Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
An observational postmarketing safety registry of patients in the UK, Germany, and Switzerland, who have been prescribed Sativex® (THC:CBD, nabiximols) oromucosal spray
Authors Etges T, Karolia K, Grint T, Taylor A, Lauder H, Daka B, Wright S
Received 15 June 2016
Accepted for publication 31 August 2016
Published 11 November 2016 Volume 2016:12 Pages 1667—1675
DOI https://doi.org/10.2147/TCRM.S115014
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Tilden Etges, Kari Karolia, Thomas Grint, Adam Taylor, Heather Lauder, Brian Daka, Stephen Wright
GW Pharmaceuticals, Cambridge, UK
Abstract: The global exposure of Sativex® (Δ9-tetrahydrocannabinol [THC]:cannabidiol [CBD], nabiximols) is estimated to be above 45,000 patient-years since it was given marketing approval for treating treatment-resistant spasticity in multiple sclerosis (MS). An observational registry to collect safety data from patients receiving THC:CBD was set up following its approval in the UK, Germany, and Switzerland, with the aim of determining its long-term safety in clinical practice. Twice a year, the Registry was opened to prescribing physicians to voluntarily report data on patients’ use of THC:CBD, clinically significant adverse events (AEs), and special interest events. The Registry contains data from 941 patients with 2,213.98 patient-years of exposure. Within this cohort, 60% were reported as continuing treatment, while 83% were reported as benefiting from the treatment. Thirty-two percent of patients stopped treatment, with approximately one third citing lack of effectiveness and one quarter citing AEs. Psychiatric AEs of clinical significance were reported in 6% of the patients, 6% reported falls requiring medical attention, and suicidality was reported in 2%. Driving ability was reported to have worsened in 2% of patients, but improved in 7%. AEs were more common during the first month of treatment. The most common treatment-related AEs included dizziness (2.3%) and fatigue (1.7%). There were no signals to indicate abuse, diversion, or dependence. The long-term risk profile from the Registry is consistent with the known (labeled) safety profile of THC:CBD, and therefore supports it being a well-tolerated and beneficial medication for the treatment of MS spasticity. No evidence of new long-term safety concerns has emerged.
Keywords: cannabidiol, tetrahydrocannabinol, non-interventional, multiple sclerosis, spasticity, risk management plan
Introduction
It is estimated that globally, 2.3 million people have multiple sclerosis (MS), the most common disabling neurological condition affecting young adults with an average age of onset of 30 years.1 Several symptoms may occur as a consequence of the progressive neurological damage, and spasticity (muscle rigidity and spasms) is one of the most common of these symptoms, affecting around 80% of MS patients within 10 years of diagnosis, worsening with time,2 and leading to significant functional impairment.3
The endocannabinoid system modulator Sativex® (Δ9-tetrahydrocannabinol [THC]:cannabidiol [CBD], nabiximols) is formulated from THC and CBD, both extracted from selectively bred chemotypes of the Cannabis sativa L. plant, which has been developed to produce high and reproducible yields of these cannabinoids; each 100 μL actuation of the oromucosal spray delivers 2.7 mg THC and 2.5 mg CBD.4 THC:CBD was first granted marketing authorization in Canada (April 2005) and then in the European Union (initially the UK) in June 2010 for treatment of adult MS patients with moderate-to-severe spasticity who did not respond adequately to other antispasticity medication and demonstrated clinically significant improvement in spasticity-related symptoms during an initial trial of therapy. Significant improvements in MS spasticity symptoms have consistently been reported in randomized controlled trials (RCTs),5–9 and open-label extension studies have shown improvements in spasticity10 and spasms, pain, and bladder control11 which are maintained in the longer term without emergence of tolerance to THC:CBD. Apart from showing that THC:CBD is efficacious in the treatment of MS spasticity, these studies have demonstrated the treatment to be well tolerated in the short-to-medium term, with the majority of AEs reported being mild or moderate and the most common ones consistently being dizziness and fatigue.
As a postmarketing Risk Management Plan commitment with the Medicines and Healthcare products Regulatory Agency (MHRA), the Marketing Authorization Holder GW Pharmaceuticals (GW) gave an undertaking to maintain an observational product registry (“the Registry”) to collect safety data on patients receiving THC:CBD, with the aim of determining the long-term safety in clinical practice. The Registry opened in the UK in 2010, followed by Germany in 2012, and was extended to include Switzerland in 2015.
The Registry is a non-interventional safety study for patients prescribed THC:CBD, with the objective being to monitor for the emergence of new safety signals in the real-world setting that may not be apparent in shorter RCTs where patients have had to meet stringent eligibility criteria. Prescribers were requested to answer targeted questions related to areas of special interest identified in the Risk Management Plan concerning mainly, but not exclusively, neurological and psychiatric disorders: clinically significant AEs; falls requiring medical attention; suicidal thoughts or attempted suicide; other significant psychiatric events; changes in driving ability; and the potential for abuse, dependence, or misuse.
In early 2015, the UK arm of the Registry closed after the MHRA concluded that sufficient data had been obtained from UK patients to characterize the safety profile of long-term treatment with THC:CBD. Limited data continues to be collected under national approval requirements in Germany and Switzerland. The global postmarketing safety exposure for THC:CBD is now estimated to be above 45,000 patient-years.
Methods
The Registry was a multicenter, observational program for patients prescribed THC:CBD, and was maintained by GW. As no experimental intervention was involved, data entry was anonymized, and the medicine was being prescribed in routine clinical practice, the UK National Research Ethics Service confirmed that there was no requirement to obtain ethical approval or patient consent in the UK. In accordance with the individual national requirements, ethical approval and patient consent were obtained prior to any solicitation for information in Germany and Switzerland. Nominal compensation was provided to reporting prescribers for the time taken to complete the Case Report Forms (CRFs) only.
In the UK, prescribers of THC:CBD were identified using the prescription information supplied to the distributer, irrespective of the therapeutic indication, and were invited to participate. In Germany and Switzerland, a number of specialist MS centers were recruited and the prescribers contacted directly. All data entry was voluntary with the participating prescribers being invited to provide anonymized patient data for the Registry twice per year using either encrypted electronic or paper CRFs; there were no patient questionaires.
During each 2–3 months long data collection period (DCP), the prescribers were asked to provide the patients’ sex, year of birth, therapeutic indication for THC:CBD, daily dose, and prescription dates, state whether THC:CBD was providing benefit and the patients were still taking THC:CBD, and provide survival status. Prescribers were also asked questions targeting special safety interest topics approved by the MHRA (risk of falls, suicidality, psychosis, abuse liability, effect on driving), and to provide further information if a clinically significant AE had occurred (the term “clinical significance” was left open to the invidual prescriber’s professional opinion). All data captured was volunteered, and there was no control or guidance from GW on which patients the prescribers should provide data for and whether prescribers should meet the patient prior to submitting data to the Registry; data could be captured for the same patient at multiple DCPs (Figure 1).
Three years after the Registry started (DCP6), a new questionnaire was introduced to assess the potential for cannabinoid abuse, diversion, and dependence. Prescribers were asked if they had any evidence to suggest their patient was smoking their dose of THC:CBD, consuming larger amounts or for prolonged periods than intended, giving away, selling, or trading their THC:CBD, developing any tolerance, and whether they had observed any evidence of a cannabis-like use disorder (dependence) in their patient. All questions were answered using a 0–10 numerical rating scale, whereby 0= definitely no, 5= unknown, and 10= definitely yes; accordingly, scores of 6–10 were followed up by GW where possible, as they were suggestive of possible abuse, diversion, or dependence. The questions were derived from a Cannabis Withdrawal Scale Questionnaire, which is a validated measure of cannabis withdrawal.12,13 With assistance from the questionnaire’s author, a set of relevant and appropriate questions for this non-interventional/noncomparative study was devised.
After the close of each DCP and the database lock, an independent advisory board consisting of experts in the areas of MS, medical statistics, and pharmacovigilance reviewed the data, in order to document the emerging safety profile of THC:CBD and identify any safety signals; the reports from the board were submitted to the appropriate national competent authorities.
Data presented here are from the patients prescribed THC:CBD in the UK, Germany, and Switzerland up to and including DCP9 cutoff (31 March 2015; 4.5 years) (Figure 1). Some UK patients in the Registry had reported data that predate the market authorization for THC:CBD; this was due to compassionate/named patient use during the premarketing period.
Sample size considerations and statistics
This study is a noncomparative observational registry; no formal sample size calculation was conducted and only descriptive statistics were used. At the point of the initial Marketing Authorization Approval, the MHRA recommended that up to 2,000–3,000 patients treated for at least 1 year should be included in the Registry. There was only one analysis set, the safety analysis set, in which all patients were included; this was used for all statistical summaries. All recorded AEs were coded according to the Medical Dictionary for Regulatory Activities (v13.1). AEs were characterized by seriousness, outcome, and relationship to THC:CBD. Where the yearly incidence rate is shown, this is calculated by dividing the number of patients reporting an event by the total patient-years of THC:CBD exposure in the Registry (2,213.98 years; N=941).
Results
Patient population and demography
The Registry contains data for 941 patients, which are included in this report. Data from 761 UK patients (22% of the eligible population of UK [3,493 patients]) were collected, after which the UK Registry was closed. In Germany, 16 centers have provided data for 178 patients, and in Switzerland, one center has provided data for two patients (Figure 1).
A total of 540 patients (57%) in the Registry were female and 401 patients (43%) were male. The mean age for all patients at the start of THC:CBD administration was 51.2 years (standard deviation [SD] 10.8) (Table 1).
Reasons for prescribing THC:CBD
THC:CBD was prescribed for the treatment of MS in 729 patients (78%), of whom 554 patients (59% of patients in the Registry) were categorized as having a confirmed diagnosis of MS spasticity, 132 patients (14%) had an indication including MS but without mention of spasticity (or spasticity without mention of its cause), and 43 patients (6%) had an indication including probable MS symptoms, but without any mention of MS or spasticity. In 125 cases (13%), THC:CBD was prescribed for indications other than MS (off-label), primarily analgesia; in 87 cases (9%), an indication was not recorded.
Exposure and use of THC:CBD
Duration of exposure to THC:CBD was recorded for 848 patients (90%) and ranged from 1 to 4,289 days, with a mean duration of 954 days (SD 924 days). The total exposure to THC:CBD, for all patients in the Registry, was 2,213.98 patient-years. Overall, 523 patients (62%) had taken THC:CBD for a year or more and 48% of patients had taken it for more than 2 years (Figure 2).
Patients are advised when first prescribed THC:CBD that it might take up to 2 weeks to find an optimal dose and that titration is recommended in order to achieve this. Doses above 12 sprays per day are not recommended, although tolerability and therapeutic dose levels are based on the individual. Daily dose information was recorded for 798 patients (85%); the mean and median doses were 5.4 (SD 4.9) and 4.4 (interquartile range 3.0–7.0) sprays/day, respectively.
Information on the status of THC:CBD use was recorded for 868 patients (92%), the majority of whom (563 [64.9%]) were reported as continuing with THC:CBD, while 305 (35.1%) had stopped. Reasons for stopping THC:CBD were categorized into five groups, with lack of effectiveness (44%) and other/unknown causes (38%; predominantly availability and/or cost issues) being most commonly cited. Also, 25% of patients had reported AEs leading to cessation of THC:CBD. The remaining reasons for stopping THC:CBD were death (8%) and an inability to use the spray (1%); more than a single reason for stopping was provided for some patients.
Perceived benefits of using THC:CBD
A total of 822 patients (87%) had data for whether THC:CBD was providing worthwhile benefit; of these, 680 patients (83%) were considered to be receiving benefit in at least one DCP, with 640 patients (78%) reporting benefit at every DCP (where data had been supplied for two or more DCPs). A total of 40 patients (10%) reported both benefit and no benefit at different DCPs.
Special interest AEs
In response to the main targeted questions in the Registry relating to potential long-term risks, prescribers reported on 288 patients (31%) with events of special interest. Of these, clinically significant AEs were the most common with an incidence of 0.098 per patient-year of THC:CBD exposure, followed by falls that required medical attention (0.028), significant psychiatric or psychotic events (0.025), and suicidal thoughts or attempted suicide (0.007). There were 19 patients (2%) in the Registry who reported a deterioration of driving ability, while 63 patients (7%) reported an improvement (Table 2).
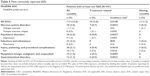
A total of 295 patients (31.3%) in the Registry reported at least one AE (all causalities) at an annual incidence of 0.133 per patient-year of exposure, of which 123 cases were recorded as being treatment related in the opinion of the prescribing physician. The most commonly reported all-causality AEs were in the system organ classes (SOCs) of “nervous system disorders” (117 patients; 12.4% of patients in the Registry), “psychiatric disorders” (68 patients; 7.2%), and “gastrointestinal disorders” (57 patients; 6.1%) (Table 3). Within the psychiatric disorders SOC, depression and depressed mood were reported in 27 (2.9%) and ten patients (1.1%), respectively; the prescribers considered the majority of these depressive events unrelated to THC:CBD. The most common treatment-related AEs were dizziness, reported in 22 patients (2.3%), and fatigue in 16 patients (1.7%) (Table 3), and the time to first onset of an AE was most commonly in the first 28 days of treatment (77 patients; 8.2%) (Table 4).
  | Table 4 AEs presented by incidence and time to first onset category |
There were 113 patients (12%) in the Registry who had at least one serious adverse event (SAE) (all causalities). Of these, 24 patients (2.6%) had SAEs that were reported as treatment related and eleven patients (1.2%) experienced an SAE where no causality was provided by the prescriber. The most common treatment-related SAEs were in the SOCs of “nervous system disorders” (34 patients; 3.6%), “psychiatric disorders” (24 patients; 2.6%), and “infections and infestations” (22 patients; 2.3%). No treatment-related SAE had an incidence of ≥1% by SOC (Table 5).
Thirty-two patients (3.4%) had SAEs leading to an outcome of death in the Registry. One case of lung cancer was reported as being related to THC:CBD treatment (“The remote possibility of a causal link could not be excluded” [verbatim from the prescriber]), although the patient was noted to have a significant confounding factor of heavy smoking. Three cases were missing causality assessment.
Reported overdose or misuse events
A total of 66 patients (7.0%) in the Registry were administering above the maximum recommended daily dose of 12 actuations of THC:CBD per day. Among the 43 patients (4.6%) reported as administering 13–23 actuations per day, AEs considered related to THC:CBD were reported in three patients (one report of paranoia [15 sprays/day], one report of nausea [16 sprays/day], and one report of fatigue [17 sprays/day], whereby the latter two patients discontinued treatment). Among the 23 patients (2.4%) administering 24 actuations or above per day, the majority reported no AEs. Two of these patients reported SAEs considered related to THC:CBD: one patient taking 30 sprays/day (anxiety and fear; dose subsequently reduced to 12 sprays/day) and the other one taking 18 sprays/day (fall; no change to dosage following the event). Following review, GW determined there was no evidence of abuse or persistent patterns of deliberate overdose or misuse in these cases.
Targeted abuse, diversion, and dependence questions
Prescribers submitted data of 427 patients (45%) for the abuse, diversion, and dependence questionnaire. Duration of exposure to THC:CBD was known for 392 of these patients; the mean duration of THC:CBD exposure was calculated as 1,091.7 days, equating to 1,172 patient-years of exposure. In total, 13 patients (3% of respondents) scored between 6 and 10 to any of the questions and were assessed individually by GW. Scores of 7 and 8, related to developing tolerance to THC:CBD, were reported in two patients; however, it was noted that worsening of condition (spasms and pain, respectively) was the possible cause for the observations. Scores of 10 for smoking their THC:CBD and for showing evidence of dependence were reported for two patients; follow-up was incomplete for one patient and for the other it did not suggest a case of abuse, misuse, or psychological dependence. For three of the 13 patients, subsequent follow-up assessments confirmed no scores above 5 and no further action was required.
Discussion
As the Registry was a voluntary observational uncontrolled study, there were a number of limitations. The accuracy of the data collected relied upon the information provided by the reporter, and the data were retrospectively provided by prescribers on a voluntary basis, creating the possibility of bias when answering questions which were left open to interpretation within the CRF. Accordingly, reporting bias must be taken into account when interpreting these data. However, the beneifts of the Registry were that it permitted the collection of safety data over a longer period of time than that in RCTs, and that the data collected were potentially more clincally meaningful as they related to prescribed patients. The targeted questions used in the Registry to address potential safety risks of special interest, including the risk of falls, suicidality, psychosis, abuse liability, and effect on driving, did not identify the safety concerns associated with the long-term use of THC:CBD.
It is widely accepted that MS affects females more, with a ratio of 2:1;1,2 however, the ratio of females to males in the Registry was lower than this (1.3:1). The exact reasons for this discrepancy are unknown, and could reflect a limitation of the Registry in that prescribers may not be reporting on all patients receiving THC:CBD under their care. Interestingly, 61% of the patients specifically prescribed for MS spasticity were female, and the 2:1 ratio was observed within the German MS centers, meaning the off-label use in the UK (albeit considered relatively low [13%]) was a contributing factor.
Daily doses of THC:CBD in short-term RCTs have ranged between 9.4 and 8.3 sprays/day,6–8 while longer-term studies have tended to show lower doses (7.6–4 sprays/day),9,14–16 in keeping with the mean doses in the Registry and supportive of lower doses being more typical in long-term treatment. This should be taken into account in pharmacoeconomic analyses of the use of THC:CBD, and also argues against the emergence of tolerance to THC:CBD.
Just over a third of patients in the registry were reported as permanently stopping THC:CBD; this is lower than has been observed in a large observational prospective study wherein 45% of patients discontinued THC:CBD after 3 months of treatment.17
The most common treatment-related AEs reported in the Registry were dizziness and fatigue; this is in keeping with the safety profiles from other studies, but at lower incidences than previously reported,5–8,10,14 which likely reflects that prescribers were only asked to report what they considered to be clinically significant AEs, rather than all AEs; importantly, the incidence of treatment-related SAEs was very low. No adverse effects relating to long-term cognitive impairment, untoward effect on mood or suicidality, suicidal behavior, and suicidal ideation in patients taking THC:CBD were observed, supporting the findings from a previous 48-week RCT.9 Furthermore, none of the AEs corresponding to the special interest area for THC:CBD (eg, AEs in the nervous system or psychiatric disorders SOC) seemed to occur disproportionately as exposure to THC:CBD increased. It is estimated that up to half of MS patients will experience clinically significant depression at some point in their lifetime.18 In the Registry, 6% of patients reported significant psychiatric events, of which the majority reported depression (approximately 1% of all patients). The long-term follow-up (mean close to 3 years) and the underlying MS must be taken into account when considering this and the other AE reporting figures.
A 2011 UK audit report of services for people with MS previously reported that 14% had attended hospital due to a fall in the previous year,19 which is much higher than that recorded in the Registry (equivalent to 2.8% per year). It, therefore, seems unlikely that THC:CBD is leading to an increase in falls in this patient population, and allows for the hypothesis that treatment with THC:CBD might reduce the rate of medically significant falls.
In the minority of patients who reported a change in driving ability, most saw improvement, thereby supporting previous findings that THC:CBD does not reduce driving ability.20 The reason for this apparent improvement in driving ability is unknown, but may be due to improved spasticity, or cognitive function. Additional studies to further clarify this observation might be useful.
Only a small proportion of responses to the cannabis-like use disorders questionnaire (5%) were deemed potential indicators of abuse or dependence, and follow-up did not identify any patterns of use to suggest that THC:CBD was being abused, misused, or had associated evidence of diversion or dependence. It should, however, be remembered that the reports were solely based on the prescribers’ perceptions, and therefore, this may limit the reliability of the measure. Drug tolerance was not evident in the data, with the overall median dose showing no change over time.
Conclusion
This Registry has provided valuable information characterizing the long-term safety of THC:CBD in the real-world clinical setting. The data recorded to date based on prescriber reports demonstrate that there are no new identified safety issues when compared with the THC:CBD approved prescribing information,21 despite the possible reporting bias due to actively soliciting this information. The benefit-risk profile for THC:CBD remains positive based on these data. Patients use lower doses of THC:CBD in clinical practice than in controlled clinical studies and, based on these data, no evidence of dependence, abuse, diversion, or misuse has emerged in postmarketing use.
Acknowledgments
This research was conducted with the independent review and advice of the Sativex Registry Advisory Board members: Dr Elliot Brown (Chairperson), Director PrimeVigilance Ltd; Prof Peter Thomas, Professor of Health Care Statistics and Epidemiology in Bournemouth University Clinical Research Unit; and Dr Stephen Kirker, consultant in rehabilitation medicine at Cambridge University Hospitals. Appreciation is extended to the members of the Advisory Board for providing their expertise over the 5-year duration of this project.
GW Pharmaceuticals, Cambridge, UK, sponsored the study.
Disclosure
All authors are employees of GW Pharmaceuticals and hold shares in the company. The authors report no other conflicts of interest in this work.
References
Atlas of MS 2013: Mapping multiple sclerosis around the world. Multiple Sclerosis International Federation, London, UK. Available from: http://www.msif.org/about-us/advocacy/atlas/. Accessed December 23, 2015. | ||
Kister I, Bacon TE, Chamot E, et al. Natural history of multiple sclerosis symptoms. Int J MS Care. 2013;15(3):146–158. | ||
Rizzo MA, Hadjimichael OC, Preiningerova J, Vollmer TL. Prevalence and treatment of spasticity reported by multiple sclerosis patients. Mult Scler. 2004;10(5):589–595. | ||
Potter DJ. A review of the cultivation and processing of cannabis (Cannabis sativa L.) for production of prescription medicines in the UK. Drug Test Anal. 2014;6(1–2):31–38. | ||
Wade DT, Makela P, Robson P, House H, Bateman C. Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult Scler. 2004;10(4):434–441. | ||
Collin C, Davies P, Mutiboko IK, Ratcliffe S; Sativex Spasticity in MS Study Group. Randomized controlled trial of cannabis-based medicine in spasticity caused by multiple sclerosis. Eur J Neurol. 2007;14(3):290–296. | ||
Collin C, Ehler E, Waberzinek G, et al. A double-blind, randomized, placebo-controlled, parallel-group study of Sativex, in subjects with symptoms of spasticity due to multiple sclerosis. Neurol Res. 2010;32(5):451–459. | ||
Novotna A, Mares J, Ratcliffe S, et al. A randomized, double-blind, placebo-controlled, parallel-group, enriched-design study of nabiximols (Sativex®), as add-on therapy, in subjects with refractory spasticity caused by multiple sclerosis. Eur J Neurol. 2011;18(9):1122–1131. | ||
Vachová M, Novotná A, Mares J, et al. A multicentre, double-blind, randomised, parallel-group, placebo-controlled study of effect of long-term Sativex® treatment on cognition and mood of patients with spasticity due to multiple sclerosis. J Mult Scler. 2014;1(2):10000122. | ||
Serpell MG, Notcutt W, Collin C. Sativex long-term use: an open-label trial in patients with spasticity due to multiple sclerosis. J Neurol. 2013;260(1):285–295. | ||
Wade DT, Makela PM, House H, Bateman C, Robson P. Long-term use of a cannabis-based medicine in the treatment of spasticity and other symptoms in multiple sclerosis. Mult Scler. 2006;12(5):639–645. | ||
Allsop DJ, Norberg MM, Copeland J, Fu S, Budney AJ. The Cannabis Withdrawal Scale development: patterns and predictors of cannabis withdrawal and distress. Drug Alcohol Depend. 2011;119(1–2):123–129. | ||
Allsop DJ, Copeland J, Norberg MM, et al. Quantifying the clinical significance of cannabis withdrawal. PLoS One. 2012;7(9):e44864. | ||
Koehler J, Feneberg W, Meier M, Pöllmann W. Clinical experience with THC:CBD oromucosal spray in patients with multiple sclerosis-related spasticity. Int J Neurosci. 2014;124(9):652–656. | ||
Oreja-Guevara C, Casanova B, Ordás CM, Silván CV, Asensio D, Massana M. Observational Safety Study of THC: CBD oromucosal spray (Sativex) in multiple sclerosis patients with spasticity. Clin Exp Pharmacol. 2015;5(5):184. | ||
Flachenecker P, Henze T, Zettl UK. Long-term effectiveness and safety of nabiximols (tetrahydrocannabinol/cannabidiol oromucosal spray) in clinical practice. Eur Neurol. 2014;72(1–2):95–102. | ||
Flachenecker P, Henze T, Zettl UK. Nabiximols (THC/CBD oromucosal spray, Sativex®) in clinical practice – results of a multicenter, non-interventional study (MOVE2) in patients with multiple sclerosis spasticity. Eur Neurol. 2014;71(5–6):271–279. | ||
Feinstein A. Multiple sclerosis and depression. Mult Scler. 2011;17(11):1276–1281. | ||
Royal College of Physicians. National Report: The National Audit of Services for People with Multiple Sclerosis; 2011. Available from: https://www.rcplondon.ac.uk/file/958/download?token=7NSA1NCx. Accessed September 19, 2016. | ||
Freidel M, Tiel-Wilck K, Schreiber H, Prechtl A, Essner U, Lang M. Drug-resistant MS spasticity treatment with Sativex(®) add-on and driving ability. Acta Neurol Scand. 2015;131(1):9–16. | ||
Sativex oromucosal spray package leaflet. GW Pharma Ltd; 2015. Available from: http://www.medicines.org.uk/emc/. Accessed December 23, 2015. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.