Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
An interprofessional approach to pressure ulcer prevention: a knowledge and attitudes evaluation
Authors Clarkson P , Worsley PR , Schoonhoven L , Bader DL
Received 21 November 2018
Accepted for publication 12 February 2019
Published 23 May 2019 Volume 2019:12 Pages 377—386
DOI https://doi.org/10.2147/JMDH.S195366
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Paul Clarkson,1,2 Peter R Worsley,1 Lisette Schoonhoven,1,3 Dan L Bader1
1School of Health Sciences, University of Southampton, Southampton, UK; 2Southern Health NHS Foundation Trust, Calmore, UK; 3Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
Background: Pressure ulcers (PUs) are a major burden to individuals, impacting their physical, mental and social wellbeing. While PU prevention is traditionally regarded as a nursing issue, an interprofessional approach has been promoted as best practice. However, little is known about current practice or the knowledge and attitudes of the wider interprofessional team (IPT).
Purpose: Pre-designed questionnaires were used to explore knowledge and attitudes with healthcare staff in the community.
Methods: Questionnaires were disseminated to all healthcare staff within a community healthcare Trust predominantly via an online tool. Data were analyzed using descriptive and inferential statistics.
Results: The median values of all professional groups demonstrated satisfactory attitudes (>75%) and levels of knowledge (>60%) to PU prevention. However, there were differences within and between groups. Management staff demonstrated the most positive attitude to PU prevention (89%), followed by occupational therapists (OTs) and healthcare assistants (HCAs) (87%, IQR: 75%→89%). OTs demonstrated the highest scores for knowledge (69%, IQR: 62%→73%), while healthcare and rehabilitation assistants scored the lowest (58%, IQR: 58%-64%).
Conclusion: This study has demonstrated that the majority of healthcare staff in a UK community setting have satisfactory levels of knowledge and attitudes in relation to PU prevention overall. Nevertheless, there were some differences between groups, albeit non-significant. There were also differences between sub-themes of the questionnaires, indicating a greater focus of pressure ulcer treatment over prevention. While PU prevention is widely regarded to be a nursing issue, these findings provide some indication of the potential for an interprofessional approach.
Keywords: pressure ulcer, interprofessional, knowledge, attitudes, community, questionnaire
Introduction
A pressure ulcer (PU), also known as bed sore, pressure sore, pressure injury or decubitus ulcer, represents “localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear”.1 PUs represent a major burden to populations across the world and have been attributed the highest disability index in a study estimating global burden of skin disease, when compared to other dermatological conditions.2 PUs have a detrimental effect on quality of life, impacting on emotional, physical, mental and social wellbeing.3 The financial impact of PUs is also significant for healthcare organizations and society, with a systematic review by Demarre et al4 reporting treatment cost estimates of between €121 million and €2.59 billion on individual country annual healthcare budgets in six European countries, the USA and Canada.
The overall prevalence of PUs shows wide variation between location and setting.1 A recent addition to such figures includes medical device related PUs (MDRPUs), with one study highlighting that a third of all hospital-acquired PUs in US medical centers were of this origin.5
Nevertheless, some authors have reported a declining prevalence in the acute sector.6–8 One explanation for this may be an increasing emphasis on healthcare delivery in the community setting.9 Consequently, an increase in community-acquired PUs might be predicted, yet little data exists to demonstrate this conclusively.10,11 In the UK community setting, prevalence values have been reported to range between 11% - 13%.11,12
An integrated team-based approach towards PU prevention has long been promoted as best practice,13–15 while conceptually interprofessional teamwork (IPT) is considered to foster interdependency amongst the team, optimizing patient care and improving staff satisfaction.16 However, the implementation of an interprofessional team approach to PU prevention is poorly understood. This may be partly explained through the variation in practice that currently exists in relation to individual professional groups and PUs. For example, while occupational therapists (OTs) and physiotherapists (PTs) in the US, Canada and Australia are widely involved in both treatment and prevention of PUs,17–21 involvement is more varied in other countries. Indeed, this is often limited to specific settings, such as spinal cord injury22 or certain aspects of practice, such as equipment provision, mobilization or with MDRPUs,23–25 and often in support of nursing practitioners. In many countries, nursing is the profession traditionally considered to be responsible for PU-related practice.24 However, the provision of daily care in relation to PUs is often delegated to healthcare assistants.23,26–28
Achieving an interprofessional team approach requires professional groups to have knowledge of the causative factors associated with PUs and strong attitudes towards prevention.29,30 While there is no specific single definition for knowledge,31 it has been considered to encompass three attributes: “experiential”, “skills” and “knowledge claims”.32 Indeed, knowledge is considered to be the foundation for healthcare practice33 and a mediator of behavior.34 Attitude has been defined as the “organization of interrelated beliefs”35,36 (p.1433) and has been significantly correlated with taking preventive action for PUs.29
Both knowledge and attitudes have been explored previously, although predominantly within nursing.29,37–39 For other professional groups, such as doctors, occupational therapists (OTs) and physiotherapists (PTs), knowledge has been reported to be dependent on setting and location.25,40 This was particularly demonstrated in a US study exploring the role of therapists in PU management for people with a spinal cord injury (SCI).41
There is limited consensus related to IPT attitudes. In examining nurses’ attitude to the IPT in PU practice, it was reported that although they were thankful for any assistance, they still adopted the traditional view that it was primarily their responsibility.24 This compares with findings from a UK hospital study, reporting that OTs and PTs demonstrated a positive attitude to PU prevention, although, in practice, they did not consider it to represent their main priority.25 By contrast, OTs in Canada reported greater satisfaction with higher referral rates for PUs as this enabled them to become more involved in a collaborative approach to practice.42 However, it was also highlighted that poor communication and tensions over role identity were barriers to IPT working.43,44
While existing research provides some insight into current practice, no previous studies have explored the collective knowledge and attitudes across the interprofessional team in a community setting. Accordingly, this research aims to explore knowledge and attitudes amongst the IPT towards PU prevention
Material and methods
Study design
A quantitative methodology was adopted using questionnaires as part of a larger multiphase mixed methods design. A convenience sample of healthcare professionals were approached to establish the knowledge and attitudes of a variety of professional groups across the community setting.
Ethical considerations
Approval was gained from the University of Southampton School of Health Sciences Ethics committee (FoHS-ETHICS-10973/20097) and the research and development team in the community location.
Study population
The study sample comprised a variety of both registered and unregistered professional groups, predominantly from one community NHS Trust, including nurses, physiotherapists (PTs), occupational therapists (OTs), podiatrists, healthcare and rehabilitation assistants (HCAs, RAs), other allied health professionals, including speech and language therapists and associate practitioners, and management staff. The community setting in this context included both the provision of healthcare in a patient’s home and in community hospitals. Community hospitals provide a variety of functions in the UK National Health Service (NHS), including inpatient and outpatient services, surgery, minor injury units and can be used by more than one healthcare organization.45 For this study, community hospital participants worked within inpatient and outpatient settings. The community organization where data were collected was split into three divisions – physical health, mental health and learning disability. A link to the questionnaires was sent out widely within each division. Consent was implied through completion of the questionnaires. Data were collected in January 2015.
Data collection
Two questionnaires were administered online and in paper form to explore knowledge and attitudes to PU prevention.33,35 The link to the online questionnaire was sent out by senior managers, area lead clinicians and tissue viability nurses (TVNs), therefore limiting the ability to collect response rate data. A series of demographic questions were included, comprising age, gender, role, clinical years’ experience post registration and division of work.
Knowledge and attitudes questionnaires
The knowledge assessment tool (PUKAT) has 26-items, separated into six categories that represent different areas of knowledge in PU practice (Table 1) and has been demonstrated to have construct validity and good overall internal consistency with nurses (Cronbach’s α: 0.77).33
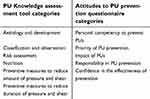 | Table 1 PUKAT and APUP categories. |
The attitude to pressure ulcer prevention questionnaire (APUP) represents a 13-item tool with content that encompasses five categories (Table 1) developed through literature review and double Delphi methodology.35 The APUP has been demonstrated with a nursing cohort to have adequate validity (CVI: 0.87–1.00), while also being reliable (Cronbach’s α: 0.79, ICC: 0.88 (95% CI=0.84–0.91, p<0.001).35 While both questionnaires were designed for nurses, they included topics that are relevant to the wider IPT. A small qualitative pilot was undertaken with a representative sample of staff (n=13) to ensure understanding and acceptability with a wider professional audience. Results indicated that the tools were generally coherent, even though the APUP tool used both positively and negatively worded items and lacked a neutral response as part of the Likert scale.
Data analysis
Questionnaire results were included in the analysis if participants completed either or both of the questionnaires in their entirety. Data were analyzed using descriptive and inferential statistics (median, IQR, Kruskal-Wallis test). The scores were summed and converted to percentage values, with thresholds of 60% for knowledge and 75% for attitudes deemed satisfactory scores.33,35 Data are presented as median scores from the total possible score for the relevant questionnaire followed by the equivalent percentage score.
Results
In total, 119 participants answered the PUKAT questionnaire and 151 participants answering the APUP questionnaire. Of those who answered the APUP questionnaire 92% (n=139) were female, while 55% of participants were aged between 45 and 64 years of age. 144 participants opted to answer further demographics questions, with 62% indicating that they had more than 10 years’ clinical experience. Over 69% of participants (n=105) indicated that they worked in the physical health clinical area, while approximately 16% were based in the learning disability sector. The remaining participants were from the mental health division or did not provide a response to this question. The six podiatrists who indicated “Other” were from a different local Trust. Table 2 provides a breakdown of clinical years’ experience and area of work for participants from both questionnaires.
 | Table 2 Demographics data by questionnaire and profession |
Knowledge
The overall median score achieved across the IPT for the knowledge questionnaire (PUKAT) was 17/26 (65%, IQR: 58% - 79%), representing an above satisfactory level (>60%).33 However, 26% (n=31) of participants did not reach this satisfactory threshold for knowledge. Descriptive statistics show variation between professional groups, with OTs demonstrating the highest score of 18/26 (69%, 65%–73%), and HCAs and RAs achieved the lowest score of 15/26 (58%, 52%–67%) (Table 3). Nevertheless, when these data were collated into four groups, comprising allied health professionals (AHP), RAs, nurses and HCAs, no statistical difference was evident (χ2 (3) =7.179, p=0.066). However, this does show a trend towards AHPs having greater knowledge than their nursing colleagues, with mean rank knowledge scores of 66 and 62, respectively.
 | Table 3 Summary of the PUKAT by profession (maximum score of 26) (other AHPs included speech and language therapists and associate practitioners) |
Overall, participants with more than 20 years’ clinical experience demonstrated the highest knowledge scores, although this trend was not significant (p=0.28). Risk assessment and nutrition represented the highest scoring categories, with registered healthcare staff achieving a median score of 100%, while HCAs and RAs had lower scores (2/3, 67%). The results of the etiology and development sub-theme demonstrated that OTs and PTs scored more highly than nursing, although this was not found to be statistically significant (p=0.433).
Knowledge of preventive measures was generally poor, with a lower than satisfactory overall median score of 6/12 (50%), and no individual professional group achieving a median score (>60%).
Close examination of the answers to specific questions revealed that although all professions achieved satisfactory level scores (>60%) for the etiology and development category, 58% of participants could not identify that a lack of tissue oxygen was a major cause of PU development (Figure 1).
Attitudes
The overall median attitude score was 43/52 (83%, IQR 75%–88%), representing an above satisfactory level (>75%).35 However, 21% (n=31) of participants did not demonstrate this level. The descriptive statistics also demonstrate distinct differences between professional groups (Table 4). Management staff (n=4) demonstrated the most positive attitude with a score of 46/52 (89%), while PTs and rehabilitation assistants (RAs) scored the lowest with a median of 41/52 (79%, IQR: 71%–88%). There was a trend for nursing clinicians to have a more positive attitude than AHPs, although this difference between professional groups was not significant (p>0.05). Years of experience was associated with attitudes towards PU prevention, with nurses, AHPs and RAs with less than 2 years’ experience having the lowest attitude score (73%–75%) relative to more experienced groups.
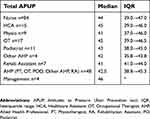 | Table 4 Summary of the APUP by profession (maximum score of 52) |
Priority of PU prevention represented the highest scoring category overall (11/12, 92%). There were differences between groups with nurses, OTs and HCAs feeling more responsible (10.5/12, 87.5%) than PTs, podiatrists and RAs (9/12, 75%). However, even within the nursing and OT cohorts, there was considerable variability in perceived responsibility (Figure 2).
Nursing staff demonstrated the highest median score for the personal competency category (10/12, 83%), although there was a large range in the scores (50%–100%). PTs, OTs, podiatrists, RAs and other AHPs demonstrated the lowest perceived competency values (9/12, 75%). Indeed, some participants were not confident in the effectiveness of PU prevention and demonstrated a belief that PUs are not preventable in high-risk patients. These views were expressed by over 32% of nurses, 11% of OTs and over 62% of HCAs/RAs, as indicated in Figure 3.
Discussion
This is the first study to explore knowledge and attitudes to PU prevention with a variety of professional groups in a UK community setting. The descriptive results demonstrate an overall satisfactory level of knowledge and attitudes across healthcare staff in the community, although unregistered staff, such as HCAs and RAs, did not achieve satisfactory levels of knowledge.
The overall median score for knowledge (65%) represented a higher result than other studies that used the same assessment tool with nurses and nursing assistants. As an example, mean values of 49.6% and 58.9% were reported in Belgium29 and Sweden,46 respectively. As PU practice is traditionally perceived to be the domain of the nursing profession14,24 it might be predicted that their knowledge would be higher than other professions. However, although small variations were seen between individual professions, overall comparison between nurses and AHPs indicated that they held similar levels of knowledge. The median scores for PTs and OTs in this study (67%–69%) are similar to those reported by Worsley and colleagues25 in an acute setting with the same professions (69%). While these results may indicate a response bias in terms of only capturing interested AHPs, they may also collectively increase confidence that AHPs can play an active role in PU prevention. In doing so, professional stereotyping, considered to be an unfavorable perspective leading to insufficient communication between professional groups,47 may be reduced and interprofessional teamwork promoted.48
Results from the knowledge categories appear to highlight a greater focus on treatment as opposed to prevention of PUs, with etiology and classification category scores being higher than preventative measures. Indeed, Panagiotopoulou and Kerr49 and Worsley et al25 both reported similar findings, with preventive strategies representing the lowest scoring category for nurses and OTs/PTs, respectively. Although individual healthcare staff undertook the questionnaires, the focus on treatment over prevention may reflect organizational culture, driven by policy recommendations. Indeed, a recent policy document review highlighted a greater focus on treatment than prevention.50 Given that wound care is currently defined as a nursing responsibility,3 this could impact on interprofessional teamwork.51,52
Although etiology and development were shown to be one of the highest scoring categories, 58% of participants could not identify that a lack of tissue oxygen was a major cause of PU development (Figure 1). Similar findings were also reported in previous studies involving nurses.29,46 Indeed, Gunningberg et al46 suggests that there is confusion about the difference between the terms “cause” and “risk factors”, with participants defining either malnutrition or moisture as a causative factor in PU development. The data from the current study demonstrated that podiatrists were the only professional group that identified tissue oxygen as the primary etiology (100% correct answers).
The overall median score for attitudes (83%) was similar to other studies that used the same questionnaire. For example, Beeckman et al29 reported a mean score of 71% with a sample of nurses and tissue viability nurses in Belgium, while in Sweden and Turkey, nurses demonstrated higher mean scores of 89% and 84%, respectively.53,54 The attitude score of the community nurses in the current study represented a median score of 85%, while three other professional groups demonstrated a more positive attitude, including management staff (89%) and OTs/HCAs (87%). These scores were higher than those reported for AHPs in a recent UK hospital based study using the same tool (median: 81%).25 The positive attitude scores demonstrated by the management staff may reflect their level of experience (10–19 years). A UK study including nurse managers reported similar findings, where greater experience lead to higher perceptions of value in relation to PU prevention.55 However, it is also possible that their attitude scores relate to a particular interest in this area of practice, a desire to reduce adverse events or an awareness of targets in relation to the incidence of PUs.
A less positive attitude was associated with lower levels of experience for nurses, AHPs and RAs. Samuriwo55 reported similar findings through semi-structured interviews with nurses, nurse managers and student nurses, finding that values in relation to PU prevention changed based on the experience of working with someone with a PU. HCAs demonstrated a positive attitude to PU prevention in the current study. However, their knowledge scores were among the lowest of all staffing groups (59.6%). This should represent a concern for current practice, as others have previously indicated that PU-related tasks are often delegated to HCAs.23,27
At the time of data collection, PU related training for staff was not mandatory and although courses were available; this relied heavily on community teams having the capacity to support staff to attend. Ensuring the appropriate cover to do so may have been a challenge, given the previously reported gaps in both the nursing and AHP community workforce.56,57 Given that PUs are traditionally viewed as a nursing domain, it is possible that fewer AHPs attended this training, which may have influenced both the uptake of the questionnaires and the results. Indeed, while AHPs collectively demonstrated the same knowledge as nurses in this study, they may only represent an interested sub-set of these professional groups.
Limitations
This study was conducted in a community NHS Trust with a relatively small sample of healthcare staff. This represents a limitation in terms of the analysis and generalizability of the results. However, the proportion of different staff was broadly representative of the clinical setting and the range of different professional disciplines can be considered a strength. While validation of the knowledge and attitudes assessment tools has only been undertaken with nurses,33,35 the content was considered to be relevant for the wider IPT, confirmed by the pilot study. A greater number of participants undertook the attitudes questionnaire (n=151), than the knowledge questionnaire (n=119). While these were administered as a single online questionnaire, the attitudes section came first, so any participants who were limited by time constraints may have neglected the knowledge section. However, it is also possible that the knowledge-based questions were perceived to be more difficult to answer, creating bias in the data.
Clinical implications
PU prevention is considered to be a priority in clinical practice, yet participants demonstrated a lack of perceived personal competency or confidence in effective prevention. It is, therefore, unsurprising that a proportion of participants considered that PUs were not preventable in high risk patients. Consequently, in light of the deficit in preventive knowledge, an associated impact on the provision of preventive measures in the community could be anticipated. However, this study has shown that knowledge and attitudes in the wider IPT can provide the basis for improved practice by integrating multifaceted knowledge from across professional groups.58 Indeed, interventions for preventing PUs have been linked to the role of a variety of healthcare professionals.41 However, more research is needed to establish collaborative practice and interdependence between professions.59
Conclusion
The findings of this study demonstrate that while PU prevention is considered to be the domain of the nurse, other professional groups exhibited both a strong knowledge and positive attitude toward this clinical challenge. These findings illustrate the potential for an interprofessional approach that utilizes knowledge from across the healthcare team to provide effective prevention. However, a lack of confidence or perceived competency in this area of practice may be limiting collaborative efforts. Future research should use qualitative methods with individual and interprofessional groups to provide further insight and context to these results.
Abbreviation list
PU, Pressure ulcer; IPT, Interprofessional team; IQR, Interquartile range; OT, Occupational Therapist; PT, Physiotherapist; HCA, Healthcare Assistant; SCI, Spinal Cord Injury; RA, Rehabilitation Assistant; TVN, Tissue Viability Nurse; APUP, Attitudes to Pressure Ulcer Prevention tool; PUKAT, Pressure Ulcer Knowledge Assessment Tool; CVI, Content Validity Index; CI, Confidence Interval; AHP, Allied Health Professional; NHS, National Health Service.
Acknowledgments
This work was supported by funding from the University of Southampton and Southern Health NHS Foundation Trust
Disclosure
Mr Paul Clarkson was a clinician in Southern Health NHS Foundation Trust where data collection took place. Professor Lisette Schoonhoven received fees as a consultant in the Scientific Advisory Board from 3M outside the submitted work. The authors report no other conflicts of interest in this work.
References
1.
2. Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi:10.1038/jid.2013.446
3. Spilsbury K, Nelson A, Cullum N, Iglesias C, Nixon J, Mason S. Pressure ulcers and their treatment and effects on quality of life: hospital inpatient perspectives. J Adv Nurs. 2007;57(5):494–504. doi:10.1111/j.1365-2648.2006.04140.x
4. Demarré L, Van Lancker A, Van Hecke A, et al. The cost of prevention and treatment of pressure ulcers: A systematic review. Int J Nurs Stud. 2015;52(11):1754–1774. doi:10.1016/j.ijnurstu.2015.06.006
5. Black JM, Cuddigan JE, Walko MA, Didier LA, Lander MJ, Kelpe MR. Medical device related pressure ulcers in hospitalized patients. Int Wound J. 2010;7(5):358–365. doi:10.1111/j.1742-481X.2010.00699.x
6. Goldberg M. General Acute Care. Washington, DC: NPUAP; 2012.
7. VanGilder C, Amlung S, Harrison P, Meyer S. Results of the 2008–2009 international pressure ulcer prevalence survey and a 3 year, acute care unit-specific analysis. Ostomy Wound Manage. 2009;55(11):39–45.
8. Vangilder C, MacFarlane GD, Meyer S. Results of nine international pressure ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Manage. 2008;54(2):40–5415.
9. Edwards N. Community Services: How They Can Transform Care. London: The King‘s Fund; 2014.
10. Inman C, Firth JR. Pressure sore prevalence in the community. Prof Nurse. 1998;13(8):515–520.
11. Stevenson R, Collinson M, Henderson V, et al. The prevalence of pressure ulcers in community settings: an observational study. Int J Nurs Stud. 2013;50(11):1550–1557. doi:10.1016/j.ijnurstu.2013.04.001
12. Hopkins A, Worboys F. Establishing community wound prevalence within an inner London borough: exploring the complexities. J Tissue Viability. 2015;23(4):121–128. doi:10.1016/j.jtv.2014.10.002
13. Gottrup F, Holstein P, Jørgensen B, Lohmann M, Karlsmar T. A new concept of a multidisciplinary wound healing center and a national expert function of wound healing. Arch Surg. 2001;136(7):765–772.
14. Cramp AFL, Warke K, Lowe-Strong AS. The incidence of pressure ulcers in people with multiple sclerosis and persons responsible for their management. Int J MS Care. 2004;6(2):52–54. doi:10.7224/1537-2073-6.2.52
15. Bergquist-Beringer S, Makosky Daley S. Adapting pressure ulcer prevention for use in home health care. J Wound Ostomy Continence Nurs. 2011;38(2):145–154. doi:10.1097/WON.0b013e31820ad115
16. Xyrichis A, Ream E. Teamwork: a concept analysis. J Adv Nurs. 2008;61(2):232–241. doi:10.1111/j.1365-2648.2007.04496.x
17.
18.
19.
20. Houghton P, Campbell K, Panel C. Canadian best practice guidelines for the prevention and management of pressure ulcers in people with spinal cord injury. Res Handb Clin. 2013. Available from: http://onf.org/system/attachments/168/original/Pressure_Ulcers_Best_Practice_Guideline_Final_web4.pdf. Accessed September 27, 2017.
21. McCulloch JM. The role of physiotherapy in managing patients with wounds. J Wound Care. 1998;7(5):241–244.
22. Coggrave M, Rose L. A specialist seating assessment clinic: changing pressure relief practice. Spinal Cord. 2003;41:692–695. doi:10.1038/sj.sc.3101527
23. Sving E, Gunningberg L, Högman M, Mamhidir A-G. Registered nurses‘ attention to and perceptions of pressure ulcer prevention in hospital settings. J Clin Nurs. 2012;21(9/10):1293–1303. doi:10.1111/j.1365-2702.2011.04000.x
24. Samuriwo R. Pressure ulcer prevention: the role of the multidisciplinary team. Br J Nurs. 2012;21:S4–s13. doi:10.12968/bjon.2012.21.Sup5.S4
25. Worsley PR, Clarkson P, Bader DL, Schoonhoven L. Identifying barriers and facilitators to participation in pressure ulcer prevention in allied healthcare professionals: a mixed methods evaluation. Physiotherapy. 2016;103(3):304–310. doi:10.1016/j.physio.2016.02.005
26. Samuriwo R. The impact of nurses‘ values on the prevention of pressure ulcers. Br J Nurs. 2010a;19(15):S4–s14. doi:10.12968/bjon.2010.19.Sup5.77702
27. Athlin E, Idvall E, Jernfält M, Johansson I. Factors of importance to the development of pressure ulcers in the care trajectory: perceptions of hospital and community care nurses. J Clin Nurs. 2010;19(15–16):2252–2258. doi:10.1111/j.1365-2702.2009.02886.x
28. Buss IC, Halfens RJG, Abu-Saad HH, Kok G. Pressure ulcer prevention in nursing homes: views and beliefs of enrolled nurses and other health care workers. J Clin Nurs. 2004;13(6):668–676. doi:10.1111/j.1365-2702.2004.00953.x
29. Beeckman D, Defloor T, Schoonhoven L, Vanderwee K. Knowledge and attitudes of nurses on pressure ulcer prevention: a cross-sectional multicenter study in belgian hospitals. Worldviews Evid-Based Nurs. 2011;8(3):166–176. doi:10.1111/j.1741-6787.2011.00217.x
30. Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez-Medina IM, Lopez-Ortega J. Pressure ulcer care in Spain: nurses‘ knowledge and clinical practice. J Adv Nurs. 2007;58(4):327–338. doi:10.1111/j.1365-2648.2007.04236.x
31. Bolisani E, Bratianu C. The elusive definition of knowledge. In: Bolisani E, Bratianu C, editors. Emergent Knowledge Strategies: Strategic Thinking in Knowledge Management. Cham: Springer International Publishing; 2018:1–22.
32. Dombrowski E, Rotenber L, Bick M. Theory of Knowledge. Oxford, UK: Oxford University Press; 2013.
33. Beeckman D, Vanderwee K, Demarré L, Paquay L, Van Hecke A, Defloor T. Pressure ulcer prevention: development and psychometric validation of a knowledge assessment instrument. Int J Nurs Stud. 2010b;47(4):399–410. doi:10.1016/j.ijnurstu.2009.08.010
34. Ajzen I, Madden TJ. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. J Exp Soc Psychol. 1986;22(5):453–474. doi:10.1016/0022-1031(86)90045-4
35. Beeckman D, Defloor T, Demarré L, Van Hecke A, Vanderwee K. Pressure ulcers: development and psychometric evaluation of the attitude towards pressure ulcer prevention instrument (APuP). Int J Nurs Stud. 2010a;47(11):1432–1441. doi:10.1016/j.ijnurstu.2010.04.004
36. Rockeach M. Attitude change and behavioral change. Public Opin Q. 1966;30:529–550. doi:10.1086/267454
37. Aydin AK, Karadag A. Assessment of nurses‘ knowledge and practice in prevention and management of deep tissue injury and stage I pressure ulcer. J Wound Ostomy Continence Nurs. 2010;37(5):487–494. doi:10.1097/WON.0b013e3181edec0b
38. Simonetti V, Comparcini D, Flacco ME, Di Giovanni P, Cicolini G. Nursing students‘ knowledge and attitude on pressure ulcer prevention evidence-based guidelines: A multicenter cross-sectional study. Nurse Educ Today. 2015;35(4):573–579. doi:10.1016/j.nedt.2014.12.020
39. Strand T, Lindgren M. Knowledge, attitudes and barriers towards prevention of pressure ulcers in intensive care units: a descriptive cross-sectional study. Intensive Crit Care Nurs. 2010;26(6):335–342. doi:10.1016/j.iccn.2010.08.006
40. Kimura S, Pacala JT. Pressure ulcers in adults: family physicians‘ knowledge, attitudes, practice preferences, and awareness of AHCPR guidelines. J Fam Pract. 1997;44(4):361–368.
41. Guihan M, Hastings J, Garber SL. Therapists‘ role in pressure ulcer management in persons with spinal cord injury. J Spinal Cord Med. 2009;32(5):560–567.
42. Giesbrecht E. Pressure ulcers and occupational therapy practice: a Canadian perspective. Can J Occup Ther. 2006;73(1):56–63. doi:10.2182/cjot.05.0011
43. Macens K, Rose A, Mackenzie L. Pressure care practice and occupational therapy: findings of an exploratory study. Aust Occup Ther J. 2011;58(5):346–354. doi:10.1111/j.1440-1630.2011.00962.x
44. Rose A, Mackenzie L. ‘Beyond the cushion‘: a study of occupational therapists‘ perceptions of their role and clinical decisions in pressure care. Disability Rehabil. 2010;32(13):1099–1108. doi:10.3109/09638280903410748
45. Pitchforth E, Nolte E, Corbett J, et al. Community Hospitals and Their Services in the NHS: Identifying Transferable Learning from International Developments – Scoping Review, Systematic Review, Country Reports and Case Studies. 2017. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28682573. Accessed September 27, 2017.
46. Gunningberg L, Mårtensson G, Mamhidir A-G, Florin J, Å MA, Bååth C. Pressure ulcer knowledge of registered nurses, assistant nurses and student nurses: a descriptive, comparative multicentre study in Sweden. Int Wound J. 2013;12(4):462–468. doi:10.1111/iwj.12138
47. Ryan AA, McKenna HP. A comparative study of the attitudes of nursing and medical students to aspects of patient care and the nurse‘s role in organizing that care. J Adv Nurs. 1994;19(1):114–123.
48. West M, Slater J. Teamworking in Primary Health Care: A Review of Its Effectiveness. London: Health Education Authority; 1996.
49. Panagiotopoulou K, Kerr SM. Pressure area care: an exploration of Greek nurses‘ knowledge and practice. J Adv Nurs. 2002;40(3):285–296.
50. Jackson D, Hutchinson M, Barnason S, et al. Towards international consensus on patient harm: perspectives on pressure injury policy. J Nurs Manag. 2016;24(7):902–914. doi:10.1111/jonm.12396
51. Bloor G, Dawson P. Understanding professional culture in organizational context. Organ Stud. 1994;15(2):275–295. doi:10.1177/017084069401500205
52. Nancarrow SA, Booth A, Ariss S, Smith T, Enderby P, Roots A. Ten principles of good interdisciplinary team work. Hum Resour Health. 2013;11:19. doi:10.1186/1478-4491-11-19
53. Florin J, Baath C, Gunningberg L, Martensson G. Attitudes towards pressure ulcer prevention: a psychometric evaluation of the Swedish version of the APuP instrument. Int Wound J. 2014;13(5):655–662.
54. Aslan A, Yavuz van Giersbergen M. Nurses‘ attitudes towards pressure ulcer prevention in Turkey. J Tissue Viability. 2016;25(1):66–73. doi:10.1016/j.jtv.2015.10.001
55. Samuriwo R. Effects of education and experience on nurses‘ value of ulcer prevention. Br J Nurs. 2010b;19:S8–s18. doi:10.12968/bjon.2010.19.Sup10.79689
56. Pinkney L, Nixon J, Wilson L, et al. Why do patients develop severe pressure ulcers? A retrospective case study. BMJ Open. 2014;4:1. doi:10.1136/bmjopen-2013-004303
57. Dorning H, Bardsley M. Quality Watch. Focus on Allied Health Professionals. London: Nuffield Trust/The Health Foundation; 2014.
58. Firth-Cozens J. Celebrating teamwork. Qual Health Care. 1998;7:S3–S7.
59. Skjørshammer M. Co-operation and conflict in a hospital: interprofessional differences in perception and management of conflicts. J Interprof Care. 2001;15(1):7–18.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



