Back to Journals » International Journal of General Medicine » Volume 15
Analysis of Risk Factors and the Establishment of a Predictive Model for Thrombosis in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis
Authors Zhang Z , Huang W, Ren F, Luo L, Zhou J, Tian M, Wang Z, Chen D, Tang L
Received 2 August 2022
Accepted for publication 10 October 2022
Published 7 November 2022 Volume 2022:15 Pages 8071—8079
DOI https://doi.org/10.2147/IJGM.S384624
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zhihuan Zhang, Wenhan Huang, Feifeng Ren, Lei Luo, Jun Zhou, Mengxue Tian, Zhongjie Wang, Dandan Chen, Lin Tang
Department of Rheumatology and Immunology, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China
Correspondence: Lin Tang, Department of Rheumatology and Immunology of the Second Affiliated Hospital of Chongqing Medical University, Chongqing, 400010, People’s Republic of China, Email [email protected]
Purpose: To explore the risk factors for thrombi occurring in patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV) and establish a risk prediction model to better predict the risk of thrombosis in patients with AAV.
Patients and Methods: We retrospectively analyzed 117 AAV patients who had been hospitalized in The Second Affiliated Hospital of Chongqing Medical University between October 2010 and December 2021. For all patients, we recorded demographic characteristics and clinical data, analyzed the risk factors for thrombosis in AAV patients and then developed a risk prediction model.
Results: Stepwise logistic regression analysis indicated that a high complement C3 level, a high BVAS score and a high Padua score were independent risk factors for thrombosis in AAV patients. According to multivariate analysis, a predictive model for thrombus risk was successfully established; the area under the ROC curve(AUC) was 0.803 (95% CI: 0.716– 0.890) and the maximum Youden index, sensitivity and specificity were 0.487, 59.0% and 89.7%, respectively.
Conclusion: A high complement C3 level, high BVAS score, and a high Padua score were shown to be independent risk factors for thrombosis in AAV patients. We developed a risk prediction model based on these three risk factors that could predict the risk of thrombosis in AAV patients to some extent.
Keywords: antineutrophil cytoplasmic antibody, thromboembolism, risk factors, risk prediction model
Introduction
Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) mainly includes microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) and eosinophilic granulomatosis with polyangiitis (EGPA) and is a group of autoimmune diseases involving multiple systems throughout the body. The survival rate of AAV patients has been significantly improved due to the use of glucocorticoids, immunosuppressors and CD20 monoclonal antibody over the last few decades. As awareness of this disease has increased, there has been increasing concern over the thromboembolic events that can occur with AAV. These thromboembolic events increase the difficulty of treating the disease and can affect the prognosis.
A number of studies have shown that the risk of arteriovenous thrombosis occurring in patients with AAV is clearly increased,1–3 although the pathogenic mechanisms involved are not clear. Such mechanisms may involve neutrophil extracellular traps (NETs), injury incurred by endothelial cells, the initiation of a coagulation cascade, the defect of fibrinolytic activity and the use of glucocorticoids.4–6 Moreover, existing research conclusions relating to the risk factors for the thromboembolic events that occur in patients with AAV are inconsistent, the predictive values for whether thromboembolism will occur in patients during the course of disease are limited, and there is no clinical guideline relating to autoimmune disease and thrombi at present.
In this study, we retrospectively analyzed potential risk factors for thromboembolism in AAV patients and developed a new risk prediction model to identify high-risk patients in the early stages of disease so that we could take targeted preventive measures.
Methods
Between October 2010 and December 2021, 39 patients were hospitalized and diagnosed with AAV thromboembolism in our hospital. All of these patients had a complete set of clinical data and thromboembolic events had been verified by computed tomography, magnetic resonance imaging, digital subtraction angiography or color Doppler ultrasound. As a control group, we randomly recruited 78 patients with AAV but without thromboembolism who had been hospitalized during the same period of time. The patients included conformed to the diagnostic criteria for systemic vasculitis formulated by the 2012 Chapel Hill Meeting.7 The exclusion criteria were as follows: (1) systemic vasculitis concomitant with other connective tissue diseases; (2) drug-induced secondary vasculitis; or (3) an incomplete data.
The demographics, clinical manifestation, and laboratory results of each patient at first diagnosis were collected, including inflammatory markers, routine blood results, renal function, blood fat, complement C3, complement C4, and ANCA. ANCA was detected by indirect immunofluorescence and enzyme linked immunosorbent assay (ELISA); the disease activity per patient was calculated according to the Birmingham Vasculitis Activity Score Version 38 and the Padua rating scale9 to evaluate the risk of thrombi. According to the Declaration of Helsinki, all patients agreed to participate and publish their data. The Ethics Committee at the Second Affiliated Hospital of Chongqing Medical University approved this study.
Statistical Analysis
Data were processed by SPSS software (version 25.0; IBM, Armonk, NY, USA) and R software (version 3.5.2; R Foundation, Vienna, Austria). To improve the reliability of data from a small sample size, all data were deemed to be non-parametric. Measurement data were expressed as medians (quartiles) and compared by the rank sum test. Numerical data were expressed as percentage ratios or rates, and compared by the Chi-squared test or Fisher’s exact test. Variables with a P < 0.1 in the single factor analysis were included in multi-factor logistic regression analysis (the step-back method) so that we could screen the specific risk factors for thrombosis in AAV patients. The risk prediction model was subsequently established pursuant to the risk factors determined by multi-factor logistic regression analysis. Receiver operator characteristic curve (ROC) analysis and DeLong inspection were used to evaluate the predictive value of the risk prediction model. P < 0.05 was deemed to be of statistical significance.
Results
Basic Information
Of the 39 patients with AAV, 20 were male and 19 were female; the median age was 70 years. Arterial thrombosis occurred in 23 of the 39 patients (58.97%); venous thrombi formed in 18 of the patients (46.15%), while both arterial and venous thrombi occurred in two patients (5.13%). Thrombosis occurred in 34 of the 39 patients (87.18%) three months before and after the diagnosis of AAV. Thrombosis occurred in four of these patients (10.26%) three months to one year after the diagnosis of AAV. Thrombus developed in one patient (2.56%) more than one year after the diagnosis of AAV (Table 1). Of the 78 AAV patients without thromboembolism, there were 39 males and 39 females; the median age was 63 years. All patients were treated with prednisolone and immunosuppressants.
 |
Table 1 General Information on 39 AAV Patients |
Comparison of General Information and Clinical Manifestations
Compared to AAV patients without thrombi, we found that age and hypertension ratio of patients in the AAV thrombus group were significantly higher (P = 0.019 and P = 0.019, respectively). There was no significant difference between the AAV thrombus group and the AAV group without thrombi in terms of gender, BMI, course of disease, smoking history, diabetes, coronary heart disease, or fever and organ involvement (P > 0.05; Table 2).
 |
Table 2 Comparison of General Information and Clinical Manifestation |
Comparison of Laboratory Results, BVAS Scores and Padua Scores
In terms of laboratory results, white blood cell count, neutrophil count and D-dimer were significantly higher in the AAV thrombus group than those in the AAV group without thrombi (P = 0.013, P = 0.049 and P = 0.009, respectively). The levels of albumin and high-density lipoprotein were significantly lower than those in the AAV group without thrombi (P = 0.017 and P = 0.005, respectively).
In terms of disease activity and thrombus assessment, compared to the AAV group without thrombi, both the BVAS score and the Padua score were significantly higher in the AAV with thrombi (P < 0.001 and P = 0.001, respectively) (Table 3).
 |
Table 3 Comparison of Laboratory Results, BVAS Scores and Padua Scores |
Multivariate Logistic Regression Analysis
Thromboembolism in AAV was used as the dependent variable for multivariate logistic regression analysis; variables that were significant (P < 0.1) in single factor analysis were used as concomitant variables. Multivariate logistic regression (the step-back method) showed that a high complement C3 level (odds ratio [OR]: 7.653; 95% confidence interval [CI]: 1.666–35.164), a high BVAS score (OR: 1.161; 95% CI: 1.068–1.263) and a high Padua score (OR 1.422: 95% CI: 1.091–1.854) were identified as independent risk factors for thrombosis in AAV patients (Table 4).
 |
Table 4 Multivariate Logistic Regression Analysis |
Establishment and Evaluation of a Predictive Model
A predictive model for the risk of thromboembolism (Table 4) was established in line with the results arising from multivariate logistic regression analysis. The regression equation is as shown in Equation (1).Equation (1): Logit(P)= −6.594 + 2.035 × complement C3 + 0.150 × BVAS score + 0.352 × Padua score. A ROC curve was generated from the model along with a separate Padua rating scale for predicting thrombus in AAV patients. DeLong inspection was used to compare the AUC of the model and the Padua rating scale(Figure 1). The AUC of the new risk prediction model was 0.803 (95% CI: 0.716–0.890), thus, showing that the predictive performance of the model was good. The maximum Youden index, sensitivity and specificity were 0.487, 59.0% and 89.7%, respectively. The AUC of the Padua rating scale was 0.671 (95% CI: 0.560–0.782); DeLong inspection showed that the new risk prediction model was significantly superior to the separate Padua rating scale (P = 0.001).
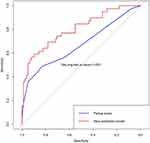 |
Figure 1 ROC curve for the new risk prediction model and Padua rating scale. |
Discussion
Although the survival rate for AAV patients has improved over the last few decades, the mortality rate for this condition is still 2.7-fold higher than that of the common population.10 As a key complication of AAV, arteriovenous thromboembolism increases the difficulty of treating AAV patients and can also influence the death rate.11,12 Therefore, identifying potential risk factors for thrombosis will help us to develop a predictive model for the risk of thrombi so that we can identify high-risk patients in the early phases of disease and thus perform targeted interventions and prevent thrombosis.
Our results suggested that age, proportion of hypertension, white blood cell count, neutrophil count and D-dimer levels of patients in the AAV group with thrombi were significantly higher than those in the AAV group without thrombi. The levels of albumin and high-density lipoprotein were significantly lower than those in the group without thrombi, indicating that these indicators might be potential risk factors for thromboembolic events. The influences of advanced age and high blood pressure on thrombi have been proven previously.13,14 An increased level of D-dimer indicates that hypercoagulability and hyperfibrinolysis have occurred and that the risk of thromboembolism has increased. Serum albumin is associated with anti-inflammatory, antioxidant, anticoagulant and anti-platelet aggregation activity as well as colloid osmosis.15 High-density lipoprotein plays a role in the reverse transport of cholesterol and also has anti-thrombosis characteristics.16 Therefore, it has been suggested that if we wish to prevent thrombosis in aged patients, then it is important to control blood pressure and correct hypoalbuminemia and lipid metabolism disorders.
The multivariate analysis carried out in this study proved that patients with AAV and high levels of complement C3 were more likely to develop thrombi. Complement C3 is the core component of the complement system and is activated by classical, lectin and alternative pathways. A substantial body of evidence now indicates that complement C3 is closely associated with the coagulation system.17,18 During the coagulation process, the coagulation/fibrinolytic cascade can activate complement C3. In contrast, the components of the complement system are also involved in thrombin activation and the regulation of platelet aggregation. The interaction between complement C3 and the coagulation system is helpful in promoting coagulation and reduce fibrinolysis and can ultimately result in a prethrombotic state.19,20 Research has shown that complement activation may contribute to thromboembolism and high concentrations of complement C3 were associated with high risk of venous thromboembolism.17 It is worth noting that new discoveries over recent years have shown that activation of the complement system is involved in the pathogenesis of AAV, especially the alternative complement pathway.21,22 This may be a common link between AAV and thrombosis, and the specific underlying mechanism needs further fundamental research. Therefore, it is important that we consider complement C3 as an important factor. However, in our single factor analysis, the difference in complement C3 between patients in the two groups was not statistically significant; it is likely that this is because the sample size of our study was too small and that the complement system activation resulted in the partial depletion of complement C3 during the onset of AAV.
The multivariate analysis performed in this study indicated that AAV patients with a high BVAS score were more likely to undergo thromboembolic events. The BVAS score is a good indicator for evaluating systemic vasculitis disease activity and higher scores indicate a higher levels of disease activity. Previous studies showed that high levels of inflammatory activity might trigger hypercoagulability in patients with inflammatory disease.23,24 Compared with patients with inactive AAV, the levels of neutrophil extracellular traps (NETs) was previously found to be significantly increased in patients with active AAV.25 NETs were activated by neutrophils and further formed, which played a key role in activating the coagulation cascade reaction, collecting platelets, and acting as a scaffold for thrombus assembly. These are all processes that facilitate the development of thrombosis, thus, suggesting that the risk of thrombosis was higher in patients with active AAV. Furthermore, our results showed that AAV patients had a high incidence of early thrombosis after diagnosis; this was consistent with previous studies;3,26 consequently, it is important that we consider the relationship between inflammatory activity and thrombosis. Therefore, AAV patients in the active stage of the disease require active treatment and the control of inflammation to prevent thrombosis; furthermore, close attention should be paid to the occurrence of thromboembolic events.
The multivariate analysis in this study showed that AAV patients with a high Padua score were more likely to suffer from thromboembolism. The Padua prediction score scale is a venous thromboembolism (VTE) risk evaluation model that was first proposed by Professor Barbar in 2010.9 The Padua thrombus scale items are succinct and clear; this scale is based on scientific items and is used widely in the clinic. The predictive value of the Padua scale for predicting thrombotic risk has been confirmed by many studies. In the present study, we found that a high Padua score was also of predictive value for arteriovenous thrombosis in AAV patients to some extent, but more research is needed. Thus, it is necessary to perform dynamic Padua score determination in AAV patients and take the appropriate preventive measures in a timely manner in patients with a high score.
At present, most studies on thromboembolism in AAV patients are still focused on the analysis of occurrence risk and risk factors. In this study, we established a risk prediction model for thrombus in AAV patients. The new model features three risk factors (complement C3 level, BVAS score, Padua score) that were identified by multivariate analysis. Receiver operator characteristic curve (ROC) analysis and DeLong inspection results showed that the new risk model could be used to predict the risk of thrombosis in AAV patients to some extent. The new model was superior to the separate Padua rating scale and was capable of rapidly evaluating the risk of thromboembolism in AAV patients clinically. The new model also supported the early identification of patients at high risk of thromboembolism and provided efficient indication to administer relevant preventive measures in high-risk groups to reduce the risk of thromboembolic events. Therefore, when patients are newly diagnosed with AAV, it is important that clinicians consider the dynamic BVAS activity score and Padua score and pay more attention to the risk of thrombosis in patients with a high level of complement C3, a high BVAS activity score and a high Padua score.
It is worth noting that this is a retrospective study and inherent limitations should not be ignored, including recall bias and limited data. Also, the Padua score is primarily used to predict the risk of VTE. Although this study shows that this score has some value in the assessment of arteriovenous thrombosis, more research is needed to explore the appropriate scale for arterial thrombosis in AAV patients. Finally, in terms of treatment, this study did not cover the effect of different doses of glucocorticoids or different immunosuppressants on thrombosis in patients with AAV, so it cannot provide effective guidance for clinical medication.
In summary, this study analyzed the risk factors of thromboembolism in ANCA-associated vasculitis patients, constructed a thrombus risk prediction model and provided a method for the early identification of thrombosis in AAV patients to help clinicians to actively prevent thrombosis in patients with AAV.27
Acknowledgments
This work was supported by grant no. 81771738 from the National Natural Science Foundation of China, the Talents Program of Chongqing and the Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Berti A, Matteson EL, Crowson CS, Specks U, Cornec D. Risk of cardiovascular disease and venous thromboembolism among patients with incident ANCA-associated vasculitis: a 20-year population-based cohort study. Mayo Clin Proc. 2018;93:597–606. doi:10.1016/j.mayocp.2018.02.010
2. Hansrivijit P, Trongtorsak A, Gadhiya KP, et al. Incidence and risk factors of venous thromboembolism in ANCA-associated vasculitis: a metaanalysis and metaregression. Clin Rheumatol. 2021;40:2843–2853. doi:10.1007/s10067-021-05589-8
3. Kang A, Antonelou M, Wong NL, et al. High incidence of arterial and venous thrombosis in antineutrophil cytoplasmic antibody-associated vasculitis. J Rheumatol. 2019;46:285–293. doi:10.3899/jrheum.170896
4. Misra DP, Thomas KN, Gasparyan AY, Zimba O. Mechanisms of thrombosis in ANCA-associated vasculitis. Clin Rheumatol. 2021;40:4807–4815. doi:10.1007/s10067-021-05790-9
5. Johannesdottir SA, et al. Use of glucocorticoids and risk of venous thromboembolism: a nationwide population-based case-control study. JAMA Intern Med. 2013;173:743–752. doi:10.1001/jamainternmed.2013.122
6. Hewins P, Savage C. Anti-neutrophil cytoplasm antibody associated vasculitis. Int J Biochem Cell Biol. 2003;35:277–282. doi:10.1016/s1357-2725(02)00094-8
7. Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum. 2013;65:1–11. doi:10.1002/art.37715
8. Mukhtyar C, et al. Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis. 2009;68:1827–1832. doi:10.1136/ard.2008.101279
9. Barbar S, Noventa F, Rossetto V, et al. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. J Thromb Haemost. 2010;8:2450–2457. doi:10.1111/j.1538-7836.2010.04044.x
10. Tan JA, Dehghan N, Chen W, et al. Mortality in ANCA-associated vasculitis: a meta-analysis of observational studies. Ann Rheum Dis. 2017;76:1566–1574. doi:10.1136/annrheumdis-2016-210942
11. Cohen AT, Tapson VF, Bergmann J-F, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371:387–394. doi:10.1016/s0140-6736(08)60202-0
12. Mercuzot C, Letertre S, Daien CI, et al. Comorbidities and health-related quality of life in patients with Antineutrophil Cytoplasmic Antibody (ANCA) - associated vasculitis. Autoimmun Rev. 2021;20:102708. doi:10.1016/j.autrev.2020.102708
13. Allenbach Y, Seror R, Pagnoux C, et al. High frequency of venous thromboembolic events in Churg-Strauss syndrome, Wegener’s granulomatosis and microscopic polyangiitis but not polyarteritis nodosa: a systematic retrospective study on 1130 patients. Ann Rheum Dis. 2009;68:564–567. doi:10.1136/ard.2008.099051
14. van den Born BJ, Löwenberg EC, van der Hoeven NV, et al. Endothelial dysfunction, platelet activation, thrombogenesis and fibrinolysis in patients with hypertensive crisis. J Hypertens. 2011;29:922–927. doi:10.1097/HJH.0b013e328345023d
15. Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med. 2018;52:8–12. doi:10.1016/j.ejim.2018.04.014
16. Nofer JR, Brodde MF, Kehrel BE. High-density lipoproteins, platelets and the pathogenesis of atherosclerosis. Clin Exp Pharmacol Physiol. 2010;37:726–735. doi:10.1111/j.1440-1681.2010.05377.x
17. Norgaard I, Nielsen SF, Nordestgaard BG. Complement C3 and high risk of venous thromboembolism: 80517 individuals from the Copenhagen general population study. Clin Chem. 2016;62:525–534. doi:10.1373/clinchem.2015.251314
18. Oikonomopoulou K, Ricklin D, Ward PA, Lambris JD. Interactions between coagulation and complement--their role in inflammation. Semin Immunopathol. 2012;34:151–165. doi:10.1007/s00281-011-0280-x
19. Hertle E, van Greevenbroek MM, Stehouwer CD. Complement C3: an emerging risk factor in cardiometabolic disease. Diabetologia. 2012;55:881–884. doi:10.1007/s00125-012-2462-z
20. Kambas K, Chrysanthopoulou A, Vassilopoulos D, et al. Tissue factor expression in neutrophil extracellular traps and neutrophil derived microparticles in antineutrophil cytoplasmic antibody associated vasculitis may promote thromboinflammation and the thrombophilic state associated with the disease. Ann Rheum Dis. 2014;73:1854–1863. doi:10.1136/annrheumdis-2013-203430
21. Brilland B, Garnier AS, Chevailler A, Jeannin P, Subra JF, Augusto JF. Complement alternative pathway in ANCA-associated vasculitis: two decades from bench to bedside. Autoimmun Rev. 2020;19:102424. doi:10.1016/j.autrev.2019.102424
22. Quintana LF, Kronbichler A, Blasco M, Zhao MH, Jayne D. ANCA associated vasculitis: the journey to complement-targeted therapies. Mol Immunol. 2019;112:394–398. doi:10.1016/j.molimm.2019.06.018
23. Antovic A, Svensson E, Lövström B, et al. Venous thromboembolism in anti-neutrophil cytoplasmic antibody-associated vasculitis: an underlying prothrombotic condition? Rheumatol Adv Pract. 2020;4:rkaa056. doi:10.1093/rap/rkaa056
24. Rao AN, Kazzaz NM, Knight JS. Do neutrophil extracellular traps contribute to the heightened risk of thrombosis in inflammatory diseases? World J Cardiol. 2015;7:829–842. doi:10.4330/wjc.v7.i12.829
25. Soderberg D, Kurz T, Motamedi A, Hellmark T, Eriksson P, Segelmark M. Increased levels of neutrophil extracellular trap remnants in the circulation of patients with small vessel vasculitis, but an inverse correlation to anti-neutrophil cytoplasmic antibodies during remission. Rheumatology. 2015;54:2085–2094. doi:10.1093/rheumatology/kev217
26. Liapi M, Jayne D, Merkel PA, Segelmark M, Mohammad AJ. Venous thromboembolism in ANCA-associated vasculitis: a population-based cohort study. Rheumatology. 2021;60:4616–4623. doi:10.1093/rheumatology/keab057
27. Asmamaw M, Hungnaw W, Motbainor A, Kedir HM, Tadesse TA. Incidence of thromboembolism and thromboprophylaxis in medical patients admitted to specialized hospital in Ethiopia using Padua prediction score. SAGE Open Med. 2022;10:20503121221079488. doi:10.1177/20503121221079488
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
