Back to Journals » Substance Abuse and Rehabilitation » Volume 9
Analysis of psychotropic drug-related deaths in south Osaka
Authors Tani N , Ikeda T, Michiue T, Oritani S, Morioka F, Ishikawa T
Received 23 January 2018
Accepted for publication 24 July 2018
Published 24 September 2018 Volume 2018:9 Pages 79—90
DOI https://doi.org/10.2147/SAR.S163491
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Li-Tzy Wu
Naoto Tani,1,2 Tomoya Ikeda,1,2 Tomomi Michiue,1,2 Shigeki Oritani,1 Fumiya Morioka,1 Takaki Ishikawa1,2
1Department of Legal Medicine, Osaka City University Medical School, Abeno, Osaka, Japan; 2Forensic Autopsy Section, Medico-legal Consultation and Postmortem Investigation Support Center, c/o Department of Legal Medicine, Osaka City University Medical School, Abeno, Osaka, Japan
Objective: The aim of this study was to investigate the occurrence of deaths due to psychotropic drugs in south Osaka during a 10-year period and discuss societal factors from a medical viewpoint.
Methods: Psychotropic drug-related deaths were retrospectively investigated based on the forensic postmortem data of 1,746 decedents in 2005–2014, and we excluded cases in which stimulant drugs were detected. Of these, 133 cases (7.6%) were found to be psychotropic drug-related deaths and were analyzed.
Results: Psychotropic drug-related deaths occurred in 78 males (59%; age range, 14–95 years) and 55 females (41%; 20–84 years). The direct cause of death was acute drug intoxication in many cases, and of these, acute combined drug intoxication due to the use of multiple drugs accounted for 76% of the deaths. Most of these victims were found to have gastrointestinal and cardiovascular diseases. Cases of psychotropic drug-related deaths had especially poor medical conditions. In addition, tests were positive for blood alcohol in 23% of the cases.
Conclusion: The descriptive results revealed several factors that may be related to psychotropic drug-related deaths. To prevent drug abuse, several factors were deemed to be important, including improvements in the medical state of an individual, the avoidance of social isolation, and from a medical standpoint, the management of prescription drugs by medical personnel.
Keywords: forensic autopsy, epidemiology, psychiatric drugs, drug abuse, dependency factor
Introduction
In recent years, deaths due to drug abuse have become a major societal problem worldwide.1–7 Psychotropic drugs in Japan have been allotted for medical use by the Ministry of Health, Labour and Welfare and were designated in the “Convention on Psychotropic Substances” of 1971. To help improve the health conditions of people across the country, Japan instituted a universal public insurance system. As a result, Japanese people can easily consult a hospital and obtain prescription drugs, including psychotropics. Although prohibited stimulants can be illegally acquired in Japan, most widely available psychotropic drugs are prescribed by physicians, and drug intoxication from overdose has resulted in several deaths.8 Causes of psychotropic drug-related deaths in Japan include frequent use of antipsychotropic polypharmacy and high doses of antipsychotics in Japanese and other Asian inpatients.9,10 Hori et al reported that patients who overdose on psychotropic drugs, especially in cases involving antipsychotics and/or barbiturates, should be observed carefully because of the higher associated risk of medical complications.5 Moreover, it was reported that psychotropic drugs can lead to strong dependency and have complicated drug interactions, and psychotropic drug abusers often suffer from depression.11 The burden of depression is significant in terms of direct treatment cost, social and intangible cost, missed working days, lower productivity, and decreased quality of life.12 In the present study, the medical records of patients who suffered a drug-related death were reviewed.
Osaka is the second most populous city in Japan, with approximately 2.7 million residents (as on October 1, 2016).13 The area of south Osaka accounts for approximately 43.1% (1.1 million) of the population in Osaka, and higher ratios of solitary persons, day laborers, and homeless people have lived in south Osaka from ancient times.14 Based on data from 2016, the unemployment rate in Japan is 3.2% although the rate was 4.5% in Osaka.15 In accordance with these unemployment rates, the proportion of welfare recipients across Japan is 14.37 per 1,000 persons, whereas that in Osaka is 34.26 per 1,000 persons.16 The population of poor people has recently been increasing, at least in part because of the many layoffs of temporary employees since the global financial crisis of 2008–2009.17,18 In Japan, drug dependency, including illegal drug abuse, has increased with growing economic uneasiness.19,20 Yamaguchi et al previously described the need to educate the public regarding the relationship between illegal drug use and poverty and infection.17
Our previous study reported that a high proportion of stimulant drug users in Osaka were living alone and/or unemployed. Specifically, of the 119 cases with a clearly identified occupational status, 83% of the stimulant drug users were unemployed, and of the 68 cases with a known living situation, 62% were living alone.21 Compared with other urban areas, the crime rate in Osaka is elevated and the abuse of drugs, such as illegal stimulants, has become a major societal problem.22 In addition, the most common cause of death observed among such users was multiple drug intoxication caused by simultaneous use of psychiatric drugs.23 The available data indicate the role of the following 3 factors contributing to stimulant abuse: societal (eg, economic situation and relationships), individual (eg, lack of knowledge about drugs and underlying mental illness), and pharmaceutical (eg, drug dependency and drug interaction).21,23
Numerous epidemiological studies on the demographic and health characteristics of illicit or nonmedical drug users in Japan have been conducted.22,25–29 Psychotropic drug users in Japan experience various problems, such as increased suicide risk, more severe family/social relationship problems, and greater harm to the health of the users.24–26 Fukui reported that the 12-month prevalence of analgesic, anxiolytic, and hypnotic use – both medical and nonmedical – in Japan was 35.5%, 6.4%, and 4.9%, respectively, according to a hospital investigation.27 It was reported that benzodiazepines were prescribed 6–20-fold more frequently in Japan than in Europe and the United States in 1998–1999.28 Additionally, it has been speculated that the use and abuse of prescription drugs, including analgesic, anxiolytic, and hypnotic drugs, might be increasing owing to easier access to such drugs through the social network system.29 Among patients with drug-related disorders, the proportion of psychotropic (sedative-hypnotic, anxiolytic) drug-related disorders doubled between 1998 and 2008.28 As prescription and psychotropic drugs are more easily accessible than illegal drugs, they are expected to have a more serious impact on society in Japan.29 Previous studies reported that the differences in abuse of psychotropic and stimulant drugs appear to be related to psychosocial and psychiatric factors.28 Thus, the present study used the mortality data to clarify the background characteristics of drug abuse based on previous epidemiological studies.19,22–25
In the present study, to clarify the background characteristics of psychotropic drug (eg, sedative-hypnotic, anxiolytic, and antidepressant drugs) abuse in south Osaka and to discuss societal factors from a medical viewpoint, we investigated deaths caused by psychotropic drugs other than illegal stimulants (eg, amphetamine and methamphetamine) from areas in south Osaka during a 10-year period (2005–2014). Moreover, we discussed preventive measures against psychotropic drug abuse based on previous epidemiological studies conducted in Japan.
Materials and methods
Sample collection
Among forensic autopsies conducted in our department from 2005 to 2014, we noted and analyzed the occurrence of psychotropic drug-related deaths in south Osaka. Psychotropic drug-related deaths were retrospectively investigated using the forensic postmortem data of 1,746 decedents in 2005–2014, and we excluded cases in which stimulant drugs were detected. Of these, 133 cases (7.6%) were psychotropic drug-related deaths and we analyzed these deaths from a medical viewpoint. Victims in which psychotropic drugs other than stimulants were detected were used in this study. The causes of death were classified according to the findings of the complete autopsy and macromorphological, micropathological, and toxicological examinations.30 If a psychotropic drug was found in a victim, then their medical history, cause of death, occupation, social status, age, sex, any organ diseases, psychotropic drug concentration and alcohol concentration in blood, and nutritional status were identified and reported. The background data of patients who suffered a psychotropic drug-related death were recorded in our database from each autopsy. These data were stored in our department and used for the present study. The variables for analysis were determined based on the autopsy record reviews and crime investigation information.
Study variable definitions
Psychotropic drug-related deaths were defined by the presence of psychotropic drugs in 1 or more biological samples, including blood, pericardial fluid, urine, gastric contents, bile, cerebrospinal fluid, bone marrow aspirate, and intrathoracic fluid. We analyzed cases in which the identified drugs were designated in Schedules III and IV in the “Convention on Psychotropic Substances”.31 If any drug was found in the victim, a classification of its schedule was identified while excluding stimulant drugs. Sample information (including age, sex, occupation, living condition, circumstances of death discovery, medical history, presence/absence of self-injury, cause of death, and organ disease) was collected based on postmortem pathological, chemical findings and crime investigation information. Nutritional status was calculated based on body mass index (BMI), determined by height and weight. Blood alcohol concentrations were determined using headspace gas chromatography/mass spectrometry.32 Ethanol levels were measured for autopsy cases within 48 hours to consider postmortem time, and n-propanol concentrations were measured at the same time. Toxicological analyses were conducted to identify the drug the victims had been using. Drug analyses were performed using gas chromatography/mass spectrometry.33 Toxicological analyses were performed in samples of right heart blood.
Data analysis
The information was stored in a Microsoft Excel database and submitted for statistical analysis. The results of quantitative and qualitative variables are described as percentages.
Results
Number of cases per year
In 10 years, 1,746 total forensic autopsies were conducted in our department. Of these, 133 cases were psychotropic drug-related deaths. Meanwhile, 102 deaths caused by stimulant drug abuse were excluded from the analysis. The number of cases per year in 2005, 2006, 2007, 2008, 2009, 2010, 2011, 2012, 2013, and 2014 was 7 cases (3 males, 4 females), 11 cases (5 males, 6 females), 14 cases (6 males, 8 females), 16 cases (10 males, 6 females), 21 cases (13 males, 8 females), 16 cases (9 males, 7 females), 12 cases (8 males, 4 females), 14 cases (9 males, 5 females), 11 cases (6 males, 5 females), and 11 cases (9 males, 2 females), respectively, or ranging from approximately 10 to 20 cases per year.
Age and sex
Psychotropic drug-related deaths occurred in 78 males (59%; age range, 14–95 years) and 55 females (41%; 20–84 years). The age distribution was as follows: 1 case (1 male) in the teens, 13 cases (4 males, 9 females; 10% of total) in their 20s, 25 cases (11 males, 14 females; 19% of total) in their 30s, 31 cases (19 males, 12 females; 23% of total) in their 40s, 18 cases (11 males, 7 females; 13% of total) in their 50s, 29 cases (22 males, 7 females; 22% of total) in their 60s, 13 cases (9 males, 4 females; 10% of total) in their 70s, 2 cases (2 females; 2% of total) in their 80s, and 1 case (1 male) in his 90s. Cases of psychotropic drug use peaked in the 30–49-year age group and the 60–69-year age group. In addition, between the ages of 20 and 39 years, females accounted for 61% of the cases, while between the ages of 40–79 years, males comprised 67% of the cases. People aged ≥70 years accounted for 16 cases (10 males, 6 females, 12% of the total; Figure 1).
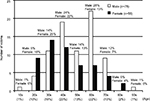  | Figure 1 Age-specific psychotropic drug-related deaths (n=133). |
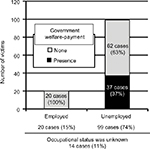
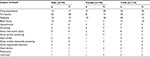
Occupation
The occupational status was as follows: 20 cases (12 males, 8 females; 15% of total) employed, 99 cases (55 males, 44 females; 74% of total) unemployed, and 14 cases (11 males, 3 females; 11% of total) unknown. Of the 119 cases with a clearly identified occupational status, 83% were unemployed and 17% were employed. Of the unemployed, 37 cases (37%) were welfare assistance recipients. Four cases (20%) were employed while receiving welfare services. In addition, when examining unemployment by age, in the standard working age (20s–50s) group of 62 cases, 8 cases (3 males, 5 females; 13%) were in their 20s, 22 cases (9 males, 13 females; 35%) were in their 30s, 19 cases (11 males, 8 females; 31%) were in their 40s, and 13 cases (7 males, 6 females; 21%) were in their 50s. In the standard working age group of the unemployed, 66% (41 cases) were aged 30–49 years; in this age group, 46% were welfare recipients (Figure 2).
Living situation
Of the 112 cases where the living situation was known, equal numbers lived alone or with family/other cohabitants (56 cases or 50% in each situation; Table 1).
  | Table 1 Study items with regard to psychotropic drug-related deaths Abbreviation: BMI, body mass index. |
Circumstances of death discovery
Deaths discovered within 12 hours were reported for 92 cases (69% of total), and those discovered after 12 hours were noted in 41 cases (31% of total). Discovery more than 2 weeks after death occurred in only 3 cases. Locations where deaths were discovered represented both indoor (111 cases; 84% of total) and outdoor (22 cases; 16% of total) environments. In the indoor discoveries, 107 cases (96%) were in homes, 2 cases (2%) were in hotels, and 2 cases (2%) were in other locations (police station and office). In the outdoor discoveries, 8 cases (36%) were on the street, 7 cases (32%) were within building premises such as parking lot stairs, 4 cases (18%) were in rivers and harbors, and 3 cases (14%) were in other public facilities (Table 1).
Medical history
Medical histories were known in 97 cases (73% of the total) and unknown in 36 cases (27% of the total). Of the 97 cases with known medical histories, mental illness was diagnosed in 82 cases (85%; Table 1).
Presence/absence of self-injury
Among the 133 cases, self-injury was present in 23 cases (11 males, 12 females; 17% of total) and absent in 110 cases (83% of the total). Self-injury was noted in 12 of 55 female (22%) cases and in 11 of 78 male (14%) cases (Table 1).
Nutritional status
The BMI in 100 deaths reported within 72 hours (survival time) was ≥30 kg/m2 (obese) in 8 cases (6%), 25–29.9 kg/m2 (overweight) in 14 cases (11%), 18.5–24.9 kg/m2 (normal weight) in 61 cases (46%), and <18.5 kg/m2 (underweight) in 17 cases (13%; Table 1).
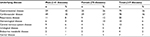
Cause of death
Death by acute drug intoxication occurred in 34 cases (26% of the total). Of these, 26 deaths were due to acute combined drug intoxication associated with multiple drug administration, and 8 deaths were caused by the use of a single drug. Causes of death other than drug intoxication were fire fatality (30 cases; 23% of the total), asphyxia (20 cases; 15% of the total), blunt injury (13 cases; 10% of the total), hypothermia (7 cases; 5% of the total), drowning (7 cases; 5% of the total), sharp instrument injury (6 cases; 5% of the total), acute alcohol poisoning (3 cases; 2% of the total), heat stroke (3 cases; 2% of the total), acute carbon monoxide poisoning (3 cases; 2% of the total), acute myocardial infarction (2 cases; 2% of the total), heart failure (2 cases; 2% of the total), pneumonia (1 case), and unknown (2 cases; Figure 3 and Table S1).
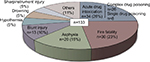  | Figure 3 Causes of death related to psychotropic drug administration. |
Organ disease
Upon performing autopsy, 219 instances of disease (including cases with co-occurring diseases) were discovered. Gastrointestinal diseases accounted for 79 cases (36%); of these, occurrences of liver cirrhosis and hepatitis (28 cases; 35%), fatty liver (23 cases; 29%), pancreatic steatosis and fibrosis (23 cases; 29%), liver cysts (2 cases; 3%), and others (3 cases; 4%) were noted. Of the 80 cases analyzed for the presence of hepatitis C virus, 22 cases (27%) were positive and 58 cases (73%) were negative. Of the 70 cases investigated for the presence of hepatitis B virus, all were negative. Cardiovascular diseases accounted for 78 cases (36%); of these, occurrences of cardiac hypertrophy and dilatation (35 cases; 45%), myocardial infarction and ischemic cardiac disease (16 cases; 21%), coronary arteriosclerosis and stenosis (11 cases; 14%), right ventricular fatty infiltration (11 cases; 14%), and heart failure (5 cases; 6%) were detected. Respiratory diseases accounted for 20 cases (9%); of these, occurrences of pneumonia (7 cases), emphysema (5 cases), tuberculosis (4 cases), pulmonary fibrosis (3 cases), and bronchitis (1 case) were noted. Central nervous system diseases accounted for 13 cases (6%); of these, occurrences of cerebral atrophy (6 cases), cerebral softening and infarction (4 cases), cerebral hemorrhage (2 cases), and pituitary abscess (1 case) were observed. Urological diseases accounted for 8 cases (4%); of these, occurrences of renal dysfunction, renal sclerosis and fibrosis, and nephritis (3, 3, and 2 cases, respectively) were noted. Hematological diseases diagnosed from blood biochemical and histopathological examinations accounted for 14 cases (5%); of these, there were occurrences of hypercholesterolemia (13 cases) and hypocholesterolemia (1 case). Endocrine metabolic disease accounted for 4 cases (3%); of these, diabetes (3 cases) and thyroiditis (1 case) were observed. Additionally, 2 cases of uterine fibroids and 1 case of prostatic hyperplasia were detected (Figure 4 and Table S2).
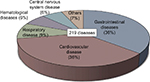  | Figure 4 Underlying disease identified on performing autopsy in cases of psychotropic drug-related deaths. |
Psychotropic drug concentration in blood
Measurable drugs in samples of right endocardial blood were noted in 69 cases. The 11 detected psychotropic drugs were amobarbital, flunitrazepam, pentobarbital, alprazolam, estazolam, diazepam, zolpidem, phenobarbital, bromazepam, midazolam, and flurazepam. In the 69 cases, the occurrences and levels of the drugs were as follows: phenobarbital in 41 cases (59%), zolpidem in 9 cases (13%), estazolam in 8 cases (12%), diazepam in 6 cases (9%), midazolam in 4 cases (6%), bromazepam in 3 cases (4%), pentobarbital in 3 cases (4%), alprazolam in 2 cases (3%), flurazepam in 2 cases (3%), and 1 case each of amobarbital and flunitrazepam (Table 2). In cases in which a psychotropic drug was detected, other drugs (without Schedules II through IV in the “Convention on Psychotropic Substances”) included acetaminophen, amitriptyline, chlorpheniramine, chlorpromazine, desalkylflurazepam, desipramine, dihydrocodeine, diphenhydramine, imipramine, levomepromazine, lidocaine, methotrimeprazine, methylephedrine, olanzapine, promethazine, and sertraline. We detected many other drugs in psychotropic drug users. Toxicological analyses were performed in samples of right heart blood. However, in this matrix, psychotropic drug concentrations may be overestimated if substances were orally administered, due to diffusion artifacts (Tables 3 and S3).
  | Table 2 Detected drug concentrations in Schedules III and IV in the “Convention on Psychotropic Substances” |
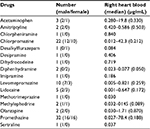  | Table 3 Detected drug concentrations except for those in Schedules III and IV in the “Convention on Psychotropic Substances” |
Blood alcohol concentration
Among the 115 cases (86% of total) that had detectable blood alcohol concentrations, 91 cases had detected blood alcohol concentrations within 48 hours postmortem. Of these, 21 cases (23%) had significantly high blood alcohol content. Alcohol concentrations in right endocardial blood were 0.1–0.5 mg/mL (exhilarating period) in 9 cases, 0.5–1.0 mg/mL (tipsy period) in 3 cases, 1.0–1.5 mg/mL (mild drunkenness period) in 2 cases, 1.5–2.5 mg/mL (drunkenness period) in 3 cases, and 2.5–3.5 mg/mL (drunk period) in 4 cases.34 Blood alcohol concentrations >3.5 mg/mL (sopor period) were not observed (Table 4).
  | Table 4 Blood alcohol concentrations in cases of psychotropic drug-related deaths (postmortem period<48 hours) |
Discussion
Psychotropic drug-related deaths in this study accounted for 7.6% of all autopsies conducted in our department over the 10-year period. To further clarify the factors associated with psychotropic drug abuse, particularly with prescription drug abuse, we excluded subjects who used illegal drugs, such as stimulants. Psychotropic drug users showed a wide age range from the teens to the 90s, with a tendency for more female deaths in younger age groups and male deaths in middle and advanced age groups. More specifically, those aged between their 30s and their 70s comprised 77% of all cases, males in their 60s comprised 28%, and females in their 30s comprised 25%. In 50% of the cases, individuals lived alone, and many were discovered in their homes. Where the occupational status was known, 83% were unemployed and a large number were receiving welfare assistance. Despite being of working age, many of those in their 30s and 40s were unemployed and were welfare recipients. Therefore, as many drug users were found living alone and unemployed, societal circumstances such as isolation are believed to be involved.35,36 These findings suggested the necessity of preventing social isolation and raising awareness regarding mental disorders and of how to improve one’s individual social skills. In younger people, there was a tendency for more unemployed females. While there were many unemployed psychotropic drug users, high unemployment rate in mentally ill individuals seems to be a major concern in Japan and throughout the world.37,38 Furthermore, prescription drug users, including psychotropic drug users, were more likely to be in their 30s and 40s, and no significant differences were observed between males and females in the proportion of psychotropic drug-related deaths in Japan. However, the present study revealed that psychoactive drug users were more likely to be males in their 60s or females in their 30s. It is presumed that social isolation after retirement is a related factor.39 Since young females are susceptible to stress and their mental condition tends to become unstable, it seems that young females increased the number of psychotropic drugs, leading to death.40,41 We speculate that exposure to psychotropic drugs among females at an earlier age than males has an influence on their differing death rates.
Medical histories revealed that 85% of the cases had mental illness and 14% had self-injurious behavior. BMIs were standard in many of the cases. Many cases of mental illness were found, and many psychotropics and other drugs were also detected. These findings suggest that, for drug users, mental illness is deeply involved as an individual factor in substance abuse. Autopsies uncovered that the most frequent organ diseases were gastrointestinal diseases, followed by cardiovascular diseases. In previous studies, not only psychiatric disorders but also cardiac and hepatic diseases were frequently seen.42,43 This suggests that anxiety and stress present in individuals by physiological deterioration are deeply involved as personal factors in drug use, and it cannot be denied that the road to societal reintegration may be closed. These results suggested the need to prevent organ disease. Many studies have reported that psychotropic drug abuse involved not only mental illness but also various diseases such as gastrointestinal diseases.42,43 Therefore, we speculated that the organ damage was due to the psychotropic drugs taken. However, we could not identify psychotropic drug-specific organ damages.
Of the 34 cases determined to be death by acute drug intoxication, 76% were due to acute combined drug intoxication. It has been speculated that the influence of multiple drugs on the psychological condition is closely related to death.44 Drug toxicology results showed the presence of phenobarbital in approximately 60% of the cases; moreover, about 20% had detectable blood alcohol concentrations. Phenobarbital was the most frequently used drug, and it was used in combination. It appears that individuals living on their own could not properly use drugs, and it was revealed that there were many cases with multiple drug and alcohol/drug combination use.45 Our results indicate that as a pharmaceutical factor, the use of psychotropic drugs to treat mental illness has a substantial effect on death.46,47
However, we could not identify whether the purpose of drug use is abuse or treatment. Furthermore, psychotropic drugs are not easily obtained as they are prescribed by a physician. Although Japan has less widespread use of illegal drugs than other countries in the world, it has been reported that the abuse of prescription drugs is still high.29 There are several reports on the danger of prescription drug abuse. Shimane et al suggested that community pharmacists play a critical role in prevention of the prescription drug abuse.8 Thus, we consider the appropriate management by medical personnel to be crucial for prescriptions of psychotropic and similar types of drugs.
There are some limitations in this study. In this study, some information was investigated based on investigation documents from the police, and some cases had missing details. We could not identify whether the purpose of drug use was abuse or treatment. Because this study covers all cases in which psychotropic drugs except stimulant drugs were detected, it was difficult to distinguish between chronic users and temporary users. Accordingly, to investigate the background of more chronic psychotropic abusers, there may be a need to distinguish between chronic users and temporary users.
In summary, our descriptive results revealed several factors that may be related to psychotropic drug-related deaths: a societal factor including occupation, living situation, and circumstances of death discovery; an individual factor including age, sex, medical history, self-injury, nutritional status, and organ disease; and a pharmaceutical factor including cause of death, psychotropic drug concentration, and alcohol concentration. However, these 3 factors are related in a complex manner.
Conclusion
The descriptive results suggest that societal, individual, and pharmaceutical factors may be related to psychotropic drug-related deaths. To prevent drug abuse, improvements in treating the psychological and physiological conditions of individuals, preventing social isolation, as well as controlling pharmaceuticals through prescription medication management appear to be important.
Disclosure
The authors report no conflicts of interest in this work.
References
Campelo EL, Caldas ED. Postmortem data related to drug and toxic substance use in the Federal District, Brazil, from 2006 to 2008. Forensic Sci Int. 2010;200(1–3):136–140. | ||
Stenbacka M, Leifman A, Romelsjö A. Mortality and cause of death among 1705 illicit drug users: a 37 year follow up. Drug Alcohol Rev. 2010;29(1):21–27. | ||
Pardo Cabello AJ, del Pozo Gavilán E, Gómez Jiménez FJ, et al. Drug-related mortality among inpatients: a retrospective observational study. Eur J Clin Pharmacol. 2016;72(6):731–736. | ||
Lee D, Delcher C, Maldonado-Molina MM, Thogmartin JR, Goldberger BA. Manners of death in drug-related fatalities in Florida. J Forensic Sci. 2016;61(3):735–742. | ||
Hori S, Kinoshita K. Clinical characteristics of patients who overdose on multiple psychotropic drugs in Tokyo. J Toxicol Sci. 2016; 41(6):765–773. | ||
Kruckow L, Linnet K, Banner J. Psychiatric disorders are overlooked in patients with drug abuse. Dan Med J. 2016;63(3):A5207. | ||
Westermeyer J. Cultural patterns of drug and alcohol use: an analysis of host and agent in the cultural environment. Bull Narc. 1987;39(2):11–27. | ||
Shimane T, Matsumoto T, Wada K. Clinical behavior of Japanese community pharmacists for preventing prescription drug overdose. Psychiatry Clin Neurosci. 2015;69(4):220–227. | ||
Xiang Y-T, Kato TA, Kishimoto T, et al. Comparison of treatment patterns in schizophrenia between China and Japan (2001-2009). Asia Pac Psychiatry. 2017;9(4):e12277. | ||
Yamada T, Kawanishi C, Hasegawa H, et al. Psychiatric assessment of suicide attempters in Japan: a pilot study at a critical emergency unit in an urban area. BMC Psychiatry. 2007;7:64. | ||
English BA, Dortch M, Ereshefsky L, Jhee S. Clinically significant psychotropic drug-drug interactions in the primary care setting. Curr Psychiatry Rep. 2012;14(4):376–390. | ||
Maniadakis N, Kourlaba G, Mougiakos T, Chatzimanolis I, Jonsson L. Economic evaluation of agomelatine relative to other antidepressants for treatment of major depressive disorders in Greece. BMC Health Serv Res. 2013;13:173. | ||
Kajino K, Kitamura T, Iwami T, et al. Impact of the number of on-scene emergency life-saving technicians and outcomes from out-of-hospital cardiac arrest in Osaka City. Resuscitation. 2014;85(1):59–64. | ||
Tabuchi T, Takatorige T, Hirayama Y, et al. Tuberculosis infection among homeless persons and caregivers in a high-tuberculosis-prevalence area in Japan: a cross-sectional study. BMC Infect Dis. 2011;11:22. | ||
Labour Force Survey Results In Osaka (January–March, 2018) [homepage on the Internet]. Available from: http://www.pref.osaka.lg.jp/toukei/roucho/index.html. Accessed August 31, 2018. | ||
Social Indicators by Prefecture 2016 [homepage on the Internet]. Tokyo: Statistics Bureau, Ministry of Internal Affairs and Communications. Available from: http://www.stat.go.jp/index.html. Accessed August 31, 2018. | ||
Yamaguchi Y, Enomoto M, Fujii H, et al. High prevalence of hepatitis C virus infection in Airin district, Osaka, Japan: a hospital-based study of 1162 patients. Hepatol Res. 2011;41(8):731–737. | ||
Danno K, Komukai J, Yoshida H, et al. Influence of the 2009 financial crisis on detection of advanced pulmonary tuberculosis in Osaka city, Japan: a cross-sectional study. BMJ Open. 2013;3(4):e001489. | ||
Kubota Y, Hasegawa K, Taguchi H, et al. Characteristics and trends of emergency patients with drug overdose in Osaka. Acute Med Surg. 2015;2(4):237–243. | ||
Muramatsu K, Matsuda S, Hayashida K, Kubo T, Fujino Y. Analysis of relationship between socio-economic factors and subjective health condition among the community inhabitants of Japan. Asia Pac J Dis Manag. 2011;5(2):35–41. | ||
Tani N, Chen JH, Michiue T, Oritani S, Ishikawa T. Retrospective investigation of psychostimulant-related fatalities in forensic autopsy during 10 years in the southern half of Osaka city and surrounding areas. Japan J Forensic Pathol. 2016;22:13–20 (in Japanese). | ||
Ikeda S, Nakamori Y, Canuet L, et al. Emerging risks of new types of drug addiction in Japan. Ment Health Fam Med. 2017;13:480–485. | ||
Zhu B-L, Oritani S, Shimotouge K, et al. Methamphetamine-related fatalities in forensic autopsy during 5 years in the southern half of Osaka city and surrounding areas. Forensic Sci Int. 2000;113(1–3):443–447. | ||
Hirokawa S, Matsumoto T, Katsumata Y, et al. Psychosocial and psychiatric characteristics of suicide completers with psychiatric treatment before death: a psychological autopsy study of 76 cases. Psychiatry Clin Neurosci. 2012;66(4):292–302. | ||
Ogai Y, Senoo E, Gardner FC, et al. Association between experience of child abuse and severity of drug addiction measured by the Addiction Severity Index among Japanese drug-dependent patients. Int J Environ Res Public Health. 2015;12(3):2781–2792. | ||
Wada K. The history and current state of drug abuse in Japan. Ann N Y Acad Sci. 2011;1216:62–72. | ||
Fukui S. Epidemiology of antianxiety and tranquilizing agent dependence in Japan. Nihon Shinkei Seishin Yakurigaku Zasshi. 1999;19(4):209–213 (in Japanese). | ||
Matsumoto T, Ozaki S, Kobayashi O, Wada K. Current situation and clinical characteristics of sedative-related disorder patients in Japan: a comparison with methamphetamine-related disorder patients. Seishin Shinkeigaku Zasshi. 2011;113(12):1184–1198 (in Japanese). | ||
Tominaga M, Kawakami N, Ono Y, et al. Prevalence and correlates of illicit and non-medical use of psychotropic drugs in Japan: findings from the World Mental Health Japan Survey 2002-2004. Soc Psychiatry Psychiatr Epidemiol. 2009;44(9):777–783. | ||
Tani N, Ikeda T, Oritani S, Michiue T, Ishikawa T. Role of circadian clock genes in sudden cardiac death: a pilot study. J Hard Tissue Biol. 2017;26(4):347–354. | ||
United Nations Office on Drugs and Crime. Convention on psychotropic substances. Available from: https://www.unodc.org/pdf/convention_1971_en.pdf. Accessed May 16, 2017. | ||
Maeda H, Zhu BL, Ishikawa T, et al. Evaluation of post-mortem ethanol concentrations in pericardial fluid and bone marrow aspirate. Forensic Sci Int. 2006;161(2–3):141–143. | ||
Tominaga M, Michiue T, Oritani S, Ishikawa T, Maeda H. Evaluation of postmortem drug concentrations in bile compared with blood and urine in forensic autopsy cases. J Anal Toxicol. 2016;40(5):367–373. | ||
Kinoshita H, Ameno K, Jamal M. Ethanol, methanol, and toluene. Japan J Forensic Pathol. 2009;15:37–44. Japanese. | ||
Minami U, Nishi M, Fukaya T, et al. Effects of the change in working status on the health of older people in Japan. PLoS One. 2015;10(12):e0144069. | ||
Batool S, Manzoor I, Hassnain S, et al. Pattern of addiction and its relapse among habitual drug abusers in Lahore, Pakistan. East Mediterr Health J. 2017;23(3):168–172. | ||
Kinoshita Y, Furukawa TA, Omori IM, et al. Supported employment for adults with severe mental illness. Cochrane Database Syst Rev. 2013;(9):CD008297. | ||
Luciano A, Meara E. Employment status of people with mental illness: national survey data from 2009 and 2010. Psychiatr Serv. 2014;65(10):1201–1209. | ||
Stickley A, Koyanagi A. Loneliness, common mental disorders and suicidal behavior: findings from a general population survey. J Affect Disord. 2016;197:81–87. | ||
van Droogenbroeck F, Spruyt B, Keppens G. Gender differences in mental health problems among adolescents and the role of social support: results from the Belgian health interview surveys 2008 and 2013. BMC Psychiatry. 2018;18(1):6. | ||
Simoni-Wastila L, Ritter G, Strickler G. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Subst Use Misuse. 2004;39(1):1–23. | ||
Carrier P, Debette-Gratien M, Girard M, et al. Liver illness and psychiatric patients. Hepat Mon. 2016;16(12):e41564. | ||
Telles-Correia D, Barbosa A, Cortez-Pinto H, Campos C, Rocha NBF, Machado S. Psychotropic drugs and liver disease: a critical review of pharmacokinetics and liver toxicity. World J Gastrointest Pharmacol Ther. 2017;8(1):26–38. | ||
Webb L, Oyefeso A, Schifano F, et al. Cause and manner of death in drug-related fatality: an analysis of drug-related deaths recorded by coroners in England and Wales in 2000. Drug Alcohol Depend. 2003;72(1):67–74. | ||
Carrà G, Johnson S, Crocamo C, et al. Psychosocial functioning, quality of life and clinical correlates of comorbid alcohol and drug dependence syndromes in people with schizophrenia across Europe. Psychiatry Res. 2016;239:301–307. | ||
Pereira-Morales AJ, Adan A, Camargo A, Forero DA. Substance use and suicide risk in a sample of young Colombian adults: an exploration of psychosocial factors. Am J Addict. 2017;26(4):388–394. | ||
Takeuchi T, Takenoshita S, Taka F, Nakao M, Nomura K. The relationship between psychotropic drug use and suicidal behavior in Japan: Japanese Adverse Drug Event Report. Pharmacopsychiatry. 2017;50(2):69–73. |
Supplementary materials
  | Table S1 Causes of death related to psychotropic drugs |
  | Table S2 Underlying disease identified based on performing autopsies in cases of psychotropic drug-related deaths |
  | Table S3 Compound drug detection and number of cases Note: aExcept for Schedules III and IV in the “Convention on Psychotropic Substances”. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.