Back to Journals » Nutrition and Dietary Supplements » Volume 12
Anti-Cancer and Other Biological Effects of a Dietary Compound 3,3ʹ-Diindolylmethane Supplementation: A Systematic Review of Human Clinical Trials
Authors Amare DE
Received 7 May 2020
Accepted for publication 7 July 2020
Published 4 August 2020 Volume 2020:12 Pages 123—137
DOI https://doi.org/10.2147/NDS.S261577
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chandrika J Piyathilake
Dagnachew Eyachew Amare
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Dagnachew Eyachew Amare
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P.O. Box 196, Gondar, Ethiopia
Tel +251-939406194
Email [email protected]
Objective: To systematically review the human clinical trial published studies regarding a dietary compound 3,3ʹ-diindolylmethane (DIM) clinical efficacy towards the prevention and treatment of cancer and other diseases, its bioavailability, safety, and consistency of the results.
Methods: An electronic literature search of PubMed database (14), Cochrane Clinical Trials library (3), and Google Scholar (5) from inception to Feb 2020 was conducted. All the in vitro, animal, epidemiological, and review studies of DIM were excluded. Twenty-two randomized or controlled human clinical trials with prospective/retrospective studies published in the English language and that involved DIM intervention on human participants were extracted.
Results: DIM has increased estrogen metabolism, decreased androgen-specific antigen, up-regulated BRCA1 expression, and increased androgen hormone-binding globulin. This suggests that DIM may have a promising beneficial role as a chemo-preventive supplement for breast and prostate cancers. DIM has shown some clinical efficacy to treat cervical/prostate dysplasia, human papilloma-virus, and warts.
Conclusion: The absence of clinical evidence about DIM efficacy to treat prostate or breast cancer patients is the concern as this dietary compound is being advocated as a supplement in the market to treat these disease conditions. The maximum DIM intervention time for breast and prostate cancer patients was 28 days and 12 months, respectively, and most of the prospective trials were targeting DIM biological fate, than adequately addressing DIM efficacy in treating breast or prostate cancer.
Keywords: 3,3ʹ-diindolylmethane, cancer, cruciferous vegetables, human clinical trials, indole-3-carbinol, supplementation
Introduction
Cruciferous vegetables such as Brussels sprouts, broccoli, kale, cabbage, and cauliflower are rich sources of dietary bioactive compounds, namely, indole-3-carbinol (I3C) and its major metabolite 3,3ʹ-diindolylmethane (DIM). Chewing or chopping cruciferous vegetables results in the hydrolysis of the glucosinolate glucobrassicin into indole-3-carbinol catalyzed by the enzyme myrosinase.1 Glucosinolate and myrosinase are stored intact in separate plant cell compartments and come together only after cell rupture. Under acid-catalyzed reaction conditions in the stomach, indole-3-carbinol degrades to several bioactive condensation products among the most known are 3,3ʹ-diindolylmethane (DIM) and indolo(3,2-b)carbazole (ICZ).2–6 Other oligomers, namely, the cyclic trimer 5,6,11,12,17,18-hexahydrocyclonona(1,2-b:4,5-b’:7,8-b”)tri-indole (CTr), a cyclic tetramer CTet, the first linear trimer (LTr1), and the second linear trimer (LTr2).2–4
Dietary consumption of cruciferous vegetables is associated with a variety of beneficial biological activities. It appears most of the I3C biological activities are result from its bioactive products, as I3C is virtually converted in the gut acidic environment.2,3,7 Most of the biomedical research on indole-3-carbinol and 3,3ʹ-diindolylmethane were conducted using animals and human cultured cells. More than a thousand studies related to indole-3-carbinol and its major derivatives exposure on human cultured cells and animals have reported significant health benefits, such as chemo-prevention and therapeutic effects.
Indole-3-carbinol mainly its derivative 3,3ʹ-diindolylmethane has received considerable attention for having properties of anti-breast cancer,8–10 anti-prostate cancer,10–13 detoxification of toxicants,14,15 induction of apoptosis,16–18 prevent bone weakness19–21 and anti-human papillomavirus.22,23 Indole-3-carbinol and its major derivatives are the topics of ongoing research since 1975 when it was first reported that I3C increases the metabolism of carcinogenic chemicals.24,25 Later on, several studies have shown that most of the biological activities of indole-3-carbinol are attributed to its condensation products. Among these, 3,3ʹ-diindolylmethane has been recognized as the major in vivo derivative responsible for most of the biological properties of indole-3-carbinol.26–29
Epidemiological studies have shown that consumption of cruciferous vegetables significantly lowers the incidence of human cancer. An inverse association was found between high intake of cruciferous vegetables, particularly broccoli, and an incidence of breast cancer.30 Higdon et al have reported that a high intake of cruciferous vegetables reduced the risk of human cancers in an epidemiological study.31 Studies using animal and human cultured cells have shown that 3,3ʹ-diindolylmethane inhibited the growth of a variety of cancer cells including prostate cancer,32–37 breast cancer,17,37-39 pancreatic cancer,40,41 colorectal cancer,42–46 lung tumors,47,48 and nasopharyngeal cancer.49,50 Other suggested roles of DIM include boosting immune function,42,51,52 increase estrogen metabolism,53 having anti-leishmaniasis54–56 and anti-human papillomavirus properties57–59 in animal and in vitro studies.
Although most of the published studies on DIM and its parent compound (I3C) were mainly in animal or in vitro models, there is an increasing media publicity advocating individuals to try I3C or DIM supplementation including formulation in drug form60 for their potential applications in the prevention and treatment of diseases such as breast and prostate cancers. Recently, researchers and companies become more interested in the formulation of DIM as a supplement.61 This is because DIM has a greater stability compared to I3C after oral ingestion, where the latter virtually converted in the stomach acidic environment. Unlike DIM, there are warnings regarding the wide-spread use of I3C supplementation for cancer prevention and other roles until sufficient clinical data established regarding their potential risks and benefits.62–67 The wide range of research outputs, marketing as a supplement, and other media publicity on I3C and DIM health benefits have evoked to review the existing human clinical-based literature in connection to DIM interventions. Therefore, the principal goal of this review was to review the human clinical trial published studies on DIM clinical efficacy towards prevention and treatment of diseases including the mechanism, and consistency of clinical trial scientific results. It also explores the nature of clinical-based studies in DIM intervention, adverse conditions/tolerability, and its bioavailability after direct oral supplementation. There is no comprehensive published review paper on human clinical trials from DIM supplementation.
Methods
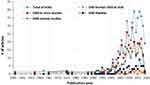
A comprehensive literature searches were conducted from three databases, namely, the PubMed, Cochrane library, and Google Scholar from inception to Feb 2020. The key search item was DIM. All of the studies with DIM supplementation in human clinical trials were selected for this systematic review by excluding all in vitro, animal, epidemiological, and review studies. Twenty-two studies with English language that reported original data on effect of supplementation of DIM or DIM-precursors were extracted. The outcomes of DIM-precursors supplementation were solely DIM-related. All the human clinical trials published studies on supplementation of DIM were from the PubMed database (14 articles), Cochrane library (3 articles), and Google Scholar (5 articles). Allrticles indexed in PubMed regarding DIM including their study nature and annual count are depicted in Figure 1. Among the 14 human clinical trials indexed in PubMed, three of the DIM clinical studies were directly from cruciferous vegetable consumption (2) or indole-3-carbinol ingestion (1).
Data Extraction and Synthesis
The extracted DIM supplementation information were about the study design, population demographics, form of DIM supplementation, dose and duration of DIM exposure, anti-cancer properties, other health effects, bioavailability of DIM, and safety/toxicity of DIM. Appraisal of methodological qualities of the studies was mainly weighted based on intervention time, sample size, and exposure dose.
Results and Discussion
Bioavailability of 3,3ʹ-Diindolylmethane in Human Clinical Trials
The pharmacokinetics of indole-3-carbinol and 3,3ʹ-diindolylmethane were studied in rodents. Oral administration of DIM to mice at the dose of 250 mg/kg has led to a rapid rise of plasma and tissues (brain, heart, liver, kidneys, and lungs) level between 0.5 to 1 h.68 In another study, indole-3-carbinol administered to mice, it was rapidly absorbed, distributed, and eliminated in the blood and body tissues, falling below the detection limit after 1 h2 whilst DIM was substantially detected in the blood and tissue samples which persists after 24 h.2
Oral administration of indole-3-carbinol to human subjects has shown that DIM is the major product detected in plasma samples relatively with a longer half-life.2,69 This showed that following ingestion of indole-3-carbinol, the formation of the major derivative product DIM and the several reported biological activities has led to the study of DIM as a possible chemopreventive and therapeutic supplement. Besides the several suggested biological benefits of DIM, it has an important role as a biomarker for indole-3-carbinol or cruciferous vegetable consumption.
Many studies have disclosed that indole-3-carbinol has very low bioavailability after oral ingestion because of its transformation to various condensation products in the gastric acidic environment. As a result of that, several clinical trial studies in recent times have been conducted using direct DIM intervention where its bioavailability not affected by the stomach acidic environment.68,70 Yet, the crystalline DIM is not well absorbed in the gastrointestinal system, and in response to that scientists have developed a formulated DIM known as an absorption enhanced “Bioresponse-DIM” (BR-DIM) which is highly absorbable23,71 compared to the generic form. Anderton et al have reported that an absorption-enhanced formulation (BioResponse-DIM) displayed approximately 50% greater bioavailability than the crystalline form after oral administration to mice.68 For that reason, the absorption-enhanced BioResponse (BR)-DIM is the most widely used form of DIM for supplementation in the human clinical trials. From the total 22 human clinical trial studies conducted in relation to DIM, 12 studies were using Bioresponse-DIM, 5 using crystalline DIM, two using Infemin (formulated DIM), two using raw cruciferous vegetables, and one using indole-3-carbinol as shown in Table 1.
 |  |  |  |
Table 1 Summary of Peer-Review Published Clinical Trials (Indexed in PubMed, Cochrane-Embase and Google Scholar Databases) Regarding DIM Supplementation |
Herein, the focus was on the primary end-points of DIM (plasma, urine, and/or tissues) resulting from BR-DIM supplementation to human subjects. It has been reported that DIM was the only product detected in plasma samples after non-smoking women subjects (n=24; age between 23 and 58 years) with an elevated risk of breast cancer (by family history) ingested at oral doses of 400, 600, 800, 1000, and 1200 mg indole-3-carbinol.72 As Reed et al reported, the maximum plasma concentration (Cmax) of DIM in the women was detected at 1000 mg I3C oral dose.72 In another study with a principal objective to quantify DIM in urine samples of women with cervical dysplasia after ingesting I3C resulted in a mean value of DIM, 12.1 ± 2.573 and 15.6 ± 22.273 μg/mg creatinine for the 200 and 400 mg DIM exposed groups, respectively.69
Two randomized human clinical trials were also performed with the primary purpose of quantifying DIM in urine after twenty-five (healthy, non-vegetarian, and non-smoking) adults’ consumed raw cruciferous vegetables (Brussels sprouts and cabbage).74,75 Fujioka et al74 revealed that urinary DIM was successfully quantified with higher quantity in Brussels sprout than cabbage after 25 subjects (10 males and 15 females who were healthy, non-vegetarian, non-smoking; ages 22 to 63 years) ingesting 50 g of these raw vegetables per day for 3 days. Fujioka et al75 demonstrated that urinary DIM increased with increasing glucobrassicin dose after the 45 subjects (19 males and 26 females, age 18 to 60 years) consumed cruciferous vegetables (with exposure doses of glucobrassicin at 25, 50, 100, 200, 300, 400 or 500 μmol). These authors claimed that the majority of DIM was eliminated in urine in the first 12 h of the intervention. In prostate cancer patients (n=45; mean age of 61.1 years), the mean value of DIM level in plasma samples was reported as 4.95±17.6, 151.42±197.1, and 280.4±217.2 ng/mL for placebo, 200 mg, and 400 mg/day BR-DIM doses, respectively, after 2 weeks of intervention period.76 Rajoria et al reported that the mean value of DIM in urine, serum, and thyroid tissues was 383.5 ng/mg of creatinine, 12.32 ng/mg of creatinine, and 40.67 ng/mg tissue, respectively, after seven women patients (between ages of 39–56 years) with thyroid proliferative disease ingested 300 mg of BR-DIM per day for 2 weeks.77 Reed et al depicted a dose-dependent DIM concentration in plasma samples of 24 healthy subjects (13 Men and 11 Women; ages 22 to 58 years) who consumed a single dose of BR-DIM at the doses of 50, 100, 150, 200 or 300 mg. These authors reported that DIM Cmax in plasma was reached at 200 mg dosage. Similarly, Heath et al have reported that BR-DIM (at the doses of 75, 150, 225, and 300 mg twice daily) supplementation to 12 prostate cancer patients resulted in rapid absorption of DIM between 2 and 4 h, and dose-proportional plasma levels.78 Another study has shown that the mean value of DIM in prostate tissue and plasma was 14.2 ng/gm tissue and 9.0 g/mL, respectively, in 36 prostate cancer patients who ingested 225 mg of BR-DIM twice daily for 2 weeks.79
DIM Supplementation and Cancer: Human Clinical Trials
The completed human clinical studies mainly focused on breast or prostate cancer patients. Besides the suggested benefits of DIM in breast and prostate cancer prevention and treatment, similar studies in animal and human cultured cells have shown the role of DIM to inhibit growth of a variety of cancer cells, namely, pancreatic cancer,40,41 colorectal cancer,42–46 lung tumors,47,48 and nasopharyngeal cancer.49,50 However, there was no single human clinical trial study conducted to establish an association between DIM supplementation, and pancreatic, colorectal, lung, or nasopharyngeal cancer. Hence, the discussion under this section emphasized on clinical trial studies that involved DIM supplementation and endpoints mainly in either healthy subjects, breast, or prostate cancer patients.
Breast Cancer
Many studies in animals and in-vitro including epidemiological have shown that 3,3ʹ-diindolylmethane modulate the endogenous estrogen hormone playing a role in the prevention and inhibition of growth of estrogen-dependent breast cancer including endometrial and cervical cancers.80–82 The human estrogen receptor becomes a crucial target of chemo-preventive and therapeutic strategies to control the estrogen-dependent proliferation of breast cancers. Thus, 3,3ʹ-diindolylmethane agonist to the human estrogen receptor has been related to having beneficial effects to treat menopausal complaints, steroids and lipid metabolism, prevent bone loss, and improve sexual problems in females.19,83-86 DIM has induced the cyochromp450 enzymes specifically, by up-regulating the CYP1A1, CYP1A2, and CYP1B1 enzymes87,88 to catalyze the human estrogen metabolism.
It has been shown that DIM promotes the metabolism of the estrogen hormone by increasing the beneficial estrogen metabolite, namely 2-hydroxyestrone over the unfavorable 16-alpha-hydroxyestrone.28,89 The endogenous estrogen (17β-estradiol), the primary female sex hormone, metabolized to 16α-OHE1 or 2-OHE1. Unlike 2-OHE1, the 16α-OHE1 metabolite has strong estrogenic properties, and highly associated to promote the proliferation of estrogenic dependent breast cancer.90,91 Previous researches suggested that changing the course of the 17β-estradiol metabolism towards 2-OHE1, and suppressing the 16α-OHE1 may have a role to reduce the incidence of estrogen-based cancers including breast cancer89,92,93 although other studies found no association.94,95 Several studies in animals and cultured cells including epidemiological have depicted that the dietary compound DIM modulates the endogenous estrogens consequently playing a role in the suppression of growth of estrogen-dependent cancers.80–82
In light of that supplementation of DIM in human clinical trial studies and its efficacy towards prevention or treatment of estrogen-dependent cancers has been discussed in this section.
Supplementation of BR-DIM to humans has significantly increased the ratio of 2-OHE1 to 16α-OHE128,76,96,97 whilst Nikitina et al98 reported no change in the ratio of the two estrogen metabolites (see the summary in Table 1). Dalessandri et al have found that BR-DIM supplementation (108 mg/day for 30 days) increased the ratio of 2-OHE1 to 16α-OHE1 (from 1.46 to 2.14) in a double-blind randomized controlled trial (10 in the treatment group and 9 in the placebo) in women (aged 50–70 years) with a history of early stage breast cancer.28 Similarly, Gee et al have reported a significant increase in urinary 2-OHE1 to 16α-OHE1 ratio in the BR-DIM (at 100 or 200 mg or placebo twice daily for 21–28 days) exposed group in a double-blind randomized controlled trial in 45 patients with prostate cancer.76 Through another molecular path-way, BR-DIM (300 mg per day for 4–6 weeks) supplementation to 13 women (with a tumor suppression BRCA1 gene carriers) has resulted in the up-regulation of BRCA1 (breast cancer type 1) gene expression in the 10 subjects.99 The increase in BRCA1 gene expression is associated with breast cancer prevention or suppression of tumor proliferation.100–103
Overall, DIM supplementation in the aforementioned clinical trials showed its effect in increasing endogenous estrogen hormone metabolism, and the ability to induce BRCA1 gene expression, where both biological activities have been linked to having beneficial effects in the prevention of estrogens-dependent cancers. Although epidemiological studies supported cruciferous vegetables consumption and a role in lowering risks of breast cancer among women,30,31 there lacks single clinical trial study that directly indicated DIM supplementation and its efficacy towards treatment of breast cancer or other estrogen-dependent cancer in the studied subjects. Given the insufficient intervention time (the maximum was 12 months), the author recommends larger cohort studies in future clinical trials to see DIM efficacy in preventing the incidence of estrogen-dependent cancers in healthy subjects or its therapeutic effect for women with breast patients.
Prostate Cancer
Several studies have revealed that 3,3ʹ-diindolylmethane has a potent anti-androgenic property mediated by the human androgen receptor that renders important benefits in preventing and reducing the proliferation of androgen-based prostate cancer cells.29,37,82,104 The antagonist properties of 3,3ʹ-diindolylmethane to androgen hormone at the receptor level have useful chemopreventive properties for prostate cancer.29,105 There are studies that supported the role of 3,3ʹ-diindolylmethane in prostate tumor growth suppression via non-receptor pathways.11,18,32,34,106
Some epidemiological studies have supported that consumption of cruciferous vegetables associated with lower risks of prostate cancer.107–110 On the other hand, there are studies that found statistically non-significant between consumption of cruciferous vegetables and risk of prostate cancer inverse association.111–114
The remaining discussion in this section focused on human clinical trial studies that have linked DIM supplementation and its effect on a number of molecular targets, believed to be beneficial for therapeutic or chemoprevention purposes related to prostate cancer. Kong et al have reported that BR-DIM (300 mg per day for 4–6 weeks) supplementation to prostate cancer patients (age between 47 and 64) resulted in the up-regulation of let-7, which is a family of microRNAs.115 Down-regulation of the let-7 family has been associated with promoting the recurrence and elevation of prostate cancer by regulating cancer stem cells.116 Previous research conducted on BR-DIM (four cohorts exposed to doses either 75, 150, 225, or 300 mg twice daily for 4 months) supplementation has resulted a decrease in prostate-specific antigen among the 10 subjects (n=13) even though the conditions eventually progressed.78 Men with elevated level of prostate-specific antigen are at the greatest risk to develop prostate cancer117–119 and hence the reduction of this antigen by DIM may have a role in combating tumor formation in prostate tissues.79 A study has shown that prostate cancer patients (n=36) who ingested DIM (at 225 mg twice daily for 2 weeks) resulted in the exclusion of the androgen receptor from the cell nucleus in the 27 (96%) of patients, and prostate-specific antigen decline in the 20 (71%) of patients.78 These human clinical trial studies have shown that DIM is a promising bioactive compound to modulate molecular targets, responsible for the initiation and progression of prostate cancer. Even though several animals and laboratory studies18,32-34,37,120,121 and some epidemiological studies107–110 depicted DIM ability to exert apoptosis and arrest proliferation in prostate cancer cells, no single clinical trial study has shown DIM efficacy towards prevention and treatment of prostate cancer. Therefore, larger prospective cohort clinical trials are recommended in future interventions to establish an inverse relation between DIM supplementation and the formation or proliferation of prostate cancer.
Anti-Viral and Anti-Dysplasia Effects: Human Clinical Trials
The human papillomavirus is an important risk determinant for the development of cervical/vaginal intraepithelial neoplasia and cervical cancer.122–126
In a double-blind randomized control trial, BR-DIM (45 DIM vs 19 placebo, 2 mg/kg body-weight for 3 months) supplementation to 64 women (mean age 28 years, range 18–61) with cervical intraepithelial neoplasia showed that 21 subjects (47%) in the treatment group improved their condition with a decrease by 1–2 grades.127 DIM (at the dose of 100, 200 mg/day or placebo for 90–180 days) intervention in 78 women (age between 19 and 39 years) with cervical intraepithelial neoplasia grade I–II resulted in regression of their conditions as reported 100%, 98.83%, and 61.1% of subjects for the high dose, low dose, and placebo, respectively.60
Paltsev et al investigated the Infemin (a formulated DIM at a dose of 900 mg daily or placebo for 3 months) supplementation effect in 14 patients (ages 18 to 60 years) with prostatic intraepithelial neoplasia and found out that clinically non-significant improvement in their conditions.128 Paltsev et al, however, continued a second-round double-blind randomized placebo-controlled multicenter clinical trial among 21 patients (11 received Infemin 900 mg vs 10 placeboes per day for 12 months) diagnosed with a high-grade prostatic intraepithelial neoplasia which resulted in a complete reversion of the 45.5% subjects condition.129 This marked difference in the clinical effect compared to the first round trial is apparently related to the extended intervention duration.
On the other hand, previous research on BR-DIM supplementation (150 mg or placebo for 6 months) to 551 women (age range 19–65 years) with human papilloma-virus and low-grade cervical cytological abnormalities showed no effect on cervical cytology or on HPV infection.130 Similarly, DIM (150 mg or placebo for 6 months) supplementation to 84 women diagnosed with low-grade cervical neoplasia and infected with HPV has resulted in statistically non-significant (only 11 subjects negative) clinical efficacy.
Although these clinical trial results are promising about the clinical efficacy of DIM to treat cervical or prostatic intraepithelial neoplasia, longer prospective cohort clinical studies may strongly support whether this dietary compound is clinically efficient to treat various cases of dysplasia.
Adverse Effects
Systemic toxicity was not observed in all of the human clinical trial studies after ingestion of DIM. Adverse health effects were not reported when 18 healthy men and women were supplemented with BR-DIM between 50 and 200 mg dose.131 When the dose was increased to 300 mg, however, one subject reported headache and nausea, and another subject reported vomiting. Reed et al have increased the BR-DIM dosage (1200 mg per day for 2 months) to healthy women (n=20) and subsequently, 5 women reported short-term gastrointestinal distress which seemed to be dose-dependent.72
Another study has reported that 49 women with cervical dysplasia were exposed to BR-DIM at the dose of 2 mg/kg/day for 3 months, and the dose was well tolerated with no systemic toxicity.127 DIM oral ingestion by all subjects was well tolerated, if any, short-term gastrointestinal distress, nausea, and vomiting were adverse effects reported but in most cases were statistically non-significant.
Limitations to the Human Clinical Trials
Most of the clinical trials focused on the determination of endpoints of DIM supplementation in human subjects. With prostate or breast cancer patients, most of the trials were merely to see DIM effect on estrogen hormone metabolism, prostate-specific antigen, or DIM plasma/urine/tissue level (Table 1). In other words, there was no single human clinical study primarily conducted to show therapeutic effect of DIM in prostate or breast cancer patients. Similarly, no single study among the pooled human clinical researches did show DIM’s (as chemopreventive) ability to impede development of cancer in healthy subjects. The major weakness of these clinical trials, in particular with prostate or breast patients was the intervention period. For prostate cancer patients the maximum DIM intervention time was 28 days78 while the minimum reported time was 2 weeks.28 The minimum and maximum DIM intervention period for the breast cancer patients were 4 weeks and 12 months, respectively,97,98 though the latter intervention was in combination with tamoxifen. For the combined intervention, the authors reported that no change in breast cell density observed in all subjects but did not disclose if treatment occurred. Therefore, the intervention time for future clinical trials should be sufficiently long for prostate and breast cancer patients or chemoprevention in healthy subjects. Paltsev et al have found initially clinically non-significant improvement in the prostatic intraepithelial neoplasia patients in the 3 months of DIM intervention,128 however, Paltsev et al increased the exposure period to 1 year with the same DIM dosage and it turned out that the 45.5% subjects showed a complete reversion in their condition.129
Conclusion and Recommendations
Several animal and human cultured cells on DIM supplementation and its effect on estrogen metabolism were consistent with the human clinical trials. DIM intervention in the human clinical trials has shown its efficacy in regulating some molecular targets responsible to induce tumor formation. This suggests that DIM can be a promising chemopreventive supplement. Among the pooled clinical trials, no single study established a research to directly see DIM’s efficacy in treating breast or prostate cancer. The absence of clinical evidence about DIM efficacy to treat prostate or breast cancer is found to be the major concern as this dietary compound is being sold on the market as a supplement for treatment in these disease conditions.
Several clinical trial studies have shown that an absorption-enhanced formulation of DIM (BioResponse-DIM) displayed 50% greater bioavailability than the crystalline form after oral ingestion.
The maximum DIM intervention time for breast and prostate cancer patients was 28 days and 12 months, respectively. Therefore, it is recommended that future larger prospective clinical trial research with substantial intervention time is required to see DIM’s ability to treat breast, prostate, and other cancer cases. Moreover, much of the completed clinical researches have focused on the lonely effect of DIM as a therapeutic or chemopreventive agent.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Johnson IT. Glucosinolates: bioavailability and importance to health. Int J Vitam Nutr Res. 2002;72(1):26–31. doi:10.1024/0300-9831.72.1.26
2. Anderton MJ, Manson MM, Verschoyle RD, et al. Pharmacokinetics and tissue disposition of indole-3-carbinol and its acid condensation products after oral administration to mice. Clin Cancer Res. 2004;10(15):5233–5241. doi:10.1158/1078-0432.CCR-04-0163
3. Bjeldanes LF, Kim JY, Grose KR, et al. Aromatic hydrocarbon responsiveness-receptor agonists generated from indole-3-carbinol in vitro and in vivo: comparisons with 2, 3, 7, 8-tetrachlorodibenzo-p-dioxin. Proc Natl Acad Sci U S A. 1991;88(21):9543–9547. doi:10.1073/pnas.88.21.9543
4. Chang Y-C, Riby J, Chang GH-F, et al. Cytostatic and antiestrogenic effects of 2-(indol-3-ylmethyl)-3, 3′-diindolylmethane, a major in vivo product of dietary indole-3-carbinol. Biochem Pharmacol. 1999;58(5):825–834. doi:10.1016/S0006-2952(99)00165-3
5. Chen I, McDougal A, Wang F, et al. Aryl hydrocarbon receptor-mediated antiestrogenic and antitumorigenic activity of diindolylmethane. Carcinogenesis. 1998;19(9):1631–1639. doi:10.1093/carcin/19.9.1631
6. Bradfield CA, Bjeldanes LF. High-performance liquid chromatographic analysis of anticarcinogenic indoles in Brassica oleracea. J Agric Food Chem. 1987;35(1):46–49. doi:10.1021/jf00073a010
7. Weng J-R, Tsai C-H, Kulp SK, et al. Indole-3-carbinol as a chemopreventive and anti-cancer agent. Cancer Lett. 2008;262(2):153–163. doi:10.1016/j.canlet.2008.01.033
8. Ashok B, Chen YG, Liu X, et al. Multiple molecular targets of indole-3-carbinol, a chemopreventive anti-estrogen in breast cancer. Eur J Cancer Prev. 2002;11:S86–S93.
9. Auborn KJ, Fan S, Rosen EM, et al. Indole-3-carbinol is a negative regulator of estrogen. J Nutr. 2003;133(7):2470S–2475S. doi:10.1093/jn/133.7.2470S
10. Bradlow HL. Indole-3-carbinol as a chemoprotective agent in breast and prostate cancer. In Vivo. 2008;22(4):441–445.
11. Garikapaty VP, Ashok BT, Tadi K, et al. 3,3ʹ-Diindolylmethane downregulates pro-survival pathway in hormone independent prostate cancer. Biochem Biophys Res Commun. 2006;340(2):718–725. doi:10.1016/j.bbrc.2005.12.059
12. Li Y, Li X, Sarkar FH. Gene expression profiles of I3C- and DIM-treated PC3 human prostate cancer cells determined by cDNA microarray analysis. Case Rep Med. 2003;133(4):1011–1019.
13. Sarkar FH, Li Y. Indole-3-carbinol and prostate cancer. J Nutr. 2004;134(12 Suppl):3493s–3498s. doi:10.1093/jn/134.12.3493S
14. Wortelboer HM, De Kruif CA, Van Iersel AAJ, et al. Acid reaction products of indole-3-carbinol and their effects on cytochrome P450 and Phase II enzymes in rat and monkey hepatocytes. Biochem Pharmacol. 1992;43(7):1439–1447. doi:10.1016/0006-2952(92)90200-3
15. Nho CW, Jeffery E. The synergistic upregulation of phase II detoxification enzymes by glucosinolate breakdown products in cruciferous vegetables. Toxicol Appl Pharmacol. 2001;174(2):146–152. doi:10.1006/taap.2001.9207
16. Abdelrahim M, Newman K, Vanderlaag K, et al. 3, 3′-diindolylmethane (DIM) and its derivatives induce apoptosis in pancreatic cancer cells through endoplasmic reticulum stress-dependent upregulation of DR5. Carcinogenesis. 2005;27(4):717–728. doi:10.1093/carcin/bgi270
17. Ge X, Yannai S, Rennert G, et al. 3, 3′-Diindolylmethane induces apoptosis in human cancer cells. Biochem Biophys Res Commun. 1996;228(1):153–158. doi:10.1006/bbrc.1996.1631
18. Nachshon-Kedmi M, Yannai S, Haj A, et al. Indole-3-carbinol and 3, 3′-diindolylmethane induce apoptosis in human prostate cancer cells. Food Chem Toxicol. 2003;41(6):745–752. doi:10.1016/S0278-6915(03)00004-8
19. Rodan GA, Martin TJ. Therapeutic approaches to bone diseases. Science. 2000;289(5484):1508–1514. doi:10.1126/science.289.5484.1508
20. Yu T-Y, Pang W-J, Yang G-S. 3, 3′-Diindolylmethane increases bone mass by suppressing osteoclastic bone resorption in mice. J Pharmacol Sci. 2015;127(1):75–82. doi:10.1016/j.jphs.2014.11.006
21. Dong L, Xia S, Gao F, et al. 3, 3′-Diindolylmethane attenuates experimental arthritis and osteoclastogenesis. Biochem Pharmacol. 2010;79(5):715–721. doi:10.1016/j.bcp.2009.10.010
22. Katsuta T, Miyaji Y, Offit PA, et al. Treatment with quadrivalent human papillomavirus vaccine for juvenile-onset recurrent respiratory papillomatosis: case report and review of the literature. J Pediatric Infect Dis Soc. 2017;6(4):380–385. doi:10.1093/jpids/pix063
23. Zeligs MA. Diindolylmethane for the treatment of HPV infection. Google Patents. 2012
24. Wattenberg LW, Weng J-R, Tsai C-H, Kulp SK, Chen C-S. Effects of dietary constituents on the metabolism of chemical carcinogens. Cancer Res. 1975;35(11 Part 2):3326–3331.
25. Loub WD, Wattenberg LW, Davis DW. Aryl hydrocarbon hydroxylase induction in rat tissues by naturally occurring indoles of cruciferous plants. J Natl Cancer Inst. 1975;54(4):985–988.
26. Aggarwal BB, Ichikawa H. Molecular targets and anticancer potential of indole-3-carbinol and its derivatives. Cell Cycle. 2005;4(9):1201–1215. doi:10.4161/cc.4.9.1993
27. Stresser DM, Bailey GS, Williams DE, et al. The anticarcinogen 3,3ʹ-diindolylmethane is an inhibitor of cytochrome P-450. J Biochem Toxicol. 1995;10(4):191–201. doi:10.1002/jbt.2570100403
28. Dalessandri KM, Firestone GL, Fitch MD, et al. Pilot study: effect of 3,3ʹ-diindolylmethane supplements on urinary hormone metabolites in postmenopausal women with a history of early-stage breast cancer. Nutr Cancer. 2004;50(2):161–167. doi:10.1207/s15327914nc5002_5
29. Le HT, Schaldach CM, Firestone GL, et al. Plant-derived 3,3ʹ-Diindolylmethane is a strong androgen antagonist in human prostate cancer cells. J Biol Chem. 2003;278(23):21136–21145. doi:10.1074/jbc.M300588200
30. Ambrosone CB, McCann SE, Freudenheim JL, et al. Breast cancer risk in premenopausal women is inversely associated with consumption of broccoli, a source of isothiocyanates, but is not modified by GST genotype. J Nutr. 2004;134(5):1134–1138. doi:10.1093/jn/134.5.1134
31. Higdon JV, Delage B, Williams DE, et al. Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. Pharmacol Res. 2007;55(3):224–236. doi:10.1016/j.phrs.2007.01.009
32. Nachshon‐Kedmi M, Fares FA, Yannai S. Therapeutic activity of 3, 3′‐diindolylmethane on prostate cancer in an in vivo model. Prostate. 2004;61(2):153–160. doi:10.1002/pros.20092
33. Rahman KM, Banerjee S, Ali S, et al. 3,3ʹ-Diindolylmethane enhances taxotere-induced apoptosis in hormone-refractory prostate cancer cells through survivin down-regulation. Cancer Res. 2009;69(10):4468–4475. doi:10.1158/0008-5472.CAN-08-4423
34. Cho HJ, Park SY, Kim EJ, et al. 3, 3′‐diindolylmethane inhibits prostate cancer development in the transgenic adenocarcinoma mouse prostate model. Mol Carcinog. 2011;50(2):100–112. doi:10.1002/mc.20698
35. Wu T-Y, Jain MG, Hislop GT, et al. Epigenetic modifications of Nrf2 by 3, 3′-diindolylmethane in vitro in TRAMP C1 cell line and in vivo TRAMP prostate tumors. AAPS J. 2013;15(3):864–874. doi:10.1208/s12248-013-9493-3
36. Fares F, Azzam N, Appel B, et al. The potential efficacy of 3, 3′-diindolylmethane in prevention of prostate cancer development. Eur J Cancer Prev. 2010;19(3):199–203. doi:10.1097/CEJ.0b013e328333fbce
37. Bhuiyan MM, Li Y, Banerjee S, et al. Down-regulation of androgen receptor by 3, 3′-diindolylmethane contributes to inhibition of cell proliferation and induction of apoptosis in both hormone-sensitive LNCaP and insensitive C4-2B prostate cancer cells. Cancer Res. 2006;66(20):10064–10072. doi:10.1158/0008-5472.CAN-06-2011
38. Rahman KM, Ali S, Aboukameel A, et al. Inactivation of NF-kappaB by 3,3ʹ-diindolylmethane contributes to increased apoptosis induced by chemotherapeutic agent in breast cancer cells. Mol Cancer Ther. 2007;6(10):2757–2765. doi:10.1158/1535-7163.MCT-07-0336
39. Ahmad A, Ali S, Wang Z, et al. 3, 3′‐diindolylmethane enhances taxotere‐induced growth inhibition of breast cancer cells through downregulation of FoxM1. Int J Cancer. 2011;129(7):1781–1791. doi:10.1002/ijc.25839
40. Ali S, Banerjee S, Ahmad A, et al. Apoptosis-inducing effect of erlotinib is potentiated by 3,3ʹ-diindolylmethane in vitro and in vivo using an orthotopic model of pancreatic cancer. Mol Cancer Ther. 2008;7(6):1708–1719. doi:10.1158/1535-7163.MCT-08-0354
41. Banerjee S, Wang Z, Kong D, et al. 3, 3′-Diindolylmethane enhances chemosensitivity of multiple chemotherapeutic agents in pancreatic cancer. Cancer Res. 2009;69(13):5592–5600. doi:10.1158/0008-5472.CAN-09-0838
42. Kim YH, Kwon HS, Kim DH, et al. 3, 3′-diindolylmethane attenuates colonic inflammation and tumorigenesis in mice. Inflamm Bowel Dis. 2009;15(8):1164–1173. doi:10.1002/ibd.20917
43. Choi HJ, Park JHY. Induction of G1 and G2/M cell cycle arrests by the dietary compound 3, 3ʹ-diindolylmethane in HT-29 human colon cancer cells. BMC Gastroenterol. 2009;9(1):39. doi:10.1186/1471-230X-9-39
44. Bhatnagar N, Li X, Chen Y, et al. 3, 3′-diindolylmethane enhances the efficacy of butyrate in colon cancer prevention through down-regulation of survivin. Cancer Prev Res. 2009;2(6):581–589. doi:10.1158/1940-6207.CAPR-08-0142
45. Femia AP, Garikapaty VPS, Ashok BT, et al. Sulindac, 3, 3ʹ-diindolylmethane and curcumin reduce carcinogenesis in the Pirc rat, an Apc-driven model of colon carcinogenesis. BMC Cancer. 2015;15(1):611. doi:10.1186/s12885-015-1627-9
46. Kim EJ, Park SY, Shin HK, et al. Activation of caspase-8 contributes to 3, 3′-diindolylmethane-induced apoptosis in colon cancer cells. J Nutr. 2007;137(1):31–36. doi:10.1093/jn/137.1.31
47. Kim EJ, Shin M, Park H, et al. Oral administration of 3, 3′-diindolylmethane inhibits lung metastasis of 4T1 murine mammary carcinoma cells in BALB/c mice. J Nutr. 2009;139(12):2373–2379. doi:10.3945/jn.109.111864
48. Ichite N, Chougule MB, Jackson T, et al. Enhancement of docetaxel anticancer activity by a novel diindolylmethane compound in human non–small cell lung cancer. Clin Cancer Res. 2009;15(2):543–552. doi:10.1158/1078-0432.CCR-08-1558
49. Wu T, Chen C, Li F, et al. 3, 3ʹ‑Diindolylmethane inhibits the invasion and metastasis of nasopharyngeal carcinoma cells in vitro and in vivo by regulation of epithelial mesenchymal transition. Exp Ther Med. 2014;7(6):1635–1638. doi:10.3892/etm.2014.1649
50. Xu Y, Zhang J, Shi W, et al. Anticancer effects of 3, 3ʹ-diindolylmethane are associated with G1 arrest and mitochondria-dependent apoptosis in human nasopharyngeal carcinoma cells. Oncol Lett. 2013;5(2):655–662. doi:10.3892/ol.2012.1063
51. Xue L, Pestka J, Li M, et al. 3, 3′-Diindolylmethane stimulates murine immune function in vitro and in vivo. J Nutr Biochem. 2008;19(5):336–344. doi:10.1016/j.jnutbio.2007.05.004
52. Cho HJ, Seon MR, Lee YM, et al. 3, 3′-Diindolylmethane suppresses the inflammatory response to lipopolysaccharide in murine macrophages. J Nutr. 2008;138(1):17–23. doi:10.1093/jn/138.1.17
53. Bradlow HL, Michnovicz JJ, Telang NT, et al. Effects of dietary indole-3-carbinol on estradiol metabolism and spontaneous mammary tumors in mice. Carcinogenesis. 1991;12(9):1571–1574. doi:10.1093/carcin/12.9.1571
54. Roy A, Ganguly A, BoseDasgupta S, et al. Mitochondria-dependent reactive oxygen species-mediated programmed cell death induced by 3, 3′-diindolylmethane through inhibition of F0F1-ATP synthase in unicellular protozoan parasite Leishmania donovani. Mol Pharmacol. 2008;74(5):1292–1307. doi:10.1124/mol.108.050161
55. Bharate SB, Bharate JB, Khan SI, et al. Discovery of 3, 3′-diindolylmethanes as potent antileishmanial agents. Eur J Med Chem. 2013;63:435–443.
56. Roy A, Das BB, Ganguly, A, et al. An insight into the mechanism of inhibition of unusual bi-subunit topoisomerase I from Leishmania donovani by 3, 3′-di-indolylmethane, a novel DNA topoisomerase I poison with a strong binding affinity to the enzyme. Biochem J. 2007;409(2):611–622.
57. Rieck GC, Fiander AN. Human papillomavirus, cervical carcinogenesis and chemoprevention with Indole derivates–a review of pathomechanisms. Mol Nutr Food Res. 2008;52(1):105–113.
58. Sepkovic DW, Stein J, Carlisle AD, et al. Results from a dose–response study using 3, 3′-diindolylmethane in the K14-HPV16 transgenic mouse model: cervical histology. Cancer Prev Res. 2011;4(6):890–896.
59. Auborn KJ, Carter TH. Treatment of human papillomavirus gynecologic infections. Clin Lab Med. 2000;20(2):407–422.
60. Ashrafian L, Sukhikh G, Kiselev V, et al. Double-blind randomized placebo-controlled multicenter clinical trial (phase IIa) on diindolylmethane’s efficacy and safety in the treatment of CIN: implications for cervical cancer prevention. EPMA J. 2015;6(1):25.
61. Luo Y, Wang TT, Teng Z et al. Encapsulation of indole-3-carbinol and 3, 3′-diindolylmethane in zein/carboxymethyl chitosan nanoparticles with controlled release property and improved stability. Food Chem. 2013;139(1–4):224–230.
62. McAlindon T, Gulin J, Chen T, et al. Indole-3-carbinol in women with SLE: effect on estrogen metabolism and disease activity. Lupus. 2001;10(11):779–783.
63. Wong GY, Bradlow L, Sepkovic D, et al. Dose‐ranging study of Indole‐3‐Carbinol for breast cancer prevention. J Cell Biochem. 1997;67(S28‒29):111–116.
64. Rosen CA, Woodson GE, Thomson JW, et al. Preliminary results of the use of indole-3-carbinol for recurrent respiratory papillomatosis. Otolaryngol Head Neck Surg. 1998;118(6):810–815.
65. Yoshida M, Katashima S, Ando J, et al. Dietary indole-3-carbinol promotes endometrial adenocarcinoma development in rats initiated with N-ethyl-N′-nitro-N-nitrosoguanidine, with induction of cytochrome P450s in the liver and consequent modulation of estrogen metabolism. Carcinogenesis. 2004;25(11):2257–2264.
66. Kim DJ, Han BS, Ahn B, et al. Enhancement by indole-3-carbinol of liver and thyroid gland neoplastic development in a rat medium-term multiorgan carcinogenesis model. Carcinogenesis. 1997;18(2):377–381.
67. Pence BC, Buddingh F, Yang SP. Multiple dietary factors in the enhancement of dimethylhydrazine carcinogenesis: main effect of indole-3-carbinol. J Natl Cancer Inst. 1986;77(1):269–276.
68. Anderton MJ, Manson MM, Verschoyle R, et al. Physiological modeling of formulated and crystalline 3,3ʹ-diindolylmethane pharmacokinetics following oral administration in mice. Drug Metab Dispos. 2004;32(6):632–638. doi:10.1124/dmd.32.6.632
69. Sepkovic DW, Bradlow HL, Bell M. Quantitative determination of 3,3ʹ-diindolylmethane in urine of individuals receiving indole-3-carbinol. Nutr Cancer. 2001;41(1–2):57–63.
70. Bradlow HL, Zeligs MA. Diindolylmethane (DIM) spontaneously forms from indole-3-carbinol (I3C) during cell culture experiments. In Vivo (Brooklyn). 2010;24(4):387–391.
71. Zeligs MA, Jacobs IC. Compositions and methods of adjusting steroid hormone metabolism through phytochemicals. Google Patents. 2000
72. Reed GA, Arneson DW, Putnam WC, et al. Single-dose and multiple-dose administration of indole-3-carbinol to women: pharmacokinetics based on 3,3ʹ-diindolylmethane. Cancer Epidemiol Biomarkers Prev. 2006;15(12):2477–2481.
73. Kravchenko LV, Avren'eva LI, Guseva GV, et al. Effect of nutritional indoles on activity of xenobiotic metabolism enzymes and T-2 toxicity in rats. Bull Exp Biol Med. 2001;131(6):544–547.
74. Fujioka N, Ainslie-Waldman CE, Upadhyaya P, et al. Urinary 3,3ʹ-diindolylmethane: a biomarker of glucobrassicin exposure and indole-3-carbinol uptake in humans. Cancer Epidemiol Biomarkers Prev. 2014;23(2):282–287.
75. Fujioka N, Ransom BW, Carmella SG, et al. Harnessing the power of cruciferous vegetables: developing a biomarker for brassica vegetable consumption using urinary 3,3ʹ-diindolylmethane. Cancer Prev Res. 2016;9(10):788–793.
76. Gee JR, Saltzstein DR, Messing E, et al. Phase Ib placebo-controlled, tissue biomarker trial of diindolylmethane (BR-DIMNG) in patients with prostate cancer who are undergoing prostatectomy. Eur J Cancer Prev. 2016;25(4):312–320.
77. Rajoria S, Suriano R, Parmar PS, et al. 3,3ʹ-diindolylmethane modulates estrogen metabolism in patients with thyroid proliferative disease: a pilot study. Thyroid. 2011;21(3):299–304.
78. Heath EI, Heilbrun LK, Li J, et al. A Phase I dose-escalation study of oral BR-DIM (BioResponse 3,3ʹ- Diindolylmethane) in castrate-resistant, non-metastatic prostate cancer. Am J Transl Res. 2010;2(4):402–411.
79. Hwang C, Sethi S, Heilbrun LK, et al. Anti-androgenic activity of absorption-enhanced 3, 3ʹ-diindolylmethane in prostatectomy patients. Am J Transl Res. 2016;8(1):166.
80. Hong C, Kim H-A, Firestone GL, et al. 3, 3′-Diindolylmethane (DIM) induces a G1 cell cycle arrest in human breast cancer cells that is accompanied by Sp1-mediated activation of p21WAF1/CIP1 expression. Carcinogenesis. 2002;23(8):1297–1305.
81. Smith S, Sepkovic D, Bradlow HL, et al. 3, 3′-Diindolylmethane and genistein decrease the adverse effects of estrogen in LNCaP and PC-3 prostate cancer cells. J Nutr. 2008;138(12):2379–2385.
82. Bovee TF, Schoonen WG, Hamers AR, et al. Screening of synthetic and plant-derived compounds for (anti) estrogenic and (anti) androgenic activities. Anal Bioanal Chem. 2008;390(4):1111–1119.
83. Bryant HU, Dere WH. Selective estrogen receptor modulators: an alternative to hormone replacement therapy. Proc Soc Exp Biol Med. 1998;217(1):45–52.
84. Jordan VC. Antiestrogens and selective estrogen receptor modulators as multifunctional medicines. 2. Clinical considerations and new agents. J Med Chem. 2003;46(7):1081–1111.
85. Nuttall ME, Bradbeer JN, Stroup GB, et al. Idoxifene: a novel selective estrogen receptor modulator prevents bone loss and lowers cholesterol levels in ovariectomized rats and decreases uterine weight in intact rats. Endocrinology. 1998;139(12):5224–5234.
86. Oseni T, Patel R, Pyle J, et al. Selective estrogen receptor modulators and phytoestrogens. Planta Med. 2008;74(13):1656–1665.
87. Tsuchiya Y, Nakajima M, Yokoi T. Cytochrome P450-mediated metabolism of estrogens and its regulation in human. Cancer Lett. 2005;227(2):115–124.
88. Martucci CP, Fishman J. P450 enzymes of estrogen metabolism. Pharmacol Ther. 1993;57(2–3):237–257.
89. Bradlow H, Telang N, Sepkovic D, et al. 2-hydroxyestrone: the ‘good’ estrogen. J Endocrinol. 1996;150(3_Suppl):S259–S265.
90. Telang NT, Suto A, Wong GY, et al. Induction by estrogen metabolite 16α;-hydroxyestrone of genotoxic damage and aberrant proliferation in mouse mammary epithelial cells. J Natl Cancer Inst. 1992;84(8):634–638. doi:10.1093/jnci/84.8.634
91. Yuan F, Chen DZ, Liu K, et al. Anti-estrogenic activities of indole-3-carbinol in cervical cells: implication for prevention of cervical cancer. Anticancer Res. 1999;19(3A):1673–1680.
92. Muti P, Bradlow HL, Micheli A, et al. Estrogen metabolism and risk of breast cancer: a prospective study of the 2: 16α-hydroxyestrone ratio in premenopausal and postmenopausal women. Epidemiology. 2000;11(6):635–640.
93. Im A, Vogel VG, Ahrendt G, et al. Urinary estrogen metabolites in women at high risk for breast cancer. Carcinogenesis. 2009;30(9):1532–1535. doi:10.1093/carcin/bgp139
94. Ursin G, London S, Stanczyk FZ, et al. Urinary 2-hydroxyestrone/16α-hydroxyestrone ratio and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1999;91(12):1067–1072.
95. Cauley JA, Zmuda JM, Danielson ME, et al. Estrogen metabolites and the risk of breast cancer in older women. Epidemiology. 2003;14(6):740–744. doi:10.1097/01.ede.0000091607.77374.74
96. Rajoria S, Suriano R, Wilson YL, et al. 3,3ʹ-diindolylmethane inhibits migration and invasion of human cancer cells through combined suppression of ERK and AKT pathways. Oncol Rep. 2011;25(2):491–497. doi:10.3892/or.2010.1076
97. Thomson CA, Chow HHS, Wertheim BC, et al. A randomized, placebo-controlled trial of diindolylmethane for breast cancer biomarker modulation in patients taking tamoxifen. Breast Cancer Res Treat. 2017;165(1):97–107. doi:10.1007/s10549-017-4292-7
98. Nikitina D, Llacuachaqui M, Sepkovic D, et al. The effect of oral 3,3ʹ-diindolylmethane supplementation on the 2:16alpha-OHE ratio in BRCA1 mutation carriers. Fam Cancer. 2015;14(2):281–286. doi:10.1007/s10689-015-9783-2
99. Kotsopoulos J, Zhang S, Akbari M, et al. BRCA1 mRNA levels following a 4-6-week intervention with oral 3,3ʹ-diindolylmethane. Br J Cancer. 2014;111(7):1269–1274. doi:10.1038/bjc.2014.391
100. Turner N, Reis-Filho JS, Russell AM, et al. BRCA1 dysfunction in sporadic basal-like breast cancer. Oncogene. 2007;26(14):2126. doi:10.1038/sj.onc.1210014
101. Thompson ME, Jensen RA, Obermiller PS, et al. Decreased expression of BRCA1 accelerates growth and is often present during sporadic breast cancer progression. Nat Genet. 1995;9(4):444. doi:10.1038/ng0495-444
102. Dobrovic A, Simpfendorfer D. Methylation of the BRCA1 gene in sporadic breast cancer. Cancer Res. 1997;57(16):3347–3350.
103. Van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530. doi:10.1038/415530a
104. Abdelbaqi K,Lack N, Guns ET, et al. Antiandrogenic and growth inhibitory effects of ring‐substituted analogs of 3, 3′‐diindolylmethane (Ring‐DIMs) in hormone‐responsive LNCaP human prostate cancer cells. Prostate. 2011;71(13):1401–1412.
105. Vasaitis T, Belosay A, Schayowitz A, et al. Androgen receptor inactivation contributes to antitumor efficacy of 17α-hydroxylase/17, 20-lyase inhibitor 3β-hydroxy-17-(1H-benzimidazole-1-yl) androsta-5, 16-diene in prostate cancer. Mol Cancer Ther. 2008;7(8):2348–2357.
106. Vivar OI, Lin C-L, Firestone GL, et al. 3, 3′-Diindolylmethane induces a G1 arrest in human prostate cancer cells irrespective of androgen receptor and p53 status. Biochem Pharmacol. 2009;78(5):469–476.
107. Cohen JH, Kristal AR, Stanford JL. Fruit and vegetable intakes and prostate cancer risk. J Natl Cancer Inst. 2000;92(1):61–68. doi:10.1093/jnci/92.1.61
108. Jain MG, Hislop GT, Howe GR, et al. Plant foods, antioxidants, and prostate cancer risk: findings from case-control studies in Canada. Nutr Cancer. 1999;34(2):173–184. doi:10.1207/S15327914NC3402_8
109. Joseph MA, Moysich KB, Freudenheim JL, et al. Cruciferous vegetables, genetic polymorphisms in glutathione S-transferases M1 and T1, and prostate cancer risk. Nutr Cancer. 2004;50(2):206–213. doi:10.1207/s15327914nc5002_11
110. Kolonel LN, Hankin JH, Whittemore AS, et al. Vegetables, fruits, legumes and prostate cancer: a multiethnic case-control study. Cancer Epidemiol Prev Biomarkers. 2000;9(8):795–804.
111. Giovannucci E, Rimm EB, Liu Y, et al. A prospective study of cruciferous vegetables and prostate cancer. Cancer Epidemiol Prev Biomarkers. 2003;12(12):1403–1409.
112. Hsing AW, McLaughlin JK, Schuman LM, et al. Diet, tobacco use, and fatal prostate cancer: results from the Lutheran Brotherhood Cohort Study. Cancer Res. 1990;50(21):6836–6840.
113. Key TJ, Allen N, Appleby P, et al. Fruits and vegetables and prostate cancer: no association among 1104 cases in a prospective study of 130,544 men in the European Prospective Investigation into Cancer and Nutrition (EPIC). Int J Cancer. 2004;109(1):119–124. doi:10.1002/ijc.11671
114. Schuurman AG, Goldbohm RA, Dorant E, et al. Vegetable and fruit consumption and prostate cancer risk: a cohort study in The Netherlands. Cancer Epidemiol Prev Biomarkers. 1998;7(8):673–680.
115. Kong D, Heath E, Chen W, et al. Loss of let-7 up-regulates EZH2 in prostate cancer consistent with the acquisition of cancer stem cell signatures that are attenuated by BR-DIM. PLoS One. 2012;7(3):e33729. doi:10.1371/journal.pone.0033729
116. Li Y, VandenBoom TG, Kong D, et al. Up-regulation of miR-200 and let-7 by natural agents leads to the reversal of epithelial-to-mesenchymal transition in gemcitabine-resistant pancreatic cancer cells. Cancer Res. 2009;69(16):6704–6712. doi:10.1158/0008-5472.CAN-09-1298
117. Lilja H, Ulmert D, Vickers AJ. Prostate-specific antigen and prostate cancer: prediction, detection and monitoring. Nat Rev Cancer. 2008;8(4):268. doi:10.1038/nrc2351
118. Oesterling JE. Prostate-specific antigen and prostate cancer. Curr Opin Urol. 1992;2(5):348–355. doi:10.1097/00042307-199210000-00006
119. Partin AW, Kattan MW, Subong EN, et al. Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer: a multi-institutional update. JAMA. 1997;277(18):1445–1451. doi:10.1001/jama.1997.03540420041027
120. Ahmad A, Kong D, Sarkar SH, et al. Inactivation of uPA and its receptor uPAR by 3, 3′‐diindolylmethane (DIM) leads to the inhibition of prostate cancer cell growth and migration. J Cell Biochem. 2009;107(3):516–527. doi:10.1002/jcb.22152
121. Li Y, Wang Z, Kong D, et al. Regulation of FOXO3a/β-catenin/GSK-3β signaling by 3, 3′-diindolylmethane contributes to inhibition of cell proliferation and induction of apoptosis in prostate cancer cells. J Biol Chem. 2007;282(29):21542–21550. doi:10.1074/jbc.M701978200
122. Kjær SK, van den Brule AJC, Bock JE, et al. Human papillomavirus—the most significant risk determinant of cervical intraepithelial neoplasia. Int J Cancer. 1996;65(5):601–606. doi:10.1002/(SICI)1097-0215(19960301)65:5<601::AID-IJC8>3.0.CO;2-6
123. Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med. 1997;102(5):3–8. doi:10.1016/S0002-9343(97)00177-0
124. Ho GY, Burk RD, Klein S, et al. Persistent genital human papillomavirus infection as a risk factor for persistent cervical dysplasia. J Natl Cancer Inst. 1995;87(18):1365–1371. doi:10.1093/jnci/87.18.1365
125. Schiffman M, Castle PE. Human papillomavirus: epidemiology and public health. Arch Pathol Lab Med. 2003;127(8):930–934.
126. Zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer. 2002;2(5):342. doi:10.1038/nrc798
127. Del Priore G, Gudipudi DK, Montemarano N, et al. Oral diindolylmethane (DIM): pilot evaluation of a nonsurgical treatment for cervical dysplasia. Gynecol Oncol. 2010;116(3):464–467. doi:10.1016/j.ygyno.2009.10.060
128. Paltsev M, Kiselev V, Muyzhnek E, et al. Safety and tolerability of DIM-based therapy designed as personalized approach to reverse prostatic intraepithelial neoplasia (PIN). EPMA J. 2014;5(1):18. doi:10.1186/1878-5085-5-18
129. Paltsev M, Kiselev V, Drukh V, et al. First results of the double-blind randomized placebo-controlled multicenter clinical trial of DIM-based therapy designed as personalized approach to reverse prostatic intraepithelial neoplasia (PIN). EPMA J. 2016;7(1):5. doi:10.1186/s13167-016-0057-3
130. Castanon A, Tristram A, Mesher D, et al. Effect of diindolylmethane supplementation on low-grade cervical cytological abnormalities: double-blind, randomised, controlled trial. Br J Cancer. 2012;106(1):45–52. doi:10.1038/bjc.2011.496
131. Reed GA, Sunega JM, Sullivan DK, et al. Single-dose pharmacokinetics and tolerability of absorption-enhanced 3,3ʹ-diindolylmethane in healthy subjects. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2619–2624. doi:10.1158/1055-9965.EPI-08-0520
132. Lorincz AT, Brentnall AR, Vasiljević N, et al. HPV16 L1 and L2 DNA methylation predicts high-grade cervical intraepithelial neoplasia in women with mildly abnormal cervical cytology. Int J Cancer. 2013;133(3):637–644. doi:10.1002/ijc.28050
133. Morales-Prieto DM, Herrmann J, Osterwald H, et al. Comparison of dienogest effects upon 3,3ʹ-diindolylmethane supplementation in models of endometriosis and clinical cases. Reprod Biol. 2018;18(3):252–258. doi:10.1016/j.repbio.2018.07.002
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.