Back to Journals » Risk Management and Healthcare Policy » Volume 15
Analysis of the Risk Factors Related to the Success Rate of Distal Transradial Artery Access in Patients with Coronary Heart Disease
Authors Li SS, Li JM, Liu LL, Liu W, Yang H, Feng CG
Received 10 January 2022
Accepted for publication 12 March 2022
Published 13 April 2022 Volume 2022:15 Pages 657—663
DOI https://doi.org/10.2147/RMHP.S357780
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Shan-Shan Li,1,* Jian-Ming Li,2,* Ling-Ling Liu,1 Wei Liu,1 Hao Yang,1 Chun-Guang Feng1
1Department of Cardiology, Xuzhou Central Hospital, Xuzhou, 221009, People’s Republic of China; 2Department of Cardiac Surgery, Xuzhou Central Hospital, Xuzhou, 221009, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chun-Guang Feng, Department of Cardiology, Xuzhou Central Hospital, Xuzhou, 221009, People’s Republic of China, Tel +86 18936376559, Email [email protected]
Objective: The aim of this study was to explore the factors influencing the success rate of distal transradial access (dTRA) for coronary intervention.
Methods: A total of 246 patients who underwent either coronary angiography or percutaneous coronary intervention in the Xuzhou Central Hospital were enrolled in this study. Access via the distal radial artery was the first choice for the procedure, and the success rate of this approach was recorded. All patients underwent color Doppler ultrasonography of the distal radial artery at the right anatomical snuff box in order to measure the artery diameter. The patients were divided into two groups depending on the success of the dTRA; 44 patients with unsuccessful punctures were assigned to the observation group and 202 patients with successful punctures acted as the control group. The basic clinical data of the two groups were recorded, and the differences between the two groups with respect to various indices were evaluated. Logistic regression analysis was carried out to explore the factors influencing the success rate of dTRA.
Results: Of the 246 patients, dTRA was achieved in 202, giving a puncture success rate of 82.11%. Logistic regression analysis showed that the success rate of dTRA was positively correlated with the diameter of the distal radial artery (odds ratio [OR] = 3.381, P = 0.005) and hypertension (OR = 2.427, P = 0.016), and negatively correlated with female gender (OR = 0.429, P = 0.036) and diabetes mellitus (OR = 0.325, P = 0.002).
Conclusion: The results of this study suggest that hypertension and distal radial artery diameter have a positive effect on the success rate of dTRA, while diabetes and female gender have a negative effect.
Keywords: distal radial artery, coronary angiography, color Doppler, inner diameter, puncture success rate, coronary atherosclerotic heart disease, regression analysis
Introduction
With continuous updating and development of coronary diagnosis and treatment technology, the latest European Society of Cardiology guidelines1 recommend the radial artery as the standard site of access for coronary angiography (CAG) and percutaneous coronary intervention (PCI). Compared with femoral artery access, transradial CAG and PCI have obvious advantages, including a significantly reduced incidence of bleeding complications, increased patient comfort, and even a reduction in mortality of patients with acute coronary syndrome.2 Nevertheless, transradial PCI is still associated with some complications, of which forearm radial artery occlusion (RAO) is the most common. Reports in the literature suggest that RAO has an incidence of 3–10%3 or may be as high as 30%.4 Distal transradial access (dTRA) is a new access approach for interventional therapy. The puncture point of dTRA is located at the wrist and, as this will not damage the radial artery in the forearm, its main advantage is a low potential risk of RAO.5 In recent years, the Department of Cardiology of the Xuzhou Central Hospital has carried out dTRA. However, worldwide, there are few studies on dTRA as a new approach for intervention. There are even fewer studies on the risk factors related to the success rate of dTRA. Therefore, the purpose of this study was to investigate the risk factors affecting the dTRA success rate.
Subjects and Methods
Subjects
A total of 246 patients who underwent CAG and/or PCI in the Department of Cardiology of the Xuzhou Central Hospital from May 2020 to February 2021 were enrolled randomly in this study; all patients were Asian. There were 181 males and 65 females, and the age range was 30–83 years old, with an average age of 62.66 ± 10.49 years old. The study was initially randomized to 263 subjects, of whom 17 were excluded or refused to participate in the study, and the attrition rate was 6.46%. This study was reviewed and approved by the ethics committee of the Xuzhou Central Hospital. All patients gave signed, informed consent prior to surgery. The success rate of dTRA and catheterization and the clinical data of patients were statistically analyzed.
Inclusion criteria were as follows: (1) patients with coronary heart disease who underwent CAG and PCI in the Xuzhou Central Hospital from May 2020 to February 2021, (2) the arterial pulse was palpable at the puncture site, (3) Allen’s test was positive prior to the procedure, (4) preoperative radial artery ultrasonography was negative.
Exclusion criteria were as follows: (1) the arterial pulse at the puncture site was weak or impalpable, (2) ultrasonography suggested severe calcification or arterial occlusion of the radial artery, (3) ultrasonography identified a radial artery malformation in the forearm, (4) patients with a history of coronary artery bypass graft or the loss of the radial artery at the puncture site as a “bridging vessel”, (5) prior transradial puncture, (6) patients with coagulation dysfunction or severe liver or kidney dysfunction, (7) patients who refused coronary intervention.
Methods
The diameter and area of the right distal radial artery in all patients were measured using a Philips color Doppler ultrasound machine (EPIQ 7C or IE33, Philips, the Netherlands). The measurements were performed by the same ultrasound physician. Procedures were carried out on all patients by the same group of interventional physicians. Patients laid in a supine position, with the upper limb on the operation side naturally straightened and extending outward, forming a 30°–45° angle with the body. The wrist was slightly padded to facilitate puncture, the skin from the palm to the elbow was routinely disinfected, and a sterile surgical towel was positioned. Local anesthesia was achieved using 1% lidocaine. The puncture point was reconfirmed and the Seldinger method was used to achieve access at the location with the strongest arterial pulse. A 20G puncture needle and a 0.025-inch guidewire were selected to place the 6F radial artery sheath (Terumo Company, Japan) following successful radial artery puncture. The 6F arterial sheath was selected according to the diameter of the blood vessel at the puncture site. An intrathecal injection of nitroglycerin was given in order to reduce radial artery spasm, and unfractionated heparin was given to prevent thrombosis. Coronary intervention was then completed via dTRA (Figure 1).
Observation Indices
The patients were divided into two groups depending on the success of the dTRA; 44 patients with unsuccessful punctures were assigned to the observation group and 202 patients with successful punctures acted as the control group. Basic clinical data from the two groups, such as gender, height, age, distal radial artery diameter, hypertension, diabetes, hyperlipidemia, and smoking history, were compared using the following settings: gender (male = 1, female = 2), history of hypertension (no = 0, yes = 1), history of diabetes mellitus (no = 0, yes = 1), history of hyperlipidemia (no = 0, yes = 1), and smoking history (no = 0, yes = 1). The differences in the various indicators between the two groups were then evaluated.
Statistical Methods
Data were analyzed using the SPSS 22.0 statistical software. Measurement data were expressed as the mean ± standard deviation (x ± SD), and those with homogeneous variance and in a normal distribution were analyzed using a one-way analysis of variance. Data with heterogeneity of variance or in a non-normal distribution were compared using the rank-sum test. Count data were compared using the χ2 test. Multivariate logistic regression analysis was conducted to determine the risk factors related to the success rate of dTRA. A P value of <0.05 was considered to be statistically significant.
Results
Characteristics of the dTRA Success Rate and Overall Distal Radial Artery Diameter
Of the 246 patients, dTRA was achieved in 202, giving a puncture success rate of 82.11%. The mean internal diameter of the distal radial artery in all patients was 2.05 ± 0.41 mm, and this was normally distributed overall (Figure 2). The mean internal diameter of the distal radial artery in female and male patients was 1.92 ± 0.37 mm and 2.09 ± 0.42 mm, respectively, and the difference between these values was statistically significant (t = 2.92, P = 0.004). The incidence of distal RAO following the procedure was 5.3% (13 patients).
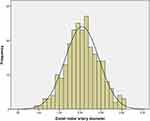 |
Figure 2 Distribution of the diameter of the distal radial artery is shown. |
Comparison of General Data Between the Two Groups
The patients were divided into two groups depending on the success of the punctures, and there were significant differences between the two groups in respect of gender, distal radial artery diameter, hypertension, and diabetes (P < 0.05 for all). However, there were no significant differences between the two groups in respect of age, height, weight, body mass index, hyperlipidemia, and smoking history (P > 0.05 for all).
Logistic Regression Analysis of Factors Related to the dTRA Success Rate
Logistic regression analysis was carried out using those factors for which there was a significant statistical difference between the two groups (gender, hypertension, diabetes, and distal radial artery diameter) as independent variables and the success rate of dTRA as the dependent variable. The results identified that the success rate of dTRA was positively correlated with the diameter of the distal radial artery, and hypertension was negatively correlated with diabetes and female gender (Table 1).
 |
Table 1 Comparison of General Clinical Data Between Two Groups of Patients and Results of Multivariate Logistic Regression Analysis |
Discussion
Transradial access6 has a number of advantages; bed rest is not required, and it is associated with fewer postoperative bleeding complications as compared with femoral artery access. For these reasons, radial artery access is gradually replacing femoral artery access and is becoming the first choice for coronary intervention. However, access via the radial artery is not without disadvantages. Multiple radial artery interventions are prone to RAO complications, the radial artery is prone to spasm leading to puncture failure, and improper compression following radial artery puncture may lead to hematoma complications that may have serious consequences. In recent years, a foreign study has determined that coronary intervention via dTRA is safe and effective and can avoid the complications of radial artery injury.7
The distal radial artery puncture point is located in the anatomical snuff box on the radial side of the wrist. Therefore, dTRA is also called the “trans-snuff box access”. The location of this site is easy to identify. When the thumb is fully extended, there is a concave area in the triangle formed by the extensor pollicis longus tendon, the extensor pollicis brevis tendon, and the radial styloid process, known as the anatomical snuff box area.8 The success rate of puncture through the radial artery distally is significantly lower than that through the radial artery more proximally. The main reason for this increase in failure rate is the smaller diameter of the radial artery in the anatomical snuff box area. A previous study showed that the average diameter of the radial artery in the anatomical snuff box area was only 2.0–2.6 mm.9 In this study, the mean internal diameter of the distal radial artery in all patients was 2.05 ± 0.41 mm. In females, the distal radial artery diameter is smaller than in males,10 and in this study, the mean internal diameter of the distal radial artery in female patients was 1.92 ± 0.37 mm; this may affect the puncture success rate to a certain extent.
There are also some problems and controversies surrounding the use of dTRA in coronary intervention. To date, relevant studies have reported a dTRA success rate of 70–100% when carried out by experienced operators. In addition, the results of one study also identified a distal radial artery puncture failure rate of up to 30%.11 In this study, the success rate of dTRA was 82.11%, and this was consistent with the results of most studies. This suggests that as a new interventional access approach, even operators with dTRA experience still need to progress along a learning curve in order to master it successfully. A previous study12 analyzed the main causes of dTRA failure and identified the following three issues: (1) The diameter of the distal radial artery is small, the puncture itself is difficult, or the sheath tube insertion following successful puncture is difficult; (2) Distortion of the distal radial artery exists extensively, resulting in poor insertion of the guidewire and sheath tube; (3) PCI via the distal radial artery is a new technology in recent years and most operators do not have sufficient relevant puncture experience.
The results of a study revealed that the diameter and structure of the distal radial artery can vary greatly. Therefore, it is difficult to predict the actual diameter of the artery. In order to ensure the safety of the procedure and to reduce the risk of RAO, it is recommended that all patients undergo preoperative ultrasonography to determine the diameter of the distal radial artery and select an appropriate radial artery sheath.13 This study showed that the success rate of dTRA was positively correlated with the diameter of the distal radial artery; the larger the diameter, the higher the puncture success rate. Therefore, to improve the success rate of dTRA, the diameter of the distal radial artery should be evaluated by ultrasonography prior to the procedure, and dTRA should not be recommended for patients with a small distal radial artery diameter.
The diameter of the distal radial artery directly affects the dTRA success rate. However, there are few studies at home and abroad on the factors affecting the diameter of the distal radial artery. A study conducted by Snehil et al on the influence of radial artery diameter in South Asians revealed that both height and wrist circumference were strong independent predictors of radial artery diameter. The presence of hypertension and male gender were also found to be important parameters affecting radial artery diameter.14 One study showed that a low body mass index (BMI) and a low body surface area were significant predictors of a DRA diameter <2.3 mm.15 BMI was significantly correlated with DRA diameter (r = 0.66, P < 0.0001) in a Japanese study of 142 patients.16 However, another Japanese study did not report an association between vessel diameter and clinical variables, including BMI, in multivariate analysis.9 In this study, there was no statistical difference in BMI between the successful and unsuccessful puncture groups.
This study revealed that the success rate of dTRA was positively correlated with hypertension, and analysis suggests that a long-term, chronic increase in blood pressure leads to a compensatory increase in the internal diameter of the distal radial artery, as in hypertensive heart disease. In patients with hypertension, the elastic fibers bearing the pressure load on the arterial wall gradually transform into non-elastic fibers and lose elasticity, resulting in decreased arterial compliance and increased vascular diameter. Additionally, because of the strong pulse of the distal radial artery in patients with hypertension, the operator has a better puncture feeling, resulting in an increase in the success rate of dTRA. The study conducted by Khder et al also demonstrated that the radial artery diameter of patients with hypertension was greater when compared with that of patients in a normal blood pressure control group.17
The results of this study also revealed that the success rate of dTRA was negatively correlated with diabetes mellitus and female gender. The main reasons for this are as follows: (1) Patients with diabetes mellitus have atherosclerosis, middle layer calcification of the arterial wall, and hyperplasia of intimal fibers, resulting in narrowing of the lumen; (2) With the development of diabetes, the diameter of the distal radial artery tends to decrease, resulting in a decrease in the success rate of dTRA. A foreign study18 also confirmed that diabetes was a factor predicting intimal hyperplasia and arteriosclerosis of the radial artery. Diabetes mellitus has a negative impact on radial artery size. In general, the diameter of the distal radial artery in female patients is significantly smaller than that in males.10 Therefore, the success rate of dTRA in females is often lower.
This study had a number of limitations. First, this was a single-center study with a limited number of cases, and there may have been bias in the data collection. Second, neither the grade of hypertension nor the control of blood pressure was taken into consideration. Finally, neither the duration of diabetes nor the control of blood glucose was taken into consideration. The duration of diabetes is difficult to ascertain accurately as most patients are initially asymptomatic with the diagnosis of diabetes being made, incidentally.
Conclusion
This study identified that the success rate of dTRA was positively correlated with the diameter of the distal radial artery and hypertension, and it was negatively correlated with diabetes and female gender. The significance is that the distal radial artery approach is not recommended for patients whose distal radial artery is found to be too small upon ultrasound examination, especially women with diabetes. The aim is to avoid injury caused by puncture failure and improve patient comfort. In the future, multicenter research with an expanded sample size is necessary. More clinical studies are needed in order to determine other factors that may affect the success rate of dTRA, and also to provide more theoretical evidence for the clinical popularization of this approach.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Xuzhou Central Hospital. Written informed consent was obtained from all participants.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014;46(4):517–592. doi:10.1093/ejcts/ezu366
2. Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial [published correction appears in Lancet. 2011 Apr 23; 377(9775):1408][published correction appears in Lancet. 2011 Jul 2;378(9785):30]. Lancet. 2011;377(9775):1409–1420. doi:10.1016/S0140-6736(11)60404-2
3. Aldoori JS, Mohammed AI. Transradial approach for coronary angiography and percutaneous coronary intervention: personal experience. Egypt Heart J. 2019;71(1):10. doi:10.1186/s43044-019-0006-2
4. Uhlemann M, Möbius-Winkler S, Mende M, et al. The Leipzig prospective vascular ultrasound registry in radial artery catheterization: impact of sheath size on vascular complications. JACC Cardiovasc Interv. 2012;5(1):36–43. doi:10.1016/j.jcin.2011.08.011
5. Hadjivassiliou A, Cardarelli-Leite L, Jalal S, et al. Left distal transradial access (ldTRA): a comparative assessment of conventional and distal radial artery size. Cardiovasc Intervent Radiol. 2020;43(6):850–857. doi:10.1007/s00270-020-02485-7
6. Valgimigli M, Gagnor A, Calabró P, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. 2015;385(9986):2465–2476. doi:10.1016/S0140-6736(15)60292-6
7. Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention. 2017;13(7):851–857. doi:10.4244/EIJ-D-17-00079
8. Rasul AM, Kumar SC, Krisna BS, et al. Comparison of distal transradial in the anatomical snuffbox versus conventional transradial access for coronary angiography and intervention-an experience in 100 cases. Univ Heart J. 2018;13(2):40. doi:10.3329/uhj.v13i2.37657
9. Naito T, Sawaoka T, Sasaki K, et al. Evaluation of the diameter of the distal radial artery at the anatomical snuff box using ultrasound in Japanese patients. Cardiovasc Interv Ther. 2019;34(4):312–316. doi:10.1007/s12928-018-00567-5
10. Kim Y, Ahn Y, Kim MC, et al. Gender differences in the distal radial artery diameter for the snuffbox approach. Cardiol J. 2018;25(5):639–641. doi:10.5603/CJ.2018.0128
11. Koutouzis M, Kontopodis E, Tassopoulos A, et al. Distal versus traditional radial approach for coronary angiography. Cardiovasc Revasc Med. 2019;20(8):678–680. doi:10.1016/j.carrev.2018.09.018
12. Li F, Xiao JQ, Cai GJ. Recent developments in percutaneous coronary intervention via distal radial artery access. Chin Gen Pract. 2021;24(06):
13. Costa F, van Leeuwen MA, Daemen J, et al. The Rotterdam radial access research: ultrasound-based radial artery evaluation for diagnostic and therapeutic coronary procedures. Circ Cardiovasc Interv. 2016;9(2):e003129. doi:10.1161/CIRCINTERVENTIONS.115.003129
14. Goswami S, Bhattacharyya D, Kar A. TCTAP A-139 factors influencing radial artery diameter in South Asians: single centre observational study. J Am Coll Cardiol. 2019;73(15):S73–S74. doi:10.1016/j.jacc.2019.03.453
15. Lee JW, Son JW, Go TH, et al. Reference diameter and characteristics of the distal radial artery based on ultrasonographic assessment. Korean J Intern Med. 2022;37(1):109–118. doi:10.3904/kjim.2020.685
16. Norimatsu K, Kusumoto T, Yoshimoto K, et al. Importance of measurement of the diameter of the distal radial artery in a distal radial approach from the anatomical snuffbox before coronary catheterization. Heart Vessels. 2019;34(10):1615–1620. doi:10.1007/s00380-019-01404-2
17. Khder Y, Bray-Desboscs L, Aliot E, Zannad F. Effects of blood pressure control on radial artery diameter and compliance in hypertensive patients. Am J Hypertens. 1997;10(3):269–274. doi:10.1016/S0895-7061(96)00347-0
18. Loh YJ, Nakao M, Tan WD, Lim CH, Tan YS, Chua YL. Factors influencing radial artery size. Asian Cardiovasc Thorac Ann. 2007;15(4):324–326. doi:10.1177/021849230701500412
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

