Back to Journals » Journal of Healthcare Leadership » Volume 12
An Unmet Need in Healthcare Leadership: A Survey of Practicing Physicians’ Perspectives on Healthcare Delivery Science Education
Authors Weeks K , Swanson M , Hansen H, Merritt K, Nellis J, Charlton M, Reed A
Received 4 June 2020
Accepted for publication 2 September 2020
Published 7 October 2020 Volume 2020:12 Pages 95—102
DOI https://doi.org/10.2147/JHL.S265377
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Russell Taichman
Kristin Weeks,1 Morgan Swanson,1 Hayley Hansen,2 Katherine Merritt,2 Joseph Nellis,3 Mary Charlton,4 Alan Reed5
1Medical Scientist Training Program, Carver College of Medicine, Iowa City, IA, USA; 2Carver College of Medicine, Iowa City, IA, USA; 3Department of Surgery, Duke University, Durham, NC, USA; 4Department of Epidemiology, University of Iowa, Iowa City, IA, USA; 5Department of Surgery, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
Correspondence: Alan Reed
Department of Surgery, University of Iowa Hospitals and Clinics, SE 427 GH, 200 Hawkins Drive, Iowa City, IA 52242, USA
Tel +1 319-356-0537
Email [email protected]
Background: Healthcare delivery science education (HDSE) is increasingly needed by physicians balancing clinical care, practice management, and leadership responsibilities in their daily lives. However, most practicing physicians have received little HDSE in undergraduate through residency training. The purpose of this study is to 1) quantify the perception of the need for HDSE and interest in HDSE among a diverse sample of physicians, and 2) determine if perspectives on HDSE vary by specialty, rurality, and years in practice.
Methods: Using a cross-sectional, single state, mailed questionnaire, we surveyed 170 physicians about their perspectives on HDSE and interest in an HDSE program. Descriptive statistics and a multivariable logistic regression are presented.
Results: Among the 70.5% of responding eligible physicians, 75% of physicians had less HDSE than they would like and 90% were interested in obtaining more HDSE. Thirty-five percent of physicians were interested in joining the described HDSE program. The most prevalent barriers to obtaining HDSE were a lack of time and existing programs. Physician perspectives were similar across specialties, years in practice, and rurality.
Conclusion: There is a high unmet need for HDSE among physicians. Diverse and innovative HDSE programming needs to be developed to meet this need. Programming should be developed not only for physicians but also for undergraduate through residency training programs.
Keywords: healthcare delivery science, management, policy, education, rurality
Introduction
Finding the equilibrium between clinical care, practice management, and leadership roles is an increasing concern for physicians in the United States.1,2 Healthcare delivery science education (HDSE) can equip physicians with the skillsets needed to optimize clinical care delivery, maintain practice viability, and lead the delivery of excellent healthcare.3,4 HDSE is the interdisciplinary, integrated study of social science, public health, population health, bio-design thinking, business, law, and medicine toward improving the effectiveness and proficiency of patient-centered care.5–8
As medical schools and residency programs continue to struggle to allocate time and resources to HDSE amidst the growing mass of medical, translational, and basic science content, many physicians continue to graduate medical school and residency with minimal HDSE.6,9,10 When physicians begin their careers, it can be challenging to allocate time toward learning basic healthcare delivery science skills, such as financial literacy, management, and advocacy. Moreover, existing alternative formal didactic opportunities are limited and often time-intensive.11,12 Without formal training, many physicians utilize the most accessible solutions such as trial-and-error. This can lead to a double loss of hospital leadership potential and physicians’ skilled time.4,8,10,12,13 Some physicians receive targeted education during their transition to a leadership position; however, on-the-job training is likely not a sustainable option. This is especially true in rural places where the organizational overhead needed to consistently train physicians and recruit persons with different, specialized skillsets is missing.6,10,12,14
To date, there has been a paucity of investigation into the amount of HDSE practicing physicians receive post-residency and minimal investigation into the perceived need for HDSE among physicians. Our group previously conducted a qualitative study investigating 18 practicing physicians’ viewpoints on HDSE, including their past experiences with HDSE, interests in HDSE, barriers to obtaining HDSE, and interest in an example HDSE program. The qualitative study was useful for understanding the culture of a group of physicians in our state and for creating an appropriate survey instrument with relevant response options for this quantitative study. We hope this quantitative study can build upon the prior study by presenting numerical data and classifying physicians’ viewpoints.
This survey study was conducted among a sample of physicians in a single Midwestern state with a growing number of health professional shortage areas and rural populations. The aims of this study are to 1) quantify the perception of the need for HDSE and interest in HDSE among a diverse sample of physicians practicing across varied healthcare structures, practice locations (rurality), and practice settings and 2) determine if perspectives on HDSE vary by specialty type, rurality of practice, and length of career.
Methods
This cross-sectional study analyzes responses from a sample of physicians practicing in Iowa who were asked about their perspectives on HDSE in July–September of 2019 through a paper survey mailed to their work addresses. The Institutional Review Board at the University of Iowa reviewed and approved this research study (IRB# 201901815). Our study complied with the Declaration of Helsinki.
Sample
A self-administered questionnaire was mailed through the United States postal service to a random, stratified sample of 170 licensed physicians in Iowa. A list of all licensed physicians in Iowa, their current practice addresses, the medical school they graduated from, and their residency and fellowship training information were obtained from the Iowa Board of Medical Examiners. Inclusion criteria consisted of physicians that 1) were licensed through the Iowa Board of Medical Examiners as of January 2019 and 2) had reported primary work addresses in the state of Iowa at the time of their last medical license obtainment and/or renewal. Physicians were excluded if they were not employed at the work mailing address listed for the Iowa Board of Medical Examiners or if their work mailing address could not be verified online.
The sample was stratified by residency training. Twenty emergency medicine, pediatric, obstetrics/gynecology, psychiatry, and surgery trained physicians, as well as 40 internal medicine physicians, and 30 family medicine physicians, were randomly sampled. Random sampling was completed using a random-number generator and corresponding numbered lists of licensed physicians in each specialty. A greater number of internal medicine and family medicine physicians were sampled because they comprise a proportionally larger percentage of the work force in our state. Our sampled population aimed to and ultimately represented about 10% of eligible physicians in emergency medicine, pediatric, obstetrics/gynecology, psychiatry, and surgery, 5% of eligible physicians in internal medicine, and 3% of eligible physicians in family medicine.
Procedures
We used a modified Dillman approach to recruit physicians for the survey.15,16 Physicians were first mailed a postcard to notify them about the upcoming survey. One week later they were mailed a $5 cash incentive, prepaid return envelope, cover letter and a questionnaire instrument labeled with their study identification number. Potential participants were provided an informational letter describing the study and the potential risks and benefits of participation. In the letter, they were informed that completion of the survey indicated a willingness to participate in the study. Non-responders received up to three follow up telephone calls to their work telephone numbers four to eight weeks following the first mailing. At the minimum, a message was left on their personal voicemail or with their office staff. In each message and follow-up telephone conversation, the physician was asked if they would like to receive the survey a second time via fax or email, read over the telephone, or sent through the mail to a different mailing address. If we could not directly speak with the prospective participant or their staff, we verified their employment at their place of work via human resource personnel.
Questionnaire
The questionnaire instrument was created by two members of the research team. A qualitative study was conducted prior to instrument development in order to inform questions and response options. A literature review preceded the qualitative study. The questionnaire was pre-tested with two physicians and four non-physicians using think-aloud methods to ensure consistency in interpretation.
The first component of the survey (Part A) asked questions about physicians’ experience with HDSE, interest in future HDSE, barriers to obtaining HDSE, and perspectives on the importance of HDSE. The second part of the survey (Part B) asked questions about physicians’ interest in joining a continuing education program and their likes and dislikes of the program. The final section (Part C) asked demographic questions. Healthcare delivery science was defined in the instrument as all aspects of the business of medicine, including advocacy, entrepreneurship, finance, leadership, management and policy. The continuing education program was described as it appears in Figure 1.
 |
Figure 1 Description of educational program. |
Theoretical Frameworks Considered
Part B of the instrument, which focused on the assessment of an HDSE program, was created using the Diffusion of Innovation Theory.17 Our goal was to understand physicians’ perception of their need for HDSE, perspectives on advantageous and compatible components of the program, and barriers to the attainment of HDSE. The explanation of our program aimed to provide a simple description of a program that was easy to join and had didactic application opportunities. These efforts should theoretically provide a strong indication of physicians’ likelihood to utilize innovative HDSE programing.
Data Analysis
Prior to data entry, ambiguous survey marks were discussed by two team members and rectified with mutual consensus. Questionnaire responses were entered into a locked electronic file in Microsoft Excel. A second team member checked a random sample of 20 percentage of survey entries and found no mistakes. Survey results were quantified with SAS (Version 9.4; SAS Institute, Cary, NC).
We conducted multivariable logistic regressions to determine if having less HDSE training than the physician would have liked (binary), having interest in HDSE (binary), having interest in an HDSE program (binary), and feeling that HDSE would help their career (binary) varied by physicians’ self-reported practice setting (rural versus in between or urban), years in practice (0–15 and >15 years), and specialty (primary care vs. non-primary care). Primary care was defined as psychiatry, internal medicine, pediatrics, and family medicine. Using stepwise backward selection and comparing AICs, the final models of each outcome included rurality and years in practice.
Results
Survey Response
Of the 149 physicians eligible to complete the survey, 105 physicians (70.5%) responded (Figure 2). Physicians were excluded due to no longer working at the address (14), retirement from job (4), deployment overseas (2), and maternity leave (1).
 |
Figure 2 Sample response rate. |
Demographics of Responding Physicians
Participants had a wide range of career lengths, practice environments, and specialties (Table 1). Almost half of the participants practiced in a setting that was in-between a rural and urban setting.
 |
Table 1 Demographics of Physicians (N=105) That Participated in the Survey |
Participants Perceptions of HDSE
Seventy-five percent of physicians stated that they had less didactic HDSE than they would have preferred while 4% had received more HDSE than they would have preferred. Most physicians (90%) were interested in obtaining more HDSE with 24% being very interested, 38% somewhat interested, and 28% a little interested. Ten percent of physicians were not interested in obtaining HDSE. The major barriers physicians identified to obtaining further HDSE were limited time (66%), limited available resources (37%), low interest (18%), and cost (12%).
Ninety percent of physicians agreed or strongly agreed that ongoing HDSE was needed by physicians after residency. Sixty-three percent of physicians agreed or strongly agreed that obtaining more HDSE could improve their future career opportunities. Additionally, 96% of physicians disagreed or strongly disagreed that HDSE was not important to their specialty and 89% of physicians disagreed or strongly disagreed that HDSE was not important to physicians in their practice type.
Interest in Obtaining a HDSE Certificate
Physician interest in joining the described HDSE program was split relatively equally between would join (35%), would not join (35%), and uncertain about joining (30%). Affirmative plans to join the program were higher among the physicians that indicated that time and resources were barriers to obtaining HDSE. For example, among the physicians who indicated that a lack of resources prevented them from obtaining HDSE, 48% indicated they would join the program.
Physicians were most interested in the online resources (51%), expert speakers (49%), and the ability to virtually attend class (49%) (Table 2). The aspects of the certificate that were most disliked included collaborating on research (27%) and learning alongside medical students (23%).
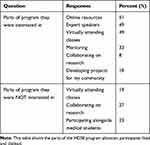 |
Table 2 Aspects of the HDSE Program That Interested and Disinterested Physicians |
Difference by Specialty Type, Rurality of Practice, and Length of Career
In all bivariate analyses and most multivariable logistic regressions, there was no difference in prior HDSE experience, interest in obtaining HDSE, interest in the HDSE program, and perceived career benefits of HDSE by years in practice (0–15 years versus >15 years), rurality of practice setting (rural versus non-rural), and specialty type (primary care versus non-primary care). With exception, in multivariable analysis while controlling for rurality, physicians practicing 0–15 years (versus >15 years) were significantly less likely to endorse that obtaining HDSE could improve their future career opportunities.
Conclusion
Our survey study of practicing physicians in a Midwestern state found most physicians have less HDSE than they would like. Physicians across many specialties see value in HDSE for their specialty and practice type. A great majority of physicians are interested in receiving HDSE and about one third are interested in joining a distance-learning program with didactic lectures and group project components. Time, existing resources and cost limited physicians from obtaining HDSE. Viewpoints on HDSE largely did not vary by years in practice, rurality of practice setting, and specialty type.
The scale of physicians’ unmet need for HDSE is concerning, especially as policies and reimbursement models continue to evolve, physicians are increasingly asked to evaluate and improve their efficiency based on data, and sustainability and cost-effectiveness are increasingly demanded.6,18–22 However, the scale of physicians’ perceived need is not surprising given the historic lack of HDSE in medical school and continuing medical education.23–27 Likewise, the breadth of need across all specialties was concerning, but expected. The need for HDSE across specialties, such as orthopedic surgery,28,29 pediatrics,29,30 internal medicine,30,31 emergency medicine,29,30 and general surgery30,32 has previously been reported. Moreover, studies of graduate and undergraduate medical education have previously reported the widespread need for HDSE, such as in the areas of finance and policy.6,30,33–37 Our study quantifies the population-based perceived need for HDSE among practicing physicians in healthcare systems across a state.
Our survey found physicians believe HDSE is needed by other physicians in their state and important to their specialty and practice type. Physicians see value in their peers obtaining HDSE and medical directors see value in developing organizational leadership training programs.38,39 Physicians who receive HDSE gain the ability to improve their working environments, address and reduce disparities among their patient populations, and make their healthcare systems more efficient.40–43 Newly developed HDSE programs may be championed and well received by the physician community even among physicians not directly interested in participating.
The described HDSE program was of interest to a broad physician population. As physicians advance in their careers (>15 years in practice), they may find more direct applicability for HDSE in improving their career opportunities. Physicians across varied specialties, practice settings, and prior experience levels reported a high interest in online learning and resources. As HDSE programs continue to develop, online resources and web-based learning could be well-received platforms for delivering expert content.5,14,44 Development of many HDSE program types may be needed in order to appeal to diverse physician populations with independent preferences.
Disinterest in the HDSE program seemed to most strongly relate to the mixed peer group and project requirements. HDSE program leadership often advocate for and incorporate these components into certificates and masters programs.5 Mentoring has been shown to be one of the most effective methods for achieving success and satisfaction in the workplace.39 Moreover, projects can help physicians find direct applicability of didactic content in their practice environments.9,39 However, given that only 20% of physicians were interested in completing projects, but 90% were interested in obtaining further education, future program development should consider making project requirements optional. Explaining the value of mixed peer groups to the physician learners may also help reduce dissatisfaction.
The perceived lack of time and paucity of existing HDSE continuing medical education programs is likely driving the disparity between interest and HDSE attainment among physicians. Short-term one-day or one-week long truncated courses that reduce time limitations may not provide the ability to overcome broad HDSE foundational deficits among physicians.39 However, longer and more comprehensive programs may greatly burden physicians already fatigued from the length of their prior education and training and those with many professional and personal responsibilities.7,11 Mentoring, coaching, and networking with peers or senior leaders are other existing options for physicians working within larger healthcare systems.9 However, these options are often lacking for physicians managing rural populations and independent practices.9 While developing new HDSE programs for practicing physicians is important, educating undergraduate pre-medical students, medical students, and medical residents could help reduce post-residency HDSE needs.
Our study has some limitations. First, our results may not be generalizable to all states and practice types or specialties. Our analyses investigating prior HDSE experiences and interest may be limited by a small sample size. We tried to mitigate the response bias of fixed survey response options by not forcing participants to respond to every question. The instrument was informed by an interview study in the same state. Cognitive interviewing and pilot testing improved the accuracy and validity of our survey instrument.
In conclusion, the majority of physicians were interested in HDSE and perceived they would benefit from HDSE. The need for HDSE existed equally among physicians by rurality, time in practice, and specialty. Time and existing resources limited physicians from obtaining HDSE. There is not consensus among physicians about the aspects of HDSE programing they like and dislike, and therefore diverse and innovative HDSE programming may be needed to meet physicians’ individualized circumstances. Improving HDSE could reduce physician burn out and improve professional capacities and practice viability. More HDSE programs should be developed for physicians pre- and post-residency.
Acknowledgments
We sincerely thank Hugh Hansen, Amanda Manorot, Gabe Conley, Savannah Borman, Usha Balakrishnan, Clay Walker, Telligen Community Initiative, and the participating physicians.
Disclosure
A grant from Telligen Community Initiative obtained by the student leadership board of the Healthcare Delivery Science, Management, and Policy Distinction track at the University of Iowa funded this study. No one on the research team received a direct payment or increase in salary from Telligen Community Initiative for conducting this study. KW reports a grant from Telligen Community Initiative, during the conduct of the study. The authors report no other potential conflicts of interest for this work.
References
1. Institute of Medicine, Gray BH, ed. The New Health Care for Profit: Doctors and Hospitals in a Competitive Environment. Washington (DC): National Academies Press (US); 1983.
2. Erickson SM, Rockwern B, Koltov M, McLean RM, Medical Practice and Quality Committee of the American College of Physicians. Quality committee of the American College of Physicians. putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659–661. doi:10.7326/M16-2697
3. Hill AD. Improving business IQ in medicine through mentorship and education. J Orthop Trauma. 2014;28(Suppl 9):S9–S11. doi:10.1097/BOT.0000000000000177
4. Patel AT, Bohmer RMJ, Barbour JR, Fried MP. National assessment of business-of-medicine training and its implications for the development of a business-of-medicine curriculum. Laryngoscope. 2005;115(1):51–55. doi:10.1097/01.mlg.0000150677.75978.75
5. Faerber A, Andrews A, Lobb A, et al. A new model of online health care delivery science education for mid-career health care professionals. Healthcare. 2019;7(4). doi:10.1016/j.hjdsi.2018.12.002
6. Myers CG, Pronovost PJ. Making management skills a core component of medical education. Acad Med. 2017;92(5):582–584. doi:10.1097/ACM.0000000000001627
7. Zarrabi B, Burce KK, Seal SM, et al. Business education for plastic surgeons. Plast Reconstr Surg. 2017;139(5):1263–1271. doi:10.1097/PRS.0000000000003290
8. Patel R, Rhee K, Barone J, Elsamra SE. Business education for residents: results of a pilot business course at a urology residency program. Urol Pract. 2018;5(2):107–112. doi:10.1016/j.urpr.2017.02.003
9. Warren OJ, Carnall R. Medical leadership: why it’s important, what is required, and how we develop it. Postgrad Med J. 2011;87(1023):27–32. doi:10.1136/pgmj.2009.093807
10. Ackerly DC, Sangvai DG, Udayakumar K, et al. Training the next generation of physician-executives: an innovative residency pathway in management and leadership. Acad Med. 2011;86(5):575–579. doi:10.1097/ACM.0b013e318212e51b
11. DeQuesada I, Falgun C, Mullins M, Duszak R. Practice management and health policy education in radiology: an emerging imperative. J Am Coll Radiol. 2015;12(10):1085–1092. doi:10.1016/j.jacr.2015.04.004
12. Revere L, Robinson A, Schroth L, Mikhail O. Preparing academic medical department physicians to successfully lead. Leadersh Health Serv. 2015;28(4):317–331. doi:10.1108/LHS-03-2014-0023
13. Satiani B, Sena J, Ruberg R, Ellison EC. Talent management and physician leadership training is essential for preparing tomorrow’s physician leaders. J Vasc Surg. 2014;59(2):542–546. doi:10.1016/j.jvs.2013.10.074
14. Schwartz RW, Pogge CR, Gillis SA, Holsinger JW. Programs for the development of physician leaders: a curricular process in its infancy. Acad Med. 2000;75(2):133–140. doi:10.1097/00001888-200002000-00008
15. De Leeuw ED, Hox J, Dillman D. International Handbook of Survey Methodology. Routledge; 2012.
16. Dillman DA. Mail and Telephone Surveys: The Total Design Method. Vol. 19. Wiley New York; 1978.
17. Kaminski J. Diffusion of innovation theory. Can J Nurs Inf. 2011;6(2):1–6.
18. Chaudry J, Jain A, McKenzie S, Schwartz RW. Physician leadership: the competencies of change. J Surg Educ. 2008;65(3):213–220. doi:10.1016/j.jsurg.2007.11.014
19. Sonnino RE. Health care leadership development and training: progress and pitfalls. J Healthc Leadersh. 2016;8:19–29. doi:10.2147/JHL.S68068
20. Busari JO, Berkenbosch L, Brouns JW. Physicians as managers of health care delivery and the implications for postgraduate medical training: a literature review. Teach Learn Med. 2011;23(2):186–196. doi:10.1080/10401334.2011.561760
21. Tun MS. Fulfilling a new obligation: teaching and learning of sustainable healthcare in the medical education curriculum. Med Teach. 2019;41(10):1168–1177. doi:10.1080/0142159X.2019.1623870
22. Gonzalo JD, Chang A, Wolpaw DR. New educator roles for health systems science: implications of new physician competencies for U.S. Medical School Faculty. Acad Med. 2019;94:4. doi:10.1097/ACM.0000000000002552
23. Goodall AH. Physician-leaders and hospital performance: is there an association? Soc Sci Med. 2011;73(4):535–539. doi:10.1016/j.socscimed.2011.06.025
24. Castro PJ, Dorgan SJ, Richardson B. A healthier health care system for the United Kingdom. McKinsey Q. 2008;1–5.
25. Falcone RE, Satiani B. Physician as hospital chief executive officer. Vasc Endovascular Surg. 2008;42(1):88–94. doi:10.1177/1538574407309320
26. Hartley K. Untangling approaches to management and leadership across systems of medical education. BMC Health Serv Res. 2016;16(2):33–43. doi:10.1186/s12913-016-1391-9
27. Patel MS, Davis MM, Lypson ML. Advancing medical education by teaching health policy. N Engl J Med. 2011;364(8):695–697. doi:10.1056/NEJMp1009202
28. Jennings JD, Quinn C, Ly JA, Rehman S. Orthopaedic surgery resident financial literacy: an assessment of knowledge in debt, investment, and retirement savings. Am Surg. 2019;85(4):353–358. doi:10.1177/000313481908500424
29. McKillip R, Ernst M, Ahn J, Tekian A, Shappell E. Toward a resident personal finance curriculum: quantifying resident financial circumstances, needs, and interests. Cureus. 2018;10.
30. Ahmad FA, White AJ, Hiller KM, Amini R, Jeffe DB. An assessment of residents’ and fellows’ personal finance literacy: an unmet medical education need. Int J Med Educ. 2017;8:192–204. doi:10.5116/ijme.5918.ad11
31. Wong R, Ng P, Bonino J, Gonzaga AM, Mieczkowski AE. Financial attitudes and behaviors of internal medicine and internal medicine-pediatrics residents. J Grad Med Educ. 2018;10(6):639–645. doi:10.4300/JGME-D-18-00015.1
32. Tevis SE, Rogers AP, Carchman EH, Foley EF, Harms BA. Clinically competent and fiscally at risk: impact of debt and financial parameters on the surgical resident. J Am Coll Surg. 2018;227(2):163–171.e167. doi:10.1016/j.jamcollsurg.2018.05.002
33. Havyer RD, Norby SM, Leep Hunderfund AN, et al. Science of health care delivery milestones for undergraduate medical education. BMC Med Educ. 2017;17(1):145.
34. Starr SR, Reed DA, Essary A, et al. Science of health care delivery as a first step to advance undergraduate medical education: a multi-institutional collaboration. Healthc. 2017;5(3):98–104. doi:10.1016/j.hjdsi.2017.01.003
35. Jacobs VR, Fischer T. A pragmatic guide on how physicians can take over financial control of their clinical practice. JSLS. 2012;16(4):632–638. doi:10.4293/108680812X13517013316438
36. Laiteerapong N, Huang ES. The pace of change in medical practice and health policy: collision or coexistence? J Gen Intern Med. 2015;30(6):848–852. doi:10.1007/s11606-015-3182-0
37. Greysen SR, Wassermann T, Payne P, Mullan F. Teaching health policy to residents–three-year experience with a multi-specialty curriculum. J Gen Intern Med. 2009;24(12):1322–1326. doi:10.1007/s11606-009-1143-1
38. Gagliano NJ, Ferris T, Colton D, Dubitzky A, Hefferman J, Torchiana D. A physician leadership development program at an academic medical center. Qual Manag Health Care. 2010;19(3):231–238. doi:10.1097/QMH.0b013e3181eb13ab
39. Markuns JF, Fraser B, Orlander JD. The path to physician leadership in community health centers: implications for training. Fam Med. 2010;42(6):403–407.
40. Parekh SG, Singh B. An MBA: the utility and effect on physicians’ careers. J Bone Joint Surg Am. 2007;89(2):442–447. doi:10.2106/JBJS.F.01245
41. Ennis-Cole DL, Cullum PM, Iwundu C. Physicians as operational leaders: cost, curriculum, technology, and organizational challenges. TechTrends. 2018;62(3):239–249. doi:10.1007/s11528-018-0273-x
42. Smith CD. Teaching high-value, cost-conscious care to residents: the alliance for academic internal medicine–American College of Physicians Curriculum. Ann Intern Med. 2012;157(4):284–286.
43. Earnest MA, Wong SL, Federico SG. Perspective: physician advocacy: what is it and how do we do it? Acad Med. 2010;85(1):63–67. doi:10.1097/ACM.0b013e3181c40d40
44. Shappell E, Ahn J, Ahmed N, Harris I, Park YS, Tekian A. Personal finance education for residents: a qualitative study of resident perspectives. AEM Educ Train. 2018;2(3):195–203. doi:10.1002/aet2.10090
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
