Back to Journals » International Journal of General Medicine » Volume 15
Analysis of Clinical Characteristics of Connective Tissue Disease-Associated Interstitial Lung Disease in 161 Patients: A Retrospective Study
Authors Lu M, Gong L, Huang C, Ye M, Wang H, Liu Y, Liu D
Received 29 September 2022
Accepted for publication 5 December 2022
Published 15 December 2022 Volume 2022:15 Pages 8617—8625
DOI https://doi.org/10.2147/IJGM.S391146
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Luca Testarelli
Mingjie Lu,1,* Ling Gong,1,* Chengyan Huang,1 Meng Ye,2 Hongping Wang,3 Yi Liu,3 Daishun Liu3
1Department of Respiratory Medicine, The Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi), Zunyi, Guizhou, 563000, People’s Republic of China; 2Scientific Research Center, The Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi), Zunyi, Guizhou, 563000, People’s Republic of China; 3Zunyi Medical University, Zunyi, Guizhou, 563000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Daishun Liu, Zunyi Medical University, No. 6 Xuefu West Road, Xinpu New District, Zunyi, Guizhou, 563000, People’s Republic of China, Email [email protected]
Objective: This study was conducted to retrospectively analyze the clinical characteristics of CTD-ILD patients to provide strategies for clinical management.
Methods: This study collected and analyzed the clinical data and relevant examination results of 161 patients diagnosed with CTD-ILD between 01 January 2018 and 01 January 2021.
Results: A total of 161 CTD-ILD patients, 74.53% were females and 25.47% were males, 32.92% were elderly and 67.08% were non-elderly. The main clinical symptoms of CTD-ILD patients were cough (44.72%), decreased activity tolerance (40.37%). RA-ILD was the most common one in the non-elderly and the elderly CTD-ILD patients (48.15% and 50.94%, respectively). Compared with non-elderly, elderly patients with CTD-ILD had a longer duration of CTD (p=0.04). However, fatigue (p=0.005), activity tolerance (p=0.029), the incidence of pulmonary diffusion dysfunction (p=0.047), and systemic immunoinflammatory index (SII, p=0.014) (platelet × NLR) were all decreased. The standard deviation of red blood cell distribution width (RDW) (p=0.024) and immunoglobulin (IgA) (p=0.033) was significantly increased. The smoking index was significantly higher in men than in women with CTD-ILD (p=0.000), but symptoms of reduced activity tolerance were less pronounced than in women (p< 0.05). Elderly CTD-ILD patients (p=0.003) and women from non-elderly patients were prone to lower hemoglobin (p=0.000). Among the elderly, the lymphocyte ratio was more significantly elevated in female CTD-ILD patients than in males (p=0.018). In contrast, neutrophil to lymphocyte ratio (NLR) and SII were lower in female (p=0.038) than in male CTD-ILD patients (p=0.043).
Conclusion: CTD-ILD mainly affects non-elderly and women. Age may not be involved with decreased activity tolerance and increased lung function impairment in CTD-ILD patients. However, the elderly patients with CTD-ILD, especially the elderly female patients with low inflammation levels and high immune disorders, have a poor prognosis.
Keywords: CTD-ILD, rheumatoid arthritis, pulmonary functions, clinical characteristics
Introduction
Connective tissue-associated interstitial lung disease (CTD-ILD) is a disease that results from the association of lungs with connective tissue diseases such as systemic lupus erythematosus (SLE), polymyositis (PM)/dermatomyositis (DM), systemic sclerosis (SSc), rheumatoid arthritis (RA), and sjögren’s syndrome (SS), etc. CTD-ILD patients have a significantly lower 10-year survival time and higher risk of death, and an insidious and heterogeneous onset compared to the CTD patients alone.1–4 The average survival time for CTD-ILD patients is only 6.5 years, as reported in the literature.5,6 Pulmonary involvement varies among patients with CTD-ILD, with up to 80% involvement in RA.7–9 SSc-ILD has a prevalence of 30–90%10,11 with a 10-year mortality rate of up to 40%.12,13 In addition, the prevalence of CTD-ILD in the elderly is increasing with age, progressive reduction in chest wall compliance, muscle strength, disease-induced inflammation, autophagy, mitochondrial dysfunction, and decreased lung function, among many other reasons. However, the current prevalence and clinical features of CTD-ILD in the elderly are unknown. This leads to a more challenging diagnosis and treatment of CTD-ILD in the elderly, thus burdening global health resources.
Therefore, the aim of this study is to retrospectively analyze and summarize the clinical characteristics of 161 patients with CTD-ILD as well as to analyze and compare the characteristics of CTD-ILD in non-elderly and elderly patients, and CTD-ILD in different genders. This study may provide important evidence and strategies for clinical diagnosis and treatment of CTD-ILD.
Subjects and Methods
Subjects
The study population included CTD-ILD-diagnosed patients hospitalized in the Department of Rheumatology and Immunology in the Third Affiliated Hospital of Zunyi Medical University from 01 January 2018 to 01 January 2021. Before the start of the study, the patients included in the study provided written informed consent, and this study was approved by the Ethics Committee of the Third Affiliated Hospital of Zunyi Medical University and was conducted in accordance with the Declaration of Helsinki-1964. The inclusion criteria were ① meeting the diagnostic criteria of CTD; ② the presence of interstitial lung lesions such as honeycomb lung, grid shadow, ground glass shadow, distended bronchial dilation, subpleural solid shadow, and other features confirmed by chest high-resolution computer tomography (HRCT). Those patients with combined lung tumors, pneumoconiosis, nodular disease, tuberculosis, pulmonary edema, pulmonary atelectasis, and pulmonary embolism were excluded. The basic information, clinical manifestations, serological indices, blood gas analysis, and clinical data of pulmonary functions were collected from the included patients. In this study, participants with an age group ≥65 years were used as the boundary to differentiate elderly and non-elderly groups. CTD-ILD patients were included in this study at first diagnosis of ILD. First hospitalization data was used for patients with multiple hospitalization experiences.
Methods
Observation Indicators
Basic information such as age, gender, smoking history, smoking index (number of cigarettes smoked per day×number of years smoked) were recorded. Clinical manifestations such as cough, expectoration, hemoptysis, chest tightness and pain, activity, fever, fatigue, cold history and velcro rales were also noted. The auxiliary examination included serological indicators, pulmonary function, and blood gas analysis.
Different CTD-ILD Definitions
ILD refers to a large group of diffuse diseases that are caused by different reasons and involve the alveoli, alveolar walls, bronchioles, microvessels, etc. The definitions of different CTD involved in this study are as follows. Antineutrophil cytoplasmic antibody (ANCA) associated vasculitis is characterized by systemic small vasculitis and the presence of ANCA in the circulation. PM/DM is autoimmune disease with muscle weakness and myalgia, which affects skeletal muscle, skin and other organs. SS is an autoimmune disease caused by lymphocyte infiltration of lacrimal gland and salivary gland, mainly manifested as keratoconjunctivitis and xerostomia characterized by dryness. RA is a systemic disease characterized by chronic, mainly inflammatory synovitis. SLE is an autoimmune inflammatory connective tissue disease involved multiple organs. SSc is an immune rheumatic disease characterized by localized or diffuse skin thickening and fibrosis. Interstitial pneumonia with autoimmune features (IPAF) means that a large number of ILD patients show autoimmune characteristics, but it does not meet the diagnostic criteria for CTD. Overlapping syndrome (OS) is the occurrence of two or more kinds of CTDs in the same patient.
Statistical Analysis
SPSS 22.0 software was used for statistical analysis. Tested data satisfying normal distribution for continuous variables were expressed as mean ± standard deviation (x ± s), and continuous data not satisfying normal distribution were expressed as median ± interquartile range (M ± IQR). Count data were expressed as the number of cases and percentages. Differences between the two groups were analyzed using the independent samples t-test for continuous variables whose tested data met normal distribution. The rank sum test was used for continuous variables with skewed distribution, and the x2 or Fisher’s statistic for categorical data to compare differences. Differences were considered statistically significant at p<0.05.
Results
Baseline Data
Among the 161 CTD-ILD patients, 120 were female (74.53%), and 41 (25.47%) were male, with a male-to-female ratio of 1:2.93. Amongst these, 53 were elderly (mean age 70.57±4.03 years, male to female ratio 1:2.31), and 108 non-elderly patients (mean age 52.00±11.50 years, male to female ratio 1: 3.32). Among the 161 CTD-ILD patients, 79 (49.07%) had RA-ILD, 17 (10.56%) had SS-ILD, 15 with the OS-ILD (9.32%), 14 cases (8.70%) with PM/DM-ILD, 12 cases (7.45%) with IPAF-ILD, 8 cases (4.97% each) with SSc-ILD and SLE-ILD, 4 cases (2.48%) of ANCA-ILD. Moreover, 2 cases (2.48%) of others (mixed connective tissue-related lung disease in 2 cases, diffuse 1 case of eosinophilic fasciitis-related pulmonary disease, and 1 case of diffuse connective tissue disease-related interstitial pneumonia). In non-elderly CTD-ILD, the common ones were RA-ILD and PM/DM-ILD, and in elderly CTD-ILD, the common ones were RA-ILD and SS-ILD. However, both PM/DM-ILD were non-elderly (Table 1).
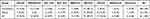 |
Table 1 Distribution Characteristics of Non-Elderly and Elderly Patients with CTD-ILD [n (%)] |
Clinical Features
One hundred and sixty-one CTD-ILD patients were characterized by cough (ANCA-ILD, SS-ILD, PM/DM-ILD, OS-ILD cough incidence ≥50%), decreased activity tolerance (OS-ILD, PM/DM-ILD, SSc-ILD, SLE-ILD, SS-ILD, ANCA-ILD incidence of decreased activity tolerance ≥50%), as the main clinical manifestations. The incidence of sputum, hemoptysis, chest tightness, chest pain, fatigue, fever, history of cold and velcro rales were all lower in the rest (Table 2).
 |
Table 2 Clinical Characteristics of Different CTD-ILD Patients |
The initiation age of elderly CTD-ILD patients was 45.61±10.41 years, and the mean age of non-elderly CTD-ILD patients was 61.07±10.26 years (p=0.001). Compared with non-elderly CTD-ILD, elderly CTD-ILD patients had a longer duration of CTD (p=0.040) but had a lower incidence of fatigue (p=0.005) and decreased activity tolerance (p=0.029). There was no significant difference in hemoptysis, chest tightness, chest pain, fever, history of cold, and velcro rales (Table 3).
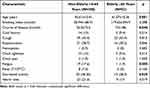 |
Table 3 Clinical Characteristics of Elderly and Non-Elderly Patients with CTD-ILD |
In both elderly and non-elderly CTD-ILD patients, the smoking index of male CTD-ILD patients was significantly higher than that of females (p=0.000, respectively). Still, the symptoms of decreased activity tolerance were not significantly higher than those of females (p<0.05, respectively). The detection rate of velcro rales in elderly men with CTD-ILD was higher than that in elderly women (p=0.027). However, there were no significant differences in age, smoking index, history of cold, cough, expectoration, hemoptysis, chest tightness, chest pain, fatigue, and fever (Table 4).
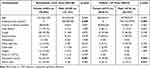 |
Table 4 Clinical Characteristics of Non-Elderly and Elderly Patients with CTD-ILD of Different Genders |
Serological Examination Indicators
Compared with non-elderly CTD-ILD, elderly CTD-ILD patients had significantly lower hemoglobin (p=0.003) but significantly higher red blood cell distribution width standard deviation (RDW-SD, p=0.024) and immunoglobulin IgA (p=0.033). In addition, compared to non-elderly CTD-ILD, the neutrophil-lymphocyte ratio NLR was not statistically significant in elderly CTD-ILD patients (p=0.109); however, there was a significant reduction in the systemic immunoinflammatory index (SII) (platelets × NLR) (p=0.014). Moreover, there was no statistically significant differences between non-elderly CTD-ILD and elderly CTD-ILD patients in comparison to leukocyte, neutrophil and lymphocyte count, neutrophil ratio, lymphocyte ratio, erythrocyte distribution width coefficient of variation (RDW-CV), platelets, C-reactive protein (CRP), Erythrocyte Sedimentation Rate (ESR), IgG/IgM, complement proteins C3/C4, blood calcium, Rheumatoid factor (RF), and Anti-cyclic citrullinated peptide antibody (CCP) indices (Table 5).
 |
Table 5 Serological Indexes of CTD-ILD Patients in Elderly and Non-Elderly Patients |
Among the non-elderly, women with CTD-ILD were more likely to have reduced hemoglobin than men with CTD-ILD (p=0.000). Among the elderly, female CTD-ILD patients had a more significant elevated lymphocyte ratio than male CTD-ILD patients (p=0.018), and NLR and SII were lower in female CTD-ILD patients (p=0.038) than in male CTD-ILD patients (p=0.043) (Table 6). However, the differences between non-elderly and elderly CTD-ILD patients, males and females, in terms of leukocyte, neutrophil and lymphocyte count, neutrophil ratio, the standard deviation of erythrocyte distribution width, coefficient of variation of erythrocyte distribution width, platelets, C-reactive protein, sedimentation, IgG/IgA/IgM, complement proteins C3/C4, blood calcium, RF index were not statistically significant.
 |
Table 6 Serological Indexes of Non-Elderly and Elderly Patients with CTD-ILD of Different Genders |
Blood Gas Analysis and Pulmonary Function
There were 77 patients with complete blood gas analysis (21 elderly and 56 non-elderly patients) and 75 patients with complete pulmonary function examination (26 elderly patients and 49 non-elderly patients). Compared with non-elderly CTD-ILD patients, elderly CTD-ILD patients had no significant difference in oxygen, carbon dioxide, alveolar oxygen, and alveolar oxygen partial pressure ratios (p > 0.05). Both elderly and non-elderly CTD-ILD patients had restrictive ventilatory and diffusing dysfunction, and the number of elderly CTD-ILD patients with diffusing dysfunction was less than that of non-elderly CTD-ILD patients (p=0.047) (Table 7).
 |
Table 7 Blood Gas Analysis and Pulmonary Function Test in Elderly and Non-Elderly Patients with CTD-ILD |
Discussion
In this study, we found that the most common clinical manifestations of CTD-ILD patients were cough (44.72%), decreased activity tolerance (40.37%), and coughing sputum (29.12%). The incidence of different CTD-ILD varied greatly. In this study, the CTD composition ratio of 161 patients with CTD-ILD was 120 females (74.53%) and 41 males (25.47%), with a male-to-female ratio of 1:2.93; 53 elderly patients (mean, 70.57 ± 4.03 years old; male to female ratio 1:2.31) and 108 non-elderly patients (mean, 52.00 ± 11.50 years old; male to female ratio, 1:3.32). These results indicated that elderly or non-elderly female patients were more likely to develop CTD-ILD than male patients. Among the 161 patients with CTD-ILD, the highest composition ratio of RA-ILD was 79 cases (49.07%), consistent with the results reported in literature.2,14,15 By analyzing the CTD composition ratio of non-elderly CTD-ILD patients, we found that the most common ones were RA-ILD and PM/DM-ILD. It is suggested that RA, PM/DM non-elderly patients, should be more alert to the occurrence of ILD. Even more surprisingly, we found that PM/DM was all non-elderly. In addition, by analyzing the CTD composition ratio of elderly CTD-ILD patients, we found that the most common ones were RA-ILD (50.94%) and SS-ILD (15.09%), which were consistent with the earlier reports.16,17 Prompt for the elderly RA, SS, should be more alert to the occurrence of ILD. Several studies suggested that male sex and advanced age are risk factors for poor prognosis in CTD-ILD.4,16,18,19 Therefore, we further analyzed the clinical characteristics of elderly and non-elderly CTD-ILD patients by gender, and we found that the smoking index was significantly higher in both men than in women (p=0.000), suggesting that male patients with CTD who smoke are more likely to have co-morbid ILD, but the current mechanism regarding smoking and CTD-ILD is unclear. It may be related to inhaling toxic chemicals and particles from tobacco smoke into the lungs causing immune cell activation and inflammatory cell aggregation.20 Therefore, elderly male smokers with significant cough, sputum, and decreased activity tolerance and with underlying diseases such as RA and SS should be alerted with regard to development of ILD.
NLR is the neutrophil value divided by the lymphocyte value and is a subclinical inflammatory marker that is often elevated in idiopathic interstitial lung disease (IPF), chronic obstructive pulmonary diseases, and asthma exacerbations. These biomarkers can indirectly assess the level of inflammation and cellular immunity in the body.21 The normal NLR value in Western countries is between 2.5% and 5%, and the Chinese is around 1.5%.22 The NLR of each CTD-ILD subgroup in our study was around 3%, suggesting that CTD-ILD patients were in an inflammatory state. SII can integrate the levels of neutrophils, lymphocytes, and platelets and is an independent risk factor for tumorigenesis23,24 and is also often used as a prognostic predictor for many tumors.25–29 Higher SII values indicate a stronger inflammatory response and weaker immune response in the body30,31. Studies have reported that NLR and SII are more likely to reflect acute inflammation levels in the body at an early stage and are associated with disease severity and poor prognosis in CTD patients.32–34 One study reported that NLR and SII can be used as markers of pulmonary interstitial involvement.33 A lower SII suggests a stronger immune response of the body, and in immune diseases, it often indicates disease progression and poor prognosis. Red blood cell distribution width (RDW) is a parameter reflecting heterogeneity in red blood cell volume and can be elevated by inflammatory and nutritional influences.31 In recent studies, RDW has been suggested to be promising biomarker for IPF, community-acquired pneumonia, chronic obstructive pulmonary disease, and CTD-ILD.35 Some studies have shown that increased RDW is significantly associated with decreased diffusing capacity of the lungs for carbon monoxide (CO diffusion capacity test, DLCO%) and is independent risk factor for survival in CTD-ILD patients.36 In healthy adults, the effect of gender on NLR is small, while on SII is higher in women, and SII and NLR values are higher in older adults,31 probably related to the decreased thymic function and absolute lymphocyte values. Our study showed that all elderly CTD-ILD patients were more likely to have decreased hemoglobin compared to non-elderly CTD-ILD patients (p=0.003). In contrast, among non-elderly CTD-ILD patients, women were more likely to have decreased hemoglobin (p=0.000). In terms of inflammatory indicators, compared to non-elderly CTD-ILD patients, older CTD-ILD had increased RDW-SD (p=0.024), decreased SII (p=0.014), and increased IGA (p=0.033). These results suggested a stronger immune response in elderly CTD-ILD patients with predominantly IGA immunity. We also found through further analysis that in older adults, serological SII and NLR were significantly lower in female CTD-ILD patients than in male CTD-ILD patients. This suggested that compared to older male CTD-ILD, older female CTD-ILD patients have lower levels of inflammation and higher immune responses in vivo. Under normal circumstances, inflammatory responses must be accompanied by immune responses, but immune responses do not necessarily. The presence of an inflammatory response indicates the presence of a high immune response in older female CTD-ILD patients. This low inflammatory response/high immune level suggests a poor prognosis. Therefore, there are low inflammatory levels/high immune disorders in elderly CTD-ILD patients, especially in elderly female CTD-ILD patients.
Lung diffusing dysfunction is an obstacle in the physical diffusion process in which O2, CO2 and other gases exchange through the alveolar membrane. Lung diffusing dysfunction is characterized by the carbon monoxide diffusion capacity (DLCO, TLCO) <80% in lung function test. Restrictive ventilatory dysfunction is caused by limited lung expansion and retraction with a decrease of TLC in lung function test. The main pathological process of diffusion and restriction dysfunction in CTD-ILD is the accumulation and massive deposition of inflammatory cells, myofibroblasts and fibroblasts, and some extracellular matrix in the interstitial lung matrix. This leads to alveolar and capillary damage, repeated alternation of interstitial tissue damage and repair, eventually causing lung tissue remodeling and pulmonary fibrosis. Under the double blow of aging and CTD-ILD disease, elderly CTD-ILD patients are more affected with hypoxia and more severely impaired lung function. Our study analysis found that CTD-ILD patients were in a hypoxic state (arterial partial pressure of oxygen and alveolar partial pressure of oxygen were reduced), but the difference caused by age in arterial blood gas analysis was not statistically significant. Pulmonary dysfunction in CTD-ILD patients was dominated by restrictive ventilatory function and diffusion dysfunction, which was instead lower in older CTD-ILD patients who developed pulmonary diffusion dysfunction compared to non-older CTD-ILD patients (p=0.047). Although older CTD-ILD patients have a more severe systemic immune response, older CTD-ILD patients do not have worse lung function and worse blood gas outcomes, consistent with study carried out by Karen et al.37
However, there are some limitations of this study. First, the number of cases was small which needs to be expanded before statistical analysis. Second, this study was conducted in a single center; however, a multicenter study is needed to validate the above results. Third, all the data above were analyzed retrospectively, and it was not possible to collect and analyze the required data in a prospective manner. Fourth, the above cases should be followed up dynamically to observe whether there is diagnostic error.
Conclusion
In summary, our study shows that CTD-ILD mainly affects non-elderly and women. Age may not be involved with decreased activity tolerance and increased lung function impairment in CTD-ILD patients. However, the elderly patients with CTD-ILD, especially the elderly female patients with low inflammation levels and high immune disorders, have a poor prognosis. Moreover, the diagnosis should be made clinically as soon as possible by improving pulmonary function and pulmonary imaging, with the aim of early treatment, preventing complications, and improving prognosis.
Acknowledgment
This study was supported by grants from Guizhou Provincial Respiratory Critical Disease Clinical Research and Prevention and Treatment Talent Base Project ([2020]8), Zunyi Respiratory Medicine Talent Base Project ([2019]69), Science and Technology Fund of Guizhou Provincial Health Commission [gzwkj2023-017], Science and Technology Bureau Project of Zunyi City (Zunshi Kehe HZ [2020]292).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Liya L, Xiaoxia Z, Yunhui Y, et al. Mortality trend of inpatients with connective tissue diseases: ease200S—;20 I 4. J Cent South Univ. 2017;42:1.
2. Antin-Ozerkis D, Hinchcliff M. Connective tissue disease-associated interstitial lung disease: evaluation and management. Clin Chest Med. 2019;40:617–636. doi:10.1016/j.ccm.2019.05.008
3. Wells AU. New insights into the treatment of CTD-ILD. Nat Rev Rheumatol. 2021;17:79–80.
4. Rivera-Ortega P, Molina-Molina M. Interstitial lung diseases in developing countries. Ann Glob Health. 2019;2019:85.
5. Demoruelle MK, Mittoo S, Solomon JJ. Connective tissue disease-related interstitial lung disease. Best Pract Res Clin Rheumatol. 2016;30:39–52.
6. Gao Y, Zhao Q, Qiu X, et al. Vitamin D levels are prognostic factors for connective tissue disease associated interstitial lung disease (CTD-ILD). Aging. 2020;12:4371–4378.
7. Messina R, Guggino G, Benfante A, Scichilone N. Interstitial lung disease in elderly rheumatoid arthritis patients. Drugs Aging. 2020;37:11–18.
8. Esposito AJ, Chu SG, Madan R, Doyle TJ, Dellaripa PF. Thoracic manifestations of rheumatoid arthritis. Clin Chest Med. 2019;40:545–560.
9. Duarte AC, Porter JC, Leandro MJ. The lung in a cohort of rheumatoid arthritis patients-an overview of different types of involvement and treatment. Rheumatology. 2019;58:2031–2038.
10. Das A, Kumar A, Arrossi AV, Ghosh S, Highland KB. Scleroderma-related interstitial lung disease: principles of management. Expert Rev Respir Med. 2019;13:357–367. doi:10.1080/17476348.2019.1575732
11. DeMizio DJ, Bernstein EJ. Detection and classification of systemic sclerosis-related interstitial lung disease: a review. Curr Opin Rheumatol. 2019;31:553–560. doi:10.1097/BOR.0000000000000660
12. Perelas A, Silver RM, Arrossi AV, Highland KB. Systemic sclerosis-associated interstitial lung disease. Lancet Respir Med. 2020;8:304–320. doi:10.1016/S2213-2600(19)30480-1
13. Distler O, Highland KB, Gahlemann M, et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med. 2019;380:2518–2528. doi:10.1056/NEJMoa1903076
14. Tian M, Huang W, Ren F, et al. Comparative analysis of connective tissue disease-associated interstitial lung disease and interstitial pneumonia with autoimmune features. Clin Rheumatol. 2020;39:575–583. doi:10.1007/s10067-019-04836-3
15. Guo B, Wang L, Xia S, et al. The interstitial lung disease spectrum under a uniform diagnostic algorithm: a retrospective study of 1945 individuals. J Thorac Dis. 2020;12:3688–3696. doi:10.21037/jtd-19-4021
16. Chan C, Ryerson CJ, Dunne JV, Wilcox PG. Demographic and clinical predictors of progression and mortality in connective tissue disease-associated interstitial lung disease: a retrospective cohort study. BMC Pulm Med. 2019;19:192. doi:10.1186/s12890-019-0943-2
17. Salinas M, Solomon JJ, Fernandez Perez ER. Connective tissue disease-interstitial lung disease-associated mortality rates and years of potential life lost in the United States. Chest. 2021;160:1368–1371. doi:10.1016/j.chest.2021.03.034
18. Ratwani AP, Ahmad KI, Barnett SD, Nathan SD, Brown AW. Connective tissue disease-associated interstitial lung disease and outcomes after hospitalization: a cohort study. Respir Med. 2019;154:1–5. doi:10.1016/j.rmed.2019.05.020
19. Sun D, Wang Y, Liu Q, et al. Prediction of long-term mortality by using machine learning models in Chinese patients with connective tissue disease-associated interstitial lung disease. Respir Res. 2022;23:4. doi:10.1186/s12931-022-01925-x
20. Shao T, Shi X, Yang S, et al. Interstitial lung disease in connective tissue disease: a common lesion with heterogeneous mechanisms and treatment considerations. Front Immunol. 2021;12:684699.
21. Liu J, Pang Z, Wang G, et al. Advanced role of neutrophils in common respiratory diseases. J Immunol Res. 2017;2017:6710278.
22. Luo H, He L, Zhang G, et al. Normal reference intervals of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and systemic immune inflammation index in healthy adults: a large multi-center study from Western China. Clin Lab. 2019;2019:65.
23. Nøst TH, Alcala K, Urbarova I, et al. Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol. 2021;36:841–848.
24. Fest J, Ruiter R, Mulder M, et al. The systemic immune-inflammation index is associated with an increased risk of incident cancer-A population-based cohort study. Int J Cancer. 2020;146:692–698.
25. Li W, Ma G, Deng Y, et al. Systemic immune-inflammation index is a prognostic factor for breast cancer patients after curative resection. Front Oncol. 2021;11:570208.
26. Hirahara N, Tajima Y, Matsubara T, et al. Systemic immune-inflammation index predicts overall survival in patients with gastric cancer: a propensity score-matched analysis. J Gastrointest Surg. 2021;25:1124–1133.
27. Hong YM, Yoon KT, Cho M. Systemic immune-inflammation index predicts prognosis of sequential therapy with sorafenib and regorafenib in hepatocellular carcinoma. BMC Cancer. 2021;21:569.
28. Atasever Akkas E, Yucel B. Prognostic value of systemic immune inflammation index in patients with laryngeal cancer. Eur Arch Otorhinolaryngol. 2021;278:1945–1955.
29. Huang T, Zhang H, Zhao Y, et al. Systemic immune-inflammation index changes predict outcome in stage III non-small-cell lung cancer patients treated with concurrent chemoradiotherapy. Future Oncol. 2021;17:2141–2149.
30. Gürol G, Çiftci İH, Terizi HA, Atasoy AR, Ozbek A, Köroğlu M. Are there standardized cutoff values for neutrophil-lymphocyte ratios in bacteremia or sepsis? J Microbiol Biotechnol. 2015;25:521–525.
31. Fei Y, Wang X, Zhang H, Huang M, Chen X, Zhang C. Reference intervals of systemic immune-inflammation index, neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, mean platelet volume to platelet ratio, mean platelet volume and red blood cell distribution width-standard deviation in healthy Han adults in Wuhan region in central China. Scand J Clin Lab Invest. 2020;80:500–507.
32. Nathan SD, Mehta J, Stauffer J, et al. Changes in neutrophil-lymphocyte or platelet-lymphocyte ratios and their associations with clinical outcomes in idiopathic pulmonary fibrosis. J Clin Med. 2021;2021:10.
33. Ruta VM, Man AM, Alexescu TG, et al. Neutrophil-to-lymphocyte ratio and systemic immune-inflammation index-biomarkers in interstitial lung disease. Medicina. 2020;56:1.
34. Motoc NS, Man MA, Campean Urda AE, Ruta VM, Todea DA, Pop CM. Neutrophil-to-lymphocyte ratio and platelets-to-lymphocytes ratio in severe COPD exacerbation: the importance of obstructive sleep apnea. Eur Respiratory Soc. 2019;54:PA2582.
35. Liu C, Yang J, Lu Z. Study on the red blood cell distribution width in connective tissue disease associated with interstitial lung disease. Biomed Res Int. 2020;2020:8130213.
36. Shi S, Chen L, Gui X, et al. Association of red blood cell distribution width levels with connective tissue disease-associated interstitial lung disease (CTD-ILD). Dis Markers. 2021;2021:5536360.
37. Patterson KC, Shah RJ, Porteous MK, et al. Interstitial lung disease in the elderly. Chest. 2017;151:838–844.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
