Back to Journals » Infection and Drug Resistance » Volume 15
Analysis of Clinical Characteristics and Risk Factors for Drug Resistance in Newly-Treated Patients with Pulmonary Tuberculosis Complicated with Chronic Obstructive Pulmonary Disease
Received 12 January 2022
Accepted for publication 20 July 2022
Published 25 August 2022 Volume 2022:15 Pages 4861—4869
DOI https://doi.org/10.2147/IDR.S358121
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Suresh Antony
Liangliang Ma,1 Maolong Gao2
1Department of Infectious Diseases, Beijing Geriatric Hospital, Beijing, 100095, People’s Republic of China; 2Department of Science and Technology, Beijing Geriatric Hospital, Beijing, 100095, People’s Republic of China
Correspondence: Liangliang Ma, Department of Infective Diseases, Beijing Geriatric Hospital, No. 118 Wenquan Road, Haidian District, Beijing, 100095, People’s Republic of China, Tel +86-18610672953, Email [email protected]
Objective: To analyze the clinical characteristics and risk factors of drug resistance of newly-treated chronic obstructive pulmonary disease (COPD) complicated pulmonary tuberculosis (PTB).
Methods: A total of 489 newly-treated PTB patients admitted to Beijing Geriatric hospital were retrospectively enrolled in this study. Of these, 138 patients with COPD were allocated to the study group, and the remaining 351 patients without COPD were allocated to the control group. The baseline information, clinical characteristics of PTB and drug resistance of Mycobacterium tuberculosis were compared between the two groups. Logistic regression was used to explore the correlation between drug resistance and COPD complications.
Results: Patients complicated with COPD had a higher proportion of respiratory failure, cough, fever and night sweats, chest short breath, and emaciation between the study group and the control group (P< 0.05). In terms of medical history, patients complicated with COPD also had a higher proportion of childhood TB history, cough, tuberculosis exposure rate, dust exposure rate, and malnutrition (P< 0.05). There were significantly more patients with pulmonary cavities and a delayed diagnosis of TB in the study group than in the control group (P< 0.05). The single drug resistance rates of isoniazid, ethambutol, rifampicin, pyrazinamide, and rifapentine, and drug resistance with any two or more drugs in the study group were significantly higher than those in the control group (P< 0.05). Multivariate Logistic regression analysis showed that smoking, extrapulmonary tuberculosis, tuberculosis exposure history, malnutrition, pulmonary cavity, and delayed TB diagnosis were risk factors for drug resistance in newly-treated COPD complicated PTB patients.
Conclusion: The symptoms of COPD complicated PTB were more serious. Smoking history, extrapulmonary tuberculosis, tuberculosis exposure history, malnutrition, pulmonary cavity, and delayed diagnosis of tuberculosis were risk factors for TB resistance in these patients.
Keywords: chronic obstructive pulmonary disease, pulmonary tuberculosis, Mycobacterium tuberculosis, drug resistance, risk factors
Introduction
Tuberculosis (TB) is a common infectious disease in the world, mainly caused by Mycobacterium tuberculosis. TB has a strong infectivity and high prevalence with severe mortality.1 According to the 2019 Global TB Report, there were about 10 million new cases in 2018 all over the world, and China was one of the 30 countries with a high TB burden, accounting for 14% of them.2 The rate of multi-drug-resistant tuberculosis (MDR-TB) in China was 6.8%, with an estimated 339,000 incident cases among the population over 15 years old in 2010.3 Previous studies showed that TB was an important risk factor for chronic obstructive pulmonary disease (COPD).4 At the same time, COPD was also closely related to tuberculosis.5 At present, about 9.9% of people older than 40 years in China are suffering from COPD, and the number of COPD patients is increasing with ages and environmental pollution.6 Besides, COPD is also an important cause of Mycobacterium tuberculosis drug resistance.7
Compared with TB alone patients, those with COPD combined TB face more severe health threats. Patients with COPD complicated pulmonary tuberculosis (PTB) often have a poor prognosis if they could not get suitable treatment in time. In addition, the cure rate of drug-resistant TB is extremely low.8 Drug resistance of TB bacilli increases the difficulty of treatment and the cost of patients, which brings more barriers to the treatment and prevention of TB. Therefore, it is necessary to analyze the clinical characteristics of COPD complicated PTB.
The aim of this study was to analyze the clinical characteristics of newly-treated COPD complicated PTB patients, and the risk factors of Mycobacterium tuberculosis drug resistance, so as to provide reference for clinical practice.
Methods
Study Patients
This study retrospectively included 489 cases of newly-treated PTB patients admitted to Beijing Geriatric hospital from October 2019 to October 2021. They were divided into a PTB (351 cases) group and PTB with COPD group (138 cases). Patients meeting the following criteria were included: 1) Diagnosis of TB was made according to WS288-2017;9 2) patients with complete laboratory examination, chest computed tomography (CT), and X-ray imaging data; 3) patients who were newly-diagnosed PTB; 4) patients with COPD met the diagnostic criteria set by the guidelines for diagnosis and treatment of COPD;10 and 5) patients who signed the informed consent. Patients who met the following criteria were excluded: 1) patients with malignant tumors or other serious multi-organ diseases; 2) patient suffering from mental disorders; 3) patients with other chronic infectious diseases; 4) patients with contraindications to antituberculous drugs; 5) patients with primary or secondary dementia; and 6) lack of follow-up information.
General information of all patients was collected from the medical system of Beijing Geriatric hospital, including age, sex, education level, height, weight, course of tuberculosis, and smoking history. Respiratory symptoms were collected, including respiratory failure, cough, fever, night sweats, chest tightness, shortness of breath, fatigue and emaciation, extrapulmonary tuberculosis, hemoptysis, and chest pain. Other conditions included in the study were as follows: history of childhood cough, tuberculosis exposure, dust exposure, malnutrition, tuberculosis lesion extent, and concomitant cavities.
This study complied with the Declaration of Helsinki and was approved by the ethics committee of Beijing Geriatric Hospital with number 2019004294z. Informed consent was waived due to the retrospective nature of the study.
Anti-Tuberculosis Drug Therapy
All patients were treated with the tuberculosis treatment protocol in the Guidelines for the Diagnosis and Treatment of Tuberculosis.7 All patients received 2 months of intensive therapy. Those less than 80 years old were given isoniazid (Shanxi Taiyuan Pharmaceutical Co., LTD.), 0.3 g/time, once per day; ethambutol (Guangdong South China Pharmaceutical Group Co., LTD.), 0.75 g/time, once per day; rifampicin (Zhejiang Pharmaceutical Co., LTD. Xinchang Pharmaceutical Factory), 0.45 g/time, once per day; and pyrazinamide (Shenyang Hongqi Pharmaceutical Co., LTD.), 0.5 g/time, 3 times per day. Patients older than 80 years were treated as follows: isoniazid (Shanxi Taiyuan Pharmaceutical Co., LTD.), 0.3 g/time, once per day; ethambutol (Guangdong South China Pharmaceutical Group Co., LTD.), 0.5 g/time, once per day; rifapentini (Wuxi Fuprayer Pharmaceutical Co., LTD.), 0.45 g/time, once every 2 weeks; and pyrazinamide (Shenyang Hongqi Pharmaceutical Co., LTD.), 0.5 g/time, twice per day. After 2 months of treatment according to the above regimen, a 4 months consolidation therapy was continued. Patients younger than 80 years old were given rifampicin, 0.45 g/time, once per day; and isoniazid, 0.3 g/time, once per day. Patients older than 80 years were given isoniazid, 0.3 g/time, once per day; and rifapentine, 0.45 g/time, once every 2 weeks. All drugs mentioned above were taken orally.
COPD complicated PTB patients were given anti-infection treatment at the same time as anti-TB therapy. Sensitive antibiotics were selected according to the sputum culture. Commonly used antibiotics included the second and third generation cephalosporins, quinolones, or aminoglycosides. Patients with fungal infection should be treated with antifungal agents. Liver and kidney function should be reviewed regularly during drug therapy.
Drug Sensitivity Testing
Drug sensitivity was performed after 2 months intensive therapy. BACTEC MGIT960 Automatic Mycobacterium rapid culture drug sensitivity instrument (Becton Dickinson, USA) was conducted for sensitivity test. Mycobacterium TB was cultured and identified according to the “Tuberculosis Diagnostic Laboratory Test Procedures”.11 The culture media for identification of Mycobacterium TB were p-nitrobenzoic acid (PNB) and thiophen-2-hydrazine (TCH). PNB and TCH were produced by Zhuhai Besol Industrial Company of China. The drug sensitivity of isoniazid, ethambutol, rifampicin, pyrazinaimde, and rifapentine was tested by proportional method.12 The reagent used was produced by Becton Dickinson Company (USA). The operation method of the MGIT960 system referred to the method used by Kim et al.13 All patients underwent TB culture twice a month and sputum smear three times per month for acid-fast bacilli. Tuberculosis culture was performed twice every month and acid-fast bacilli in sputum was performed three times every month. Single drug resistance indicated patients were resistant to one of isoniazid, ethambutol, rifampicin, pyrazinamde, or rifapentine. Multi-drug resistance indicated patients were resistant to two or more of the drugs mentioned above.
Statistical Analysis
All the data collected in this study were analyzed using SPSS 23.0 software. Normally distributed measurement data were expressed as mean±standard deviation (SD), and the comparisons were examined by Student’s t-test. The categorical data were expressed as n(%), and the differences between the two groups were examined by chi-square analysis or Fisher’s exact test. Logistic regression was used to analyze the risk factors for TB drug resistance in newly-treated COPD complicated PTB patients. P<0.05 was considered as statistically significant.
Results
General Data
A total of 489 newly-treated TB patients were enrolled in this study, including 138 patients in the study group and 351 patients in the control group. The average age of the study group was 53.69±10.12 years old, ranging from 22–82 years, and the mean body mass index (BMI) was 22.91±3.21. The average age of the control group was 53.76±10.18 years old, ranging from 22–82 years, and the mean BMI was 22.98±3.29. There was no significant difference in age, education level, height, weight, course of tuberculosis, or range of TB lesions between the two groups (P>0.05). Compared with the control group, there were significantly higher proportions of patients with male sex, smoking history, respiratory symptoms, and a delayed diagnosis of tuberculosis in the study group (P< 0.05) (Table 1).
 |
Table 1 Comparison of General Conditions Between the Two Groups |
Drug Resistance of Mycobacterium Tuberculosis
The single drug resistance rates of isoniazid, ethambutol, rifampicin, pyrazinamide, and rifapentine, and multi-drug resistance in the study group were significantly higher than those in the control group (P<0.05). There was no difference of other drug resistance between these two groups (P>0.05) (Table 2).
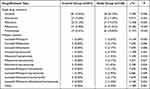 |
Table 2 Comparison of Commonly Used Anti-Tuberculosis Drug Resistance Between Two Groups |
Univariate Logistic Regression on Risk Factors for Drug Resistance of TB
Univariate Logistic regression analysis was used to analyze the risk factors for antituberculous drug resistance in patients with TB combined with COPD, including male, smoking history, extrapulmonary tuberculosis, history of cough during childhood, exposure history of tuberculosis, malnutrition, pulmonary cavity, and delayed diagnosis of tuberculosis (Table 3).
 |
Table 3 Univariate Logistic Regression Analysis of Risk Factors for Drug Resistance in Newly-Treated Pulmonary TB Patients with COPD |
Multivariate Logistic Regression on Risk Factors for Drug Resistance of TB
All risk factors with a P-value below 0.05 in univariate analysis were included in multivariate analysis.
Multivariate Logistic regression analysis revealed that the risk factors for antituberculous drug resistance in newly-diagnosed PTB patients with COPD were smoking history, extrapulmonary tuberculosis, exposure history of tuberculosis, malnutrition, pulmonary cavity, and tuberculosis diagnostic delay time (Table 4).
 |
Table 4 Multivariate Logistic Regression Analysis of Risk Factors for Anti-TB Drug Resistance in Newly-Treated Pulmonary TB Patients Complicated with COPD |
Discussion
Tuberculosis is a chronic infectious disease that seriously endangers human health.14 It is also one of the major risk factors for COPD.15 TB and COPD were both chronic respiratory diseases, with many similarities in clinical symptoms, such as cough, fever, night sweats, chest tightness, shortness of breath and hemoptysis.16 As clinical symptoms of tuberculosis can be masked by symptoms of COPD, a missed diagnosis would delay treatment for TB. In the present study, delayed diagnosis of PTB was found to be a risk factor for drug resistance of these patients with COPD, which confirmed the mask effect of COPD.
There are many similarities between PTB and COPD in respiratory symptoms. A previous study found that a history of TB was associated with airflow obstruction (FEV1/FVC <0.7) in 30.7% of patients, compared with 13.9% of those without a history of TB.17 Another population-based study in China showed that a previous TB history was an independent risk factor for airflow obstruction with an incidence of 24.2%. Thus, for patients with a previous history of TB, a combination occurrence of COPD should be suspected and cautiously examined.18 Li and Tian19 showed that cough, expectoration, weight loss, chest tightness, and shortness of breath were more common in elderly PTB. However, night sweat and fever were more common among the young PTB ones. Zhang et al20 reported that repeated expectoration, cough, asthma, and chest tightness were the main clinical symptoms, which were atypical for diagnosis, in elderly COPD complicated PTB patients Hence, laboratory and symptoms examination should be combined and evaluated repeatedly during the treatment, so as to avoid misdiagnosis and missed diagnosis.21 It was also reported that the incidence of malnutrition was higher in patients with inactive PTB complicated with COPD.22 The results of the present study showed that the clinical symptoms of newly-treated COPD complicated PTB patients included cough, fever, night sweat, chest tightness, shortness of breath, fatigue, and weight loss.
Nonstandard anti-tuberculosis drug therapy would induce Mycobacterium tuberculosis resistance. China’s tuberculosis control program has been implemented for many years, and a large number of TB patients have been discovered and treated, which effectively curbed the trend of tuberculosis transmission.23 However, due to the non-standard use of anti-tuberculosis drugs, there have been more and more drug resistant tuberculosis cases in China.23 A previous study showed that China had 120 thousand new cases of MDR-TB annually, accounting for a quarter all over the world.24 At present, the pathogenesis of MDR-TB is not clear, and risk factors affecting the occurrence of MDR-TB are varied in different countries and regions.25 This showed that the drug resistance rates of isoniazid, rifampicin, kanamycin, ofloxacin, and ethamol in patients with COPD complicated PTB were significantly higher than those of PTB alone, indicating that COPD complicated PTB had a high probability of MDR.26 Tan27 showed that patients with COPD complicated PTB could develop resistance to a variety of anti-TB drugs. The results of the present study showed that the single drug resistance rates of isoniazid, ethambutol, rifampicin, pyrazinamide, and rifapentine, and multi-drug resistance in the study group were significantly higher in the COPD complicated PTB patients than those with PTB alone (P<0.05). Thus, we should pay attention to this kind of patient in clinical practice. We can carry out a drug sensitivity test, If necessary, and adjust the treatment plan according to the drug sensitivity test plan, so as to alleviate the clinical symptoms of patients, and improve the clinical efficacy and prognosis of patients. Isoniazid and rifampicin are the first-line drugs commonly used in the treatment of pulmonary tuberculosis, among which isoniazid is the drug with the strongest bactericidal activity in the early stage. In the early stage of treatment, rifampicin alone can not achieve more than two bactericidal effects, and its bactericidal activity is significantly lower than that of isoniazid. Rifampicin single drug application can quickly induce resistance. The drug resistance of isoniazid is unstable, and there will be a certain effect of killing tuberculosis bacteria in the case of drug resistance. Therefore, when TB patients who are single resistant to isoniazid or rifampicin choose the treatment regimen containing isoniazid or rifampicin, it is easy to lead to the amplification effect of drug resistance, leading to the emergence of more multidrug-resistant TB patients. In the treatment of pulmonary tuberculosis patients, it is necessary to detect drug resistance as soon as possible, and take targeted anti-tuberculosis treatment schemes for patients with drug resistance to isoniazid or rifampicin, so as to reduce the occurrence of multi-drug resistant pulmonary tuberculosis and control the occurrence and development of pulmonary tuberculosis.
Effective prediction of risk factors for drug resistance PTB is helpful for its prevention. There were few clinical studies on the risk factors of drug resistance in newly-treated COPD complicated PTB patients. In this study, smoking history, extrapulmonary tuberculosis, tuberculosis exposure history, malnutrition, tuberculosis cavity, and delayed tuberculosis diagnosis were found to be risk factors for anti-TB drug resistance in newly-treated COPD complicated PTB patients. Previous studies had shown that smoking has negative effects on immune function and the prognosis of pulmonary tuberculosis.28 Meanwhile, smoking would reduce the phagocytosis of macrophages in the lung, result in a high possibility of infection and relapse of TB, and finally induce drug resistance.29 Malnutrition could promote the occurrence and development of tuberculosis and increase drug resistance.30 A history of childhood cough, tuberculosis, and delayed tuberculosis diagnosis can aggravate the respiratory infection, lack of oxygen, and change of lung structure and function. It was also reported that CD4+T lymphocyte levels were significantly reduced in COPD patients with PTB and who were also susceptible with MDR-TB.29 The 2021 report of the World Health Organization indicated the increased difficulty of curative treatment for COPD-complicated PTB.31 O’Toole et al32 found that the complication of COPD would result in more drug-resistance and worse outcomes in PTB patients. Liu et al33 proposed that COPD was significantly associated with multi-drug resistant PTB, which might be induced by the abuse of drug for COPD. Extrapulmonary tuberculosis means that more tissue is invaded by Mycobacterium tuberculosis, so patients with extrapulmonary tuberculosis are more likely to develop drug resistance.34 TB cavity often contains a large number of Mycobacterium tuberculosis, which was constantly proliferating, releasing, and easily leading to widespread TB and drug resistance.34
This study also had the following limitations: First, there were inherent biases due to the retrospective nature. Second, this was a single center analysis with limited validity. Thus, all results should be interpreted cautiously. Multicenter prospective analysis should be conducted in the future. Third, due to the limited data, correlation between COPD and PTB was not explored in this study and gene mutation of PTB was also not investigated. We would further study on this point in the future.
In conclusion, the clinical symptoms of newly-diagnosed COPD complicated PTB were more serious. Smoking history, extrapulmonary tuberculosis, tuberculosis exposure history, malnutrition, pulmonary cavity, and delayed diagnosis of tuberculosis were risk factors for TB resistance in these patients.
Abbreviations
COPD, chronic obstructive pulmonary disease; PNB, p-nitrobenzoic acid; PTB, pulmonary tuberculosis; TCH, thiophen-2-hydrazine; MDR, multi-drug-resistant.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Beijing Geriatric Hospital (No. 2018BJLNYY-008). Written consent was obtained from all study participants.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest.
References
1. Sinigaglia A, Peta E, Riccetti S, et al. Tuberculosis-associated microRNAs: from pathogenesis to disease biomarkers. Cells. 2020;9(10):2160. doi:10.3390/cells9102160
2. Harding E. WHO global progress report on tuberculosis elimination. Lancet Respir Med. 2020;8(1):19. doi:10.1016/S2213-2600(19)30418-7
3. Zhao JN, Zhang XX, He XC, et al. Multidrug-resistant tuberculosis in patients with chronic obstructive pulmonary disease in China. PLoS One. 2015;10(8):e0135205. doi:10.1371/journal.pone.0135205
4. Lee C-H, Lee M-C, Lin -H-H, et al. Pulmonary tuberculosis and delay in anti-tuberculous treatment are important risk factors for chronic obstructive pulmonary disease. PLoS One. 2012;7:e37978. doi:10.1371/journal.pone.0037978
5. Kim JH, Park JS, Kim KH, et al. Inhaled corticosteroid is associated with an increased risk of TB in patients with COPD. Chest. 2013;143(4):1018–1024. doi:10.1378/chest.12-1225
6. Huang TM, Kuo KC, Wang YH, et al.; On the behalf of Taiwan Clinical Trial Consortium for Respiratory Diseases (TCORE). Risk of active tuberculosis among COPD patients treated with fixed combinations of long-acting beta2 agonists and inhaled corticosteroids. BMC Infect Dis. 2020;20(1):706. doi:10.1186/s12879-020-05440-6
7. Acharya B, Acharya A, Gautam S, et al. Advances in diagnosis of Tuberculosis: an update into molecular diagnosis of Mycobacterium tuberculosis. Mol Biol Rep. 2020;47(5):4065–4075. doi:10.1007/s11033-020-05413-7
8. Li Z, Mao X, Liu Q, et al. Functional variations of the TLR4 gene in association with chronic obstructive pulmonary disease and pulmonary tuberculosis. BMC Pulm Med. 2019;19(1):184. doi:10.1186/s12890-019-0939-y
9. Suárez I, Fünger SM, Kröger S, et al. The diagnosis and treatment of tuberculosis. Dtsch Arztebl Int. 2019;116(43):729–735. doi:10.3238/arztebl.2019.0729
10. Mirza S, Clay RD, Koslow MA, et al. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93(10):1488–1502. doi:10.1016/j.mayocp.2018.05.026
11. Sia JK, Rengarajan J. Immunology of Mycobacterium tuberculosisInfections. Microbiol Spectr. 2019;7(4):10.
12. Huang YH, Kuang YB, Liang HD, et al. Discussion of the optimum concentration of bacterial liquid in the drug sensitivity test of Mycobacterium tuberculosis. Med Lab Sci Clin. 2018;29(3):21–24.
13. Gallo JF, Pinhata JMW, Saraceni CP, et al. Evaluation of the BACTEC MGIT 960 system and the resazurin microtiter assay for susceptibility testing of Mycobacterium tuberculosis to second-line drugs. J Microbiol Methods. 2017;139:168–171. doi:10.1016/j.mimet.2017.06.007
14. MacNeil A, Glaziou P, Sismanidis C, et al. Global epidemiology of tuberculosis and progress toward meeting global targets - worldwide, 2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):281–285. doi:10.15585/mmwr.mm6911a2
15. Sakornsakolpat P, Prokopenko D, Lamontagne M, et al. Genetic landscape of chronic obstructive pulmonary disease identifies heterogeneous cell-type and phenotype associations. Nat Genet. 2019;51(3):494–505. doi:10.1038/s41588-018-0342-2
16. Perez-Padilla R, Menezes AMB. Chronic obstructive pulmonary disease in Latin America. Ann Glob Health. 2019;85(1):7. doi:10.5334/aogh.2418
17. Menezes AM, Hallal PC, Perez-Padilla R, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J. 2007;30(6):1180–1185. doi:10.1183/09031936.00083507
18. Lam KB, Jiang CQ, Jordan RE, et al. Prior TB, smoking and airflow obstruction: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Chest. 2010;137(3):593–600. doi:10.1378/chest.09-1435
19. Li GJ, Tian XM. Analysis of clinical features and misdiagnosis causes of elderly and middle-aged and young patients with pulmonary tuberculosis. J Ningxia Med Univ. 2020;42(8):830–833.
20. Zhang ST, Tang BJ, Zhang XW, et al. Clinical analysis of chronic obstructive pulmonary disease with tuberculosis in elderly people. Chin Commun Doctors. 2020;36(12):34.
21. Park YB, Rhee CK, Yoon HK, et al.; Committee of the Korean COPD Guideline 2018. Revised (2018) COPD Clinical PracticeGuideline of the Korean Academy of Tuberculosis and Respiratory Disease: a Summary. Tuberc Respir Dis. 2018;81(4):261–273. doi:10.4046/trd.2018.0029
22. Park HY, Kang D, Shin SH, et al. Pulmonary tuberculosis and the incidence of lung cancer among patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2022;19(4):640–648. doi:10.1513/AnnalsATS.202010-1240OC
23. Nishi MP, Mancuzo EV, Sulmonett N, et al. Pulmonary functional assessment: longitudinal study after treatment of pulmonary tuberculosis. Rev Inst Med Trop Sao Paulo. 2021;63(63):e65. doi:10.1590/s1678-9946202163065
24. Tiberi S, Zumla A, Migliori GB. Multidrug and extensively drug-resistant tuberculosis: epidemiology, clinical features, management and treatment. Infect Dis Clin North Am. 2019;33(4):1063–1085. doi:10.1016/j.idc.2019.09.002
25. Shadrach BJ, Kumar S, Deokar K, et al. A study of multidrug resistant tuberculosis among symptomatic household contacts of MDR-TB patients. Indian J Tuberc. 2021;68(1):25–31. doi:10.1016/j.ijtb.2020.09.030
26. Li F. Clinical characteristics of pulmonary tuberculosis complicated with chronic obstructive pulmonary disease and drug resistance of anti-tuberculosis drugs. Chin J Clin Rational Drug Use. 2019;12(1):68–69.
27. Tan W. Clinical characteristics of tuberculosis patients with chronic obstructive pulmonary disease and analysis of antituberculosis drug resistance. Syst Med. 2020;5(2):53–55.
28. Shimeles E, Enquselassie F, Aseffa A, et al. Risk factors for tuberculosis: a case-control study in Addis Ababa, Ethiopia. PLoS One. 2019;14(4):e0214235. doi:10.1371/journal.pone.0214235
29. Chu AL, Lecca LW, Calderón RI, et al. Smoking cessation in tuberculosis patients and the risk of tuberculosis infection in child household contacts. Clin Infect Dis. 2021;73(8):1500–1506. doi:10.1093/cid/ciab504
30. Tellez-Navarrete NA, Ramon-Luing LA, Muñoz-Torrico M, et al. Malnutrition and tuberculosis: the gap between basic research and clinical trials. J Infect Dev Ctries. 2021;15(3):310–319. doi:10.3855/jidc.12821
31. World Health Organization. Global Tuberculosis Report 2021. Geneva: World Health Organization; 2021.
32. O’Toole RF, Shukla SD, Walters EH. TB meets COPD: an emerging global co-morbidity in human lung disease. Tuberculosis. 2015;95(6):659–663. doi:10.1016/j.tube.2015.08.005
33. Liu FP, Zhang CJ, Wang Y, et al. Multidrug-resistant tuberculosis drug resistance analysis and adverse reactions. Hebei Med J. 2015;37(15):2366–2368.
34. Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ. Extrapulmonary tuberculosis: pathophysiology and imaging findings. Radiographics. 2019;39(7):2023–2037. doi:10.1148/rg.2019190109
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
