Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 6
Analysis of factors affecting rehospitalization of patients with chronic kidney disease after educational hospitalization
Authors Kose E, An T, Kikkawa A, Matsumoto Y, Hayashi H
Received 12 November 2013
Accepted for publication 31 December 2013
Published 8 April 2014 Volume 2014:6 Pages 71—78
DOI https://doi.org/10.2147/CPAA.S57442
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Eiji Kose,1 Taesong An,2 Akihiko Kikkawa,2 Yoshiaki Matsumoto,3 Hiroyuki Hayashi1
1Department of Pharmacotherapy, School of Pharmacy, Nihon University, Funabashi, 2Yokosuka Kyousai Hospital, Yokosuka, 3Department of Clinical Pharmacokinetics, School of Pharmacy, Nihon University, Funabashi, Japan
Background: Chronic kidney disease (CKD) is associated with a high risk of cardiovascular disease complications. Therefore, medical institutions conduct educational hospitalization for early treatment and education of CKD patients. However, patients who have been discharged after achieving educational targets can end up showing poor symptoms at home. There also have been several cases of rehospitalization or disease aggravation. In this study, we analyzed rehospitalized patients who were discharged from the hospital after CKD educational hospitalization and investigated the purpose of analyzing rehospitalization factors.
Materials and methods: This was an observational case-control study conducted at Yokosuka Kyousai Hospital. We performed univariate analysis using patient background features and laboratory data between a rehospitalization group and a no-rehospitalization group. Next, we performed multiple logistic regression analysis using the results of the univariate analysis.
Results: From the results of this study, we identified independent risk factors, such as serum albumin level, heart-failure complications, and estimated glomerular filtration rate (eGFR). Moreover, the serum Alb level was identified as the most important risk factor for rehospitalization. Therefore, we considered that it is important to live a life that makes it possible to maintain CKD stage G3b for a long time after discharge, because the cutoff level of eGFR is 31 mL/minute/1.73 m2.
Conclusion: We believe that it is important to educate patients, their families, and medical staff on the importance of early detection and treatment, and we consider that this approach is important to inclusively protect the kidney.
Keywords: albumin, glomerular filtration rate, cardiovascular disease, stages of chronic kidney disease
Introduction
The number of patients with chronic kidney disease (CKD) in Japan is approximately 13,300,000, and continues to increase. It is reported that these patients constitute approximately 13% of the adult population. In addition, the number of end-stage kidney disease (ESKD) patients, ie, patients in whom CKD had deteriorated and required dialysis, increased by ≥7,000 annually. At the end of 2011, the number of maintenance-dialysis patients surpassed 300,000 for the first time, and continues to increase.1 There are many cases without subjective symptoms in the early stage of CKD.2 If left untreated, the condition progresses gradually. After that, renal failure takes place and dialysis becomes necessary. In addition, CKD has been suggested as an important risk factor for cardiovascular disease (CVD). It has been reported that it significantly increases the incidence rates of coronary heart disease in the men and cerebral infarction in the women of Hisayama, a town in Fukuoka Prefecture, Japan.3
CKD increases the burden on patients. It also poses serious problems from the medical and economic viewpoints.4 In contrast, the progression of CKD can be inhibited and improved by early detection or early treatment. Therefore, it is very important to detect and treat CKD early to delay its progression. The participation of patients and their families in the treatment is necessary to delay the progression of CKD. Moreover, we consider that early detection or early treatment is necessary to protect the kidney comprehensively. Therefore, medical institutions in Japan should conduct “educational hospitalization” to promote early treatment of CKD patients. Educational hospitalization means that CKD patients who are not yet suffering ESKD are hospitalized for the purpose of suppressing progress of the disease as much as possible for around 1–2 weeks. Health care workers in various fields, such as doctors, nurses, pharmacists, and nutritionists, educate patients on how to deal with CKD during educational hospitalization. This educational system approach is generally conducted in Japan. However, this system may differ from other educational systems, because medical systems and insurance regimes differ between Japan and other countries. Patients can maintain their quality of life through this educational hospitalization, and can hope for a lifestyle similar to that of individuals without CKD. However, a patient who has achieved his/her educational target may still have poor compliance at home following his/her discharge from the hospital. We believe that certain characteristics of patients and factors for rehospitalization are involved in the aggravation of CKD. However, there are very few reports that have analyzed factors for rehospitalization. There have been no reports related to the follow-up of CKD patients after their hospitalization for educational purposes in Japan. Therefore, in this study, we examined nonrehospitalized patients for comparison to determine the factors for rehospitalization of patients after initial CKD educational hospitalization.
Summary of educational hospitalization
There are three purposes of educational hospitalization: 1) learning how to deal with kidney disease, 2) slowing the progression of renal function disorder, and 3) preventing the onset of CVD.
We determined the educational topics with the help of doctors and nurses. The topics were: 1) kidney function, 2) how to interpret laboratory data, 3) pharmacological treatment of CKD, 4) nutritional management of CKD, and 5) renal replacement therapy (hemodialysis and peritoneal dialysis). The patients were instructed about these five topics by the aforementioned health care workers during hospitalization. Of these topics, the pharmacist was in charge of topic 3. Our goals were to make the patient understand the need for medicines and the necessity to take these medicines properly. In addition, we prepared a brochure about therapeutic drugs used in kidney disease to improve the knowledge of patients of the medicines. We instructed the patients during educational hospitalization that a follow-up could be conducted at any time.
Materials and methods
How to categorize rehospitalization and no rehospitalization
We categorized patients who were rehospitalized at least once within 1 year after discharge from educational hospitalization in the rehospitalization group. We categorized patients who satisfied all the following conditions in the no-rehospitalization group: 1) not rehospitalized within 1 year after discharge from educational hospitalization, 2) visiting Yokosuka Kyousai Hospital for treatment >6 months before and after hospitalization, 3) availability of data on renal function for continuous analysis. We analyzed the following items in both groups. The data of patients in the rehospitalization group collected at the time of the rehospitalization were used. If there were patients who were rehospitalized more than once, we used the data obtained at their first rehospitalization after discharge from educational hospitalization. The data collected at the first outpatient department visit after discharge from educational hospitalization were used in the no-rehospitalization group.
Investigation items
The factors examined as patients’ background features were sex, age, body mass index, number of oral medicines, CKD stage, primary disease (eg, diabetes mellitus, nephrotic syndrome), number of metabolic syndrome (MetS) configuration factors, and complications (eg, heart failure or nephrogenic anemia). The laboratory data included levels of total protein, albumin (Alb), C-reactive protein (CRP), hemoglobin (Hb), glycated Hb (HbA1c), blood glucose (BG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), triglyceride, K, Ca, P, Ca × P, blood urea nitrogen (BUN), serum creatinine (SCr), and serum uric acid (SUA). Estimated glomerular filtration rate (eGFR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse pressure were also collected. In addition, we determined the number of times that patients were instructed by a pharmacist and a nutritionist as instruction-related items. We also determined about preserve of absence of spouse and family members as the home environment. We analyzed data obtained during educational hospitalization as instruction-related items and home-environment data. We defined the MetS configuration factors as diabetes mellitus, hypertension, hyperlipidemia, and history of smoking.
Subjects
We recruited 105 patients who were discharged after hospitalization for CKD educational purposes in Yokosuka Kyousai Hospital Nephrology Department from March 2011 to October 2012. We excluded 28 patients with CKD at stages G2 and G5 and patients whose data were not available for investigation. Therefore, finally, we had 77 patients (rehospitalization group, 20; no-rehospitalization group, 57) with CKD at stages G3a, G3b, and G4. This study complied with the Declaration of Helsinki and the Japanese Ministry of Health, Labour and Welfare’s “Ethical guidelines for clinical studies.”
In addition, the stages of CKD are classified from stage G1 to G5 on the basis of renal function (GFR): G1, GFR >90 mL/minute/1.73 m2; G2, GFR 60–89 mL/minute/1.73 m2; G3a, GFR 45–59 mL/minute/1.73 m2; G3b, GFR 30–44 mL/minute/1.73 m2; G4, GFR 15–29 mL/minute/1.73 m2; and G5, GFR <15 mL/minute/1.73 m2. The disease severity of CKD is shown by a combination of GFR and albuminuria.
Statistical analysis
The results are presented as means ± standard deviation. We performed the normality test to compare the data volume between the two groups. We used Student’s t-test after we confirmed that the data showed a normal distribution. We used the Mann–Whitney U test when the data did not show a normal distribution. We used the χ2 test or Fisher’s exact test to compare the categorical data. Next, we adjusted for the confounder, and we performed multiple logistic regression analysis with the presence or absence of rehospitalization as a dependent variable to investigate the relationships among rehospitalization, patient background, laboratory data, instruction-related items, and home environment. We chose significant factors as independent variables on the basis of the results of univariate analysis. We chose factors that were reported to be associated with the progression of CKD5–7 from factors whose P-values were small. We incorporated MetS configuration factors into regression equations compulsorily. None of the data on eGFR, Alb, or MetS configuration factors showed a normal distribution. Therefore, we calculated a cutoff level by receiver operating-characteristic analysis. As a result, the following were determined as cutoff levels: eGFR, 31 mL/minute/1.73 m2; serum Alb level, 3.5 g/dL; and MetS configuration factor, 2. We performed multiple logistic regression analysis using values obtained from the receiver operating-characteristic analysis. We confirmed using multiple logistic regression analysis that there was no multicollinearity between factors using Pearson’s correlation coefficient or Spearman’s rank-correlation coefficient. The significance level was 5% (P<0.05). In addition, statistical analysis was performed using JMP® (version 10; SAS Institute, Cary, NC, USA).
Ethics regulation
This study was conducted with the approval of the Yokosuka Kyousai Hospital ethics committee (approval number 12-18). This was a retrospective study using medical records.
Results
Subject background
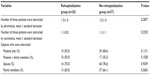
Table 1 shows the results of comparison of subject-background features between the rehospitalization (male 13; female, 7) and no-rehospitalization groups (male, 31; female, 26). There were no significant differences in sex, age, weight, body mass index, CKD stage, or nephrotic syndrome between the two groups. The numbers of oral medicines used by the rehospitalization group and no rehospitalization group were 10.1±2.3 and 7.5±3.4, respectively which were significantly different. Similarly, we compared the percentage of patients with a primary disease (diabetes mellitus), MetS configuration factors, and the percentage of patients with complications, such as heart failure and nephrogenic anemia, between both groups. As a result, in the rehospitalization and no-rehospitalization groups, diabetes mellitus was noted in 75.0% and 33.3% of patients, MetS configuration factors in 2.9±0.9 and 1.7±1.4 patients, heart-failure complications in 55.0% and 7.1% patients, and nephrogenic anemia complications in 25.0% and 5.4% patients, respectively. These data showed significantly higher values in the rehospitalization group.
Comparison of laboratory data
Table 2 shows the results of comparison of laboratory data between the rehospitalization and no-rehospitalization groups. Serum Alb levels were 3.0±0.8 g/dL and 3.9±0.8 g/dL, respectively. Serum Alb levels were significantly lower in the rehospitalization group than that in the no-rehospitalization group. Similarly, we compared the Hb level, Ca level, and eGFR between both groups. As a result, in the rehospitalization and no-rehospitalization groups, Hb levels were 10.1±1.3 g/dL and 12.1±1.8 g/dL, Ca levels were 8.3±0.5 mg/dL and 9.1±0.4 mg/dL, and eGFR was 23.4±14.3 mL/minute/1.73 m2 and 39.1±13.9 mL/minute/1.73 m2, respectively. These data showed significantly lower values in the rehospitalization group. We also compared HbA1c levels between both groups, and found that HbA1c levels were significantly higher (6.1±0.8 g/dL) in the rehospitalization group than in the no-rehospitalization group (5.5±0.8 g/dL). Similarly, we compared BG, LDL-C, Ca × P, BUN, SCr, SUA, SBP, and DBP levels between the rehospitalization and no-rehospitalization groups. This comparison revealed the following results: BG levels, 148.4±57.8 mg/dL and 109.9±47.2 mg/dL; LDL-C levels, 117.1±45.7 mg/dL and 100.4±30.4 mg/dL; Ca × P levels, 35.2±10.9 mg/dL2 and 30.1±6.9 mg/dL2; BUN levels, 48.2±24.6 mg/dL and 24.4±10.7 mg/dL; SCr levels, 2.7±1.6 mg/dL and 1.7±0.6 mg/dL; SUA levels, 8.0±2.0 mg/dL and 6.4±1.7 mg/dL; SBP levels, 144.9±20.8 mmHg and 127.2±15.4 mmHg; and DBP levels, 80.5±17.0 mmHg and 74.2±11.2 mmHg, respectively. These data showed significantly higher values in the rehospitalization group. In contrast, no significant differences were observed in total protein, CRP, HDL-C, TC, triglyceride, K, P, or pulse-pressure levels between the groups.
Comparison of instruction-related items and home environment
Table 3 shows the results of comparison of instruction-related items and home environment between the rehospitalization and no-rehospitalization groups. No significant differences were noted in the number of times the patients were instructed by a pharmacist and nutritionist between the groups. In addition, we divided the patients into a patients-only group and a patients + family group on the basis of subjects who were instructed, and compared these groups. As a result, no significant difference in subjects who were instructed was noted between the groups. Next, we divided the patients on the basis of home environment into the spouse group and the patients + family group, and compared these groups. As a result, no significant difference in home environment was noted between the groups according to these results.
  | Table 3 Comparison of instruction-related items and home environment between rehospitalization group and no-rehospitalization group |
Multiple logistic regression analysis
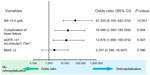
We analyzed all 77 patients using multiple logistic regression analysis of various factors associated with rehospitalization. As a result, significant differences were observed among Alb level of <3.5 g/dL, heart-failure complications, and eGFR of <31 mL/minute/1.73 m2. We have listed the results in a forest plot in Figure 1.
Discussion
The most valuable finding of this study was that the serum Alb level of rehospitalization patients was the most important risk factor for rehospitalization. In addition, we revealed that the heart-failure complications and eGFR of <31 mL/minute/1.73 m2 were new risk factors. These radically new findings on factors for rehospitalization after CKD educational hospitalization were noted. Decrease in serum Alb level leads to malnutrition and sthenic inflammatory response. Therefore, we believe that it is necessary to instruct CKD patients with more focus on infections and nutritional management. In addition, we should intervene positively to halt further progression of eGFR after educational hospitalization. Furthermore, we consider that it is necessary to monitor factors revealed in this study as surrogate markers with time. There are only a few reports about the risk factor for rehospitalization in Japan.8–10 There are few reports that serum Alb level is a factor associated with rehospitalization.10 However, our results were similar to previous studies.
CKD is a disease whose aggravation due to complications can be inhibited by pharmacotherapy, acquisition of knowledge in pathology, and improvement of lifestyle factors, such as proper diet or exercise. Educational hospitalization of CKD patients is a measure that inhibits its aggravation.11 Patients can obtain knowledge necessary for lifestyle improvement and prevention of aggravation by CKD educational hospitalization. Moreover, patients can continue leading a social life by managing their lifestyle on their own. However, some patients who have accomplished their educational target may show poor compliance at home following their discharge from the hospital. Therefore, in this study, we analyzed the characteristics and conditions of patients at the time of educational hospitalization of rehospitalized patients. Moreover, we examined nonrehospitalized patients to determine factors leading to the rehospitalization of patients after the initial CKD educational hospitalization.
In this study, serum Alb level was the most important risk factor for rehospitalization. It is also a marker used as a nourishment index of patients. In general, a serum Alb level of 3.5 g/dL or lower indicates malnutrition.12 Therefore, we speculated on the cause of the significantly low serum Alb levels in the rehospitalization group. We considered the possibility that the main conservative treatment of CKD is a low-protein diet, which may have led to this decrease. However, BUN reflecting dietary intake or protein content, serum P level, and serum K level decrease were not noted in either group. In addition, similar results were noted for TC level, which is an index of protein-energy wasting. In other words, we suggest that the decrease in serum Alb level was a secondary change in this study. However, we believe that it is necessary to examine this in detail in future studies.
We also believe that an increase in CRP level may be associated with a decrease in serum Alb level. Hypoalbuminemia is recognized as being strongly associated with inflammation. CRP level is a determinant factor for Alb level.13 In this study, a significant negative correlation (r=−0.4386, P=0.0003) was noted between serum Alb levels and CRP levels. This finding supports the results of a previous study.14 Therefore, it was considered that the decrease in serum Alb levels in the rehospitalization group was caused by the increase in CRP levels. The following studies are informative regarding the reason CRP levels increase in patients with CKD. Sato reported that diabetes mellitus complications increase the risk of hospitalization due to bacterial infections in CKD patients.15 Koziel and Koziel16 and McMahon and Bistrian17 reported that the morbidity of respiratory tract infection or urinary tract infection is higher in high-blood sugar or diabetic patients than in healthy individuals. In this study, the percentage of patients who had diabetes mellitus as the primary disease in the rehospitalization group was 75.0%, which was significantly higher than that in the no-rehospitalization group. CRP levels were significantly higher in the rehospitalization group (2.3±4.8 mg/dL) than in the no-rehospitalization group (0.1±0.1 mg/dL) (P=0.0016). Therefore, we hypothesize that the increase in CRP levels in the rehospitalization group was caused by increases in inflammatory cytokine levels because of an infection.
We revealed factors for heart-failure complications, and an eGFR of <31 mL/minute/1.73 m2 is another risk factor. The rate of patients with heart-failure complications in the rehospitalization group was 55.0%, significantly higher than in the no-rehospitalization group. We considered that the effects of enhancing the renin–angiotensin system due to the progression of renal function disorder, blood pressure elevation due to fluid retention, and aggravation of arteriosclerosis was associated with heart-failure complications in the rehospitalization group.
The number of medical conditions causing MetS has been reported as one of the factors for renal function decreases.18 MetS is defined as the disease concept that “hypertension, diabetes mellitus, and hyperlipidemia happens as a result of fat accumulated in the internal organs by overeating and lack of exercise”. In this study, we identified smoking history as another factor for these diseases. However, multiple logistic regression analysis did not show MetS configuration factors as a risk factor. However, Ninomiya et al reported that CKD progresses as the number of diseases associated with MetS increases.19 In other words, if patients could correct their lifestyle, the decrease in eGFR may be controlled, which in turn may lead to a decrease in the rate of rehospitalization. Therefore, it is considered that the expectations from the pharmacist, who teaches the significance of taking medicines to patients, and from the nutritionist, who enhances the dietary habit of patients, are significant. Therefore, in this study, we also determined the effects of the number of times patients were instructed by both the pharmacist and nutritionist and subjects who were instructed on rehospitalization. As a result, there was no significant difference in the number of times patients were instructed and subjects who were instructed between both groups. Therefore, it was considered that it was necessary to increase the quality of instruction content rather than repeating these instructions. The instruction of patients by the pharmacist and nutritionist during the educational hospitalization tended to be monotonous, and the contents were also often undifferentiated. Therefore, it is necessary to explain fully the significance of taking medicines and correction of lifestyle, and we should tailor the method of instruction according to individual patients. Review of the educational program is also considered necessary.
The problems of this study are as follows. It was a section investigation within a single facility. There was a small number of patients who underwent educational hospitalization. In addition, we should also have evaluated urinary protein level, data on nutritional supplements, or drug compliance as indicators of the risks of CKD progression and CVD development. However, we were unable to investigate these data in this study. Therefore, it is possible that these factors had an effect on the results of this study. We consider that it is necessary to improve educational programs and administer them in multiple facilities to investigate factors for rehospitalization of patients universally.
We identified a serum Alb level of <3.5 g/dL, heart-failure complications, and an eGFR of <31 mL/minute/1.73 m2 as factors that cause the rehospitalization of CKD patients after initial educational hospitalization. In other words, we considered that it is important to live a lifestyle that makes it possible to maintain stage G3b for a long time after discharge, because the cutoff level of eGFR was 31 mL/minute/1.73 m2. Keith et al compared the incidence and mortality rates of ESKD according to renal function level in the general American population. As a result, the mortality and incidence rates of ESKD in stage G4 were noted to be several times higher than those in stages G3a and G3b, respectively.6 Furthermore, it is necessary to initiate renal replacement therapy, such as dialysis and combined modality therapy, to inhibit the deterioration of renal function in stage G4. Therefore, we considered that it is very important to inhibit the progression of renal function disorder to stage G3b in terms of quality of life for patients.
Conclusion
We believe that it is important to educate patients, their families, and medical staff on the importance of early detection and treatment, and we believe that it is necessary to protect the kidney inclusively for a good prognosis. It is important to minimize decrease in renal function and inhibit decrease in serum Alb level to inhibit CKD progression and decrease the incidence of CVD. Moreover, we consider that appropriate drug management focusing on angiotensin-converting enzyme-inhibitor or angiotensin II receptor-blocker medicines is important.
Disclosure
The authors report no conflicts of interests in this work.
References
Nakai S, Watanabe Y, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of December 31, 2011). Ther Apher Dial. 2013;17:567–611. | |
Kimura K. [Methylarginies-induced endothelial dysfunction in chronic kidney disease]. Yakugaku Zasshi. 2012;4:443–448. Japanese. | |
Ninomiya T, Kiyohara Y, Kubo M, et al. Chronic kidney disease and cardiovascular disease in a general Japanese population: the Hisayama Study. Kidney Int. 2005;68:228–236. | |
Lysaght MJ. Maintenance dialysis population dynamics: current trends and long-term implications. J Am Soc Nephrol. 2002;13:S37–S40. | |
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–2081. | |
Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;6:659–663. | |
Iseki K, Asahi K, Moriyama T, et al. Risk factor profiles based on estimated glomerular filtration rate and dipstick proteinuria among participants of the Specific Health Check and Guidance System in Japan 2008. Clin Exp Nephrol. 2012;16:244–249. | |
Saito M, Yanagihori A, Yamada T, et al. [Examination of the risk factors associated with heart failure rehospitalization after heart surgery]. J Jpn Assoc Card Rehabil. 2008;13:96–99. Japanese. | |
Tabata M, Nakagawa S, Ui S, Mitamura H. [Examination of the factors affecting the hospitalization rehabilitation period of rehospitalized chronic heart failure patients by multiplex logistic analysis]. J Jpn Assoc Card Rehabil. 2008;13:88–91. Japanese. | |
Kitamura Y, Kobara Y, Nakano H, et al. [Which factors contribute to early hospital readmission? The significance of serum albumin level at discharge]. J Jpn Soc Parenter Enteral Nutr. 2009;24:77–81. Japanese. | |
Yamaji K, Kurusu A, Okamoto M, Sekiguchi Y, Horikoshi S, Tomino Y. Effect of educational hospitalization on chronic kidney disease (CKD) patients. Clin Nephrol. 2007;6:401–404. | |
Kita E, Itoh H, Someya H, et al. [The relevance between serum albumin and age; investigation in acute period hospitals]. J Jpn Soc Parenter Enteral Nutr. 2010;25:63–70. Japanese. | |
Kaysen GA, Chertow GM, Adhikarla R, Young B, Ronco C, Levin NW. Inflammation and dietary protein intake exert competing effects on serum albumin and creatinine in hemodialysis patients. Kidney Int. 2001;60:333–340. | |
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–454. | |
Sato T. [Risk factors for bacterial infection-related hospitalization in chronic kidney disease (CKD) patients]. J Saitama Med Univ. 2013;39:105–112. Japanese. | |
Koziel H, Koziel MJ. Pulmonary complications of diabetes mellitus. Pneumonia. Infect Dis Clin North Am. 1995;9:65–96. | |
McMahon MM, Bistrian BR. Host defenses and susceptibility to infection in patients with diabetes mellitus. Infect Dis Clin North Am. 1995;9:1–9. | |
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6:2364–2373. | |
Ninomiya T, Kiyohara Y, Kubo M, et al. Metabolic syndrome and CKD in a general Japanese population: the Hisayama Study. Am J Kidney Dis. 2006;48:383–391. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.