Back to Journals » Infection and Drug Resistance » Volume 16
Analysis of Pathogenic Bacteria and Drug Resistance Among Girls with Bacterial Vaginitis
Authors Zhang M, Liu J, Pan YC, Liu HL, Shu J, Wu XM, Yang Y
Received 28 January 2023
Accepted for publication 16 March 2023
Published 30 March 2023 Volume 2023:16 Pages 1849—1863
DOI https://doi.org/10.2147/IDR.S403304
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Miao Zhang, Jing Liu, Yu-Chen Pan, Hui-Li Liu, Jing Shu, Xiao-Ming Wu, Yang Yang
Department of Pediatric Gynecology, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, China
Correspondence: Jing Liu, Department of Pediatric Gynecology, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, People’s Republic of China, Tel +86 010 59616889, Email [email protected]
Objective: The aim of this study was to analyze the prevalence of vaginal flora and drug resistance in bacterial vaginitis among girls.
Methods: A total of 3099 girls (0– 10 years old) with vaginitis who visited the Beijing Children’s Hospital from January 2020 to December 2021 were included in the present study. The clinical data, results of bacterial culture of vaginal secretions, and drug sensitivity reports of the subjects were collected and analyzed.
Results: Of the 3099 girls with vaginitis, 399 girls had a positive bacterial culture of vaginal secretions. Nineteen types of bacteria were cultured from the vaginal secretions of these 399 girls, with a total of 419 strains. The top three infective bacteria were Haemophilus influenzae (127 strains, 30.31%), Staphylococcus aureus (66 strains, 15.75%), and Streptococcus agalactiae (32 strains, 7.64%). Additionally, 20 girls were simultaneously infected with two types of bacteria. Staphylococcus aureus, Group G Streptococcus, Haemophilus parainfluenzae, and Pseudomonas aeruginosa more frequently occurred in mixed infections. The number and bacterial detection rate among school-age girls were higher than those of preschool-age girls. We found seasonal variation in infection rates, and vaginitis among girls was higher in summer. Recurrence of vaginitis in girls was not related to the type of pathogenic bacteria in the infection. Drug sensitivity analyses showed that the resistance rates of clindamycin and erythromycin were generally high, 70– 100%. After the coronavirus disease 2019 outbreak, the resistance rates of some antibiotics had decreased to varying degrees.
Conclusion: Improving the understanding of vaginal flora and drug resistance in girls with vaginitis will facilitate the selection of highly effective and sensitive antibacterial drugs and reduce the production of drug-resistant strains.
Keywords: drug sensitivity analysis, girls, pathogenic bacteria, vaginitis
Introduction
Vulvovaginitis is one of the most common gynecological diseases in pediatric and adolescent females.1 A study of paediatric and adolescent gynaecology services in a British district general hospital mentioned the commonest presentations were vulvovaginitis.2 The situation is similar in our country. In the past 5 years, our pediatric gynecology department has seen more than 10,000 cases of children throughout the year, and the incidence is increasing year by year, with vulvovaginitis accounting for more than 60% of the cases. This is attributable to the vulnerability of girls to infection due to the low level of estrogen, poor development of the vulva and vagina, thin vaginal mucosa, few glycogen in the vaginal epithelium, low resistance of the vaginal epithelium, and unformed natural defenses of the vagina.3 The pathogenic spectrum of vulvovaginitis infection varies between developmental periods in children, with Candida infection being more common in adolescence.4 Vaginitis in girls most commonly results from bacterial infections.5 The literature has reported that the main pathogen of vaginitis in 52.7% of prepubertal girls was bacteria6 which may induce diseases such as vulvar eczema, urinary tract infection, adhesions of the labia minora, masturbation syndrome, and vulvar lichen sclerosus if not treated promptly and regularly.7 It may seriously affect the child’s life, lead to negative emotions, and affect school, marriage and reproductive health in adulthood.7 It is important to note that pathogenic bacteria involved in vaginal infections among girls have partially changed after the coronavirus disease 2019 (COVID-19) outbreak. In this study, we included girls with vaginitis who visited the Pediatrics and Gynecology Clinic of the Beijing Children’s Hospital, Capital Medical University from 2020 to 2021 to analyze the detection, prevalence, change, and drug resistance of pathogenic bacteria in the bacterial culture of vaginal secretions, to offer a reliable basis for clinical diagnosis, treatment, and rational use of antibacterial drugs.
Materials and Methods
Study Respondents
We selected girls with vaginitis who were first-visit patients at the Pediatrics and Gynecology Clinic at Beijing Children’s Hospital, Capital Medical University between 2020 and 2021, Age 0~<10 years, and collected their clinical and laboratory data. The study was approved by the Hospital Medical Ethics Committee (Approval No.IEC-C-006-A03-V.05). The parents of the girls also signed an informed consent form. All procedures performed in this study were following the Declaration of Helsinki and its later amendments or comparable ethical standards.
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: Main complaints of vulvar odor, itching, burning sensation, pain, and discomfort as per the diagnostic criteria for vaginitis in Pediatric and Adolescent Gynecology;3 gynecologic examination showed red and swollen vulvar skins, congested vulval vestibular or vaginal mucosa, and purulent vaginal secretions; girls were clinically diagnosed with vaginitis. Exclusion criteria were as follows: Patients who had recently used antibiotics and other drugs; girls who had coexisting severe organ lesions. Subjects who have poor compliance and cannot complete the test.
Specimen Collection
Before taking the specimen, the child’s vulva was fully rinsed with 0.9% sterile sodium chloride, and then the specimen was taken by gentle rotation after probing into the lower third of the vaginal orifice with a sterile cotton swab, and the specimen was sent for examination immediately after removal.
Bacterial Culture and Drug Sensitivity Analysis
Bacteria were identified using the BD PhoenixTM 100 Bacterial Identification and Drug Sensitivity Analysis Instrument (BD Biosciences, Franklin Lakes, NJ, USA). Drug sensitivity analyses were done using the disk diffusion method. The results were analyzed with reference to the Performance Standards for Antimicrobial Susceptibility Testing (29th edition) published by the Clinical and Laboratory Standards Institute.
Statistical Analysis
Quantitative data were expressed as frequency (N) and percentage (%). The χ2 or Fisher’s exact test was used for the analysis of differences between two groups. Measurement data were tested for normality with the Shapiro–Wilk test and described as mean ± standard deviation. The t-test was utilized for comparisons of measurement data with normality between two groups, whereas the Mann–Whitney rank sum test was used for comparisons of data with skewed distribution between two groups. P < 0.05 was considered a statistically significant difference.
Results
Epidemiological Profile
Between 2020 and 2021, there were 3099 girls with vaginitis who were first-visit patients at the Pediatrics and Gynecology Clinic. Among these, 932 girls (30.07%) were <6 years old and 2167 girls (69.93%) were ≥6 years old, with 318 visits (10.26%) in spring (March–May), 1308 visits (42.21%) in summer (June–August), 912 visits (29.43%) in autumn (September–November), and 561 visits (18.10%) in winter (December–February). There were 399 girls with a positive bacterial culture of vaginal secretions, among which 136 girls (34.09%) were <6 years old and 263 girls (65.91%) were >6 years old, with 76 cases (19.05%) detected in spring (March–May), 170 cases (42.60%) in summer (June–August), 93 cases (23.31%) in autumn (September–November), and 60 cases (15.04%) in winter (December–February).
Among the children with bacterial vaginitis, there were 14 cases of vulvar eczema, 2 cases of adhesions of the labia minora, 5 cases of vulvar lichen sclerosus, and 17 cases of urinary tract infection.
Analysis of Bacterial Species
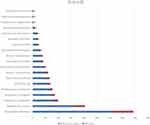
Among the 399 children with a positive bacterial culture of vaginal secretions, 19 species of bacteria were detected, with a total of 419 strains. Of these, 20 children were infected with 2 species of bacteria at the same time, and the top three infective bacteria in order of frequency were Haemophilus influenzae (127 strains, 30.31%), Staphylococcus aureus (66 strains, 15.75%), and Streptococcus agalactiae (32 strains, 7.64%) (Table 1, Figure 1).
 |
Table 1 Distribution of Bacteria in Vaginal Secretions |
Analysis of Bacterial Infections in Different Age Groups
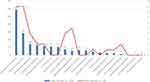
The prevalence rate of Haemophilus influenzae in the flora of preschool girls (Age <6 years) was 42.6%, which was higher than that of school-age girls (Age ≥6 years) (26.2%). In addition, the prevalence rate of Streptococcus pneumoniae was higher in preschool girls, while that of Staphylococcus aureus and Streptococcus pyogenes were higher in school-age girls (P < 0.05) (Table 2, Figure 2).
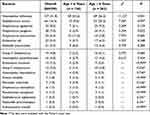 |
Table 2 Age-Wise Prevalence of Bacterial Infections |
 |
Figure 2 Distribution of bacterial strains in different age groups, both in children younger than 6 years of preschool age and in children older than 6 years of school age. |
Analysis of Bacterial Infections in Different Seasons
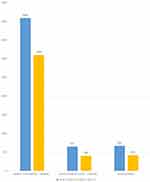
The prevalence rate of Haemophilus influenzae was higher in summer than in other seasons. Meanwhile, Streptococcus pyogenes had a higher prevalence rate in winter and Actinomyces turicensis in autumn, with a statistically significant difference. There was no difference in terms of onset seasons in the prevalence rates among girls with other bacterial infections (Table 3, Figure 3).
 |
Table 3 Season-Wise Prevalence Rates of Vaginitis |
 |
Figure 3 Differences in the distribution of pathogenic bacteria in different seasons. |
Analysis of Vaginitis Duration in Different Bacterial Species
The duration of vaginitis in children infected with Haemophilus influenzae, Streptococcus pyogenes, and Streptococcus pneumoniae was mostly ≤1 week. The duration of disease in girls infected with Streptococcus agalactiae and Actinomyces turicensis was mostly >1 month and ≤1 year, respectively. Girls infected with group G streptococcus had a disease duration of >1 year, with a statistically significant difference. There was no difference in the duration of disease among girls infected with other bacteria (Table 4, Figure 4).
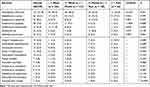 |
Table 4 Duration of Vaginitis |
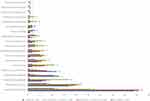 |
Figure 4 Distribution of pathogenic bacterial infections in children with different causes of bacterial vaginitis. |
Analysis of Bacteria in Single and Mixed Infections
There were 399 children with a positive bacterial culture of vaginal secretions, and a total of 419 strains of bacteria were cultured. Additionally, 20 children were infected with 2 kinds of bacteria at the same time. Staphylococcus aureus, Group G Streptococcus, Haemophilus parainfluenzae, and Pseudomonas aeruginosa were prevalent in a higher ratio in girls with mixed infections, with a statistically significant difference. No difference was observed in the percentage of other bacteria in single and mixed infections (Table 5, Figure 5).
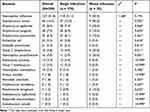 |
Table 5 Prevalence of Different Strains of Bacteria in Single and Mixed Infections |
Analysis of Recurrence in Different Bacteria Species
The analysis of the recurrence rate among girls infected with different bacteria showed a difference in the prevalence of Group F streptococcus in the groups with and without recurrence (P < 0.05). The prevalence of the other bacteria did not differ in girls with recurrence (Table 6, Figure 6).
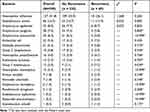 |
Table 6 Comparison of Recurrence Rates in Girls Infected with Different Bacteria |
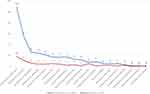 |
Figure 6 Comparison of recurrence rates in children with vaginitis infected with different bacteria. |
Drug Sensitivity Analyses of Bacteria in Vaginal Secretions
The results of drug sensitivity analyses of bacteria showed that Haemophilus influenzae had the highest resistance rate of 50.39% to ampicillin, followed by 49.61% to trimethoprim-sulfamethoxazole, 0.00% to ceftriaxone, meropenem, levofloxacin, and erythromycin, and less than 2.00% to chloramphenicol and tetracycline. A prior study reported that Haemophilus influenzae in vaginal secretions was generally sensitive to amoxicillin in the drug sensitivity analysis.8 However, the resistance rate of Haemophilus influenzae to amoxicillin/clavulanic acid was 14.17% in this study.
Staphylococcus aureus was resistant to penicillin with a rate of up to 89.39%, erythromycin with a rate of 75.21%, and clindamycin with a rate of 65.15%. Conversely, Staphylococcus aureus was highly sensitive to levofloxacin, moxifloxacin, ciprofloxacin, linezolid, and vancomycin, as well as had a resistance rate of below 20% to trimethoprim-sulfamethoxazole, tetracycline, gentamicin. Streptococcus agalactiae, Streptococcus pyogenes, Group F Streptococcus, and Streptococcus pneumoniae were all insensitive to erythromycin and clindamycin with a resistance rate of above 90.00%. Additionally, the resistance rate of Group G Streptococcus to erythromycin and clindamycin was over 89.00%. Streptococcus agalactiae, Streptococcus pyogenes, Group F Streptococcus, and Group G Streptococcus were highly sensitive to ceftriaxone, penicillin, cefepime, vancomycin, and linezolid with a resistance rate of 0. Streptococcus pneumoniae had a resistance rate of more than 50% to tetracycline, penicillin, and trimethoprim-sulfamethoxazole, 0 to amoxicillin, cefepime, moxifloxacin, vancomycin, and linezolid, and 8% to chloramphenicol and meropenem. The resistance rate of Streptococcus agalactiae to levofloxacin was 71.88%, while Streptococcus pneumoniae, Streptococcus pyogenes, Group F Streptococcus, and Group G Streptococcus were not resistant to levofloxacin. Escherichia coli was resistant to ampicillin with a rate of up to 90.91%, followed by trimethoprim-sulfamethoxazole (63.64%), and ciprofloxacin and cefazolin (50%). In addition, Escherichia coli was highly sensitive to amoxicillin, amikacin, and meropenem with a resistance rate of 0 and resistant to aztreonam, ceftazidime, ceftriaxone, and cefuroxime with a rate of less than 20%. Klebsiella pneumoniae had a resistance rate of 100% to ampicillin and no more than 10% to other antibiotics in the drug sensitivity analysis. The resistance rate of Haemophilus haemolyticus was 40% to trimethoprim-sulfamethoxazole and less than 10% to other antibiotics in the drug sensitivity analysis (Table 7).
 |
Table 7 Analysis of Drug Resistance Rate (%) of Common Bacteria Detected in the Vaginal Secretions (Bacterial Culture >10 Strains) |
Discussion
Vulvovaginitis is the most common gynecological disease in prepubertal girls and is gradually increasing in incidence.9,10 In this study, we collected data from 3099 girls with vaginitis who were first-visit patients at the Pediatrics and Gynecology department of Beijing Children’s Hospital, Capital Medical University between 2020 and 2021. There were 399 girls with positive bacterial cultures and a total of 419 strains were detected, which was significantly lower than those in the year 2018 before the COVID-19 epidemic (4089 girls with vaginitis, including 647 girls with positive bacterial cultures and a total of 669 strains)8 (Figure 7).
This phenomenon may be explained by the fact that after the COVID-19 epidemic, children generally wear masks when going out, going to school, and gathering in public places and pay attention to hand hygiene, which greatly reduces the risk of respiratory infections and other infectious diseases, consequently reducing the incidence of vaginitis. Importantly, a European study reported that upper respiratory infections caused by bacterial pathogens are the most common risk factor for vaginitis among girls.11 The data obtained in this study showed that the incidence and positive bacterial culture rate of vaginitis were higher in school-aged girls (≥6 years), 69.93% and 65.91%, respectively, consistent with the findings previously reported by Chinese researchers.12 This result may be attributed to the fact that school-age children go out more frequently than preschool children, increasing the risk of infections. The positive bacterial culture rate was highest in summer at 42.60%, because children are more prone to exposure to a variety of pathogens due to thin clothing and recreational water activities in summer. Several Chinese researchers noted that poor hygiene habits and unclean public places (such as pools and spas) are frequent causes of vulvovaginitis in girls.13–15
Among the 419 strains of bacteria detected in the vaginal secretions of the girls in this study, Haemophilus influenzae ranked first among the pathogenic bacteria in girls with bacterial vaginitis, and this finding is concurrent with foreign literature.16 The rest were Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, Escherichia coli, and Streptococcus pneumoniae, in that order. In 2018, a Beijing Children’s Hospital report detailed the prevalence of bacterial infections among girls with vaginitis,8 and identified the top six infective bacteria as Haemophilus influenzae, Streptococcus pyogenes, Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus parainfluenzae, and Streptococcus agalactiae. Comparison of this with our findings revealed that the results were slightly different, and Haemophilus influenzae, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, and Streptococcus pneumoniae were the most common pathogenic bacteria in girls with vaginitis. Notably, the incidence of Streptococcus pyogenes decreased most markedly after the COVID-19 epidemic, consistent with data previously reported by Chinese scholars.17 The specific causes related to this need to be further investigated. In addition, Haemophilus influenzae is the most widespread cause of bacterial vaginitis in children since it is mainly of respiratory origin.18 Specifically, bacteria of respiratory origin can colonize the vagina due to a lack of attention to personal hygiene or incorrect methods of wiping the vulva in girls, thus resulting in infections. This theory is consistent with the data from the current study that Haemophilus influenzae and Streptococcus pneumoniae were more prevalent in preschool girls (<6 years). In contrast, Staphylococcus aureus and Streptococcus pyogenes were more prevalent in school-age girls (≥6 years).
Our results showed seasonal differences in the rates of pathogenic bacterial infections, with a higher prevalence rate of Haemophilus influenzae in summer and Streptococcus pyogenes in winter. The duration of vaginitis in children infected with Haemophilus influenzae, Streptococcus pyogenes, and Streptococcus pneumoniae was relatively short, mostly ≤1 week. On the contrary, in children infected with Streptococcus agalactiae and Actinomyces turicensis, the duration of disease was mostly >1 month and ≤1 year, respectively. We detected 419 strains of bacteria from the vaginal secretions of 399 girls with bacterial vaginitis, and 20 children were infected with two kinds of bacteria at the same time. Staphylococcus aureus, Group G Streptococcus, Haemophilus parainfluenzae, and Pseudomonas aeruginosa frequently appeared in mixed infections. Our analysis of the recurrence rate of girls with vaginitis infected with different bacteria demonstrated that the recurrence of vaginitis in girls was not related to the type of infective pathogens. In addition, only the distribution of Group F streptococcus differed in the population with and without recurrence, but girls infected with this bacterium were few, and the difference was not statistically significant. The results of drug sensitivity analyses suggest that the resistance rate of clindamycin and erythromycin was generally high, 70–100%, but these drugs are not recommended for clinical use in treating girls with vulvovaginitis. Haemophilus influenzae, Staphylococcus aureus, Streptococcus pyogenes, and Streptococcus pneumoniae, which had a high infection rate, were highly sensitive to levofloxacin. Clinically, levofloxacin eye drops are applied into the vagina of girls for anti-infection and achieved favorable results with relatively few adverse reactions to topical drugs. Amoxicillin is also recommended in several countries as the antibacterial drug of choice for the treatment of girls with vulvovaginitis.19,20 In this study, Escherichia coli, Streptococcus pneumoniae, and Klebsiella pneumoniae had a resistance rate of 0 to amoxicillin, indicating that this could also be used as an empirical drug for girls with vaginitis. Meanwhile, this study revealed that the resistance rate of Haemophilus influenzae to amoxicillin was 14.17%, higher than the resistance rate found in an earlier study. This phenomenon may be related to the long-term widespread clinical use of the drug in recent years, which increases the resistance of the colonized bacteria in vivo to the drug and decreases their sensitivity to antibacterial drugs. A notable finding in this study was that the drug resistance of bacteria in vaginal secretions was found to change when data from the Beijing Children’s Hospital for 2018 and 2020–2021 were compared. For example, the resistance rate of Haemophilus influenzae to some drugs decreased to different degrees after the COVID-19 epidemic. Specifically, its resistance rate to cefuroxime decreased from 29.50% to 29.13%, to ampicillin from 53.64% to 50.39%, to azithromycin from 18.39% to 0, to sulfamethoxazole from 50.96% to 49.61%, and to chloramphenicol from 1.53% to 0.79%. These decreases may be associated with the general attention to protective measures for children and the reductions in infectious diseases and antibiotic use after the COVID-19 epidemic.21
The widespread and irrational use of antimicrobial drugs in the past few years has altered pathogenic bacteria and enhanced drug-resistant strains. This, coupled with the lack of clinical understanding of vaginitis in girls, contributes to the failure to provide accurate and symptomatic treatment for the disease and to curb its prolonged duration, while leading to the emergence of drug-resistant bacteria, thereby resulting in the development of refractory and drug-resistant vaginitis in some girls.22 Therefore, dynamically monitoring the prevalence, change, and drug resistance of pathogenic bacteria is crucial to reliably guide the clinical use of first-line drugs for girls with vulvovaginitis in children.
Conclusion
After the new crown epidemic, children wore masks when going out, going to school, and gathering in public places, and focused on hand hygiene, which greatly reduced the risk of respiratory infections and other infectious diseases, and consequently, the incidence of vaginitis. School-age children (≥6 years) have a higher incidence and positive bacterial culture rate. Summer is the peak incidence of vulvovaginitis in children. The highest rate of infection was with Haemophilus influenzae. Health promotion, cultivation of good personal hygiene habits in girls and avoidance of recurrent respiratory infections are of great value in the prevention of vulvovaginitis.
It is necessary to strengthen clinicians’ understanding of vulvovaginitis in girls, increase the use of bacteria culture tests for detecting pathogenic bacteria in girls with vulvovaginitis, perform drug sensitivity analyses before treatment, select efficient and sensitive antibacterial drugs, and standardize their use to effectively control the infection at the earliest, and reduce the creation of drug-resistant strains.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of the Beijing Children’ s Hospital, Capital Medical University (No. IEC-C-006-A03-V.05), and registered in the Chinese Clinical Trial Register website (http://www.chictr.org.cn/listbycreater.aspx, ChiCTR2000029046, 2020-1-12). A written consent was obtained from legal guardian.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was funded by the National key research and development program (No. 2017YFC1703205).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Itriyeva K. Evaluation of vulvovaginitis in the adolescent patient. Curr Probl Pediatr Adolesc Health Care. 2020;50(7):100836. doi:10.1016/j.cppeds.2020.100836
2. McGreal S, Wood PL. A study of paediatric and adolescent gynaecology services in a British district general hospital. BJOG. 2010;117(13):1643–1650. doi:10.1111/j.1471-0528.2010.02724.x
3. Shi YF, Zhu XQ. Pediatric and Adolescent Gynecology. Beijing: Science Press; 2019:125–146.
4. Kosová H. Disorders of vulva and vagina in children and adolescent. Cas Lek Cesk. 2018;157(7):354–357.
5. Sianou A, Galyfos G, Moragianni D, Baka S. Prevalence of vaginitis in different age groups among females in Greece. J Obstet Gynaecol. 2017;37(6):790–794. doi:10.1080/01443615.2017.1308322
6. Yilmaz AE, Celik N, Soylu G, Donmez A, Yuksel C. Comparison of clinical and microbiological features of vulvovaginitis in prepubertal and pubertal girls. J Formos Med Assoc. 2012;111(7):392–396. doi:10.1016/j.jfma.2011.05.013
7. Loveless M, Myint O. Vulvovaginitis- presentation of more common problems in pediatric and adolescent gynecology. Best Pract Res Clin Obstet Gynaecol. 2018;48:14–27. doi:10.1016/j.bpobgyn.2017.08.014
8. Pan YC, Liu J, Lui HL, Zhang M. Etiology and drug resistance analysis of vulvovaginitis in children.International. J Lab Med. 2020;41(18):2198–2202. doi:10.3969/j.issn.1673-4130.2020.18.006
9. Romano ME. Prepubertal Vulvovaginitis. Clin Obstet Gynecol. 2020;63(3):479–485. doi:10.1097/GRF.0000000000000536
10. Cemek F, Odabaş D, Şenel Ü, Kocaman AT. Personal hygiene and vulvovaginitis in prepubertal children. J Pediatr Adolesc Gynecol. 2016;29(3):223–227. doi:10.1016/j.jpag.2015.07.002
11. Cuadros J, Mazón A, Martinez R, et al. The aetiology of paediatric inflammatory vulvovaginitis. Eur J Pediatr. 2004;163(2):105–107. doi:10.1007/s00431-003-1373-x
12. Gao KJ, Yang JW, Fang PP, et al. Analysis of pathogenic bacteria and drug resistance of vulvovaginitis in 319 children. Chin J Integr Med. 2021;46(10):958–963. doi:10.13461/j.cnki.cja.007048
13. Zhang TL, Yi NH. Clinical analysis of 60 cases of youngest daughter with vulvovaginitis. Chin J Women Child Health. 2015;6(05):66–68. doi:10.19757/j.cnki.issn1674-7763.2015.05.021
14. Gao CZ, Zhao JC, Cao YY. Analysis of related factors of youngest daughter with vulvovaginitis. Proceeding Clin Med. 2018;27(02):
15. Zuckerman A, Romano M. Clinical Recommendation: vulvovaginitis. J Pediatr Adolesc Gynecol. 2016;29(6):673–679. doi:10.1016/j.jpag.2016.08.002
16. Li JP, Hua CZ, Sun LY, Wang HJ, Chen ZM, Shang SQ. Epidemiological features and antibiotic resistance patterns of haemophilus influenzae originating from respiratory tract and vaginal specimens in pediatric patients. J Pediatr Adolesc Gynecol. 2017;30(6):626–631. doi:10.1016/j.jpag.2017.06.002
17. Fang C, Zhou Z, Zhou M, Li J. Decrease in incidence of Streptococcus pyogenes-induced vulvovaginitis among prepubertal girls after COVID-19 outbreak. Infect Dis. 2022;54(12):947–950. doi:10.1080/23744235.2022.2109726
18. Hansen MT, Sanchez VT, Eyster K, Hansen KA. Streptococcus pyogenes pharyngeal colonization resulting in recurrent, prepubertal vulvovaginitis. J Pediatr Adolesc Gynecol. 2007;20(5):315–317. doi:10.1016/j.jpag.2006.12.001
19. Tartaglia E, Giugliano B, Ucciferri C, et al. Vulvo-vaginitis in prepubertal girls: new ways of administering old drugs. J Pediatr Adolesc Gynecol. 2013;26(5):277–280. doi:10.1016/j.jpag.2013.05.003
20. Bayer C, Parks L. Vulvovaginal Complaints. Curr Treat Options Pediatr. 2016;2(3):209–215. doi:10.1007/s40746-016-0062-8
21. Wang YP, Tang CX, Han MH, et al. Temporal trend of antibiotic use among primary school children in Shanghai, 2017–2020. Chin J Prev Med. 2022;56(06):843–846. doi:10.3760/cma.j.cn112150-20210709-00663
22. Chen X, Zhao X, Chen L, Zeng W, Haiou X. Vaginitis Caused by Corynebacterium amycolatum in a Prepubescent Girl. J Pediatr Adolesc Gynecol. 2015;28(6):e165–7. doi:10.1016/j.jpag.2015.03.008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.