, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Saxony, Germany; 7Department of Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
Correspondence: Maria S Simon, Department of Psychiatry and Psychotherapy, University Hospital, Ludwig-Maximilians-University Munich, Nußbaumstraße 7, Munich, 80336, Germany, Tel +4989440052769, Email [email protected]
Purpose: Immune imbalances in major depressive disorder (MDD) have been targeted by anti-inflammatory treatment approaches in clinical trials to increase responsiveness to therapy. However, even after several meta-analyses, no translation of evidence into clinical practice has taken place. We performed a systematic review to evaluate meta-analytic evidence of randomized controlled trials on the use of anti-inflammatory agents for MDD to summarize efficacy estimates and elucidate shortcomings.
Methods: Pooled effect estimates and heterogeneity indices were primary outcomes. Characteristics of the included meta-analyses were extracted. Scientific quality of meta-analyses was assessed using the Revised Assessment of Multiple Systematic Reviews (R-AMSTAR).
Results: N=20 meta-analyses met the eligibility criteria. Study characteristics like outcome scales, composition of patient populations, and add-on or monotherapy regimen varied very little for celecoxib studies, varied little for minocycline studies, and were rather variable for omega 3 fatty acids studies. R-AMSTAR scores ranged from 26 to 39 out of 44 points indicating variable quality, where a comprehensive literature search was the strongest and the consideration of scientific quality in the conclusions was the weakest domain across all meta-analyses. For minocycline and celecoxib, superiority was demonstrated with medium to large effect size with substantial heterogeneity and with large to very large effect size with negligible heterogeneity, respectively. For omega 3 fatty acids, superiority was also demonstrated with mainly small and medium effect sizes with substantial heterogeneity. However, for minocycline and omega 3 fatty acids, non-significant meta-analyses were found also.
Conclusion: Even in our synthesized approach, no clear recommendations could be derived on the use of anti-inflammatory treatment for MDD due to several critical aspects like heterogeneity, diversity of patient populations, treatment regimen, and outcomes, and limited scientific quality. However, we observed clear inter-substance differences with meta-analytic evidence being strongest for celecoxib and weakest for omega 3 fatty acids.
Keywords: major depressive disorder, inflammation, anti-inflammatory therapy, state of knowledge, methodological shortcomings
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Wessa has been published for this article.
Introduction
Major depressive disorder is a worldwide health problem. The Global Burden of Diseases, Injuries, and Risk Factors Study shows that depressive disorders rank at 13 in the disability-adjusted life years ranking, where in the younger age groups (10–49 years) they even rank among the top ten.1 A variety of treatment options have been established, and medication like selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), or serotonin-norepinephrine reuptake inhibitors (SNRIs) are prescribed very often.2–4 However, the course of disease is often recurring, and a considerable number of patients do not respond to established therapies appropriately.5–7
The most prominent etiological theory is the monoamine hypothesis which proposes a lack of neurotransmitter availability during neurotransmission (specifically serotonin, noradrenaline, and/or dopamine), leading to depressive symptomatology.8–10 Now a mounting body of evidence supports the role of inflammatory activation and immune deregulations in depression, where several components of the immune system have been investigated. Most studies focused on levels of pro-inflammatory circulating cytokines, many of which were found to be elevated in depression.11,12 Much attention has also been paid to the kynurenine pathway which is stimulated by pro-inflammatory activation.13 Neurotoxic kynurenine pathway metabolites are thought to play a role in the pathophysiology of depression, but diverging evidence exists.13,14 Further, altered lymphocyte apportioning for T regulatory cells, Th2 cells, Th17 cells, T memory cells, and NK cells was found among patients with major depressive disorder.15–17 Last but not least, low-grade inflammation was also present in the monocyte gene expression signature of such patients.18 These studies give an impression of the variety of compounds studied and the complexity of assembling the pathophysiological mechanisms of major depressive disorder. So far, no integrative theory exists.
Inflammation has been discussed as a major contributor to non-response to established antidepressants.19–21 Thus, anti-inflammatory treatment approaches have been introduced and were tested in numerous clinical trials to treat depression. These studies investigated anti-inflammatory agents as single agents or as add-on regimen to standard therapy and in patients diagnosed with major depressive disorder or with depressive symptoms (eg, Freeman et al, Müller et al).22,23 The investigated agents exhibit their mechanism of action at different points in the pathway of the inflammatory machinery. For example, non-steroidal anti-inflammatory drugs, (NSAID) like the cyclooxygenase (cox)-2 selective NSAID celecoxib, inhibit the enzymes cox while cox-2 is mainly involved in the stimulation of inflammation.24 Anti-tumor necrosis factor (TNF) antibodies (such as infliximab) directly target and inactivate the pro-inflammatory cytokine TNF.25 N-acetylcysteine (NAC) reduces reactive oxygen species and oxidative stress and thus has anti-inflammatory properties.26,27 Minocycline also exerts anti-oxidative and anti-inflammatory properties, but multiple mechanisms are under consideration such as the inhibition of the inflammation stimulating enzymes matrix metalloproteinases, cox-2, and caspase-1.28,29 Lastly, omega 3 fatty acids also have immune-modulating capacities through multiple mechanisms such as inhibition of cox, pro-inflammatory cytokines, or transcription nuclear factor kappa B.30 In fact, a reduction of inflammatory parameters in depressed patients after the application of anti-inflammatory treatment has been shown: C-reactive protein (CRP) levels declined from baseline to endpoint during infliximab therapy.31 However, other studies on macrophage migration inhibitory factor (MIF) during celecoxib treatment, on CRP and interleukin-6 (IL-6) during NAC treatment, or on CRP during minocycline treatment showed no significant change or even an increase in their levels.20,32–34 This demonstrates the complexity of underlying mechanisms in that the choice of inflammatory biomarkers may not be representative for the mechanism of action of the given treatment. Nevertheless, response to anti-inflammatory agents like minocycline, celecoxib, or omega 3 fatty acids and their superiority over the placebo condition has been shown (eg, Husain et al, Su et al).23,35,36 Noteworthy, some studies show contradictory results in that no significant difference was found between the treatment and the placebo groups.37,38 Concluding from this research, anti-inflammatory agents may be a promising approach to treat depression but diverging results on efficacy exist. Thus, the gain over placebo (as single or add-on regimen) and with that the gain for clinical care is somewhat questionable. Despite the ongoing interest and studies on those drugs, they have not been incorporated in treatment guidelines so far. Meta-analyses have been conducted to provide an overview of and to summarize the current evidence from single studies. However, still no definite judgement on usability and a perspective for clinical translation are available.
A possible reason for the lack of applicability of research into clinical practice may lie in the diversity of study designs leading to heterogeneity of effect sizes, especially regarding the inclusion of patients with MDD diagnoses and patients with depressive symptoms. The present work evaluated the current state of research by systematically reviewing the pooled efficacy from meta-analyses and their quality of a variety of sole anti-inflammatory treatments compared to placebo or as add-on to standard care in MDD. Included agents were chosen based on their known direct anti-inflammatory mechanism. Further, the systematic review examines several study characteristics and limiting factors to this research as potential explanations for why it is difficult to obtain consistent and translatable results. With this review, the strength of evidence will be evaluated and thus indicate clinical usability of past research in this field.
Methods
The protocol for this systematic review was designed a priori and registered in PROSPERO under the reference number CRD42022296596. As far as applicable, the review was conducted according to the PRISMA guideline (PRISMA checklist is appended as Supplementary Material).39
Eligibility Criteria
Inclusion criteria for human studies were established in PICOS format according to PRISMA: participants – adult patients with a confirmed diagnosis of major depressive disorder as assessed by physician diagnosis, DSM or ICD criteria, or diagnostic interview; intervention – at least one of the following anti-inflammatory drugs as single or add-on agent: minocycline, non-steroidal anti-inflammatory drugs (NSAID), omega 3 fatty acids, anti-TNF, N-acetylcysteine; comparator – placebo, or active comparator such as treatment as usual (TAU) or antidepressants, or TAU/antidepressants plus placebo, corresponding to the intervention setup; outcome – validated depression rating scale; study design – meta-analysis of at least two randomized controlled trials (RCTs) with pooled effect estimates.39 In case a meta-analysis only included a subset of eligible patients, the meta-analysis was included if a subset analyses on eligible patients was performed and reported. Further, only meta-analyses in English language were included. Exclusion criteria were as follows: 1) patients with otherwise diagnosed depressive episodes, eg, bipolar depression; 2) children and adolescents; 3) classification of depression only by rating scales; 4) other anti-inflammatory agents; 5) meta-analyses including quasi-experimental or observational studies.
Search Strategy
A systematic search was conducted in the databases PubMed/MEDLINE, PsychINFO, Cochrane Library, and Web of Science from inception up until November 2021. Two of the authors conducted the search independently where databases were last consulted by MSS on November 1, 2021, and last consulted by GAH on November 14, 2021. The following search terms were used: ((“depression” [Title/Abstract] OR “depressed”[Title/Abstract] OR “depressive” [Title/Abstract]) AND (“response” [Title/Abstract] OR “effect” [Title/Abstract] OR “efficacy” [Title/Abstract] OR “therapy” [Title/Abstract] OR “treatment” [Title/Abstract]) AND (“anti inflammatory” [Title/Abstract] OR “NSAID” [Title/Abstract] OR “non steroidal anti inflammatory drugs” [Title/Abstract] OR “ASA” [Title/Abstract] OR “acetylsalicylic acid” [Title/Abstract] OR “ASS” [Title/Abstract] OR “aspirin” [Title/Abstract] OR “cox 2 inhibitor” [Title/Abstract] OR “celecoxib” [Title/Abstract] OR “ibuprophen” [Title/Abstract] OR “minocycline” [Title/Abstract] OR “infliximab” [Title/Abstract] OR “anti tnf” [Title/Abstract] OR “omega” [Title/Abstract] OR “NAC” [Title/Abstract] OR “acetylcysteine” [Title/Abstract]) AND (meta-analysis[Publication Type] OR meta analysis[Publication Type])) NOT (“children” [Title/Abstract] OR “adolescent” [Title/Abstract]). Rather broad terms were chosen in order to increase the likelihood of identifying all relevant studies. The search term was entered into Pubmed/Medline as shown previously. For the search in Web of Science ‘Publication Type’ was exchanged for ‘Title’ or ‘Abstract’ and in PsychInfo ‘Publication Type’ was exchanged for ‘Document Type’, and, the search was carried out twice with ‘Title’ and ‘Abstract’ separately for both databases. For the search in Cochrane library, ‘Title/Abstract’ was exchanged for ‘Title Abstract Keyword’.
Selection Process
Two independent reviewers (MSS and GAH) screened the records by title and abstract resulting from database search. Full articles were assessed for eligibility for all remaining records after screening, as well as records where title and abstract were not sufficient to identify non-eligibility. Upon selection differences between the two reviewers, a second screening of the article was conducted, and discrepancies were resolved by consensus.
Data Collection Process and Data Items
The data of interest were obtained by MSS from the eligible records using a data extraction form. Data were retrieved from the full article and the Supplementary Material. If not stated in the article or Supplementary Material, data were obtained from the single studies that were included in the meta-analyses. Extracted data were confirmed by double extraction.
The primary data items of interest were efficacy outcome measures for therapy. This includes pooled effect estimates for mean differences in validated depression rating scales, pooled effect estimates for response and remission rates obtained from validated depression rating scales, and the respective p-values and 95% confidence intervals. Further, the number of studies included in the meta-analysis and I2 index for heterogeneity were extracted. Heterogeneity is classified according to the Cochrane handbook: 0% to 40% negligible heterogeneity, 30% to 60% moderate heterogeneity, 50% to 90% substantial heterogeneity, 75% to 100% considerable heterogeneity.40 In case the I2 statistic was not given, Q-statistic and the corresponding p-value were extracted. If a meta-analysis included a study more than once due to multiple intervention arms, each separately included arm was counted as one study. For description of characteristics of the meta-analyses, the composition of populations included in the single studies, the intervention and comparator regimen, the total number of subjects analyzed under the intervention in the meta-analysis, the type of rating scales pooled, and the study design were extracted. In case the number of analyzed subjects was not reported, the number of randomized subjects was used.
Quality Assessment
The quality of included meta-analyses was assessed using the Revised Assessment of Multiple Systematic Reviews tool by MSS (R-AMSTAR).41 The template to conduct the rating was provided by PEROSH OSH Evidence Group.42 The R-AMSTAR has the benefit of providing a score between 1 and 4 in several items relevant to risk of bias as assessed by the strength of methodology and the reporting of crucial aspects. By calculating the sum score, a quantitative measure can be derived, allowing the comparison of the quality of meta-analysis with each other in relation to the maximum possible score of 44 points. However, no classification has been established of which value is considered low, medium, or high quality yet. The following aspects are covered by 11 items: provision of an a priori design, selection and extraction by at least two reviewers, methods of literature search, restrictions to publication type and language, traceability of included and excluded studies, provision of study characteristics, assessment of study quality, consideration of study quality for conclusions, appropriateness of study combination methods, assessment of publication bias, and assessment of conflicts of interest.41 The quality assessment was double checked.
Effect Measures
No restrictions were set to the effect measures used in the meta-analyses. The main outcomes of interest were the mean differences in depressive symptoms (continuous variable) and the comparison of response and remissions rates (dichotomous variables) between the intervention and the control group, as measured by a validated rating scale. Thus, effect estimates can include standard mean difference (SMD), pooled mean difference (MD), weighted mean differences (WMD), Hedges’ g, or others if available for mean differences in depressive symptoms. Effect estimates for response and remission rates can include risk ratio (RR), odds ratio (OR), or others if available for response and remission rates.
Synthesis Methods
Since the present work is a systematic review, data were structured to provide a summary and an overview of available data. For presentation of characteristics and results of meta-analyses, data were grouped and tabulated per each intervention type and meta-analyses were sorted by publication date within. If a meta-analysis provided multiple effect measures, the mean differences were listed first, and the response and remission rates were listed second. Regarding the characteristics, ranges of analyzed patients in the intervention group, ranges of publication years, number of studies with comorbid diagnoses or special characteristics of the patient population, and number of studies with monotherapy and/or add-on regimen were evaluated. Regarding the results of the meta-analyses, ranges of effect estimates and heterogeneity indices were evaluated per intervention type to give an impression of the consistency of findings. Further, single studies in the respective meta-analyses were listed to explore the overlap and diversity of studies used to calculate the effect measures. For graphical presentation of the quality assessment, the relative frequencies (percentage) of studies that were rated by each point category for each item were calculated and output as stacked bar graph. This was done using IBM SPSS Statistics for Mac OS version 28.0. For graphical presentation of Forrest plots R studio version 4.0.3 was used.
Results
Search Results
Initially, n=254 studies were retrieved from the databases of which n=20 studies finally met the eligibility criteria. The main reason for exclusion during eligibility assessment was the presence of not purely diagnosed MDD samples. For more details on the selection process see Figure 1 according to the PRISMA guideline.39 The included studies are listed in Table 1. With respect to the agents of interest, n=5 studies reported on minocycline, n=7 studies reported on NSAIDs (celecoxib), n=14 studies reported on omega 3 fatty acids, n=1 study reported on multiple agents (celecoxib and anti-TNF), and n=0 studies reported on NAC. A list of seriously considered studies that were excluded can be found in Supplementary Table 1.
 |  |  |
Table 1 Study Characteristics of the Included Meta-Analyses |
 |
Figure 1 PRISMA 2020 flow diagram of the study selection process. Abbreviations: n, number of studies; MDD, major depressive disorder. Notes: PRISMA figure adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Creative Commons.39 |
Study Characteristics
Characteristics of the included meta-analyses are displayed in Table 1. All meta-analyses included RCTs only. Per agent of interest between n=39 and n=82 patients in the minocycline intervention group were pooled, between n=50 and n=160 patients in the celecoxib treatment group were pooled, between n=62 and n=727 patients in the omega 3 fatty acid treatment group were pooled, and n=98 patients in the multiple treatment group were pooled in the meta-analyses. Meta-analyses were conducted between the years 2018 and 2021 for minocycline, from 2014 to 2021 for celecoxib, from 2012 to 2021 for omega 3 fatty acids, and the multiple agents meta-analysis was conducted in 2014. Minocycline meta-analyses included studies using HAMD and MADRS as outcome measure. For celecoxib, only studies using HAMD were pooled in the meta-analyses. Meta-analyses investigating omega 3 fatty acids included a higher variability of outcome measures: HAMD, MADRS, BDI or BDI-II, EPDS, GDS, and IDS-SR. Regarding the patient population, four out of five meta-analyses on minocycline included one study with patients with comorbid HIV, while six out of seven meta-analyses on celecoxib included one study with only female patients. For meta-analyses on omega 3 fatty acids, included populations are more heterogeneous with regard to comorbid diagnoses or special population characteristics and the number of studies with such samples. The following comorbid diagnoses or characteristics were found: coronary heart disease, diabetes, Parkinson’s disease, Multiple sclerosis, renal disease, only perinatal women, only elderly women. Only two meta-analyses did not report the inclusion of studies with comorbid patient samples. Lastly, meta-analyses included studies with monotherapy or add-on design. For minocycline, two meta-analyses investigated monotherapy and three meta-analyses included studies of both designs. For celecoxib, all studies used an add-on to antidepressants design. For omega 3 fatty acids, one meta-analysis investigated monotherapy, four investigated add-on to antidepressant therapy only, and nine meta-analyses included studies of both designs.
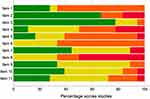
Quality Assessment
18 studies were assessed for quality. Two studies could not be assessed because they were selected re-analyses of a previously conducted study by other authors and thus did not provide a full methods and results section as usual.53,54 The R-AMSTAR assessment yielded variable quality of meta-analyses which ranged from 26 to 39 out of 44 possible points. Noteworthy, if no criteria are fulfilled in one category, it is rated with 1 point. Thus, the minimum total score is 11 points. The total scores and the quality rating conducted in the meta-analyses for the single studies are presented in Table 2. Supplementary Table 2 shows the item-based scores. Domains that were generally well reported were duplicate data extraction, methods of literature search, quality assessment, and investigation of heterogeneity and publication bias (see total scores per item in Supplementary Table 2). The domains generally not well reported were provision of a protocol, publication type, retracing excluded studies, study characteristics, and especially consideration of quality assessment in the conclusions (see total scores per item in Supplementary Table 2). Important to note is that in 50% of the meta-analyses, a lack of reporting on consideration of quality assessment in the conclusions (item 8) was present. Figure 2 provides a visual overview of study quality by R-AMSTAR domain. The quality assessment in the meta-analyses of the included studies ranged from very low to high and was thus highly variable despite overlap of included studies.
 |
Table 2 R-AMSTAR Quality Rating of Meta-Analyses Ranked in Descending Order and Quality Ratings by the Meta-Analyses of the Included Single Studies |
Results of Meta-Analyses
Minocycline
Details on the results are displayed in Table 3. Three meta-analyses showed superiority of minocycline over the placebo condition for mean difference (SMD ranging between −0.78 and −0.87), while one of them reached significance only when all three studies were included. Those meta-analyses yielded substantial heterogeneity between 53% and 63%. Two studies showed no significant difference with an SMD of −0.81 also with substantial heterogeneity (75% and 77%). One meta-analysis demonstrated superiority of minocycline using response rates by showing that the risk of becoming a responder is 2.83 times higher under exposure to minocycline than becoming a responder under placebo condition, without heterogeneity. The reported meta-analyses are based on two to three studies and have a high overlap in those (see Supplementary Table 3A).
 |
Table 3 Parameters Extracted from the Meta-Analyses Indicative of Pooled Efficacy of Anti-Inflammatory Agents |
Celecoxib
All meta-analyses demonstrated superiority of celecoxib over placebo. SMD ranged between −0.82 and 3.43 for mean difference, signs depending on the calculation method. One study calculated WMD of 3.26. Those meta-analyses yielded none or low heterogeneity of 0% or 33%. Six meta-analyses calculated pooled response rates, also resulting in superiority of celecoxib. As for risk ratios, the risk of becoming a responder is 1.55 or 1.88 times higher under exposure to celecoxib than becoming a responder under placebo condition. As for odds ratios, responders have between 6.49 and 9.23 times higher risk of having been exposed to celecoxib as compared to the placebo condition. Heterogeneity of studies was not present. Five meta-analyses calculated pooled remission rates, again resulting in superiority of celecoxib. As for risk ratio, the risk of becoming a remitter is 4.11 times higher under exposure to celecoxib than becoming a responder under placebo condition. As for odds ratios, remitters have between 6.47 and 7.89 times higher risk of having been exposed to celecoxib as compared to the placebo condition. No heterogeneity was present. Details on the results for celecoxib are displayed in Table 3. The reported meta-analyses are based on three to four studies and thus have a high overlap in those (see Supplementary Table 3B).
Omega 3 Fatty Acids
Twelve meta-analyses demonstrated superiority of omega 3 fatty acids over placebo. SMD ranged between −0.91 and 1.243 for mean difference, signs depending on the calculation method, and one meta-analysis calculated Hedges’ g of 0.608. Those meta-analyses yielded none to substantial heterogeneity between 0% and 87.4%. One study with two meta-analyses did not show superiority of omega 3 fatty acids for mean difference (pooled MD of 0.42 and SMD of 0.50). Heterogeneity was found to be moderate at 35.7% and considerable at 94.1%. Two meta-analyses calculated pooled response rates, not demonstrating superiority of omega 3 fatty acids. Here, heterogeneity of 6% and 30% was low. One meta-analysis calculated pooled remission rates, also not showing superiority of omega 3 fatty acids and a low heterogeneity of 7%. Details on the results are displayed in Table 3. The reported meta-analyses are based on 2 to 25 studies resulting in a low to moderate overlap (see Supplementary Tables 3C.1–3C.3). This seems a specialty of the omega 3 fatty acids meta-analyses at least partly due to a higher variety in populations of interest (see section study characteristics).
Multiple Agents
One meta-analysis included celecoxib and infliximab showing an SMD of −0.54 at the border of significance and substantial heterogeneity of 68%. Details are presented in Table 3. The reported results are based on five studies; a statement on overlap is obsolete (see Supplementary Table 3D).
Overall Overview
Figure 3A and B show a Forrest plot for mean differences to provide an easy to grasp overview of the reviewed data and thus the strength and consistency across meta-analyses. Depending on the calculation method of mean differences, positive and negative values can occur. To avoid misleading interpretation, positive and negative values are displayed as separate figures. Similarly, like for mean differences, Figure 4 shows a Forrest plot for risk ratios and odds ratios, separately for response and remission rates.
Figure 3 Continued.
 |
Figure 4 Risk ratios and odds ratios from meta-analyses by agent for response and remission. Abbreviations: RCTs, randomized controlled trials; RR, risk ratio; OR, odds ratio. |
Discussion
Summary of Main Findings
In total, 20 meta-analyses were analyzed, some of which provided multiple effect estimates. Investigated agents were minocycline, celecoxib, omega 3 fatty acids, and a combination of celecoxib and infliximab. All meta-analyses included RCTs only. A diversity of characteristics was observed regarding included study populations, sample size, outcome scales, treatment regimen, the variety of dosages for omega 3 fatty acids (different combination or monotherapy of EPA and DHA), and year of publication. Characteristics were quite consistent for meta-analyses on celecoxib, rather consistent for meta-analyses on minocycline, and rather diverse for meta-analyses on omega 3 fatty acids. Noteworthy, only few single studies were available for celecoxib and minocycline which were included in multiple meta-analyses.
Interpreting results, SMD corresponds to Cohen’s d and Hedges’ g is the adjusted Cohen’s d and thus approximates it.133,134 Minocycline showed superiority over placebo conditions in three meta-analyses with medium to large effect size in mean difference and substantial heterogeneity in single study effect sizes. Findings on response rates are in accordance with these results. Two meta-analyses with similar effect sizes did not deliver significant superiority of minocycline. Those included only the same two studies and had the highest heterogeneity. In general, a high overlap in studies was present between the meta-analyses, thus leading to high overlap in investigated patient populations. Celecoxib showed superiority over placebo conditions in five meta-analyses with large and very large effect size in mean difference (at the border of medium to large effect size in one case) and with practically no heterogeneity in single study effect sizes. Effect sizes diverge more than in the minocycline meta-analyses even though a very high overlap in included studies exists also. For response and remission rates a large effect is present as well. Omega 3 fatty acids showed superiority over placebo conditions in twelve meta-analyses with mainly small and medium effect sizes in mean differences, but also a large effect size in two cases, and with substantial heterogeneity and negligible heterogeneity in one case. These effect sizes have a smaller range than for celecoxib but a higher range in heterogeneity. Two meta-analyses with small to medium effect sizes did not deliver significant superiority of omega 3 fatty acids. Those had moderate to considerable heterogeneity and included only two and three studies, respectively. Also, for response and remission rates no significant effects emerged with negligible heterogeneity. In omega 3 fatty acids meta-analyses, much less overlap in included studies was present than in minocycline and celecoxib meta-analyses. Only Martins et al and Lin et al as well as Martins et al and Appleton et al had a rather high overlap in included studies, thus leading to rather high overlap in therapy regimen, sample sizes, patient populations, outcome scales, SMD, and p-values.53,54,56 In general, the small overlap in included studies may be due to different main research questions in the omega 3 fatty acids meta-analyses. Lastly, the mixed agents study almost showed superiority of anti-inflammatory treatment over placebo with a medium effect size and substantial heterogeneity.
Heterogeneity
Notably, in general when response or remission rates were evaluated, heterogeneity was almost in every case at 0% as compared to much higher heterogeneity for pooled mean differences. This observation was also made by Alba et al.135 The authors state that one potential explanation for this phenomenon is the precision of included studies in a meta-analysis.135 As continuous outcomes have more statistical power, they result in narrower confidence intervals.135 Combining results with narrow confidence intervals can then lead to higher heterogeneity since these confidence intervals may have a smaller overlap and differences in study effects for the I2 statistic are created. Further, meta-analyses with continuous outcomes seemed to produce higher heterogeneity the more studies were included as opposed to meta-analyses with binary outcomes.135 Vice versa, with lower precision of study results and a higher confidence interval, heterogeneity is smaller, which appears to be more prevalent in meta-analyses investigating studies with binary outcomes.135 The celecoxib meta-analysis showed a heterogeneity of 0% independently of a continuous or a binary outcome. This may speak for the strength of the results since single studies seem to produce similar effects. Indeed, for mean differences the confidence intervals were highly overlapping, but also small explaining the highly significant results.45 The same can be observed for response rates, while a high overlap but also large confidence intervals exist for remission rates.45 For the minocycline meta-analyses, the described differences in heterogeneity depending on the outcome are present. For mean differences, the confidence intervals are largely overlapping but not as much as in celecoxib studies.43,45 For response rates, the confidence interval of one study contains the confidence interval of the other study entirely which may explain the low heterogeneity.47 The omega 3 fatty acids meta-analyses show a similar trend, even though with dichotomous outcomes heterogeneity is larger than 0%. For mean differences, the confidence intervals of single studies vary in range and are less overlapping, while for dichotomous outcomes single studies presented much larger confidence intervals and thus are overlapping to a greater extent.56 However, variety seems larger than in celecoxib and minocycline studies supporting the idea of Alba et al of higher heterogeneity the more studies are included.135 This may be attributed to a larger sample size which leads to even smaller confidence intervals and thus less overlap. Indeed, the omega 3 fatty acids meta-analyses included the most studies, thus the largest sample sizes, and have the smallest confidence intervals (see Figures 3A and B and 4). Further, between the omega 3 fatty acids meta-analyses exists higher variety in the number of included studies as compared to minocycline and celecoxib meta-analyses. Noteworthy, it is difficult to compare the statistical indices numerically between the meta-analyses due to different statistical methods which result in different numeric outcome estimates and confidence intervals. Thus, the described observations rather refer to the consistency of patterns noticed within the respective meta-analyses. However, Russo proposes that the statistical methods are less relevant than the determination of combinability of studies prior to statistical testing.136 In case of critical heterogeneity in study characteristics statistical methods cannot account for erroneous combination attempts.136 The analyzed meta-analyses of the present systematic review often did not report sufficiently on defined criteria for data combination (only 6 out of 18 rated meta-analysis fulfilled this criterion on subitem 9A) and a priori testing of heterogeneity guiding this decision.
It is important to note that heterogeneity test results are often misinterpreted.136 These tests do not validate the similarity of studies to be combined in meta-analysis but test the hypothesis whether effect sizes of single studies are sufficiently equal to guide the decision to calculate a pooled effect estimate.136 Variability in study characteristics can influence the study’s effect size and differences in (the variability of) those characteristics between studies can deliver an explanation for heterogenous effect sizes and the strength of evidence from meta-analysis. In the present work, next to statistical aspects, potential sources of heterogeneity may lie in the study characteristics. In the celecoxib meta-analyses very little diversity of certain characteristics can be observed: same outcome scales were used, add-on studies exclusively, high overlap of single studies included in meta-analyses and thus overlap in included populations. In the minocycline meta-analyses, somewhat higher diversity in characteristics was present: two outcome scales, monotherapy and add-on regimen, but on the other hand, a high overlap of single studies included and thus overlap in included populations. For the omega 3 fatty acids meta-analyses, the highest variability in characteristics was present: multiple outcome scales, monotherapy and add-on regimen, composition of omega 3 treatment with different dosages and different placebo agents, low overlap of single studies included and thus higher variety in included populations.
Diagnostic Misclassification
During the conduct of the present systematic review, some obstacles occurred. First, studies often consider bipolar depression a similar pathology as unipolar depression, while differences in biological underpinnings, especially in immune disturbances, have barely been investigated. Thus, the present work focusses on unipolar depression, exclusively, to provide higher clinical relevance of findings. Many meta-analyses that were excluded throughout the selection process, especially on omega 3 fatty acids, claimed to have investigated MDD patients while the samples from the single studies included mixed diagnoses and some based patient inclusion solely on the score of a depression rating scale (see Supplementary Table 1). Appleton et al and Mocking et al, for example, included studies with diagnosed MDD patients and included an eligible diagnosed MDD subset if samples were mixed with non-diagnosed depressive symptoms (like in the study of Lucas et al).56,57,114 Much caution is needed to disentangle the diagnostic status of included populations, while the inclusion of an MDD sample is sometimes claimed improvidently. This often makes it necessary to carefully review the eligibility criteria for patients in the single studies included in the meta-analyses. It would be interesting though to compare treatment efficacy of meta-analyses on diagnosed MDD populations versus populations with depressive symptoms as measured by standard rating scales.
Treatment Regimen
A critical aspect is the use of different treatment regimen in add-on studies, which make it difficult to deduce specific treatment recommendations from meta-analytical results. Furthermore, not all meta-analyses provided information on what defined treatment as usual (eg, Rosenblat et al).43 Additionally, the validity of placebo in the omega 3 fatty acid studies can be questioned since other types of oil may also be defined as an active comparator, at least if an anti-inflammatory mechanism of action cannot be ruled out entirely. Lastly, on meta-analytical level one publication included combined agents of interest.51 To formulate recommendations for treatment, this approach seems rather counterproductive because it again does not provide specific information.
Outcomes
A problem with combining different rating scales in one meta-analysis arises from their differences in sensitivity to changing symptoms, which in turn questions the comparability of changes in symptom scores. Another considerable aspect is the choice of values for continuous outcomes which has been discussed by Andrade.137 Some studies assess the endpoint values as efficacy outcome, which can only be positive values, and some studies assess the score change from baseline to endpoint, which can be positive or negative values depending on how the difference was calculated and whether values increased or decreased.137 Different outcome values must be interpreted differently, and pooled effect sizes are thus difficult to compare between meta-analyses and should not be pooled in one meta-analysis in general. The presented meta-analyses often analyzed the score change (eg, Bai et al, Köhler-Forsberg et al).45,46 Some of them analyzed the endpoint score (eg, Zheng et al, Jeremiah et al).44,62 Further, the choice of outcome values may not be stated, so it is not possible to judge comparability appropriately (eg, Wei-Hong et al).59 All meta-analyses on mean differences for celecoxib used the score change which strengthens the comparability of effect sizes and conclusions drawn from these investigations.
Quality Assessment
Summarizing findings from the quality assessment, a variable quality of meta-analyses and a highly variable quality of respective included studies become apparent. According to Figure 2, the conduct of study selection and data extraction by at least two independent investigators (item 2) and the usage of multiple databases, an a priori defined search strategy, and additional sources (item 3) were the strongest domains overall. Sufficient provision of study characteristics (item 6) and the consideration of scientific quality in the conclusions (item 8) were the weakest domains overall. Consequently, even if the overall scientific quality of a meta-analysis may be satisfactory, drawing conclusions while neglecting single study quality can result in misleading clinical practices. Thus, the quality in design and reporting of meta-analyses still offers potential for improvement. Further, rating of quality can be improved. For example, the rating of potential publication bias (item 10) remains unsatisfactory since the R-AMSTAR assesses whether meta-analyses consider publication bias at all, but not whether publication bias is actually present or not. Thus, from quality assessment a potential publication bias does not become apparent, which however has relevance to the confidence of interpretation of results. Lastly, the way of scoring may be revisited as the minimum score is 11 points corresponding to a high lack of quality parameters. This seems misleading considering that 25% of the total possible score indicates poor quality.
General discussion
In the following paragraphs some more general aspects are discussed. There are other agents like glucocorticoids, statins, or pioglitazone investigated in meta-analyses that are considered anti-inflammatory by some authors.45–47 Those were not included in the present work for the following reasons: in depression a known glucocorticoid resistance and consequently lacking downregulation of inflammation exists, which questions the potential benefit and makes it difficult to assess efficacy.138 Seemingly, statins and pioglitazone only have an indirect anti-inflammatory action.
Efficacy is not only an matter of heterogeneity but also in addressing the correct pathophysiological mechanism. If anti-inflammatory drugs are efficacious, it can be assumed that those reduce inflammatory markers. However, the application of anti-inflammatory agents does not necessarily correlate to such reduction in the course of treatment.20,32–34 It is thus important to make well-considered decisions on which mechanism in the inflammatory pathway should be addressed and which markers should be determined to measure treatment success also on the molecular level. This will also lead to stronger prospective studies where treatment response can be predicted by certain levels of biomarkers that correspond to the chosen agents. These studies should provide a better understanding of mechanisms for tailored treatment choice and thus efficacy improvement.
Despite the more uniform and larger effect for change in depressive symptomatology of antidepressants compared to placebo, antidepressant efficacy is still an issue to discuss due to considerable and variable placebo effects.139–141 Thus, the alternative anti-inflammatory agents were introduced to increase treatment response. However, most studies investigated these agents in add-on study designs, so the true efficacy is difficult to estimate. This is due to the usage of active antidepressant comparators which imply an inestimable placebo effect. A study design comparing the anti-inflammatory agent to a sole placebo can provide more specific information on the gain in efficacy and potentially spare patients multiple drug regimens but is mostly not done due to ethical reasons. Consequently, combining monotherapy and add-on studies in a meta-analysis is critical (many of the meta-analyses presented here did that; see also Table 1), because both designs have different implications for the interpretation of efficacy and the gain over antidepressants can only be estimated when add-on designs are included solely.
Lastly, meta-analyses should be updated regularly as new literature emerges. For example, contrary findings for celecoxib and minocycline were published just recently suggesting no gain in efficacy for celecoxib or minocycline over the placebo condition (add-on designs) as opposed to rather strong evidence found in the presented meta-analyses.20,34,37 A general shortcoming in this research field is the investigation of MDD patients without considering the inflammatory status. In this regard it would be interesting to take the duration of disease into account, which was rarely reported in the meta-analyses, unfortunately. Assuming that patients with a long disease history are rather treatment refractory to standard antidepressant regimen, an anti-inflammatory treatment may generate a larger effect size compared to standard treatment/placebo in those patients. This is supported by the notion that treatment resistance seems to go along with inflammatory activation.19–21 A systematic review evaluated response to anti-inflammatory regimen in patient subgroups with and without inflammatory activation, which suggested that patients with an inflammatory signature had higher response rates to such regimen than patients without an inflammatory signature.19 The benefit of patient stratification is also supported by recently published trials on minocycline and celecoxib.20,34 An eminent shortcoming is that the trials summarized in the meta-analyses analyzed here included MDD patients regardless of their immune status or other known subtypes. A remaining challenge for stratification is the determination of reliable biomarkers or rather their cut-off values to distinguish inflamed and non-inflamed patient subgroups. The relevance, however, of developing precision medicine to improve treatment success using inflammatory biomarkers is an important goal for the future and has also been pointed out in recent literature.142
Limitations
Several limitations apply to the present work. Apart from the databases no additional sources and only meta-analyses in English language were “searched”. Further, publication bias was not assessable since many meta-analyses provided funnel plots only across multiple agents (eg, Köhler-Forsberg et al) but not per single agent.45 Thus, the information of interest to this review could not be extracted.
Furthermore, certain characteristics were not considered in the present investigation. First, age of patients could be interesting to add to the description of characteristics because a positive association with inflammation is known.143 Second, different treatment duration in the studies and their variety when combined in meta-analyses may pose an important contributor to heterogeneity. In general, treatment duration should be an issue for discussion in this research field since the inflammatory state in depression is considered to be a chronic low-grade inflammation.144 Third, different depression severity should be considered because it may influence the efficacy of certain drugs and may thus also have a critical impact for heterogeneity. Fourth, some meta-analyses included patients with comorbid inflammatory or immune system diseases that partly makes it difficult to discriminate treatment effects on depression. Fifth, an evaluation of different inclusion and exclusion criteria in meta-analyses may be interesting as they represent different research questions leading to inclusion of a different set of studies. Subgroup analyses should be conducted in future studies considering these variables.
In general, it is important to discuss the generalizability of study results. With respect to this review, different populations included in the meta-analyses increase the overall generalizability of findings from the various meta-analyses to a larger population. This is especially the case for omega 3 fatty acids studies, which also showed the highest variability in other characteristics. The generalizability and transfer to clinical practice is limited for highly controlled study conditions, as is the case for celecoxib meta-analyses with high consistency of characteristics across the included studies. On the other hand, applicable data for transfer to clinical guidelines, eg, information on which patient group benefits from the treatment and which dose should be administered, can hardly be concluded from results based on large variety and thus limits individualized approaches. Highly controlled study conditions are more likely to produce strong evidence (high internal validity). Consequently, weighing a limited broadness of applicability against the possibility to deduce clear conditions of application is a challenging task.
A general aspect that poses a limitation to this research field is the little understanding of the linkage between peripheral inflammatory processes and the central nervous system. Some authors discuss connecting routes in depression where immune cells and inflammatory compounds can enter the central nervous system via the blood-brain-barrier.145,146 However, further research is warranted to elucidate how treating peripheral inflammation may affect central inflammation and reduce depressive symptoms.
Conclusion
Altogether, the presented meta-analyses demonstrate an overall significant benefit for the use of anti-inflammatory treatment regimen in major depressive disorder. However, several limitations and challenges were identified: differences between the agents are evident, where heterogeneity and diversity of characteristics, especially in omega 3 fatty acid studies, play an important role for the strength of evidence. Even though the inclusion criteria for this systematic review were defined rather homogeneous, heterogeneity can be found in several aspects like patient characteristics, treatment regimen, comparators, outcome scales and outcome values. Further, mixed scientific quality of meta-analyses with lacking definition of combination criteria, lacking consideration of quality for conclusions, and lacking rating of existence of publication bias also contributes to rather reserved conclusions about the strength of evidence. Diagnostic misclassification poses an additional challenge. Thus, methodological issues prevent the discovery of the true potential of such treatment strategies for a specific patient group and methodologically strong studies and meta-analyses are needed. However, based on the strength of evidence a ranking of agents and thus their potential for clinical applicability can be deduced: celecoxib > minocycline > omega 3 fatty acids. In future research, the named shortcomings regarding the conduct, reporting, and quality assessment of meta-analyses should be addressed. Further, biomarkers indicating inflamed patients should be investigated comprehensively to establish patient immune profiles that guide stratification for an appropriate treatment choice. Efficacy studies and meta-analyses should then be carried out again to shape clinical treatment guidelines. Further, a comprehensive analysis of safety should be carried out.
Registration and Protocol
This review was registered at PROSPERO under the registration number CRD42022296596 (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=296596). A protocol was prepared in advance of conducting the study.
Acknowledgments
This work is part of a Master’s thesis of the Master’s Program in Clinical Research, Dresden International University, Dresden, Germany.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
TS received grants from the German Federal Ministry of Health and Kurt Goldstein Institut that were not related to this study. TS received royalties from AstraZeneca for consulting and from Dresden International University for serving as program director and lecturer of the Master’s Program in Clinical Research. TS is editorial board member at Neuropsychiatric Disease and Treatment. BI reports financial interest in NOVA discovery and Biomind that were not related to this study. BI serves as program director and lecturer for the Master’s Program in Clinical Research at Dresden International University. MSS, GAH, and AFA declare no potential conflicts of interest.
References
1. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
2. Bauer M, Monz BU, Montejo AL, et al. Prescribing patterns of antidepressants in Europe: results from the Factors Influencing Depression Endpoints Research (FINDER) study. Eur Psychiatry. 2008;23(1):66–73. doi:10.1016/j.eurpsy.2007.11.001
3. Chee K-Y, Tripathi A, Avasthi A, et al. International study on antidepressant prescription pattern at 40 major psychiatric institutions and hospitals in Asia: a 10-year comparison study. Asia Pac Psychiatry. 2015;7(4):366–374. doi:10.1111/appy.12176
4. Treviño LA, Ruble MW, Treviño K, Weinstein LM, Gresky DP. Antidepressant medication prescribing practices for treatment of major depressive disorder. Psychiatr Serv. 2017;68(2):199–202. doi:10.1176/appi.ps.201600087
5. Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184–191. doi:10.1111/j.1600-0447.2009.01519.x
6. Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman ATF. Recurrence of major depressive disorder and its predictors in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Psychol Med. 2013;43(1):39–48. doi:10.1017/S0033291712002395
7. Mahlich J, Tsukazawa S, Wiegand F. Estimating prevalence and healthcare utilization for treatment-resistant depression in japan: a retrospective claims database study. Drugs Real World Outcomes. 2018;5(1):35–43. doi:10.1007/s40801-017-0126-5
8. Coppen A, Brooksbank BWL, Peet M. Tryptophan concentration in the cerebrospinal fluid of depressive patients. Lancet. 1972;299(7765):1393. doi:10.1016/S0140-6736(72
9. McClure DJ. The role of dopamine in depression. Can Psychiatr Assoc J. 1973;18(4):309012.
10. Schildkraut JJ. The catecholamine hypothesis of affective disorders: a review of supporting evidence. Am J Psychiatry. 1965;122(5):509–522. doi:10.1176/ajp.122.5.509
11. Köhler CA, Freitas TH, Maes M, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. 2017;135(5):373–387. doi:10.1111/acps.12698
12. Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD. Inflammatory markers in depression: a meta-analysis of mean differences and variability in 5166 patients and 5083 controls. Brain Behav Immun. 2020;87:901–909. doi:10.1016/j.bbi.2020.02.010
13. Myint AM. Kynurenines: from the perspective of major psychiatric disorders. FEBS J. 2012;279(8):1375–1385. doi:10.1111/j.1742-4658.2012.08551.x
14. Arteaga-Henriquez G, Burger B, Weidinger E, et al. Activation and deactivation steps in the tryptophan breakdown pathway in major depressive disorder: a link to the monocyte inflammatory state of patients. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110226. doi:10.1016/j.pnpbp.2020.110226
15. Grosse L, Carvalho LA, Birkenhager TK, et al. Circulating cytotoxic T cells and natural killer cells as potential predictors for antidepressant response in melancholic depression. Restoration of T regulatory cell populations after antidepressant therapy. Psychopharmacology. 2016;233:1679–1688. doi:10.1007/s00213-015-3943-9
16. Grosse L, Hoogenboezem T, Ambrée O, et al. Deficiencies of the T and natural killer cell system in major depressive disorder. T regulatory cell defects are associated with inflammatory monocyte activation. Brain Behav Immun. 2016;54:38–44. doi:10.1016/j.bbi.2015.12.003
17. Schiweck C, Valles-Colomer M, Arolt V, et al. Depression and suicidality: a link to premature T helper cell aging and increased Th17 cells. Brain Behav Immun. 2020;87:603–609. doi:10.1016/j.bbi.2020.02.005
18. Simon MS, Schiweck C, Arteaga-Henríquez G, et al. Monocyte mitochondrial dysfunction, inflammaging, and inflammatory pyroptosis in major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2021;111:110391. doi:10.1016/j.pnpbp.2021.110391
19. Arteaga-Henríquez G, Simon MS, Burger B, et al. Low-grade inflammation as a predictor of antidepressant and anti-inflammatory therapy response in MDD patients: a systematic review of the literature in combination with an analysis of experimental data collected in the EU-moodinflame consortium. Front Psychiatry. 2019;10:458. doi:10.3389/fpsyt.2019.00458
20. Simon MS, Burger B, Weidinger E, et al. Efficacy of sertraline plus placebo or add-on celecoxib in major depressive disorder: macrophage migration inhibitory factor as a promising biomarker for remission after sertraline - results from a randomized controlled clinical trial. Front Psychiatry. 2021;12:615261. doi:10.3389/fpsyt.2021.615261
21. Strawbridge R, Arnone D, Danese A, Papadopoulos A, Herane Vives A, Cleare AJ. Inflammation and clinical response to treatment in depression: a meta-analysis. Eur Neuropsychopharmacol. 2015;25(10):1532–1543. doi:10.1016/j.euroneuro.2015.06.007
22. Freeman MP, Davis M, Sinha P, Wisner KL, Hibbeln JR, Gelenberg AJ. Omega-3 fatty acids and supportive psychotherapy for perinatal depression: a randomized placebo-controlled study. J Affect Disord. 2008;110(1–2):142–148. doi:10.1016/j.jad.2007.12.228
23. Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680–684. doi:10.1038/sj.mp.4001805
24. Ghlichloo I, Gerriets V. Nonsteroidal anti-inflammatory drugs (NSAIDs). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
25. Billmeier U, Dieterich W, Neurath MF, Atreya R. Molecular mechanism of action of anti-tumor necrosis factor antibodies in inflammatory bowel diseases. World J Gastroenterol. 2016;22(42):9300–9313. doi:10.3748/wjg.v22.i42.9300
26. Ershad M, Naji A, Vearrier D. N acetylcysteine. In: StatPearls. Treasure Island (FL): StatPearls Publishing;; 2022.
27. Pedre B, Barayeu U, Ezeriņa D, Dick TP. The mechanism of action of N-acetylcysteine (NAC): the emerging role of H2S and sulfane sulfur species. Pharmacol Ther. 2021;228:107916. doi:10.1016/j.pharmthera.2021.107916
28. Garrido-Mesa N, Zarzuelo A, Gálvez J. Minocycline: far beyond an antibiotic. Br J Pharmacol. 2013;169(2):337–352. doi:10.1111/bph.12139
29. Nazarian S, Akhondi H. Minocycline. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
30. Krupa K, Fritz K, Parmar M. Omega-3 fatty acids. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
31. Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor-alpha antagonist infliximab in treatment resistant depression: role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31–41. doi:10.1001/2013.jamapsychiatry.4
32. Hasebe K, Gray L, Bortolasci C, et al. Adjunctive N-acetylcysteine in depression: exploration of interleukin-6, C-reactive protein and brain-derived neurotrophic factor. Acta Neuropsychiatr. 2017;29(6):337–346. doi:10.1017/neu.2017.2
33. Musil R, Schwarz MJ, Riedel M, et al. Elevated macrophage migration inhibitory factor and decreased transforming growth factor-beta levels in major depression — no influence of celecoxib treatment. J Affect Disord. 2011;134(1–3):217–225. doi:10.1016/j.jad.2011.05.047
34. Nettis MA, Lombardo G, Hastings C, et al. Augmentation therapy with minocycline in treatment-resistant depression patients with low-grade peripheral inflammation: results from a double-blind randomised clinical trial. Neuropsychopharmacology. 2021;46(5):939–948. doi:10.1038/s41386-020-00948-6
35. Husain MI, Chaudhry IB, Husain N, et al. Minocycline as an adjunct for treatment-resistant depressive symptoms: a pilot randomised placebo-controlled trial. J Psychopharmacol. 2017;31(9):1166–1175. doi:10.1177/0269881117724352
36. Su K-P, Huang S-Y, Chiu T-H, et al. Omega-3 fatty acids for major depressive disorder during pregnancy: results from a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2008;69(4):644–651. doi:10.4088/jcp.v69n0418
37. Baune BT, Sampson E, Louise J, et al. No evidence for clinical efficacy of adjunctive celecoxib with vortioxetine in the treatment of depression: a 6-week double-blind placebo controlled randomized trial. Eur Neuropsychopharmacol. 2021;53:34–46. doi:10.1016/j.euroneuro.2021.07.092
38. Mischoulon D, Nierenberg AA, Schettler PJ, et al. A double-blind, randomized controlled clinical trial comparing eicosapentaenoic acid versus docosahexaenoic acid for depression. J Clin Psychiatry. 2015;76(1):54–61. doi:10.4088/JCP.14m08986
39. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
40. Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions.
41. Kung J, Chiappelli F, Cajulis OO, et al. From systematic reviews to clinical recommendations for evidence-based health care: validation of Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J. 2010;4:84–91. doi:10.2174/1874210601004020084
42. PEROSH OSH Evidence Group. PEROSH - OSH evidence. Clearinghouse of systematic reviews. METHODS; 2014. Available from: https://perosh.eu/wp-content/uploads/2013/06/PEROSH-Clearinghouse-Methods_Last-update-June-2014.pdf.
43. Rosenblat JD, McIntyre RS. Efficacy and tolerability of minocycline for depression: a systematic review and meta-analysis of clinical trials. J Affect Disord. 2018;227:219–225. doi:10.1016/j.jad.2017.10.042
44. Zheng W, Zhu X-M, Zhang Q-E, et al. Adjunctive minocycline for major mental disorders: a systematic review. J Psychopharmacol. 2019;33(10):1215–1226. doi:10.1177/0269881119858286
45. Köhler-Forsberg O, Lydholm CN, Hjorthøj C, Nordentoft M, Mors O, Benros ME. Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: meta-analysis of clinical trials. Acta Psychiatr Scand. 2019;139(5):404–419. doi:10.1111/acps.13016
46. Bai S, Guo W, Feng Y, et al. Efficacy and safety of anti-inflammatory agents for the treatment of major depressive disorder: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91(1):21–32. doi:10.1136/jnnp-2019-320912
47. Hang X, Zhang Y, Li J, et al. Comparative efficacy and acceptability of anti-inflammatory agents on major depressive disorder: a network meta-analysis. Front Pharmacol. 2021;12:691200. doi:10.3389/fphar.2021.691200
48. Faridhosseini F, Sadeghi R, Farid L, Pourgholami M. Celecoxib: a new augmentation strategy for depressive mood episodes. A systematic review and meta-analysis of randomized placebo-controlled trials. Hum Psychopharmacol. 2014;29(3):216–223. doi:10.1002/hup.2401
49. Na KS, Lee KJ, Lee JS, Cho YS, Jung HY. Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:79–85. doi:10.1016/j.pnpbp.2013.09.006
50. Na KS, Lee KJ, Lee JS, Cho YS, Jung HY. Corrigendum to “Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis” [Prog Neuropsychopharmacol Biol Psychiatry 48 (3 January 2014) 79–85]. Prog Neuropsychopharmacol Biol Psychiatry. 2016;66:136. doi:10.1016/j.pnpbp.2015.11.011
51. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12):1381–1391. doi:10.1001/jamapsychiatry.2014.1611
52. Yuan Z, Chen Z, Xue M, Zhang J, Leng L. Application of antidepressants in depression: a systematic review and meta-analysis. J Clin Neurosci. 2020;80:169–181. doi:10.1016/j.jocn.2020.08.013
53. Martins JG, Bentsen H, Puri BK. Eicosapentaenoic acid appears to be the key omega-3 fatty acid component associated with efficacy in major depressive disorder: a critique of Bloch and Hannestad and updated meta-analysis. Mol Psychiatry. 2012;17(12):1144–1167. doi:10.1038/mp.2012.25
54. Lin P-Y, Mischoulon D, Freeman MP, et al. Are omega-3 fatty acids antidepressants or just mood-improving agents? The effect depends upon diagnosis, supplement preparation, and severity of depression. Mol Psychiatry. 2012;17(12):1161–1167. doi:10.1038/mp.2012.111
55. Grosso G, Pajak A, Marventano S, et al. Role of omega-3 fatty acids in the treatment of depressive disorders: a comprehensive meta-analysis of randomized clinical trials. PLoS One. 2014;9(5):e96905. doi:10.1371/journal.pone.0096905
56. Appleton KM, Sallis HM, Perry R, Ness AR, Churchill R. Omega-3 fatty acids for depression in adults. Cochrane Database Syst Rev. 2015;11:CD004692. doi:10.1002/14651858.CD004692.pub4
57. Mocking RJT, Harmsen I, Assies J, Koeter MWJ, Ruhé HG, Schene AH. Meta-analysis and meta-regression of omega-3 polyunsaturated fatty acid supplementation for major depressive disorder. Transl Psychiatry. 2016;6(3):e756. doi:10.1038/tp.2016.29
58. Sarris J, Murphy J, Mischoulon D, et al. Adjunctive nutraceuticals for depression: a systematic review and meta-analyses. Am J Psychiatry. 2016;173(6):575–587. doi:10.1176/appi.ajp.2016.15091228
59. Wei-Hong L, Cheng-Gui Z, Peng-Fei G, Heng L, Jian-Fang Y. Omega-3 fatty acids as monotherapy in treating depression in pregnant women: a meta-analysis of randomized controlled trials. Iran J Pharm Res. 2017;16(4):1593–1599.
60. Schefft C, Kilarski LL, Bschor T, Köhler S. Efficacy of adding nutritional supplements in unipolar depression: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2017;27(11):1090–1109. doi:10.1016/j.euroneuro.2017.07.004
61. Luo X-D, Feng J-S, Yang Z, et al. High-dose omega-3 polyunsaturated fatty acid supplementation might be more superior than low-dose for major depressive disorder in early therapy period: a network meta-analysis. BMC Psychiatry. 2020;20(1):248. doi:10.1186/s12888-020-02656-3
62. Jeremiah OJ, Cousins G, Boland F, Kirby BP, Ryan BK. Evaluation of the effect of insulin sensitivity-enhancing lifestyle- and dietary-related adjuncts on antidepressant treatment response: a systematic review and meta-analysis. Heliyon. 2020;6(9):e04845. doi:10.1016/j.heliyon.2020.e04845
63. Chambergo-Michilot D, Brañez-Condorena A, Falvy-Bockos I, Pacheco-Mendoza J, Benites-Zapata VA. Efficacy of omega-3 supplementation on sertraline continuous therapy to reduce depression or anxiety symptoms: a systematic review and meta-analysis. Psychiatry Res. 2021;296:113652. doi:10.1016/j.psychres.2020.113652
64. Lin P-Y, Su K-P. A meta-analytic review of double-blind, placebo-controlled trials of antidepressant efficacy of omega-3 fatty acids. J Clin Psychiatry. 2020;81(5):19r13106. doi:10.4088/JCP.19r13106
65. Kraguljac NV, Montori VM, Pavuluri M, Chai HS, Wilson BS, Unal SS. Efficacy of omega-3 fatty acids in mood disorders - a systematic review and metaanalysis. Psychopharmacol Bull. 2009;42(3):39–54.
66. Marins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525–542. doi:10.1080/07315724.2009.10719785
67. Sublette ME, Ellis SP, Geant AL, Mann JJ. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577–1584. doi:10.4088/JCP.10m06634
68. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis. Mol Psychiatry. 2012;17(12):127212–127282. doi:10.1038/mp.2011.100
69. Yang R-J, Han D, Qiao Z-X, Tian X, Qi D, Qiu X-H. Combined application of eicosapentaenoic acid and docosahexaenoic acid on depression in women: a meta-analysis of double-blind randomized controlled trials. Neuropsychiatr Dis Treat. 2015;11:2055–2061. doi:10.2147/NDT.S86581
70. Fernandez BS, Dean OM, Dodd S, Malhi GS, Berk M. N-acetylcysteine in depressive symptoms and functionality: a systematic review and meta-analysis. J Clin Psychiatry. 2016;77(4):e457–e466. doi:10.4088/JCP.15r09984
71. Hallahan B, Ryan T, Hibbeln JR, et al. Efficacy of omega-3 highly unsaturated fatty acids in the treatment of depression. Br J Psychiatry. 2016;209(3):192–201. doi:10.1192/bjp.bp.114.160242
72. Husain MI, Strawbridge R, Stokes PR, Young AH. Anti-inflammatory treatments for mood disorders: systematic review and meta-analysis. J Psychopharmacol. 2017;31(9):1137–1148. doi:10.1177/0269881117725711
73. Bae J-H, Kim G. Systematic review and meta-analysis of omega-3-fatty acids in elderly patients with depression. Nutr Res. 2018;50:1–9. doi:10.1016/j.nutres.2017.10.013
74. Bai Z-G, Bo A, Wu S-J, Gai Q-Y, Chi I. Omega-3 polyunsaturated fatty acids and reduction of depressive symptoms in older adults: a systematic review and meta-analysis. J Affect Disord. 2018;241:241–248. doi:10.1016/j.jad.2018.07.057
75. Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry. 2018;23(2):335–343. doi:10.1038/mp.2016.167
76. Liao Y, Xie B, Zhang H, et al. Efficacy of omega-3 PUFAs in depression: a meta-analysis. Transl Psychiatry. 2019;9(1):190. doi:10.1038/s41398-019-0515-5
77. Bavaresco DV, Uggioni MLR, Ferraz SD, et al. Efficacy of infliximab in treatment-resistant depression: a systematic review and meta-analysis. Pharmacol Biochem Behav. 2020;188:172838. doi:10.1016/j.pbb.2019.172838
78. Cai DB, Zheng W, Zhang QE, et al. Minocycline for depressive symptoms: a meta-analysis of randomized, double-blinded, placebo-controlled trials. Psychiatr Q. 2020;91(2):451–461. doi:10.1007/s11126-019-09707-3
79. Kishi T, Miyake N, Okuya M, Sakuma K, Iwata N. N-acetylcysteine as an adjunctive treatment for bipolar depression and major depressive disorder: a systematic review and meta-analysis of double-blind, randomized placebo-controlled trials. Psychopharmacology. 2020;237(11):3481–3487. doi:10.1007/s00213-020-05629-2
80. Mocking RJT, Steijn K, Roos C, et al. Omega-3 fatty acid supplementation for perinatal depression: a meta-analysis. J Clin Psychiatry. 2020;81(5):19r13106. doi:10.4088/JCP.19r13106
81. Zhang MM, Zou Y, Li SM, et al. The efficacy and safety of omega-3 fatty acids on depressive symptoms in perinatal women: a meta-analysis of randomized placebo-controlled trials. Transl Psychiatry. 2020;10(1):193. doi:10.1038/s41398-020-00886-3
82. Deane KHO, Jimoh OF, Biswas P, et al. Omega-3 and polyunsaturated fat for prevention of depression and anxiety symptoms: systematic review and meta-analysis of randomised trials. Br J Psychiatry. 2021;218(3):135–142. doi:10.1192/bjp.2019.234
83. Lin PY, Huang SY, Su KP. A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression. Biol Psychiatry. 2010;68(2):140–147. doi:10.1016/j.biopsych.2010.03.018
84. Lin PY, Chang CH, Chong MF, Chen H, Su KP. Polyunsaturated fatty acids in perinatal depression: a systematic review and meta-analysis. Biol Psychiatry. 2017;82(8):560–569. doi:10.1016/j.biopsych.2017.02.1182
85. Yang Y, Kim Y, Je Y. Fish consumption and risk of depression: epidemiological evidence from prospective studies. Asia Pac Psychiatry. 2018;10(4):e12335. doi:10.1111/appy.12335
86. Tolkien K, Bradburn S, Murgatroyd C. An anti-inflammatory diet as a potential intervention for depressive disorders: a systematic review and meta-analysis. Clin Nutr. 2019;38(5):2045–2052. doi:10.1016/j.clnu.2018.11.007
87. Farooq S, Singh SP, Burke D, Naeem F, Ayub M. Pharmacological interventions for prevention of depression in high risk conditions: systematic review and meta-analysis. J Affect Disord. 2020;269:58–69. doi:10.1016/j.jad.2020.03.024
88. Asher GN, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of complementary and alternative medicine therapies for initial treatment of major depressive disorder: systematic review and meta-analysis. J Altern Complement Med. 2017;23(12):907–919. doi:10.1089/acm.2016.0261
89. Freeman MP, Mischoulon D, Tedeschini E, et al. Complementary and alternative medicine for major depressive disorder: a meta-analysis of patient characteristics, placebo-response rates, and treatment outcomes relative to standard antidepressants. J Clin Psychiatry. 2010;71(6):682–688. doi:10.4088/JCP.10r05976blu
90. Xu Y, Zeng L, Zou K, et al. Role of dietary factors in the prevention and treatment for depression: an umbrella review of meta-analyses of prospective studies. Transl Psychiatry. 2021;11(1):478. doi:10.1038/s41398-021-01590-6
91. Köhler O, Benros M, Nordentoft M, Mors O, Krogh J. Effect of anti-inflammatory treatment on depression and side effects: a systematic review and meta-analysis of randomized clinical trials. Pharmacoepidemiol Drug Saf. 2014;23(Suppl 1):252–253.
92. Köhler O, Benros M, Nordentoft M, Mors P, Krogh J. Effect of anti-inflammatory treatment on depression, depressive symptoms and side effects: a systematic review and meta-analysis of randomized clinical trials. Eur Psychiatry. 2015;30(Suppl 1):0342. doi:10.1016/S0924-9338(15)30268-6
93. Benros M. Immune-related risk factors for schizophrenia and depression in Danish epidemiological studies and meta-analysis of anti-inflammatory treatment for depression. Early Interv Psychiatry. 2016;10(Suppl 1):27.
94. Kim H-B, Kim J-S, Jung J-G. The association between aspirin use and depression: a systematic review and meta-analysis of observational studies. Pharmacoepidemiol Drug Saf. 2020;29(6):613–622. doi:10.1002/pds.5011
95. Suradom C, Suttajit S, Oon-Arom A, Maneeton B, Srisurapanont M. Omega-3 polyunsaturated fatty acid (n-3 PUFA) supplementation for prevention and treatment of perinatal depression: a systematic review and meta-analysis of randomized-controlled trials. Nord J Psychiatry. 2021;75(4):239–246. doi:10.1080/08039488.2020.1843710
96. Reis DJ, Casteen EJ, Ilardi SS. The antidepressant impact of minocycline in rodents: a systematic review and meta-analysis. Sci Rep. 2019;9(1):261. doi:10.1038/s41598-018-36507-9
97. Zheng W, Zhang QE, Cai DB, et al. N-acetylcysteine for major mental disorders: a systematic review and meta-analysis of randomized controlled trials. Acta Psychiatr Scand. 2018;137(5):391–400. doi:10.1111/acps.12862
98. Emadi-Kouchak H, Mohammadinejad P, Asadollahi-Amin A, et al. Therapeutic effects of minocycline on mild-to-moderate depression in HIV patients: a double-blind, placebo-controlled, randomized trial. Int Clin Psychopharmacol. 2016;31(1):20–26. doi:10.1097/YIC.0000000000000098
99. Dean OM, Kanchanatawan B, Ashton M, et al. Adjunctive minocycline treatment for major depressive disorder: a proof of concept trial. Aust N Z J Psychiatry. 2017;51(8):829–840. doi:10.1177/0004867417709357
100. Akhondzadeh S, Jafari S, Raisi F, et al. Clinical trial of ad- junctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. 2009;26(7):607–611. doi:10.1002/da.20589
101. Hashemian F, Majd M, Hosseini SM, Sharifi A, Panahi MVS, Bigdeli O. A randomized, double-blind, placebo-controlled trial of celecoxib augmentation of sertraline in the treatment of a drug-naive women with major depression. Klin Psikofarmakol B. 2011;21:S183–S184.
102. Abbasi SH, Hosseini F, Modabbernia A, Ashrafi M, Akhondzadeh S. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: randomized double-blind placebo-controlled study. J Affect Disord. 2012;141(2–3):308–314. doi:10.1016/j.jad.2012.03.033
103. Majd M, Hashemian F, Hosseini SM, Vahdat Shariatpanahi M, Sharifi A. A randomized, double-blind, placebo-controlled trial of celecoxib augmentation of sertraline in treatment of drug-naive depressed women: a pilot study. Iran J Pharm Res. 2015;14(3):891–899.
104. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry. 2002;159(3):477–479. doi:10.1176/appi.ajp.159.3.477
105. Peet M, Horrobin DF. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry. 2002;59(10):913–919. doi:10.1001/archpsyc.59.10.913
106. Marangell LB, Martinez JM, Zboyan HA, Kertz B, Kim HF, Puryear LJ. A double-blind, placebo-controlled study of the omega-3 fatty acid docosahexaenoic acid in the treatment of major depression. Am J Psychiatry. 2003;160(5):996–998. doi:10.1176/appi.ajp.160.5.996
107. Su KP, Huang SY, Chiu CC, Shen WW. Omega-3 fatty acids in major depressive disorder. A preliminary double-blind, placebo-controlled trial. Eur Neuropsychopharmacol. 2003;13(4):267–271. doi:10.1016/s0924-977x(03)00032-4
108. Silvers KM, Woolley CC, Hamilton FC, Watts PM, Watson RA. Randomised double-blind placebo-controlled trial of fish oil in the treatment of depression. Prostaglandins Leukot Essent Fatty Acids. 2005;72(3):211–218. doi:10.1016/j.plefa.2004.11.004
109. Grenyer BF, Crowe T, Meyer B, et al. Fish oil supplementation in the treatment of major depression: a randomised double-blind placebo-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(7):1393–1396. doi:10.1016/j.pnpbp.2007.06.004
110. Jazayeri S, Tehrani-Doost M, Keshavarz SA, et al. Comparison of therapeutic effects of omega-3 fatty acid eicosapentaenoic acid and fluoxetine, separately and in combination, in major depressive disorder. Aust N Z J Psychiatry. 2008;42(3):192–198. doi:10.1080/00048670701827275
111. Rees AM, Austin MP, Parker GB. Omega-3 fatty acids as a treatment for perinatal depression: randomized double-blind placebo-controlled trial. Aust N Z J Psychiatry. 2008;42(3):199–205. doi:10.1080/00048670701827267
112. da Silva TM, Munhoz RP, Alvarez C, et al. Depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled pilot study of omega-3 fatty-acid supplementation. J Affect Disord. 2008;111(2–3):351–359. doi:10.1016/j.jad.2008.03.008
113. Carney RM, Freedland KE, Rubin EH, Rich MW, Steinmeyer BC, Harris WS. Omega-3 augmentation of sertraline in treatment of depression in patients with coronary heart disease: a randomized controlled trial. JAMA. 2009;302(15):1651–1657. doi:10.1001/jama.2009.1487
114. Lucas M, Asselin G, Merette C, Poulin MJ, Dodin S. Ethyleicosapentaenoic acid for the treatment of psychological distress and depressive symptoms in middle-aged women: a double-blind, placebo-controlled, randomized clinical trial. Am J Clin Nutr. 2009;89:641–651. doi:10.3945/ajcn.2008.26749
115. Mischoulon D, Papakostas GI, Dording CM, et al. A double-blind, randomized controlled trial of ethyl-eicosapentaenoate for major depressive disorder. J Clin Psychiatry. 2009;70(12):1636–1644. doi:10.4088/JCP.08m04603
116. Bot M, Pouwer F, Assies J, et al. Eicosapentaenoic acid as an add-on to antidepressant medication for co-morbid major depression in patients with diabetes mellitus: a randomized, double-blind placebo-controlled study. J Affect Disord. 2010;126(1–2):282–286. doi:10.1016/j.jad.2010.04.008
117. Rondanelli M, Giacosa A, Opizzi A, et al. Effect of omega-3 fatty acids supplementation on depressive symptoms and on health-related quality of life in the treatment of elderly women with depression: a double-blind, placebo-controlled, randomized clinical trial. J Am Coll Nutr. 2010;29(1):55–64. doi:10.1080/07315724.2010.10719817
118. Gonzalez A, Mata S, Sanchez P, et al. Omega-3 fatty acids as adjunctive of antidepressant therapy and its effects on brain-derived neurotrophic factor in serum, monocytes and lymphocytes. Arch Venez Farmacol Ter. 2011;30(4):72–78.
119. Lespérance F, Frasure-Smith N, St-André E, Turecki G, Lespérance P, Wisniewski SR. The efficacy of omega-3 supplementation for major depression: a randomized controlled trial. J Clin Psychiatry. 2011;72(8):1054–1062. doi:10.4088/JCP.10m05966blu
120. Rondanelli M, Giacosa A, Opizzi A, et al. Long chain omega 3 polyunsaturated fatty acids supplementation in the treatment of elderly depression: effects on depressive symptoms, on phospholipids fatty acids profile and on health-related quality of life. J Nutr Health Aging. 2011;15(1):37–44. doi:10.1007/s12603-011-0011-y
121. Gertsik L, Poland RE, Bresee C, Rapaport MH. Omega-3 fatty acid augmentation of citalopram treatment for patients with major depressive disorder. J Clin Psychopharmacol. 2012;32(1):61–64. doi:10.1097/JCP.0b013e31823f3b5f
122. Rizzo AM, Corsetto PA, Montorfano G, et al. Comparison between the AA/EPA ratio in depressed and non depressed elderly females: omega-3 fatty acid supplementation correlates with improved symptoms but does not change immunological parameters. Nutr J. 2012;11:82. doi:10.1186/1475-2891-11-82
123. Mozaffari-Khosravi H, Yassini-Ardakani M, Karamati M, Shariati-Bafghi SE. Eicosapentaenoic acid versus docosahexaenoic acid in mild-to-moderate depression: a randomized, double-blind, placebo-controlled trial. Eur Neuropsychopharmacol. 2013;23(7):636–644. doi:10.1016/j.euroneuro.2012.08.003
124. Gharekhani A, Khatami MR, Dashti-Khavidaki S, et al. The effect of omega-3 fatty acids on depressive symptoms and inflammatory markers in maintenance hemodialysis patients: a randomized, placebo-controlled clinical trial. Eur J Clin Pharmacol. 2014;70(6):655–665. doi:10.1007/s00228-014-1666-1
125. Park Y, Park YS, Kim SH, Oh DH, Park YC. Supplementation of n-3 polyunsaturated fatty acids for major depressive disorder: a randomized, double-blind, 12-week, placebo-controlled trial in Korea. Ann Nutr Metab. 2015;66(2–3):141–148. doi:10.1159/000377640
126. Rapaport MH, Nierenberg AA, Schettler PJ, et al. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Mol Psychiatry. 2016;21(1):71–79. doi:10.1038/mp.2015.22
127. Shinto L, Marracci G, Mohr DC, et al. Omega-3 fatty acids for depression in multiple sclerosis: a randomized pilot study. PLoS One. 2016;11(1):e0147195. doi:10.1371/journal.pone.0147195
128. Jahangard L, Sadeghi A, Ahmadpanah M, et al. Influence of adjuvant omega-3-polyunsaturated fatty acids on depression, sleep, and emotion regulation among outpatients with major depressive disorders - results from a double-blind, randomized and placebo-controlled clinical trial. J Psychiatr Res. 2018;107:48–56. doi:10.1016/j.jpsychires.2018.09.016
129. Carney RM, Freedland KE, Rubin EH, Rich MW, Steinmeyer BC, Harris WS. A randomized placebo-controlled trial of omega-3 and sertraline in depressed patients with or at risk for coronary heart disease. J Clin Psychiatry. 2019;80(4):19m12742. doi:10.4088/JCP.19m12742
130. Yang B, Lin L, Bazinet RP, et al. Clinical efficacy and biological regulations of ω-3 PUFA-derived endocannabinoids in major depressive disorder. Psychother Psychosom. 2019;88(4):215–224. doi:10.1159/000501158
131. Coryell WH. Essential fatty acids for major depression. NLM identifier: NCT00256412; 2014 Available from: https://clinicaltrials.gov/ct2/show/NCT00256412?cond=major+depression&intr=essential+fatty+acids&draw=2&rank=1.
132. Raison C, Rutherford RE, Woolwine B, et al. The tumor necrosis factor-alpha antagonist infliximab reduces depressive symptoms in patients with treatment resistant depression and high inflammation. Brain Behav Immun. 2012;26(suppl 1):S49. doi:10.1016/j.bbi.2012.07.200.W
133. Andrade C. Mean difference, Standardized Mean Difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 2020;81(5):20f13681. doi:10.4088/JCP.20f13681
134. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi:10.3389/fpsyg.2013.00863
135. Alba AC, Alexander PE, Changa J, MacIsaac J, DeFry S, Guyatt GH. High statistical heterogeneity is more frequent in meta-analysis of continuous than binary outcomes. J Clin Epidemiol. 2016;70:129–135. doi:10.1016/j.jclinepi.2015.09.005
136. Russo MW. How to review a meta-analysis. Gastroenterol Hepatol. 2007;3(8):637–642.
137. Andrade C. Anti-inflammatory treatments for depression: perspectives on how to read a meta-analysis critically. J Clin Psychiatry. 2019;80(3):19f12907. doi:10.4088/JCP.19f12907
138. Silverman MN, Sternberg E. Glucocorticoid regulation of inflammation and its functional correlates: from HPA axis to glucocorticoid receptor dysfunction. Ann N Y Acad Sci. 2012;1261:55–63. doi:10.1111/j.1749-6632.2012.06633.x
139. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–1366. doi:10.1016/S0140-6736(17)32802-7
140. Furukawa TA, Cipriani A, Cowen PJ, Leucht S, Egger M, Salanti G. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601–609. doi:10.1016/S2215-0366(19)30217-2
141. Guo X, McCutcheon RA, Pillinger T, et al. The magnitude and heterogeneity of antidepressant response in depression: a meta-analysis of over 45,000 patients. J Affect Disord. 2020;276:991–1000. doi:10.1016/j.jad.2020.07.102
142. Drevets WC, Wittenberg GM, Bullmore ET, Manji HK. Immune targets for therapeutic development in depression: towards precision medicine. Nat Rev Drug Discov. 2022;21:224–244. doi:10.1038/s41573-021-00368-1
143. Sorgdrager FJH, Naudé PJW, Kema IP, Nollen EA, De Deyn PP. Tryptophan metabolism in inflammaging: from biomarker to therapeutic target. Front Immunol. 2019;10:2565. doi:10.3389/fimmu.2019.02565
144. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200. doi:10.1186/1741-7015-11-200
145. Medina-Rodriguez EM, Lowell JA, Worthen RJ, Syed SA, Beurel E. Involvement of innate and adaptive immune systems alterations in the pathophysiology and treatment of depression. Front Neurosci. 2018;12:547. doi:10.3389/fnins.2018.00547
146. Visentin A, Colombo R, Scotton E, et al. Targeting inflammatory-mitochondrial response in major depression: current evidence and further challenges. Oxid Med Cell Longev. 2020;2020:2972968. doi:10.1155/2020/2972968
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.