Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 9
Anemia among adult HIV patients in Ethiopia: a hospital-based cross-sectional study
Authors Melese H, Wassie MM, Woldie H, Tadesse A , Mesfin N
Received 30 August 2016
Accepted for publication 13 January 2017
Published 14 February 2017 Volume 2017:9 Pages 25—30
DOI https://doi.org/10.2147/HIV.S121021
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Hermela Melese,1 Molla Mesele Wassie,2 Haile Woldie,2 Abilo Tadesse,3 Nebiyu Mesfin3
1HIV Follow-up Care Clinic, Debre-Tabor Hospital, Debre‑Tabor, 2Department of Human Nutrition, Institute of Public Health, 3Department of Internal Medicine, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Anemia is a major public health problem in HIV patients around the world. It has a negative effect on the quality of life of HIV patients and progression of the HIV disease. In the sub-Saharan African setting, including Ethiopia where both HIV infection and under-nutrition are expected to be high, there is a paucity of data on the matter. This study was aimed to reveal the magnitude and factors associated with anemia among adult HIV patients in Debre-Tabor Hospital, northwest Ethiopia.
Methods: A hospital-based cross-sectional study was used among adult HIV patients in Debre-Tabor Hospital from April 1 to May 30, 2015. The diagnosis of anemia was made following the 2011 World Health Organization recommendation on hemoglobin cut-off points. Univariable and multivariable logistic regression was carried out to assess factors associated with anemia.
Results: A total of 377 patients’ charts were reviewed. Most of the participants (n=237, 62.9%) were taking antiretroviral treatment (ART). The overall prevalence of anemia was 23% (95% CI: 19.1, 27.6). Being ART-naïve (adjusted odds ratio [AOR]: 3.37; 95% CI: 1.59, 7.14), having treatment history with anti-tuberculosis (TB) drug (AOR: 3.2; 95% CI: 1.19, 8.67), taking zidovudine (ZDV)-containing ART regimen (AOR: 2.14; 95% CI: 1.03, 4.57), and having recent CD4+ T-lymphocytes count of <200 cells/µL (AOR: 2.13; 95% CI: 1.04, 4.36) were associated with occurrence of anemia among adult HIV patients.
Conclusion and recommendation: Anemia continues to be a major co-morbidity among adult HIV patients in Ethiopia. Adult HIV patients who are taking ZDV-containing ART, with a history of TB treatment, have a low CD4+T-lymphocytes count and are ART-naïve should be carefully screened and treated for anemia.
Keywords: anemia, HIV/AIDS, antiretroviral treatment, ZDV toxicity, Ethiopia
Background
Anemia is a major health problem globally, which can cause a vicious impediment on quality of life, mortality, morbidity, and socioeconomic progress of a country. It affects more the developing than the developed countries.1 Anemia is the most common hematologic abnormality among HIV-infected individuals; this includes those who are taking antiretroviral treatment (ART) and those who are ART-naïve.2
Anemia among HIV patients can lead to impaired physical functioning, psychological distress, poor quality of life, accelerated disease progression, and shorter life expectancy.3 Although anemia can occur at any stage of HIV infection, its severity is correlated with progression of the HIV disease stage.4 A study conducted in the very early years of HIV discovery had shown the overall prevalence of anemia to be about 28% among people with HIV infection in the pre-AIDS stage of the disease, whereas it could reach as high as 71% in the advanced or AIDS stage of the HIV disease.5
According to reports, the prevalence of anemia among adult HIV patients taking ART ranges between 23% and 50% globally and 24% and 58% in Africa.6–9 Generally, the prevalence of anemia tends to be higher in ART-naïve patients compared to ART users. In Ethiopia, the prevalence of anemia among ART-naïve adult HIV patients was reported to reach up to 35%.10 A study done 3 years ago in the southwest part of Ethiopia has shown the prevalence of anemia to be 29.9% and 16.2% among ART-naïve and ART-experienced HIV patients, respectively.11 Another study conducted 3 years ago in southern Ethiopia has shown the prevalence of anemia among ART-naïve adult HIV patients to be 23.4%, and the prevalence after 6-month course of ART was only 12%.12
Various reports have identified different factors to have association with anemia among adult HIV patients including gender, residence, marital status, educational status, income, duration of ART, type of ART regimen, history of anti-tuberculosis (TB) drug treatment, presence of opportunistic infections (OIs), advanced stage of the HIV disease, CD4+T-lymphocyte count <200 cells/µL, white blood cell (WBC) count <4,000 cells/µL, and platelets count <200,000 cells/µL.7,11–19
However, the reported magnitudes and associated factors are different from one geographic area to another and have shown different time trends as the interplay between the various socioeconomic, health, and nutritional conditions alter in sub-Saharan country setting. Therefore, this study was aimed at assessing the prevalence of anemia and its associated factors among adult HIV patients who were getting follow-up HIV care at Debre-Tabor Hospital, northwest Ethiopia.
Methods
Study design and setting
Hospital-based quantitative cross-sectional study was conducted from April 1 to May 30, 2015, at Debre-Tabor Hospital located in northwest Ethiopia. The hospital is found in Amhara Regional State in the town called Debre-Tabor, which is 665 km northwest of the capital city Addis Ababa. The hospital has a catchment population of nearly 2.3 million people and is one of the HIV-care providing centers in the region. It has an average daily patient flow of 20–30 adult HIV patients in the working hours of the HIV-care clinic of the hospital excluding emergency presentations on duty hours.
Sample size determination, sampling procedure, and study subjects
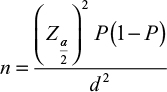
The sample size was calculated based on single population proportion formula using a confidence interval (CI) of 95% and previous prevalence of anemia being 35% among ART-naïve HIV patients,10
|
Where, n = sample size, P = prevalence of anemia among ART-naïve HIV patients and d = assumed marginal error.
Finally, a minimum sample size of 385 was calculated after anticipating a 10% non-response rate. Simple random sampling technique was used to recruit 385 patients’ charts from a total of 689. The study populations were all adult HIV patients above the age of 18 years who were on HIV follow-up care at Debre-Tabor Hospital during January 1, 2010 to December 30, 2014, regardless of their ART status. Those adult patients with incomplete information for hemoglobin (Hb) status on the chart, either at baseline or during follow-up; pregnant women; and women in the post-partum period were excluded from the study.
Data collection instrument and procedures
Pretested and structured questionnaires were used to collect the data. The questionnaires were constructed with sociodemographic and economic characteristics; hematological characteristics; and disease stage, medication treatment, and co-morbidity status-related characteristics. The questionnaires were prepared in English. A total of four health professionals, three ART nurses as data collectors, and one public health officer as supervisor were recruited for the data collection process of this study. The 2011 World Health Organization (WHO) report on Hb concentration level to diagnose anemia was used in the hospital.20 Accordingly, anemia for males was defined as Hb concentration <13 g/dL (11.0–12.9 g/dL=mild; 8.0– 10.9 g/ dL moderate, and <8.0 g/dL=severe), whereas anemia for females was defined as Hb <12.0 (11.0–11.9 g/ dL=mild, 8.0–10.9 g/dL=moderate, and <8.0 g/dL=severe).
Data quality control
The data collection tool was pre-tested without Hb status determination on 5% of sample size charts of HIV/AIDS patients before the actual data collection period. Training was given to recruited data collectors and supervisor. All questionnaires were checked during the data collection period by the responsible supervisor on daily basis to check completeness, clarity, and consistency. Before analysis, the data were cleaned thoroughly to check for errors during entry.
Data processing and analysis
Data were entered into Epidemiological Information (EPI INFO), version 7.1 and analyzed using the Statistical Package for Social Sciences (SPSS) version 20. Descriptive statistics, including frequencies and proportions, was used to summarize the study variables. Univariable and multivariable logistic regression was used for factors associated with Hb status of the study subjects. Those variables with a P-value of <0.2 in the univariable analysis were exported to multivariable analysis to control the possible effect of confounders. The adjusted odds ratio (AOR) at a 95% confidence interval and P-value of ≤0.05 was used to declare the statistical significance in the multivariable analysis.
Ethical approval
Ethical clearance was obtained from the institutional review board of the Institute of Public Health of University of Gondar. Permission letter for the next steps was secured from the Debre-Tabor Hospital administrative body. Written informed consent was obtained from participants, and the confidentiality of information obtained was maintained by coding and restricting access to the questionnaire.
Results
We did not include the planned sample of 385 patients’ charts due to incomplete documentations identified in some charts. Therefore, a total of 377 patients’ chart were reviewed in this study out of which 237 (62.9%) were from patients taking ART and 140 (37.1%) were ART-naïve. More than 60% of the study participants were female, and the mean age of the study subjects was 35.21 with a standard deviation (SD) of ±9.27 years. Three hundred and seventy-five (99.5%) of the participants were Amhara by ethnicity and 367 (97.3%) were orthodox Christian by religion. A total of 291 participants (77.2%) were urban residents and 191 (50.5%) were married (Table 1).
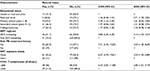
Eighty-seven participants (23%) were found to have anemia out of whom 61 were among the 112 ART-naïve patients making the prevalence of anemia in this group 54.5%. One hundred twenty-six (33.4%) participants had a CD4+ T-lymphocyte count <200 cells/µL. Seventy-three (19.4%) had a WBC count <4000 cells/µL. Seventy-six (20.2%) study participants had a platelet count of <200,000 cells/µL. Nearly three fourths of patients taking ART were found to have a normal nutritional status (Table 2).
Hundred and ninety-one (50.7%) of the participants have had OIs, and <7% of the participants were found to be at the fourth stage of WHO’s clinical disease classification. One hundred and twelve (29.7%) of the study participants were taking zidovudine (ZDV) containing ART regimen. More than 90% of the study participants had no history of anti-TB treatment (Table 3).
In the bivariate logistic regression analysis, educational status, types of ART regimen, history of treatment with anti-TB drugs, duration of ART usage, history of OI, WHO ; ZDV, Zidovudine. stage of HIV disease, CD4+ T-lymphocyte count, WBC count and platelets count were significantly associated with anemia. In the multivariate binary logistic regression analysis, type of ART regimen, ART-usage status, history of treatment with anti-TB drugs, and CD4+ T-lymphocyte count remained to be significantly associated with anemia (Table 3).
Being ART-naïve was found to be associated with anemia (AOR: 3.37; 95% CI: 1.59, 7.14). Having treatment history with anti-TB drug was also found to be associated with anemia (AOR: 3.2; 95% CI: 1.19, 8.67). Taking ZDV-containing regimen was found to be associated with anemia (AOR: 2.1; 95% CI: 1.03, 4.57). Having a recent CD4+ T-lymphocyte count of <200 cells/µL was also found to be associated with anemia (AOR: 2.1; 95% CI: 1.04, 4.36).
Discussion
Our study has demonstrated a high overall prevalence (23%) of anemia among HIV patients who are ART-naïve and taking ART. This finding is concordant with a study done 3 years ago in the southwest Ethiopia (23.1%);13 similar findings were reported from studies in India (23%)6 and Ghana (24%).8 The prevalence was lower compared to the a study done 3 years ago from northwest Ethiopia (35%); however, that study included only ART-naïve HIV patients.10 Another study also done 3 years ago in southern Ethiopia reported the prevalence of anemia to be 23.4% among ART-naïve adult HIV patients and only 12% after 6-month course of ART.12 Studies in Indonesia7 (49.6%), Nigeria9 (57.5%), and Uganda18 (47.8%) have reported a much higher prevalence of anemia compared to our study. However, in addition to the sociodemographic differences, those reports reflected the prevalence of anemia among ART-naïve patients. In our study where two thirds of the participants were taking ART, it is expected to get lower prevalence.
Various studies have pointed out multiple potential factors associated with anemia among HIV patients.7,11–19 Being ART-naïve was found to be associated with anemia in our study. This finding is in agreement with the reports from southern Ethiopia,12,13 Ghana,8 and South Africa.11 This can be explained by the various direct and indirect effects of the effective ART. One plausible explanation is the fact that ART can suppress HIV, a virus which is known to directly affect the bone marrow; therefore, by suppressing the viral load ART could prevent anemia. The other explanation could be related to the indirect effect of ART, which is expected to improve the immunity of HIV patients thereby decreasing the occurrence of multiple OIs, which are identified to potentially cause anemia.
Type of ART regimen, ZDV-containing regimen, was also found to be associated with anemia among HIV patients in this study. This finding is in concordance with reports from Addis Ababa,15 Cambodia,19 and Iran.16 Zidovudine (ZDV) has long been identified to be a potential cause of anemia in HIV patients especially early in the ART initiation and with low baseline Hb.19
Additionally, a history of treatment with anti-TB drugs was significantly associated with anemia in our study. A similar finding was reported from the study done in Iraq.16 Since TB is known to cause anemia through various mechanisms including anemia of chronic illness, bone marrow involvement, malnutrition and hemoptysis, the presence of TB treatment history could partly suggest susceptibility of those HIV patients for anemia from the TB. Moreover, the anti-TB drugs such as isoniazid are identified to cause anemia.
The CD4+ T-lymphocyte count, <200 cells/µL, was found to be associated with anemia. Similar findings were reported by various studies in southern Ethiopia,12,13 Cambodia,19 and South Africa.11 The possible explanation for this association includes the fact that HIV patients with low CD4+ T-lymphocyte count are known to be at risk of multiple OIs, which are known to cause anemia, and the fact that such patients are also likely to have high HIV viral load which could lead to viral infiltration of the bone marrow subsequently causing anemia.
Since the causes and types of anemia in HIV patients are multi-factorial, we recognize the inability of this study to identify the specific types and specific causes of anemia as a limitation.
Conclusion and recommendation
Anemia continues to be a major co-morbidity among adult HIV patients in Ethiopia. Adult HIV patients who are taking ZDV-containing ART, with a history of TB treatment, have low CD4+T-lymphocytes count and ART-naïve should be carefully screened and treated for anemia. We recommend further longitudinal studies to determine predictors of anemia in the setting and intervention programs to change the existing situation.
Acknowledgments
The authors thank University of Gondar for financing the study and Debre-Tabor Hospital for approving and facilitating the study.
Author contributions
HM conducted the study, participated in the data analysis, and interpreted the findings. HM, MMW, HW, AT, and NM participated in the design of the study, data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
McLean E, Cogswell M, Egli I, Wojdyla D, De Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutrition. 2009;12(4):444–454. | ||
Pande A, Bhattacharyya M, Pain S, et al. Anemia in antiretroviral naïve HIV/AIDS patients: a study from Eastern India. Online J Health All Sci. 2011;10(4):1–5. | ||
Volberding PA, Levine AM, Dieterich D, Mildvan D, Mitsuyasu R, Saag M. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38(10):1454–1463. | ||
De Santis GC, Brunetta DM, Vilar FC, et al. Hematological abnormalities in HIV-infected patients. Int J Infect Dis. 2011;15(12):e808–e811. | ||
Zon LI, Groopman JE. Hematologic manifestations of the human immunodeficiency virus (HIV). Semin Hematol. 1988;25(3):208–218. | ||
Bhattad D, Kulkarni V, Bhave A, Balasubramanian M, Upase DP, Khude S. Refractory anaemia in an immunocompromised patient–What is it? J Assoc Physicians India. 2013;61(9):673–675. | ||
Wisaksana R, Sumantri R, Indrati AR et al. Anemia and iron homeostasis in a cohort of HIV-infected patients in Indonesia. BMC Infect Dis. 2011;11:213. | ||
Owiredu WK, Quaye L, Amidu N, Addai-Mensah O. Prevalence of anaemia and immunological markers among Ghanaian HAART-naïve HIV-patients and those on HAART. Afr Health Sci. 2011;11(1):2–15. | ||
Denue BA, Kida IM, Hammagabdo A, Dayar A, Sahabi MA. Prevalence of anemia and immunological markers in HIV-infected patients on highly active antiretroviral therapy in Northeastern Nigeria. Infect Dis (Aucki). 2013;6:25–33. | ||
Ferede G, Wondimeneh Y. Prevalence and related factors of anemia in HAART-naive HIV positive patients at Gondar University Hospital, Northwest Ethiopia. BMC Hematol. 2013;13(1):8. | ||
Gedefaw L, Yemane T, Sahlemariam Z, Yilma D. Anemia and risk factors in HAART naïve and HAART experienced HIV positive persons in south west Ethiopia: a comparative study. PLoS One. 2013;8(8):e72202. | ||
Daka D, Lelissa D, Amsalu A. Prevalence of anemia before and after the initiation of antiretroviral therapy at ART centre of Hawassa University Referral Hospital, Hawassa, South Ethiopia. Sch J Med. 2013;3(1):1–6. | ||
Takuva S, Maskew M, Brennan AT, Sanne I, MacPhail AP, Fox MP. Anemia among HIV-infected patients initiating antiretroviral therapy in South Africa: improvement in hemoglobin regardless of degree of immunosuppression and the initiating ART regimen. J Trop Med. 2013;2013:162950. | ||
Owiredu WK, Quaye L, Amidu N, Addai-Mensah O. Prevalence of anaemia and immunological markers among Ghanaian HAART-naïve HIV-patients and those on HAART. Afr Health Sci. 2011;11(1):2–15. | ||
Wolde HM, Lerebo WT, Melaku YA, Girmay KH. Incidence and risk factors of anemia among HIV/AIDS patients taking anti-retroviral therapy at tertiary hospitals in Addis Ababa, Ethiopia: a Retrospective Cohort Study. J HIV AIDS Infect Dis. 2014;2:1–62. | ||
Meidani M, Rezaei F, Maracy MR, Avijgan M, Tayeri K. Prevalence, severity, and related factors of anemia in HIV/AIDS patients. J Res Med Sci. 2012;17(2):138–142. | ||
Subbaraman R, Chaguturu SK, Mayer KH, Flanigan TP, Kumarasamy N. Adverse effects of highly active antiretroviral therapy in developing countries. Clin Infect Dis. 2007;45(8):1093–1101. | ||
Kyeyune R, Saathoff E, Ezeamama AE, Löscher T, Fawzi W, Guwatudde D. Prevalence and correlates of cytopenias in HIV-infected adults initiating highly active antiretroviral therapy in Uganda. BMC Infect Dis. 2014;14:496. | ||
Phe T, Thai S, Veng C, Sok S, Lynen L, van Griensven J. Risk factors of treatment-limiting anemia after substitution of zidovudine for stavudine in HIV-infected adult patients on antiretroviral treatment. PLoS One. 2013;8(3):e60206. | ||
WHO. Hemoglobin Concentration for the Diagnosis of Anemia and Assessment of Severity. Vitamin and Mineral Nutrition Information System. Geneva, Switzerland: World Health Organization; 2011 (WHO/NMH/NHD/MNM/11.1). |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.