Back to Journals » International Journal of Women's Health » Volume 14
Analysis of the Risk Factors for Massive Hemorrhage in Pernicious Placenta Previa and Evaluation of the Efficacy of Internal Iliac Artery Balloon Occlusion
Authors Zhang LL, Wang WH, Hou YL
Received 24 June 2022
Accepted for publication 4 November 2022
Published 21 December 2022 Volume 2022:14 Pages 1769—1776
DOI https://doi.org/10.2147/IJWH.S379965
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Li-Li Zhang,* Wen-Hao Wang,* Yong-Li Hou
Department of Obstetrics and Gynecology, The Second Hospital of Shanxi Medical University, Taiyuan, 030000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yong-Li Hou, Department of Obstetrics and Gynecology, The Second Hospital of Shanxi Medical University, No. 382 of Wuyi Road, Xinghualing District, Taiyuan, 030000, People’s Republic of China, Tel +86 03513382151, Email [email protected]
Objective: To investigate the risk factors of intraoperative massive hemorrhage in patients with pernicious placenta previa (PPP) and analyze the value of bilateral internal iliac artery balloon occlusion in Cesarean section for these patients.
Methods: The clinical data of 134 patients with PPP admitted to the Second Hospital of Shanxi Medical University from January 2012 to January 2019 were analyzed. A logistic regression analysis was used to analyze the risk factors for intraoperative massive hemorrhage in PPP. The study subjects were divided into the intervention group (38 cases) and the routine group (96 cases) according to whether bilateral internal iliac artery balloon occlusion was conducted during the operation. The differences in some clinical indicators were compared between the two groups.
Results: The risk factors for intraoperative massive hemorrhage in PPP were age ≥ 35 years, gestational age ≥ 34 weeks, complete placenta previa, and the presence of placenta accreta. The differences in the operation time, postoperative transfer to the intensive care unit, postoperative length of the hospital stay, and neonatal weight and score were not statistically significant between the intervention group and the routine group (P > 0.05 for all). While the intraoperative blood loss and the transfusion volume in the intervention group were lower than in the routine group, the hospitalization cost was higher in the former than in the latter, and the differences were statistically significant (P < 0.05 for all). Moreover, there was no case of hysterectomy in the intervention group, while there were two cases of hysterectomies in the routine group.
Conclusion: The risk factors for intraoperative massive hemorrhage in PPP were age ≥ 35 years, gestational age ≥ 34 weeks, complete placenta previa, and the presence of placenta accreta. Internal iliac artery balloon occlusion during PPP could reduce intraoperative blood loss and the hysterectomy rate.
Keywords: pernicious placenta previa, internal iliac artery balloon occlusion, intraoperative bleeding, risk factor
Introduction
Pernicious placenta previa (PPP) is a serious long-term complication after a Cesarean section. It may cause fatal perioperative hemorrhage and, in severe cases, hysterectomy, resulting in the loss of fertility in young patients and even endangering maternal and neonatal lives. After an initial Cesarean section, the structural changes of the uterine scar tissue result in metaplasia and dysplasia in the uterus; the placental villi may implant easily into the muscular and serosal layers of the uterus and lead to the formation of PPP, which is characterized by high risk, high incidence, and high mortality.1–3 According to clinical data, PP may be diagnosed with an average blood loss before or during delivery of 4500 mL, and PPP may be diagnosed with an average blood loss of 7800 mL.4,5 Therefore, it may be concluded that fatal perinatal massive hemorrhage is the most serious complication of PPP since it may easily lead to disseminated intravascular coagulation, hemorrhagic shock, and multiple organ failure, which are life-threatening conditions. Hysterectomy is sometimes necessary, which causes great harm to patients’ physical and mental health.6,7 In recent years, with the introduction of the second-child policy in China, the Cesarean section rate has been increasing, resulting in a significant rise in the number of patients with PPP and more challenges for obstetricians. Therefore, it is of great significance to explore the risk factors for intraoperative massive hemorrhage in PPP, to carry out reasonable intervention for the population with high-risk factors, reduce the hysterectomy rate in those with PPP, and improve patients’ physical and mental health. In the present study, the clinical data of 134 patients with PPP admitted to the Second Hospital of Shanxi Medical University from January 2012 to January 2019 were analyzed retrospectively to investigate the risk factors leading to intraoperative massive hemorrhage and the efficacy of the intraoperative application of internal iliac artery balloon occlusion to guide clinical practice.
Materials and Methods
Study Subjects
The clinical data of 134 patients with PPP admitted to the Second Hospital of Shanxi Medical University from January 2012 to January 2019 were analyzed retrospectively. The patients were aged between 22 and 44 years, with a gestational age of ≥28 weeks. All patients underwent a Cesarean section for the termination of pregnancy. The study subjects were divided into the intervention group (38 patients) and the routine group (96 patients) depending on the intraoperative application of bilateral internal iliac artery balloon occlusion. The Cesarean sections were conducted by a senior associate or chief physician. The study was approved by the ethics committee of the hospital, and the patients and their families gave informed consent.
The inclusion criteria were as follows: (1) patients with a history of Cesarean section, (2) patients with placenta previa (PP) and placenta attached to the incision of a previous Cesarean section (according to the 8th edition of the undergraduate textbook of obstetrics and gynecology published by the People’s Health Publishing House), and (3) patients with complete general information.
The diagnostic criteria were as follows: placenta previa and the placenta type were diagnosed by the last findings of ultrasonography or magnetic resonance imaging before the termination of pregnancy or by postpartum examination of the relationship between the placental margin and the fetal membrane rupture, which were confirmed by intrauterine examination of the placental position during Cesarean section. Placenta accreta was diagnosed by the intraoperative findings during Cesarean section, and the pathological diagnosis of the placenta was sent for postoperative examination.
The exclusion criteria were as follows: (1) patients with twin or multifetal pregnancies, (2) patients with uterine fibroids or malformations, (3) patients with abnormal coagulation function, (4) patients with induced labor, and (5) patients with incomplete general information.
Study Methods
The 134 patients with PPP who were delivered surgically in the hospital were grouped according to the surgical approaches involved. In the intervention group, 38 patients were delivered by Cesarean section with bilateral internal iliac artery balloon occlusion. For the 96 cases in the routine group, since the patients or their families refused to undergo internal iliac artery balloon occlusion, the surgical procedures were performed according to the procedures for a conventional Cesarean section, and other methods and treatments were used for hemostasis according to the actual intraoperative condition.
Surgery in the Intervention Group
Before the operation, the right and left inguinal areas of the patient were routinely disinfected and toweled in the intervention room of the radiology department, and local anesthesia was applied with 2% lidocaine guided by digital subtraction angiography. The bilateral femoral arteries were punctured with the aid of the Seldinger technique together with the placement of a 5F vascular sheath. A 5F-Cobra catheter and 0.035-inch guide balloon were introduced through the vascular sheath into the bilateral internal iliac arteries, and the balloon catheter was implanted in the bilateral uterine artery orifice of the internal iliac artery. During the operation, approximately 2 mL of iohexol diluent was injected to temporarily fill the internal iliac artery balloon. If the blood flow of the internal iliac artery was blocked with the manual injection of the contrast agent, the contrast stagnated distal to the internal iliac artery; in this case, the contrast was withdrawn, and the artery with the balloon was kept unobstructed. With the catheter fixed, the patient was transferred into the operating room. After the fetus was delivered and the umbilical cord was cut, the bilateral balloons were filled to block the blood flow of the bilateral internal iliac arteries during the follow-up surgical procedures. The balloon was released at an interval of 30–40 min during the operation to restore the blood flow of the bilateral internal iliac arteries and to prevent ischemia and necrosis of the distal tissue. The balloon and catheter were extracted after surgery.
Surgery in the Routine Group
The surgery was conducted according to conventional Cesarean section procedures. Based on the conditions of intraoperative hemorrhage and placenta accreta, figure-of-8 sutures, B-Lynch sutures, Cook® hemostatic balloons, intrauterine gauze tamponades, partial myometrial excisions, etc., were applied for hemostasis. For those with severe uncontrollable hemorrhage, an emergency hysterectomy was performed.
Observation Indicators
The patients’ general information included (1) age, (2) gestational week, (3) number of pregnancies, (4) number of deliveries, (5) number of abortions, and (6) number of Cesarean deliveries.
The intraoperative observation indicators were (1) operation time, (2) volume of intraoperative hemorrhage (as assessed by the anesthesiologist and the attending surgeon based on the amount and extent of the soaked gauze, the volume of blood drawn by negative pressure suction, and the changes in hemoglobin levels), (3) intraoperative blood transfusion volume, (4) hysterectomy rate, (5) placenta type, (6) presence of placental adhesions, and (7) the presence of placenta accreta.
The postoperative observation indicators were (1) postoperative length of the hospital stay and (2) hospitalization cost.
The observation indicators in the neonates were (1) neonatal Apgar score and (2) neonatal weight.
Statistical Methods
The study used SPSS™ Statistics v20.0 software for statistical processing. The measurement data that satisfied the normal distribution were expressed as mean ± standard deviation, and a t-test was used for intergroup comparison. Countable data were expressed by percentages and tested by the X2 test or Fisher’s exact probability method. A logistic regression analysis was used for the analysis of the risk factors for massive hemorrhage. A value of P < 0. 05 was considered statistically significant.
Results
Analysis of the Risk Factors of Intraoperative Massive Hemorrhage
Results of the Univariate Analysis
The variables with significance included age, gestational week, presence of placental adhesions, and presence of placenta accreta (Table 1). The variables without significance included the number of pregnancies, number of deliveries, number of abortions, and number of Cesarean deliveries.
 |
Table 1 Univariate Analysis of the Risk Factors of Intraoperative Massive Hemorrhage |
Results of the Multivariate Analysis
The above significant variables were introduced into a multivariate analysis, and the results showed that the risk of intraoperative massive hemorrhage in patients with PPP aged ≥35 years was 2.876 times greater than in those aged <35 years (P = 0.019). The risk of intraoperative massive hemorrhage in patients with PPP with a gestational age ≥34 weeks was 4.756 times greater than in those with a gestational age of <34 weeks (P = 0.010). The risk of intraoperative massive hemorrhage in patients with PPP and placenta accreta was 5.607 times greater than in those without placenta accreta (P = 0.016). Additionally, the risk of intraoperative massive hemorrhage in complete PP was 4.591 times that of incomplete PP (P = 0.001). Therefore, it was suggested that age ≥35 years, gestational age ≥34 weeks, placenta accreta, and complete PP were the risk factors for intraoperative massive hemorrhage in PPP (Table 2).
 |
Table 2 Multivariate Analysis of the Risk Factors of Intraoperative Massive Hemorrhage |
Evaluation of the Therapeutic Effects of Bilateral Internal Iliac Artery Balloon Occlusion During Cesarean Section
Comparison of the General Characteristics Between the Two Groups of Patients
The differences in age, number of Cesarean sections, number of pregnancies, number of deliveries, number of abortions, and gestational age at delivery were not statistically significant between the intervention group and the routine group (P > 0.05 for all). Concerning the placenta type, it was revealed that the risk of the application of a bilateral internal iliac artery balloon occlusion increased significantly in those with complete PP, and the difference between the two groups was statistically significant (P < 0.05) (Table 3).
 |
Table 3 Comparison of the General Characteristics Between the Two Groups of Patients |
Comparison of the Intraoperative Indicators Between the Two Groups of Patients
The intraoperative blood loss and transfusion volume in the intervention group were lower than those in the routine group, but the hospitalization cost was higher in the intervention group than in the routine group. The differences were statistically significant between the two groups (P < 0.05 for all). The differences in the operation time, the postoperative transfer to the intensive care unit (ICU), and the postoperative length of the hospital stay were not statistically significant between the two groups (P > 0.05 for all) (Table 4). There was no case with hysterectomy in the intervention group, while two cases had hysterectomies in the routine group.
 |
Table 4 Comparison of Intraoperative Conditions Between the Two Groups |
Comparison of the Neonatal Outcomes Between the Two Groups of Patients
There were no maternal or neonatal deaths in either group. The differences in neonatal weight and neonatal score were not statistically significant between the intervention group and the routine group (P > 0.05 in both) (Table 5).
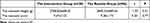 |
Table 5 Comparison of Neonatal Outcomes After Operation |
Discussion
The Analysis of the Risk Factors for Intraoperative Massive Hemorrhage in Pernicious Placenta Previa
In clinical practice, PPP is a very high-risk pregnancy and a complication of re-pregnancy after a cesarean section. If we can found the risk factors of intraoperative massive hemorrhage in PPP, it will reduce the hysterectomy rate in patients with PPP.
For this purpose, univariate and multivariate logistic analyses were conducted in the present study, and it was found that age ≥35 years, gestational age ≥34 weeks, a complete PP placenta type, and the presence of placenta accreta were the risk factors for intraoperative massive hemorrhage.
Clinically, pregnant women over the age of 35 with advanced maternal age are defined as puerperae. This is because, with increasing age, puerperae of advanced maternal age are prone to developing serious comorbidities and complications during pregnancy, delivery, and postpartum. The results of the present study suggest that age ≥35 years is a risk factor for intraoperative massive hemorrhage during cesarean section. The reason might be due to the decline in the physical quality of puerperae of advanced maternal age in whom the uterine muscle fiber tension might be weaker than that of younger women; they might be prone to uterine atony, resulting in poor closure of the blood sinuses on the uterine wall and eventually, massive hemorrhage.8–11 Moreover, puerperae of advanced maternal age will have increased collagen content and decreased placental blood supply, which will increase the area of the placenta and the probability of PPP.12 Therefore, in puerperae of advanced maternal age with PPP, intraoperative massive hemorrhage is more likely to occur.
The repair of scar uterine tissue after Cesarean section will manifest mainly as the fibrous scar of connective tissue, with a small amount of smooth muscle involved.13,14 In the case of re-pregnancy, the scar tissue will bear the high tension of pregnancy for a long time, and the thickness of the upper and lower uterine walls will be different. With the increase in gestational age, this difference becomes more prominent, and the lower uterine segment is more prone to develop edema, which leads to the occurrence of uterine atony, incision rupture, and uterine rupture, making a massive hemorrhage more likely.13 This might be the reason for the findings that those with PPP with a gestational age of ≥34 weeks were more prone to develop massive intraoperative hemorrhage in the present study.
In addition, it was suggested in the present study that the risk of intraoperative massive hemorrhage in complete PP was 4.591 times that of patients with incomplete PP (P = 0.001). The reason might be because the area of complete PP attached to the lower uterine segment was larger than that of partial or marginal PP and was more difficult to avoid during the operation, resulting in a significant increase in the degree of hemorrhage. Moreover, with the delivery of the fetus, the muscle tissue of the lower segment of the uterus becomes thin, with poor contractility. With the stripping of the attached placenta, the opened blood sinus is not easily closed, and uncontrollable hemorrhage is more likely to develop.
Placenta accreta is the main cause of serious complications, such as hemorrhage and shock in patients with PPP. The present study also revealed that the risk of intraoperative massive hemorrhage in patients with PPP and placenta accreta was 5.607 times greater than in those without placenta accreta (P = 0.016). This might be because it was difficult to strip the placenta accreta, which would affect uterine contraction. With the stripping of the placenta, the opened blood sinuses on the placenta attachment surface failed to close, resulting in severe intraoperative hemorrhage.15
The Analysis of the Therapeutic Effects of Bilateral Internal Iliac Artery Balloon Occlusion During Cesarean Section in Pernicious Placenta Previa
At present, the pre-positioning of balloon catheters in the bilateral internal iliac arteries for blood flow occlusion by interventional means is a common domestic and international trend for solving this problem.16 The therapeutic effect of bilateral internal iliac artery balloon occlusion and conventional surgery were compared between the two groups in the present study. The results suggested that the differences in the volume of intraoperative blood loss and blood transfusion were statistically significant between the two groups (P < 0.05 in both). The conclusions of the present study were consistent with the results of the study reported by Tan et al.17 Both studies confirmed that internal iliac artery balloon occlusion was more effective than conventional Cesarean section in controlling hemorrhage and significantly reduced the volume of intraoperative blood loss.
There was no case of hysterectomy in the intervention group, while two cases had hysterectomies in the routine group. The differences in the operation time, postoperative transfer to the ICU, and postoperative length of the hospital stay were not statistically significant between the two groups. A study by Panici et al18 involving 33 patients with PP and placenta accreta showed that the hysterectomy rate, postoperative length of the hospital stay, and rate of transfer to the ICU in those with internal iliac artery balloon occlusion were lower than those without it, and the differences were statistically significant (P < 0.05 for all). The above discrepancies might be related to the insufficient sample size in the present study, and it will be necessary to accumulate more cases and expand the sample size in further investigations.
In addition, there were no maternal or neonatal deaths in either group in the present study, and the differences in neonatal weight and neonatal score were not statistically significant between the two groups (P > 0.05 in both). The above results suggested that bilateral internal iliac artery catheterization had no adverse effect on neonates and might reduce the incidence of neonatal asphyxia. However, the number of cases in the present study was small, and it needs to be confirmed by a larger sample size.
Therefore, the intraoperative application of bilateral internal iliac artery balloon occlusion was more satisfactory than the conventional operation procedures in hemorrhage control. Surgical experience shows that when the bilateral internal iliac artery balloons were filled with the delivery of the placenta, the hemorrhage on the uteroplacental dissection surface was significantly reduced. However, when faced with severe and extensive placenta accreta, the role of the balloon was limited, hysterectomy should be considered for hemostasis.
Conclusions
In summary, during the process of Cesarean section in patients with PPP, the occurrence of intraoperative hemorrhage might be caused by various factors. Obstetricians should pay attention to the abovementioned high-risk factors, and prevention and treatment should be implemented accordingly. It was recommended to conduct bilateral internal iliac artery balloon implantation. However, the option for Hysterectomy is there to chose according to the operator assessment. In the event of rapid and massive hemorrhage during the operation, a hysterectomy should be performed immediately. The management of high-risk pregnant women should be strengthened to improve their safety during delivery.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki(as was revised in 2013). The study was approved by Ethics Committee of the Second Hospital of Shanxi Medical University. Written informed consent was obtained from all participants.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was supported by the Scientific research project of Health Commission of Shanxi Province (No.2019047).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Cui R, Li M, Lu J, Bai H, Zhang Z. Management strategies for patients with placenta accreta spectrum disorders who underwent pregnancy termination in the second trimester: a retrospective study. BMC Pregnancy Childbirth. 2018;18(1):298. doi:10.1186/s12884-018-1935-6
2. Zhang HX, Zhao YY, Wang YQ. Analysis of the Characteristics of Pregnancy and Delivery before and after Implementation of the Two-child Policy. Chin Med J. 2018;131(1):37–42. doi:10.4103/0366-6999.221268
3. Zuo Q, Liu H, Huang SH. Clinical analysis of 107 cases of dangerous placenta previa. Prog Obstet Gynecol. 2015;34(8):605–608. Chinese.
4. Zhou Y, Wang Y, Li JN, et al. Evaluation of hemostatic effect of cervix internal orifice lower uterine segment compression suture in the operation of dangerous placenta previa with placenta accreta. J Practical Obstet Gynaecol. 2017;33(1):69–71. Chinese.
5. Liu HY, Lin XG, Wu JL, et al. Multiposition spiral suture of the lower uterine segment: a new technique to control the intraoperative bleeding of pernicious placenta previa. Chin J Obstetrics Gynecol. 2016;51(10):754–758. Chinese.
6. Zeng H, Wang Y, Wang Y, et al. Perioperative management of abdominal aortic balloon implantation for penetrating placenta accreta: a case report. J Peking Univ. 2015;47(6):1031–1033. Chinese.
7. Benrashid E, McCoy CC, Rice HE, Shortell CK, Cox MW. Mycotic saccular abdominal aortic aneurysm in an infant after cardiac catheterization: a case report. Ann Vasc Surg. 2015;29(7):1447.e5–1447.e11. doi:10.1016/j.avsg.2015.06.061
8. Pan CS. Study on Influencing Factors of bleeding during cesarean section in elderly pregnant women. Electronic J Gynaecol Endocrinol. 2017;4(24):116–119. Chinese.
9. Shazly SA, Hortu I, Shih JC, et al. Prediction of clinical outcomes in women with placenta accreta spectrum using machine learning models: an international multicenter study. J Matern Fetal Neonatal Med. 2021;7:1–10. PMID: 34233555. doi:10.1080/14767058.2021.1918670
10. Shazly SA, Hortu I, Shih JC, et al. Prediction of success of uterus-preserving management in women with placenta accreta spectrum (CON-PAS score): a multicenter international study. Int J Gynaecol Obstet. 2021;154(2):304–311. PMID: 33278833. doi:10.1002/ijgo.13518
11. Cırpan T, Akdemir A, Okmen F, Hortu I, Ekici H, Imamoglu M. Effectiveness of segmental resection technique in the treatment of placenta accreta spectrum. J Matern Fetal Neonatal Med. 2021;34(19):3227–3233. PMID: 31830832. doi:10.1080/14767058.2019.1702019
12. Li JJ. Analysis of risk factors of placenta previa and pregnancy outcome. Guide Chin Med. 2016;14(21):9–10. Chinese.
13. Watanabe T, Matsubara S. No bleeding before, more bleeding later: the relationship between the presence of warning bleeding and the amount of bleeding during caesarean section in placenta praevia. J Obstet Gynaecol. 2010;30(8):836. doi:10.3109/01443615.2010.509827
14. Mimura T, Hasegawa J, Nakamura M, et al. Correlation between the cervical length and the amount of bleeding during cesarean section in placenta previa. J Obstet Gynaecol Res. 2011;37(7):830–835. doi:10.1111/j.1447-0756.2010.01446.x
15. Liang F, Liu EL, Guan X, et al. Clinical analysis of 91 cases of pernicious placenta previa and exploration of risk factors of hysterectomy. J North Chin Univ Sci Technol. 2019;21(2):122–126. Chinese.
16. Lin L, Yang Y, Li Q. Clinical analysis of abdominal aorta pre balloon occlusion during cesarean section in the treatment of dangerous placenta previa. Matern Child Health Care Chin. 2015;30(19):3168–3171. Chinese.
17. Tan CH, Tay KH, Sheah K, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. AJR Am J Roentgenol. 2007;189(5):1158–1163. doi:10.2214/AJR.07.2417
18. Panici PB, Anceschi M, Borgia ML, et al. Intraoperative aorta balloon occlusion: fertility preservation in patients with placenta previa accreta/increta. J Matern Fetal Neonatal Med. 2012;25(12):2512–2516. doi:10.3109/14767058.2012.712566
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
