Back to Journals » Journal of Asthma and Allergy » Volume 13
An Asthma Specialist’s Consult Letter: What Do Parents Think About Receiving a Copy?
Authors Amirav I , Vandall-Walker V , Rasiah J , Saunders L, Belur H, Sahlin B, Roduta Roberts M , Redlich-Amirav D
Received 15 February 2020
Accepted for publication 19 April 2020
Published 8 May 2020 Volume 2020:13 Pages 179—186
DOI https://doi.org/10.2147/JAA.S249893
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amrita Dosanjh
Israel Amirav,1,* Virginia Vandall-Walker,2,3,* Jananee Rasiah,2,3 Laura Saunders,4 Harsha Belur,4 Brenda Sahlin,4 Mary Roduta Roberts,5 Dorit Redlich-Amirav6
1Department of Pediatrics, University of Alberta, Edmonton, Alberta, Canada; 2Patient Engagement Platform, Alberta SPOR Support Unit, Edmonton, Alberta, Canada; 3Faculty of Health Disciplines, Athabasca University, Athabasca & Faculty of Nursing, University of Alberta, Edmonton, Alberta, Canada; 4Parent Advisory Council, Edmonton, Alberta, Canada; 5Department of Occupational Therapy, University of Alberta, Edmonton, Alberta, Canada; 6Faculty of Rehabilitation Medicine, University of Alberta, Edmonton, Alberta, Canada
*These authors contributed equally to this work
Correspondence: Israel Amirav
Pediatric Pulmonology Unit, Dana-Dwek Children’s Hospital, Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
Tel +1 972-55-664-9359
Email [email protected]
Objective: Written summaries about visits with general practitioners’ have influenced increased patient knowledge, satisfaction, recollection, and compliance, and strengthened the doctor–patient relationship. All previous studies about this communication pre-dated the electronic medical record (EMR) era, and none examined views from parents of children with asthma. We explored parents’ perceptions about receiving a hard copy summary Letter immediately following the visit, with the pediatric asthma specialist about findings and the care plan for their child.
Methods: A Parent Advisory Council helped inform this pilot study, an observational cross-sectional electronic survey. Each Letter included a comprehensive summary of the child’s visit with the specialist.
Results: Previous findings from patients about the benefits of receiving this Letter were strongly supported by data from 51 participants. Interestingly, more than 54% of respondents preferred receiving a hard copy Letter over an electronic copy, and 98% wanted other clinicians to adopt this practice.
Conclusion: Parents of children with asthma value and want timely written information of this nature from other clinicians.
Practice Implications: These results can influence further asthma research to promote a change in the perceptions of clinicians, parents, and patients about timely access to health information in the EMR era.
Keywords: patient perspectives, provider–patient communication, asthma, parents
Highlights
In this study, we explored parents’ perceptions about receiving a hard copy of an asthma specialist’s summary EMR letter at the end of the consult visit.
What’s Known on This Subject
Sharing written communication following an asthma specialists’ visit with adult patients has influenced an increase in their knowledge, recollection, compliance, and satisfaction with care. To date, all previous studies about this communication pre-date the electronic medical record (EMR) era, and none examined views from parents of children with asthma.
What This Study Adds
Parents value and want to receive a hard copy of their child’s asthma specialist’s EMR-generated summary letter at the end of the visit. They would like to receive information of this nature in the future from other clinicians.
Introduction
Development of care partnerships with parents, caregivers, and children, a goal of pediatric patient and family-centred care, have informed and improved the quality of pediatric self-management alliances and programs, including those targeted toward children with asthma.1 Specifically, improved oral and written communication by physicians in pediatric asthma care have increased patients’ satisfaction, improved health outcomes, reduced unnecessary use of health-care resources,2,3 and enhanced patient adherence4 to treatment. Providing parents with copies of General Practitioners’ (GP) referral requests5,6 to specialists, or specialists’ summary Letters immediately at the end of the child’s visit, for later review and discussion, are family-centred care practices. Recent technological advancements such as the availability of electronic medical records (EMRs) can assist parents and clinicians to more readily access and share health information with each other in a timely manner.
Since 2000, the National Health Service (NHS) in the United Kingdom (UK) has recommended that clinicians’ share Letters with patients to increase patient satisfaction and improve compliance,7 and to strengthen the doctor–patient relationship.8–10 Patients have reported a high-level of satisfaction with, and understanding of, the content included in these Letters, an overall positive feeling about receiving them,11–14 and better recollection of visit discussions.7,15 Perkins16 conducted a survey and found that patients who received Letters, asked more focused questions at subsequent appointments and followed treatment recommendations more closely because they had greater understanding of those recommendations. Of particular note is the finding that improved communication did not lengthen consultation times.17
The studies cited were conducted in the pre-EMR era, and none solicited views from parents or caregivers of children with respiratory disorders. To address this knowledge gap in current pediatric respiratory practice, we conducted a pilot study to examine the perspectives of parents (term used throughout and inclusive of caregivers) who received an EMR-generated hard copy Letter (the “Letter”) from one pediatric pulmonologist at the end of their child’s consult visit for asthma. The Letter, addressed to the referring GP, included a summary of the child’s presenting condition, medical history, physical exam, and recommendations for treatment, and was part of the pediatric pulmonologist routine practice. The objectives of this pilot study were to: (1) survey parents’ perceptions about receiving a hard copy of this Letter at the end of their child’s consult visit; (2) explore parents’ reasons for reading the Letter; and (3) determine whether parents wanted to receive this type of communication, and how, from other clinicians.
Methods
Aim, Setting, and Design
The aim of this pilot study was to examine parents’ perceptions about receiving a hard copy EMR-generated letter from a pediatric pulmonologist at the end of their child’s first asthma consult visit. This study was conducted between October 2016 and October 2017 in Alberta, Canada, with parents who attended a pediatric pulmonologist’s outpatient clinic with their child. We chose an observational cross-sectional survey design18 to examine and describe parents’ perceptions about receiving the Letter at the end of their child’s visit with the specialist, so at one point in time.
Parent Engagement
At the inception of this study, the primary investigator sought the expertise of the Lead (VV-W) of the Patient Engagement Platform, Alberta Strategy for Patient Oriented Research Support Unit (AbSPORU),19 to identify and support parent volunteers in engaging as research partners20 on the Parent Advisory Council (PAC) at the “Involve” level of engagement.21,22 The three PAC members (a mother of two; a father of two; a grandparent/caregiver) were not participants in the study. They collectively provided feedback on the study design, questionnaire development, data analysis, and dissemination of findings.22 Two PAC members lived in the city where the study was conducted, and the third member lived in a rural community 4 hours north of the city. All PAC members had accessed various specialists, at numerous times as part of the care of their children/grandchildren.
Questionnaire Development
The questionnaire chosen for the survey was adapted from one used in a United States (US) study about the impact of providing patients with access to their medical information.23 Content validation was completed by engaging with PAC members and 10 other parents who volunteered to evaluate questions for clarity and relevance to the purpose of this study. Based on their input, the study team with the PAC members, made revisions to seven questions to enhance clarity (see Appendix A for the final version of the questionnaire used in this study).
Recruitment and Data Collection
Following ethical approval for the study from two university Research Ethics Boards (Athabasca and Alberta), recruitment was initiated. Parents who consecutively attended a pediatric pulmonologist’s outpatient clinic with their child for the first time for asthma evaluation were invited to participate. At the end of the consult visit parents received a hard copy Letter summarizing their child’s visit. At this point the pulmonologist (IA) explained the purpose of the study, provided them with a copy of the study information letter, and invited them to participate. Expressions of interest were confirmed by parents providing their e-mail addresses on an enrollment sheet. No other identifying information was collected. Since the visit was over and the parents had already received their Letters there was no coercion to participate.
At the end of each week, one of the co-investigators (JR) sent the online link to the questionnaire to those who had provided e-mail addresses, requesting each to complete the survey within 14 days of receiving it. Consent was implied when participants completed and submitted the questionnaire. As needed, one follow-up email reminder was sent, after which, seven additional days were provided for completion and submission of the questionnaire. A parent could change his/her mind and decline to participate by simply not submitting the questionnaire. The decision to participate in the study or not, had no bearing on the care received, since the responses were aggregated with no linkage to identifying information.
Study data were collected and managed using the Research Electronic Data Capture (REDCap©) tools24 hosted and supported by the Women and Children’s Health Research Institute at the University of Alberta.
Analysis
Descriptive statistics were used to summarize parent perceptions of the format of, and information in, the Letter, their experiences with reading and understanding the Letter, and their preferences for receiving Letters from clinicians in the future. Response options included: 1) Disagree, 2) Somewhat disagree, 3) Somewhat agree, 4) Agree, 5) Do not know. Agree or Somewhat Agree responses were pooled when reporting endorsement of statements. Spearman Rank correlations were used to: 1) explore the perceived helpfulness of the Letter in terms of facilitating parents’ care of their child, and 2) trust in and open communication with, the pulmonologist. Missing data were handled with pairwise deletion. All statistical analyses were completed using IBM SPSS 24.0.
Results
Sample
Over the one-year period assigned for recruitment, 160 parents of children with asthma were consecutively provided information about this study and 118 agreed to participate and provided their email addresses. In total 51 (43%) submitted a completed questionnaire. Additional 11 incomplete questionnaires submitted were not included in the analysis. To meet ethical requirements for this specific study, no demographic data was collected and thus we could not characterize incomplete or non-responders from complete responders.
Descriptive Analyses
Of the 51 parents, over 90% agreed that the Letter they received accurately summarized the visit and details about their child’s condition, including medical history and physical examination findings (Figure 1). Over 80% of these parents agreed that the information within the Letter was helpful as a tool to learn more about their child’s medical condition, further tests, and recommended treatments (Figure 1). Parents’ experiences reading the Letter were very positive (Figure 2) with the majority of parents (94%) reporting a better understanding of their child’s condition and improved recollection about future treatment plans. A majority of parents also reported (Figure 3) feeling more in control of their child’s health (80%) and better able to take care of their child (82%). Most notably, a strong majority of parents reported greater trust in the pulmonologist and that the Letter facilitated open communication with him.
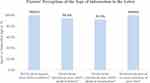 |
Figure 1 Percentage of parents who “agreed” or “somewhat agreed” with statements about information provided in the Letter they received. |
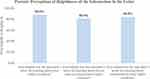 |
Figure 2 Percentage of parents who found the Letter “very helpful” or “helpful” for learning about aspects of their child’s condition. |
 |
Figure 3 Percentage of parents who “agreed” or “somewhat agreed” with statements about their experiences reading the Letter. |
Almost all parents (98%) stated that they wanted to receive similar Letters at future clinician visits (Figure 4). One-third of parents stated that they would like the option of adding comments to the Letter that was sent to their GP. Interestingly, fewer than half of the parents wanted to receive these Letters electronically (45.1%) or through a secure website or mobile app (45.1%).
 |
Figure 4 Percentage of parents who agreed with statements about preferences for receiving similar Letters in the future. |
Correlational Analysis
Our results demonstrated that parents’ perceptions of an improved understanding of their child’s medical condition were moderately and positively associated (Table 1 and Appendix B) with perceptions of their: ability to take care of their child (rs=0.419, p<0.01); feeling more in control of their child’s medical condition (rs=0.452, p<0.01); and learning about their child’s condition and future tests that might be ordered (rs=0.412, p<0.01; rs=0.324, p<0.05). Learning more about their child’s medical condition was also moderate to moderately high and positively associated with learning more about associated tests and treatments related to the condition (rs=0.663 to 0.678, p<0.01). Learning about treatments was moderately and positively associated with parents’ reports of feeling better able to remember the care plan, better able to take care of their child, and feeling more in control (rs=0.385 to 0.424, p<0.01).
 |
Table 1 Spearman’s Rank Order Correlations Between Statements About Parents’ Experiences Reading the Letter (See Appendix B for List of Statements) |
Notably, perceived improved understanding and knowledge about their child’s medical condition and feeling more in control were moderately and positively associated with higher levels of trust in the pulmonologist (rs=0.392 to 0.496, p<0.01; rs=0.337 p<0.05). Also related to trust, were parents’ statements that were positively associated with being able to openly communicate with the pulmonologist: understanding and learning about the child’s medical condition (rs=0.420, p<0.01); remembering the plan of care (rs=0.372, p<0.01); and having trust in the specialist (rs=0.572, p<0.01).
Discussion
This pilot study focused on previously unexplored perceptions of parents of children with asthma (where communication and partnerships-in-care between parents and physicians are so important3,4,17), with regard to the practice of providing each with a copy of the EMR-generated specialist’s Letter to the referring GP, at the end of the first asthma consult visit. Parents in this study indicated that their child’s medical condition was summarized accurately in the Letter and that they were more familiar with their child’s overall health condition because of the information included in the Letter. As well, most parents understood the terminology used, and wanted to receive similar Letters at the end of clinician visits in the future.
There were positive associations across a number of variables in our study such as, parents’ improved understanding of their child’s health, their perceived ability to take care of their child, and their reports of feeling more in control about their child’s overall health.
Concomitantly, parents reported trusting the pulmonologist more. The results of this study support the findings of Damian,8 Saunders,9 and Tomkins10 who previously reported that this practice of information sharing in a Letter had resulted in increased patient satisfaction, improved uptake of recommendations, and strengthened doctor–patient relationships.
While patients in other studies have reported feeling better prepared for their next appointments as a result of having previously received a copy of the referral request letter,6 have demonstrated improved adherence to treatment, and reported the benefit of having time to plan questions for next appointments,7,16 these were not variables assessed in the current study and should be explored in future studies with parents. Clinicians’ time used to prepare the Letter should also be assessed.
An unexpected result from this study was that the majority of parents identified that it was less desirable for them to receive the Letter electronically or through a mobile app, compared to receiving a hard copy of the Letter at the end of the visit. These results are worthy of closer examination because the current climate in healthcare is such that many practices are being migrated to online or electronic interfaces for improved accessibility and reduced costs. Given the initiative in Alberta to build a province-wide electronic health record system in acute care settings to bridge online information sharing among patients, caregivers, and clinicians, more research around patient and parent preferences for accessing this information online is timely.
The PAC members expressed frustration during post-study meetings, that a practice so obviously beneficial to parents and their children would most likely be restricted and hindered from timely implementation in clinical practice due to policies and procedures related to information access, concerns about litigation, and the risk of privacy breaches. They were also intrigued by parent participants’ hesitancy to receive Letters in electronic formats or through online portals. PAC members had the following insights about this result: 1) concern for information leaks and whether the use of the “cloud” to store and share online information could have possible impacts when applying for medical insurance etc.; 2) preferences some had for the tangible paper Letter which could be read together and easily shared with other family members or caregivers; and 3) the sharing of information online is so normalized now (for example, online banking), that this may eventually become true of medical information. Other important observation by our PAC members were that 1) they had not realized what was missing in their child’s care (ie, access to the Letter from specialists) until they participated in this study, and 2) the waste of time and money with the current practice of needing to make an appointment with the referring GP to hear the results of the specialist’s assessment. They also suggested shortening the questionnaire for future studies.
To date, all previous studies about this written communication practice pre-date the EMR era, and no researchers examined views from parents of children with asthma. Providing the patient or caregiver with a copy of a GP’s referral request5,6 or a specialist’s summary Letter is a practice increasingly being adopted in many Western countries. In fact, copying (ie, carbon coping [cc.]) patients on such Letters has become mandatory in some locales, such as in the UK and Israel. In that respect, Canada is lagging behind.25 The results of this study identify an opportunity to improve the patient and family centredness of pediatric clinical care.26 As one of our PAC members, Laura Saunders publicly shared …
The thing that stood out in my mind was how little involvement I have had in my health care. … I, a key stakeholder, am not often in the loop regarding the management and delivery of the care I or my children, receive.22
Limitations
To address ethical considerations of confidentiality and the risk of coercion since the PI recruited all potential participants, no demographic data of participants were obtained. Collecting and analyzing demographic information such as age, income, relationship to child, education, or ethnic/cultural background, would have helped to identify additional factors that could have influenced participation and responses. It is unknown as well, how recruitment by the PI as the specialist, influenced overall and individual participation and responses. We also acknowledge that as this was a pilot study, it was necessarily a small-size single-center study, with only a 43% response rate. As a result, the findings have limited generalizability beyond similar specialty clinics in Canada. Nonetheless, these results do clarify this opportunity to provide improved parent/child-centered care.
Conclusion
We anticipate that the results of this pilot study will help influence both additional research and policy revisions, to promote change in the perceptions of clinicians, parents, and patients about ready access to health information of this nature from clinicians. We also experienced the benefits of engaging with parents as partners in asthma research, through the Parent Advisory Council. They helped ensure that the study design, questionnaire development, analysis of data, and dissemination of results were informed by their valuable perspectives as front-line stakeholders. Together, these results have the potential to influence further study around this practice so as to positively shift not only asthma specialists’ standard practices to include the provision of an EMR-generated letter for parents at the end of every child’s visit, but indeed, how research with stakeholder partners such as parents, is conducted in the future.
Abbreviations
EMR, electronic medical record; GP, General Practitioner; PAC, Parent Advisory Council.
Ethics and Consent Statement
Ethical approval was received for the study from two Research Ethics Boards Athabasca University [File No: 22283] and University of Alberta [MS2_Pro00063884]. Participants consent was implied by submitting a completed questionnaire electronically.
Acknowledgments
We acknowledge the participation, and support of the Patient Engagement (PE) Platform of the ABSPORU (Alberta Strategy for Patient-oriented Research SUPPORT Unit) for in-kind contributions, and the parents who participated in this study. Participants consented to de-identified and aggregate data being published.
Author Contributions
Israel Amirav and Virginia Vandall-Walker are co-first authors. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
Funding for the EMR Letters Study and part of this work was generously provided by the Respiratory Health Strategic Clinical Network (RHSCN) Research and Innovation Seed Grant.
Disclosure
The authors have indicated they have no conflicts of interest to disclose.
References
1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention; 2019. Available from: www.ginasthma.org.
2. Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on patient outcomes. Pediatrics. 2006;117:2149–2157. doi:10.1542/peds.2005-1055
3. Partridge MR, Hill SR. Enhancing care for people with asthma: the role of communication, education, training and self-management. 1998 world asthma meeting education and delivery of care working group. Eur Respir J. 2000;16:333–348. doi:10.1183/09031936.00.16233400
4. Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181:566–577. doi:10.1164/rccm.200906-0907OC
5. Jelley D, Zwanenberg TV. Copying general practitioner referral letters to patients: a study of patient views. Br J Gen Pract. 2000;50:657e8.
6. Jelley D, Scott D, Zwanenberg TV. Copying GP referral letters to patients: the benefits and practical implications. Prim Health Care Res Dev. 2003;4:319e28. doi:10.1191/1463423603pc165oa
7. Pothier DD, Nakivell P, Hall CEJ. What do patients think about being copied into their GP letters? Ann R Coll Surg Engl. 2007;89(7):718–721. doi:10.1308/003588407X205413
8. Damian D, Tattersall MH. Letters to patients: improving communication in cancer care. Lancet. 1991;338:923–925. doi:10.1016/0140-6736(91)91782-P
9. Saunders N, Georgalas C, Blaney SEA, Dixon H, Topham JH. Does receiving a copy of correspondence improve patients’ satisfaction with their outpatient consultation? J Laryngol Otol. 2003;117:126e9. doi:10.1258/002221503762624576
10. Tomkins CS, Braid JJ, Williams HC. Do dermatology outpatients value a copy of the letter sent to their general practitioner? In what way and at what cost? Clin Exp Dermatol. 2004;29:81e6. doi:10.1111/j.1365-2230.2004.01437.x
11. Krishna Y, Damato BE. Patient attitudes to receiving copies of outpatient clinic letters from the ocular oncologist to the referring ophthalmologist and GP. Eye. 2005;19:1200e4. doi:10.1038/sj.eye.6701740
12. Eaden J, Ward B, Smith H, et al. Are we telling patients enough? A pilot study to assess patient information needs in a gastroenterology outpatient department. Eur J Gastroenterol Hepatol. 1998;10:63e7. doi:10.1097/00042737-199801000-00012
13. Nixon J, Courtney P. Copying clinic letters to patients. Rheumatology. 2005;44(2):255e6. doi:10.1093/rheumatology/keh469
14. Waterston T, San Lazaro C. Sending parents outpatient letters about their children: parents’ and general practitioners’ views. Qual Health Care QHC. 1994;3(3):142–146. doi:10.1136/qshc.3.3.142
15. White P, Singleton A, Jones R. Copying referral letters to patients: the views of patients, patient representatives and doctors. Patient Educ Couns. 2004;55(1):94–98. doi:10.1016/j.pec.2003.08.003
16. Perkins P, Jordan A, Prentice W, Regnard C. Copying letters to patients: a survey of patients and GPs views. Palliat Med. 2007;21(4):355–356. doi:10.1177/0269216307077793
17. Clark NM, Cabana MD, Nan B, et al. The clinician-patient partnership paradigm: outcomes associated with physician communication behavior. Clin Pediatr (Phila). 2008;47:49–57. doi:10.1177/0009922807305650
18. Abrahamyan L. Survey methods for health services research: theory & application Canadian Centre for Health Economics (CCHE) seminar series. October 2017:1–67. Available from: https://www.canadiancentreforhealtheconomics.ca›uploads›2017/10.
19. Canadian Institutes of Health Research (CIHR). Strategy for patient-oriented research– patient engagement framework; 2014. Available from: http://www.cihr-irsc.gc.ca/e/48413.html-a4.
20. Shen S, Doyle-Thomas KA, Beesley L, et al. How and why should we engage parents as co-researchers in health research? A scoping review of current practices. Health Expect. 2017;20(4):543–554. doi:10.1111/hex.12490
21. Vandall-Walker V Patient-researcher engagement in health research: active, mutually beneficial, co-creation. In:
22. Amirav I, Vandall-Walker V, Rasiah J, et al. Patient and researcher engagement in health research: a parent’s perspective. Pediatrics. 2017;140(3):e20164127. doi:10.1542/peds.2016-4127
23. Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med. 2012;157(7):461–470. doi:10.7326/0003-4819-157-7-201210020-00002
24. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (RED-Cap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi:10.1016/j.jbi.2008.08.010
25. Amirav I. Transparency of care. CMAJ. 2015;187(4):278. doi:10.1503/cmaj.1150013
26. Eichner JM, Johnson BH. Policy statement: patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
