Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
An Empirical Study of Feedforward Control in Unplanned Extubation of Nasogastric Tube
Authors Ma H, Pan H, Dong X, Li L
Received 15 February 2023
Accepted for publication 17 May 2023
Published 25 May 2023 Volume 2023:16 Pages 1465—1471
DOI https://doi.org/10.2147/JMDH.S408676
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hexing Ma,1 Hailong Pan,2 Xiangxiang Dong,2 Lingyu Li2
1Department of General Surgery, Affiliated Hospital of Yangzhou University, Yangzhou, 225007, People’s Republic of China; 2Department of Major Surgery, Affiliated Hospital of Yangzhou University, Yangzhou, 225007, People’s Republic of China
Correspondence: Lingyu Li, Department of Major Surgery, Affiliated Hospital of Yangzhou University, Yangzhou, 225007, People’s Republic of China, Tel +86 15861356494, Fax +86 514-87213549, Email [email protected]
Objective: To explore the effect of feedforward control on reducing the incidence of unplanned extubation and improving the quality of catheter nursing.
Methods: A total of 186 patients with nasogastric tube after gastrointestinal surgery in the eastern region of our hospital from September 2020 to September 2021 were selected as the control group; 186 patients with nasogastric tube after gastrointestinal surgery in the western region of our hospital at the same period were selected as the experimental group. The influencing factors of unplanned extubation in patients with long-term postoperative nasogastric tube were analyzed, and effective preoperative and postoperative health education was conducted. The ratio of unplanned extubation of nasogastric tube and nursing satisfaction of patients in the two groups were compared.
Results: Patient constraint, perceived pressure score, anxiety score, nasal gastrointestinal canal health education feedback score and indwell tube comfort score were independent risk factors for unplanned extubation. The restraint rate and the incidence of unplanned extubation in the experimental group were lower than those in the control group after intervention, with statistical significance (P < 0.05). The nursing satisfaction of the experimental group was significantly higher than that of the control group after feedforward cognitive intervention. After intervention, serum albumin and gastric PH in the experimental group were significantly higher than those in the control group (P < 0.05).
Conclusion: The safe nursing management method of feed forward control can effectively reduce the incidence of unplanned extubation in inpatients, which is worth further promoting in nursing work.
Keywords: feedforward control, unplanned extubation, nasogastric tube, health education
Introduction
Due to the need of postoperative treatment after our surgery, many patients need to retain the nasogastric tube to promote the recovery of the disease. One more tube on the patient will increase the infection rate and our nursing staff will have more worries about unplanned extubation. Any unplanned adverse event of extubation will cause physical pain, increase economic burden and even endanger your life.1 Feedforward control, in fact, is to collect information before the start of management, prevent and correct possible problems, and then take the corresponding measures to prevent them to the extent required to achieve the intended purpose.2 In recent years, the feedforward control management method has also been widely used in the field of clinical patient care.3–6 Luo has found that feedforward control can reduce the incidence of perioperative risk events and complications of elderly patients, and improve nursing quality and satisfaction.7 To examine the effectiveness of feedforward control, this comparative study takes the patients with nasogastric tube after surgery as the research object, analyzes the risk factors of unplanned extubation, and gives such patients nursing intervention based on the concept of feedforward control management, which has achieved good results.
Materials and Methods
General Information
One hundred and eighty-six patients with nasogastric tube after surgery in the eastern region of Affiliated Hospital of Yangzhou University from September 2020 to September 2021 were selected as the control group; At the same time, 186 patients with nasogastric tube after surgery in the western region of Affiliated Hospital of Yangzhou University were selected as the experimental group. This study was conducted in accordance with the declaration of Helsinki and with approval from the Ethics Committee of Affiliated Hospital of Yangzhou University (NO. YZUHL2020021). Written informed consent was obtained from all participants.
Inclusion criteria: ① Those who are expected to undergo surgery and have retained nasogastric tube or nasogastric tube; ② Patients without history of mental illness and consciousness disorder; ③ Obtain the informed consent of the patient and be willing to participate in the study; ④ The nasogastric tube of the patient is fixed and the identification is consistent. Exclusion criteria: ① mental retardation or severe cognitive impairment cannot cooperate with researchers; ② Those with a history of serious mental illness or family disease; ③ Unconscious person; ④ Unplanned unplugging due to incorrect location.
Methods
In the Control Group, the Patients Received Conventional Nursing Methods
In the control group, routine nursing was carried out and proper restraint was adopted. The nurses strengthened the patrol of patients with extubation risk.
In the Experimental Group, All Patients Received Relevant Nursing Measures of Feedforward Cognitive Intervention on the Basis of the Control Group
The nurse will carry out pre-operation health education for the patients and their families. After the education, the patient or family members will be asked to repeat the content of the education to ensure that they have understood the importance of retaining the nasogastric tube. The contents of the education mainly include: introducing the purpose of intubation, the relationship between intubation and disease treatment, the importance of early enteral nutrition, the possible discomfort after intubation and the consequences of extubation, etc. to the patients and their families in detail. And we will take the restrictive measures to make the patients cognitively accept intubation after the operation. We will also inform patients and their families of the common reasons for unplanned extubation and the common time period of extubation according to our experience, so that they can pay additional attention.
Observation Indicators
Inpatient Nursing Satisfaction Scale
The scale has five dimensions, including health education, medical facilities, safety management, timeliness of service, and humanistic care. It contains 19 items.8 It is evaluated with a 5-level scoring method of 1–5 points, representing satisfaction, partly satisfaction, general, dissatisfaction, and extremely dissatisfaction, with a total score of 19–95 points. The Cronbach’s alpha is 0.935. The higher the score, the better the satisfaction of nursing service.
Feedback Score of Nasogastric Health Education
This questionnaire was designed by ourselves. The main items included patients’ understanding of the role of nasogastric tube, the fixation method and the risk caused by extubation. Select 10 experts who were engaged in clinical nursing and medical work in relevant departments to revise the questionnaire, and analyze whether the questionnaire is consistent with the purpose of the survey, and put forward suggestions for revision. The CVI coefficient of the internal validity is 0.954. It has good surface validity and content validity.
Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS)
Self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used for evaluation.9–11 The two scales both contain 20 items, with 1–4 points from “no”, “sometimes”, “most of the time”, and “frequently”, with a total score of 0–80 points. SAS is bounded by 50 points. The higher the score is, the more serious the anxiety is. The Cronbach’s alpha is 0.911, and the CVI value of content validity is 0.810. SDS is bounded by 53 points. The higher the score of >53 points, the more serious the depression of the patient. The Cronbach’s alpha is 0.927, and the CVI value of content validity is 0.826.
Comfort Assessment Form of Retained Tube
Each indicator in the table is divided into three levels: ① none; ② Mild, but acceptable; ③ Unbearable.12 Observe the comfort degree of the two groups of patients, and compare whether there was statistical significance in nasopharynx pain, thirst degree, nausea and vomiting, ear pain, reflux and other aspects.
SF-36 Scale
It includes 36 items and is divided into 8 dimensions, including physical health (PF), social function (SF), role limits due to physical health problems (RP), body pain (BP), mental health (MH), role limits due to emotional problems (RE), vitality (VT) and general health (GH). Each dimension contains 2~10 entries.13
Perceived Stress Scale
It includes two dimensions of sense of control and sense of tension, with a total of 14 items.14,15 The Likert 5-grade scoring method was used. Seven items in the scale were scored in reverse, with a score range of 14 to 70 points. The higher the score, the greater the pressure the patient felt. The Cronbach’s alpha is 0.872.
Patients Constrained
The patient must be evaluated and made a decision before starting constraint. During the implementation of the constraint, attention should be paid to ensuring the safety of the patient, doing a good job in observing the condition, maximizing the comfort of the patient, and taking measures to distract the patient. Evaluate whether it is necessary to continue the constraint, and evaluate the condition and result of the constraint. No matter how many times a patient is constrained, it is defined as a constrained patient.
Statistical Methods
SPSS22.0 statistical processing software was used. The measurement data were expressed by mean ± standard deviation ( ). F-test was used for inter-group comparison, and t-test was used for two independent samples. The counting data were expressed as percentages (%), with comparisons made by means of the χ2 test. Rank sum test was used to grade data of nursing satisfaction, and the possible influencing factors were analyzed by binary unconditional logistic regression based on single factor analysis. A value of P < 0.05 was considered to be statistically significant.
). F-test was used for inter-group comparison, and t-test was used for two independent samples. The counting data were expressed as percentages (%), with comparisons made by means of the χ2 test. Rank sum test was used to grade data of nursing satisfaction, and the possible influencing factors were analyzed by binary unconditional logistic regression based on single factor analysis. A value of P < 0.05 was considered to be statistically significant.
Results
Basic Clinical Characteristics of Research Subjects
There is no significant difference between the two groups in general information, including age, sex, education, drinking and smoking, marital status, and family genetic history (P > 0.05) (Table 1).
 |
Table 1 Baseline Characteristics Description and Comparison Between the Control Group and the Study Group |
Univariate Analysis of Unplanned Extubation
Compared with the group without unplanned extubation, the constituent ratio of constraint, perceived pressure score, anxiety score, nasogastric intestinal health education feedback score, and indwelling comfort of patients with unplanned extubation increased significantly (P < 0.05), as shown in Table 2.
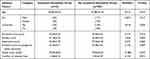 |
Table 2 Univariate Analysis of Unplanned Extubation in Patients |
Logistic Regression Analysis of Risk Factors for Unplanned Extubation
Two-category non-conditional logistic regression analysis was carried out on the risk factors with statistical significance screened out in univariate analysis. The results showed that patients’ constraint, perceived pressure score, anxiety score, depression score, nasogastric intestinal health education feedback score, and indwelling tube comfort were independent risk factors for patients’ unplanned extubation (P < 0.05), as shown in Table 3.
 |
Table 3 Relevant Results in Logistic Regression Analysis of Risk Factors for Unplanned Extubation |
Comparison of Restraint Rate and Unplanned Extubation Rate Between the Two Groups
The restraint rate and unplanned extubation rate of patients in the experimental group were lower than those in the control group after the feedforward cognitive intervention (P < 0.05), as shown in Table 4.
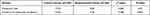 |
Table 4 Comparison of the Incidence of Unplanned Extubation Between the Two Groups (%) |
Comparison of Nursing Satisfaction Between the Two Groups
The nursing satisfaction of patients in the experimental group after feedforward cognitive intervention was significantly higher than that in the control group (P < 0.05), as shown in Table 5.
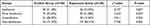 |
Table 5 Comparison of Nursing Satisfaction Between the Two Groups After Intervention [n (%)] |
Discussion
Unplanned extubation refers to the patient pulling out the pipe without the consent of the medical staff, and also includes the extubation caused by improper medical operation.16,17 According to statistics, 296 nursing adverse events occurred in the East and West region of our hospital from December 2018 to June 2020, of which 49 were unplanned extubation, accounting for 17.75%. The results cannot be ignored. It is urgent to solve this problem. Feedforward control, also known as advance or preventive control, refers to predicting the consequences of management activities and taking preventive measures before management to avoid possible deviations.18,19 The application of feedforward control in the medical field can minimize the risk of patients and ensure that the care they receive conforms to their best interests.20 One study shows that the number of patients involved in ICU catheters decreased from 55 to 23 after the implementation of feedforward control system, which indicates that feedforward control management can also be used as an effective method for ICU nurses to manage catheters.21 The research results show that patient constraint, perceived stress score, anxiety score, feedback score of nasogastric intestinal health education, and comfort of retained tube are independent risk factors for unplanned extubation. Reasonable use of constraint measures can shift the patient’s focus, indirectly enhance the patient’s understanding of the tube and nursing awareness, play a role in relieving negative emotions, and reduce the incidence of spontaneous extubation.22,23 Patients with long-term nasogastric intestinal tube are prone to fear, irritability, anxiety and other negative psychology. This study adopts feedforward cognitive intervention to explain the disease and relevant knowledge of gastric tube indwelling to patients, which can help patients understand the importance and necessity of gastric tube indwelling during treatment, thus effectively reducing the occurrence of accidental extubation.24 Research shows that it can prevent patients with gastrointestinal tube from suffering from dry throat, swelling and pain, so as to reduce the incidence of accidental extubation, improve their comfort during postoperative intubation, and ensure nursing safety.25 The study also showed that the constraint rate and unplanned extubation rate in the experimental group were lower than those in the control group after intervention. The nursing satisfaction in the experimental group after feedforward cognitive intervention was significantly higher than that in the control group. It may be related to the feedforward cognitive intervention, which reduces the unplanned extubation rate, reduces the treatment costs, reduces the economic burden of patients and families, and improves the nursing satisfaction.17
Limitation
Because this study is not a randomized controlled study, and there are individual differences in the study, different selection results lead to bias. In the future, a larger randomized controlled study is needed to confirm the results of this study and determine whether there are other factors affecting the results; only in this way will we be able to draw firmer conclusions.
Conclusion
To sum up, the safety nursing management method of feedforward cognitive intervention has increased the communication between nurses and patients, improved the quality of catheter care and the comfort of patients with indwelling catheter, reduced the hospitalization costs, increased the awareness about the harm of unplanned extubation and the importance of catheter for disease rehabilitation, and enhanced their self-protection awareness to reduce the incidence of unplanned extubation in hospitalized patients. It is worthy of further promotion and application in nursing work.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Affiliated Hospital of Yangzhou University. Written informed consent was obtained from all participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study is funded by the “Care for Fragrance” Fund of the Key Laboratory of Zoonosis in Jiangsu Province in 2020 (Project No.: HX2007).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Motta APG, Rigobello MCG, Silveira RC, Gimenes FRE. Nasogastric/nasoenteric tube-related adverse events: an integrative review. Rev Lat Am Enfermagem. 2021;29:e3400. doi:10.1590/1518-8345.3355.3400
2. Man APN, Lam CKM, Cheng BCP, Tang KS, Tang PF. Impact of locally adopted simulation-based crew resource management training on patient safety culture: comparison between operating room personnel and general health care populations pre and post course. Am J Med Qual. 2020;35(1):79–88. doi:10.1177/1062860618824863
3. Ma DF, Wu JY, Wang YT, Yi WY. Application of detail management in nursing safety management in operating room. Minerva Med. 2020. doi:10.23736/S0026-4806.20.07107-4
4. Labrague LJ. Influence of nurse managers’ toxic leadership behaviours on nurse-reported adverse events and quality of care. J Nur Manag. 2020;29(4):855–863. doi:10.23736/S0026-4806.20.07107-4
5. Liu GP. The value evaluation of PDCA cycle method in nursing quality management of gynecological tumor endoscopic surgery. Chin J Cancer Prev Treat. 2019;26(S1):245–247.
6. Ma L, Yuan Y, Wang X. Effect of a feedforward control model on nursing attitudes in the operating room. J Multidiscip Healthc. 2022;15:2399–2406. doi:10.2147/JMDH.S377581
7. Meiyi L, Jie H, Aidi L. Application of multidisciplinary cooperation in risk feedforward control of surgical nursing for elderly patients. Qilu J Nurs. 2020;26(2):101–103. doi:10.3969/j.issn.1006-7256.2020.02.034
8. Bo G, Yijuan C, Jun Z. Development of inpatient nursing satisfaction scale. China Nurs Manage. 2006;6(10):17–19. doi:10.3969/j.issn.1672-1756.2006.10.005
9. Zung WWK. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi:10.1016/S0033-3182(71)71479-0
10. Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20(1):90. doi:10.1186/s12888-019-2427-6
11. Zung W. Self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi:10.1001/archpsyc.1965.01720310065008
12. Anqiong Z. Discussion on nursing methods for patients with long-term gastric tube retention. Sichuan Med J. 2006;27(4):432. doi:10.3969/j.issn.1004-0501.2006.04.059
13. Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14(3):875–882. doi:10.1007/s11136-004-1014-5
14. Graves BS, Hall ME, Dias-Karch C, Haischer MH, Apter C. Gender differences in perceived stress and coping among college students. PLoS One. 2021;16(8):e0255634. doi:10.1371/journal.pone.0255-634
15. Furman M, Joseph N, Miller-Perrin C. Associations between coping strategies, perceived stress, and health indicators. Psi Chi J Psychol Res. 2018;23(1):61–72. 10.24839/2325–7342.jn23.1.61. doi:10.24839/2325-7342.JN23.1.61
16. Torres GM, Nascimento ER, Hermida PMV, Malfussi LBH, Galetto S. Care for unplanned extubation prevention: analysis of the validity of an instrument’s content. Rev Bras Enferm. 2021;74(1):e20180998. doi:10.1590/0034-7167-2018-0998
17. Liu K, Liu Z, Li LQ, Zhang M, Deng XX, Zhu H. Predictive value of the unplanned extubation risk assessment scale in hospitalized patients with tubes. World J Clin Cases. 2022;10(36):13274–13283. doi:10.12998/wjcc.v10.i36.13274
18. Du J. Application effect of feedforward control in the nursing safety management of operating room. Clin Res Pract. 2017;2(5):158–159. doi:10.19347/j.cnki.2096-1413.201705084
19. Song LF, Xu RX. Intervention strategies for the management of nosocomial infection among cleaning staff in the operating room. Chin J Nosocomiol. 2013;23(12):2963–2964.
20. Allen RW, Taaffe KM, Neilley V, Busby E. First case on-time starts measured by incision on-time and no grace period: a case study of operating room management. J Healthc Manag. 2019;64(2):111–121. doi:10.1097/JHM-D-17-00203
21. Lu PP, Li N, Zhang LN. Influence of feedforward control model on nursing error behavior and nursing attitude of nurses in operating room nursing management. Shanxi Med J. 2022;51(13):1535–1537. doi:10.3969/j.issn.0253-9926.2022.13.034
22. Hur S, Min JY, Yoo J, et al. Development and validation of unplanned extubation prediction models using intensive care unit data: retrospective, comparative, machine learning study. J Med Internet Res. 2021;23(8):e23508. doi:10.2196/23508
23. Ai ZP, Gao XL, Zhao XL. Factors associated with unplanned extubation in the Intensive Care Unit for adult patients: a systematic review and meta-analysis. Intensive Crit Care Nurs. 2018;47:62–68. doi:10.1016/j.iccn.2018.03.008
24. Na S. Effect of comprehensive nursing on the incidence of accidental extubation and negative psychology of patients with indwelling gastric tubes. Psychol Magazine. 2021;16(13):141–142. doi:10.19738/j.cnki.psy.2021.13.064
25. Yu. J. The effect of lidocaine aerosol inhalation on the throat comfort of patients with gastrointestinal tube. Electron J Pract Clin Nurs Sci. 2018;3(34):76–77. doi:10.3969/j.issn.2096-2479.2018.34.065
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
