Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 12
Anomalies and Clinical Significance of Mylohyoid Nerve: A Review
Authors Kini S, Somayaji K , Acharya S, Sampath S
Received 7 July 2020
Accepted for publication 29 August 2020
Published 21 October 2020 Volume 2020:12 Pages 429—436
DOI https://doi.org/10.2147/CCIDE.S269882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Sandya Kini,1 Krishnaraj Somayaji,1 Shashirashmi Acharya,1 Shivakumar Sampath2
1Department of Conservative Dentistry and Endodontics, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, India; 2Department of Conservative Dentistry and Endodontics, Vivekananda Dental College for Women, Tiruchengod, Tamilnadu, India
Correspondence: Krishnaraj Somayaji
Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, India
Tel +918277025409
Email [email protected]
Background: The mylohyoid nerve is a branch of the inferior alveolar nerve (IAN), which is a branch of the posterior division of the mandibular nerve (MN). It is the source of motor nerve supply to the mylohyoid and anterior belly of the digastric muscle. At times, it provides sensory innervation to the mandibular teeth and skin below the chin. Since the location, anatomical variation and communications of the mylohyoid nerve are varied, it becomes clinically important to have an in-depth knowledge when treating patients for dental and maxillofacial procedures. Such anatomical variations of the mylohyoid nerve innervations may account for failure of the nerve blocks and hence, knowledge is very important for the practitioner.
Materials and Methods: A thorough literature search was done using the key words mandibular nerve, communications of the mylohyoid nerve, inferior alveolar nerve, lingual nerve, failure of dental anaesthesia, mylohyoid nerve and dental implants “from the Databases – PubMed, Scopus Embase and Web of Science (years 1952– 2020)”.
Results: The mylohyoid nerve may contain motor and sensory fibres, it may pass through the mylohyoid groove or canal and communicate with other nerves, which is clinically significant. Such anatomical variations may be one of the reasons for the failure of the inferior alveolar nerve block.
Conclusion: Awareness of these variations is very significant in planning treatment and avoiding any unnecessary steps. The most frequently encountered anatomic variation of the mylohyoid nerve was innervation of the submental skin and the anterior teeth.
Keywords: mylohyoid nerve, inferior alveolar nerve, mylohyoid groove, anaesthesia
Introduction
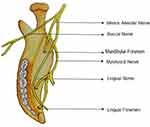
The mylohyoid nerve (MHN) or “nervus mylohyoideus”, stems from the inferior alveolar nerve (IAN), which springs from dorsal division of the mandibular nerve (MN).1 It is given off just before the IAN passes through the mandibular foramen (MF). Then, it passes downwards deep to the mandibular ramus, penetrates the sphenomandibular ligament to enter into the mylohyoid groove and finally lies inferolateral to the mylohyoid muscle (MM), but superior to the anterior belly of the digastric muscle (ADM).1 Though the MHN is considered to be the motor component of the posterior branch of the MN, it is not always consisting of only efferent fibres. It has been reported to have some sensory fibres that convey cutaneous sensation below the chin and lower incisors.2 The MM and ADM, involved in mastication, deglutition, respiration and speech, are innervated by the MHN.3,4 The nerve also carries the sensory information from other teeth.5 Histological study6 revealed that MHN contains fibres that might provide sensory innervation to the mesial root of the mandibular first molar, premolars, incisor teeth and the skin below the chin.7–9 Heasman and Beynon reported innervation of premolars, canine and incisors by the sensory fibres of the MHN in 60% of cases.10 Innervation of skin of the chin was first described by Valentin in 184311 and later reported by others.12 According to a histological observation, Heasman and Beynon concluded the average fibre count of MHN is 1251.13 Due to the small diameter of the nerve it becomes difficult to detect the nerve on magnetic resonance imaging.14 The aim of this review is to discuss and make the clinicians aware of the anomalies of the MHN and its clinical implications.
Materials and Methods
A thorough literature search was done using the key words “”Mandibular nerve, Mylohyoid nerve, Mylohyoid groove, Communications of the mylohyoid nerve, Inferior alveolar nerve, Lingual nerve, Failure of dental anaesthesia, mylohyoid nerve and dental implants“ from
the databases PubMed, Scopus, Embase and Web of Science (years 1952–2019). Apart from this, a literature search was also done using the phrases “Anatomic variations of mylohyoid nerve, Clinical implications of mylohyoid nerve, and Distribution of mylohyoid nerve“.
Out of a total no. of 82 preselected articles and 7 data from other sources (total=89), 5 almost duplicate articles were excluded. Abstracts were screened on the basis of their course and relations, anomalies, distribution and clinical implications. Among the screened articles, 44 articles that were clinically relevant were selected (Original article=19, Review article=5, case report=19, short communication=1, other databases=3). Articles and databases that almost resembled each other in their clinical relevance (articles not resembled=24, articles not in English=2, articles not relevant=7, other sources=4) and those which were not in English were excluded (Figure 1).
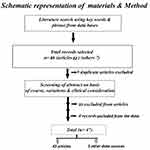 |
Figure 1 Schematic representation of materials and method. |
Anatomical Anomalies of the MHN
Although the MHN classically arises from the IAN, it has different anatomical variations. Such anatomical anomalies cause anaesthetic failures. The origin of the MHN from the IN varies from 13.4 to 14.7 mm superior to the MF15 (Figure 2). Reports of MHN origin from the trunk of the MN are seen in about 10% of cases.16 In these cases, MHNs were posteromedial to the IAN.17 In about 45% of cases, the terminal branches of mylohyoid nerve pass through the small foramina near the symphysis menti of the lower jaw or immediately inferior to premolars to supply the lower incisors, premolars and their soft tissues.18,19 Sutton demonstrated an additional opening related to the MHN and the mylohyoid groove on the deep surface of the lower jaw.20 Haveman and Tebo observed the presence of openings on the medial surface of the mandible in 53.5% cases during their study on 150 dry crania.21 In 68.92% of the samples, a small foramen was observed on the lingual aspect of the mandibular base opposite the premolar region.22 Adding on to the complexity of the MHN variations, there are reports of communications of the LN and MHN.23 Jablonski et al reported the origin of the MHN from the LN. In such cases, sensory fibres of the LN may supply mandibular teeth via branches of the MHN.24 Sinha et al23 reported communication of the mylohyoid and lingual nerves, showing that some of the afferents of the MHN may also supply the tongue, teeth and the skin below the chin. Such communications close to the lower third molar are susceptible for nerve injury during third molar extraction. Sato et al reported, in 1.45% of cases, two large communications between the MHN with the LN in submandibular and submental regions.25 However, Kameda reported 46.3% connection between these nerves.26 An unusual communication between these nerves also was reported after the LN crossed the mandibular third molar3 (Figure 3). The MHN furnishing branches to the muscles and submandibular gland was also reported.27 Other documented variations of the MHN include its origin from the ninth cranial nerve or LN and communications with the plexus of IAN.17 There are case reports of the mylohyoid groove and the nerve duplicated, constricted or rarely covered by an osseous bridge.28 Iwanaga et al28 observed the presence of the mylohyoid canal with many orifices of the mandible. Bennett and Townsend reported incidences of terminal branches of the mylohyoid nerve entering the accessary foramina on the lingual aspect of symphyseal or premolar regions of the lower jaw, to furnish the nerve fibres to the anterior and posterior lower teeth.1 Branches of the MHN within the mandibular canal may directly supply incisor teeth and gingivae or join the incisive nerves of the same or opposite side. Bennett and Townsend,1 in their study, observed the conversion of the mylohyoid groove containing the mylohyoid nerve into a mylohyoid canal by a bridge or plate of bone. Some authors8 were of the opinion that supplementary sensory branches of the MHN passed through the accessary lingual foramina of mandibular symphysis or inferior retromental foramen to supply the incisor teeth and the gingivae (Figure 4). The nerve also communicated with the incisive nerve of the ipsilateral or contralateral side.8 Varol et al reported that the MHN during its course has also been shown to give periosteal twigs to the inner cortex of the mandible and fine sporadic filaments to the LN in the pterygomandibular space.27 The MHN gave many filaments to the MM, submaxillary gland, one sensory branch to the skin along its course, periosteal twigs to the inner cortex of the lower jaw, fine sporadic branches to the LN, distal branches to the ADM and a terminal cutaneous branch called Valentin's27,29 nerve to the skin of submental area. The IAN before entering the MF gave medial and lateral accessory mylohyoid branches, and the medial branch divides into branches to supply the upper and lower surfaces of the MM independently. Its lateral branch communicates with the LN30 (Table 1).
 |
Table 1 Anomalies of the Mylohyoid Nerve |
Results
Variations in the origin, course, communications and distributions of the MHN can be one reason for failure of the IAN.
1.Type of nerve fibres contained in the mylohyoid nerve
Motor fibres supply the MM and ADM, sensory fibres may supply a small area of submental skin, variable number of teeth and sometimes the submandibular gland and LN.
2.Course of the nerve
Normally through the mylohyoid groove, sometimes in the mylohyoid canal.
3. Communication with other nerves
The LN, glossopharyngeal nerve and nerve of the contralateral side.
Discussion
It is very significant for the surgeons to be thorough with the anomalies of the MHN in order to avoid injury and complications to the MHN and its branches during maxillofacial procedures.27 Transient reduced sensation of the lower aspect of the chin around the mental prominence of both sides was reported by a patient after genioplasty due to the damage of cutaneous branches of the MHN.31 Third molar extraction and submandibular glandectomy may also damage the MHN and its branches.32,33 Extraction of the last mandibular molar may injure the communications between the MHN and LN, leading to impairment of anterior two-third tongue sensation. Varol et al reported damage of the MHN during reduction of the mylohyoid ridge, symphysis/parasymphyseal fractures and severing of muscles in the floor of the oral cavity in the process of genioplasty.27 Hence, prior to surgical procedures, the use of an accurate method such as cone beam computed tomography is of prime importance in order to know the course of the nerve and its relation to the surrounding anatomical structures.34
Injury to the LN during the surgical procedures will not lead to complete paraesthesia of the oral part of the tongue of the respective side because of communication of the LN and MHN. Such communications are also significant in the functional recovery of the LN.32,33 Communication of the accessory MHN nerve and lingual nerve has been reported.35 These anatomical anomalies are important to understand the cause of pathological conditions like treatment failure of trigeminal neuralgia. The variations may lead to local nerve block failure or accidental surgical injuries. Awareness of abnormal connections is important in the management of lesions in the infratemporal fossa.36
Investigators37 had done a standardized bilateral sagittal split osteotomy in 40 hemi-mandibles of cadavers to analyse the association of the lingual fracture line and the mylohyoid groove. In 30% of cases, the mylohyoid groove is crossed by lingual fracture lines (12/40). This shows a significant relationship between the mylohyoid groove and lingual fracture line and possible injury to the MHN. The concept of the mylohyoid groove forming the line of least resistance for the lingual fracture was therefore partly true.
Loughner et al38 observed a rare entrapment of the MHN as it passes through the lateral pterygoid muscle in a cadaver. Such trauma to the MHN may result in poorly localized deep pain from the muscles supplied by the nerve. Muscular paresis can also result from long-standing pressure of the nerve. Difficulty in swallowing may also be provoked by bilateral nerve compression.
Inferior alveolar nerve block (IANB) is the normally used technique for anaesthesia for the surgeries of the mandible and procedures of the teeth. This block has a notable failure rate from 38 to 90%.18 Anatomic variations of the MHN, such as the more the distance between its origin from the IAN and the site of deposition of the anaesthetic solution, the greater are the chances the MHN may not be fully anaesthetized. Other reasons could be the presence of accessory mylohyoid nerve, potential physical barriers such as the pterygomandibular fascia and the sphenomandibular ligament that may obstruct diffusion of anaesthetic solution during an IANB. The density and shape of the physical barriers can stop effective diffusion of anaesthetic agents during IANB. In the same way, if part of the MHN course is enclosed by bone, the latter may be a potential barrier.39 Other reasons for anaesthetic failures which the clinician has to keep in mind are psychological issues such as exaggerated pain and uneasiness, or even severe infections which are localized within the pterygomandibular space that reduce the effectiveness of the local anaesthesia.40 In recent times, the dynamics of infiltration of local anaesthesia is analysed using computed tomographic imaging.41 In such failures, regional anaesthesia such as the Gow-Gates and Akinosi methods are the best techniques for cases where the conventional IANB fails. Nevertheless, these extra oral methods have the potency to lead to excess complications than standard nerve block. The clinician should be aware of the fact that the higher the needle insertion in the above techniques, the more chances of injury to the maxillary artery and the pterygoid plexus. This may lead to blanching and pain due to arteriospasm caused by piercing the maxillary artery. Tearing of the wall of pterygoid venous plexus of vessels can lead to formation of haematoma.41 Numerous additional techniques given as supplementary injection techniques include the mental and incisive nerve block, intraligamentary, intraosseous and intra-pulpal anaesthesia. Stein et al highlighted the importance of supplemental injection to the MHN for the favourable result of IANB.42 Stein et al42 stressed the significance of mylohyoid block infiltration into the thin cortical bone of the mandible. The mylohyoid nerve anaesthesia technique is achieved by infiltrating the anaesthetic solution 1.5 cm inside the oral floor supraperiostally under the mylohyoid muscle at the level of the distal root of the first mandibular molar tooth.7 Clark et al18 in their study found that MHN block, with or without a concomitant IANB, will not furnish or increase anaesthesia to the lower incisors and adjacent soft tissues. At times, cross-innervations across the midline with the nerve fibres of the opposite side of the lower central incisors will lead to failure of complete anaesthesia during root canal treatment. In such cases, an additional infiltration or intrapulpal anaesthesia will be mandatory.40
During the placement of mandibular molar implants, there is a possibility of permanent damage to the neurovascular structure of the IAN which can cause damage to venous or arterial structures leading to serious systemic complications. In such clinical scenarios, anaesthetizing the MHN and buccal nerve is a safe and simple alternative technique as compared to a standard IANB. Anaesthesia of the mylohyoid and the buccal nerves has been successful in anaesthetizing the posterior mandibular ridge.7 Since MHN supplies only lingual cortical bone, it is supplemental and its blockage cannot anaesthetize the lower molar tooth completely.43
Microdissection studies proved the presence of both motor and sensory fibres in the MHN. Such sensory fibres of the MHN pass through the communication between the MHN and LN to provide sensory innervation to the tongue. Such innervations show the impairment of tongue sensation in lesions of the posterior part of the MHN without lesions of the LN. Such communications may also help in recovery of LN nerve function after its injury during the extraction of a mandibular third molar.32 Trigger points in the ADM which is supplied by the MHN can lead to referred pain in the tooth. Recent studies have shown feasibility of choosing the MHN as a donor in a reanimation procedure of the facial nerve. The MHN could be interchanged to the facial nerve trunk with limited morbidity.44
Though MHN arises just before the IAN entering the MF, which is located in the ventral and inferior two-thirds of the mandibular ramus, there is a case report where the origin of the MHN is within the mandibular canal and emerged from a small mylohyoid foramen on the inner aspect of the mandibular angle. Invariably, such understanding is of paramount importance during reconstructive surgeries of the mandibular region.45,46
Conclusions
Variations of embryological origin and their ignorance can pose unusual difficulty for surgeons and clinicians. Variations are very crucial and need to be noted for procedures such as placement of implants over an edentulous mandible, osteotomies, submandibular region surgeries, removal of tori, harvesting a graft, and screw placement in cases of fracture management and also during normal clinical procedures. Knowledge of anatomical anomalies and communications of the MHN prepare the surgeon for a better diagnosis and efficient treatment planning, and minimizing complications to the patient.
Acknowledgment
The authors are thankful to Manipal Academy of Higher Education and Manipal College of dental science for their constant support.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest for this work.
References
1. Bennett S, Townsend G. Distribution of the mylohyoid nerve: anatomical variability and clinical implications. Aust Endod J. 2001;27(3):109–111. doi:10.1111/j.1747-4477.2001.tb00470.x.
2. Kim SY, Hu KS, Chung IH, Lee EW, Kim HJ. Topographic anatomy of the lingual nerve and variation in communication pattern of the mandibular nerve branches. Surg Radiol Anat. 2004;26(2):128–135. doi:10.1007/s00276-003-0179-x.
3. Potu BK, D’Silva SS, Thejodhar P, Jattanna NC. An unusual communication between the mylohyoid and lingual nerves in man: its significance in lingual nerve injury. Indian J Dent Res. 2010;21(2):141–142. doi:10.1007/s00276-003-0179-x.
4. Oth O, Louryan S, Van Sint Jan S, Rooze M, Glineur R. Impact of the mandibular divergence on the position of the inferior alveolar nerve and mylohyoid nerve: a computed tomography study and its relevance to bilateral sagittal split osteotomy. Surg Radiol Anat. 2013;35(3):241–247. doi:10.1007/s00276-012-1010-3.
5. De Santis GL, Lievow C. Four common mandibular anomalies that lead to local anesthesia failure. J Am Dent Assoc. 1996;127(7):1081–1086. doi:10.14219/jada.archive.
6. Frommer J, Mele FA, Monroe CW. The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc. 1972;85(1):113–117. doi:10.14219/jada.archive.1972.0285
7. Altug HA, Sencimen M, Varol A, Kocabiyik N, Dogan N, Gulses A. The efficacy of mylohyoid nerve anesthesia in dental implant placement at the edentulous posterior mandibular ridge. J Oral Implantol. 2012;38(2):141–147. doi:10.1563/AAID-JOI-D-10-00037.
8. Madeira MC, Percinoto C, Silva MDGM. Clinical significance of supplementary innervation of the lower incisor teeth: a dissection study of the mylohyoid nerve. Oral Surg Oral Med Oral Pathol. 1978;46(5):608–614. doi:10.1016/0030-4220(78)90455-3.
9. Madhyastha S, Prabhu LV, Saralaya VV, Nayak SR, D’Costa S, Acharya A. Dual innervations of mylohyoid muscle: a case report. Rom J Morphol Embryo. 2009;50(2):305–306.
10. Heasman PA, Beynon AD. The role of the mylohyoid nerve in mandibular tooth innervation. J Dent. 1986;14(2):80–81. doi:10.1016/0300-5712(86)90057-6.
11. Valentin G. Traité de neurologie. 2009.Paris: JB Bailliére; 1843–1880.
12. Hwang K, Han JY, Chung IH, Hwang SH. Cutaneous sensory branch of the mylohyoid nerve. J Craniofac Surg. 2005;16(3):343–345. doi:10.1097/01.scs.0000147393.29488.b4
13. Heasman PA, Beynon AD. Quantitative and spectrum analysis of human mylohyoid nerves. J Anat. 1987;151:45–49.
14. Fujii H, Fujita A, Yang A, et al. Visualization of the peripheral branches of the mandibular division of the trigeminal nerve on 3D double-echo steady-state with water excitation sequence. AJNR Am J Neuroradiol. 2015;36(7):1333–1337. doi:10.3174
15. Wilson S, Johns P, Fuller PM. The inferior alveolar and mylohyoid nerves: an anatomic study and relationship to local anaesthesia of the anterior mandibular teeth. J Am Dent Assoc. 1984;108(3):350–352. doi:10.14219/jada.archive.1984.0005.
16. Kumar S, Kumar CJ, Bhat S, Kumar A. Anatomical study of the unusual origin of a nerve to the mylohyoid muscle and its clinical relevance. Br J Oral Maxillofac Surg. 2011;49(5):e14–e15. doi:10.1016/j.bjoms.2010.08.001.
17. Tubbs RS, Shoja MM, Loukas M. Bergman’s Comprehensive Encyclopaedia of Human Anatomic Variation. Hobojken, NJ: John Wiley & Sons; 2016.
18. Clark S, Reader A, Beck M, Meyers WJ. Anaesthetic efficacy of the mylohyoid nerve block and combination inferior alveolar nerve block/mylohyoid nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87(5):557–563. doi:10.1016/s1079-2104(99)70133-2.
19. He P, Truong MK, Adeeb N, Tubbs RS, Iwanaga J. Clinical anatomy and surgical significance of the lingual foramina and their canals. Clin Anat. 2017;30(2):194–204. doi:10.1002/ca.22824
20. Sutton RN. The practical significance of mandibular accessory foramina. Aust Dent J. 1974;19(3):167–173. doi:10.1111/j.1834-7819.1974.tb05034.x
21. Haveman CW, Tebo HG. Posterior accessory foramina of the human mandible. J Prosthet Dent. 1976;35(4):462–468. doi:10.1016/0022-3913(76)90015-9.
22. Chapnick L. A foramen on the lingual of the mandible. J Can Dent Assoc. 1980;46(7):444–445.
23. Sinha P, Tamang BK, Sarda RK. Communication between mylohyoid and lingual nerve: an anatomical variation. J Clin Diagn Res. 2014;8(4):AD01–AD02. doi:10.7860/JCDR/2014/7560.4223.
24. Jablonski T, Cheng NG, Cheng CM. Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol. 1985;60(5):487–488. doi:10.1016/0030-4220(85)90235-x.
25. Sato I, Sunohara M, Ueno R, Yoshida S. Branch of mylohyoid and lingual nerves on submandibular and submental triangles. Okajimas Folia Anat Jpn. 2004;81(2–3):45–48. doi:10.2535/ofaj.81.45.
26. Kameda K. Mandibularis bei Japanern. Acta Inst Anat Niigataensis. 1952;28:15–37.
27. Varol A, Sencimen M, Kocabiyik N, Gulses A, Ozan H. Clinical and anatomical aspects of possible mylohyoid nerve injury during genioplasties. Int J Oral Maxillofac Surg. 2009;38(10):1084–1087. doi:10.1016/j.ijom.2009.06.019
28. Iwanaga J, Watanabe K, Saga T, et al. A novel method for observation of the mandibular foramen: application to a better understanding of dental anatomy. Anat Rec (Hoboken). 2017;300(10):1875–1880. doi:10.1002/ar.23639
29. Guyot L, Cheynet F, Faissal A, Gola R. Valentine’s nerve: preliminary report of the innervation of the mental region. Rev Stomatol Chir Maxillofac. 1998;99:106–114.
30. Jha S, Khorwal G. A rare case of accessory nerve to mylohyoid communicating with lingual nerve and its clinical implications. Int J Anat Res. 2018;6(3.2):5550–5553. doi:10.16965/ijar.2018.279
31. Guyot T, Layoun W, Richard O, Cheynet F, Gola R. Alteration of chin sensibility due to damage of the cutaneous branch of mylohyoid nerve during genioplasty. J Oral Maxillofac Surg. 2002;60(11):1371–1373. doi:10.1053/joms.2002.35753.
32. Fazan VPS, Rodrigues Filho OA, Matamala F. Communication between the mylohyoid and lingual nerves: clinical implications. Int J Morphol. 2007;25(3):561–564. doi:10.4067/S0717-95022007000300015
33. Adjei SS, Hammersley N. Mylohyoid nerve damage due to excision of the submandibular salivary gland. J Oral Maxillofac Surg. 1989;27(3):209–211. doi:10.1016/0266-4356(89)90146-0.
34. Pippi R, Santoro M, Ambrosio FD. Accuracy of cone-beam computed tomography in defining spatial relationships between third molar roots and inferior alveolar nerve. Eur J Dent. 2016;10(04):454–458. doi:10.4103/1305-7456.195168
35. Thotakura B, Rajendran SS, Gnanasundaram V, Subramaniam A. Variations in the posterior division branches of the mandibular nerve in human cadavers. Singapore Med J. 2013;54(3):149. doi:10.11622/smedj.2013051.
36. Roy TS, Sarkar AK, Panicker HK. Variations in the origin of the inferior alveolar nerve. Clin Anat. 2002;15(2):143–147. doi:10.1002/ca.1110.
37. Mensink G, Gooris PJ, Bergsma EJ, Frank MH, van Gemert JT, van Merkesteyn JP. Is the lingual fracture line influenced by the mandibular canal or the mylohyoid groove during a bilateral sagittal split osteotomy? A human cadaveric study. J Oral Maxillofac Surg. 2014;72(5):973–979. doi:10.1016/j.joms.2013.09.043.
38. Loughner BA, Larkin LH, Mahan PE. Nerve entrapment in the lateral pterygoid muscle. Oral Surg Oral Med Oral Pathol. 1990;69(3):299–306. doi:10.1016/0030-4220(90)90290-9.
39. Barker BC. Anatomy of the hard and soft tissues of the oral cavity. Ann Aust Coll Dent Surg. 1969;2:22–38.
40. Meechan J. How to overcome failed anaesthesia. Br Dent J. 1999;186(1):15–20. doi:10.1038/sj.bdj.4800006.
41. Takasugi Y, Furuya H, Moriya K, Okamoto Y. Clinical evaluation of inferior alveolar nerve block by injection into the pterygomandibular space anterior to the mandibular foramen. Anesth Prog. 2000;47(4):125–129.
42. Stein P, Brueckner J, Milliner M. Sensory innervation of mandibular teeth by the nerve to the mylohyoid: implications in local anesthesia. Clin Anat. 2007;20(6):591–595. doi:10.1002/ca.20479.
43. Choi P, Iwanaga J, Dupont G, Oskouian RJ, Tubbs RS. Clinical anatomy of the nerve to the mylohyoid. Anat Cell Biol. 2019;52(1):12–16. doi:10.5115/acb.2019.52.1.12.
44. Tubbs RS, Loukas M, Shoja MM, et al. The nerve to the mylohyoid as a donor for facial nerve reanimation procedures: a cadaveric feasibility study. J Neuro Surg. 2007;106(4):677–679. doi:10.3171/jns.2007.106.4.677.
45. Nayak SB, Soumya KV. Mylohyoid foramen of mandible: a rare exit point of intra-mandibular origin of nerve to mylohyoid. Anat Cell Biol. 2020;53(1):114–116. doi:10.5115/acb.19.186.
46. Somayaji SK, Acharya SR, Mohandas KG, Venkataramana V. Anatomy and clinical applications of the mandibular nerve. Bratisl Med J. 2012;113(7):431–440. doi:10.4149/bll_2012_097.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.