Back to Journals » Cancer Management and Research » Volume 14
All-Trans-Retinoic Acid Plus Oxaliplatin/Fluorouracil/Leucovorin for Advanced Hepatocellular Carcinoma with Pulmonary Metastasis: A Multicenter Retrospective Study
Authors Sun J, Liu C, Wang N, Jiang D, Zhang F, Shi J, Cheng S
Received 15 December 2021
Accepted for publication 24 April 2022
Published 5 May 2022 Volume 2022:14 Pages 1663—1670
DOI https://doi.org/10.2147/CMAR.S354170
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Matthew Witek
Juxian Sun,1,* Chang Liu,1,* Nanya Wang,2,* Dafeng Jiang,3 Fan Zhang,4 Jie Shi,5 Shuqun Cheng1
1Department of Hepatic Surgery VIa, Eastern Hepatobiliary Surgery Hospital, The Second Military Medical University, Shanghai, People’s Republic of China; 2Department of Oncology, First Hospital of Jilin University, Changchun, People’s Republic of China; 3Department of Oncology, Zhejiang Sian International Hospital, Jiaxing, People’s Republic of China; 4Department of General Surgery, Fujian Cancer Hospital, Fujian Medical University, Fuzhou, People’s Republic of China; 5Department of Hepatic Surgery VIb, Eastern Hepatobiliary Surgery Hospital, The Second Military Medical University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shuqun Cheng; Jie Shi, Department of Hepatic Surgery VIa, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University, Changhai Road 168, Yangpu District, Shanghai, 200433, People’s Republic of China, Tel +86-211-3901746 ; +86-211-3816768296, Fax +86-218-1875251 ; +86-218-1875252, Email [email protected]; [email protected]
Aim: To study the impact of All-trans-retinoic acid (ATRA) plus FOLFOX4 compared to FOLFOX4 alone in patients with advanced hepatocellular carcinoma (HCC) with pulmonary metastasis.
Methods: The data of patients with advanced HCC who underwent systemic chemotherapy using FOLFOX4 or ATRA plus FOLFOX4 at the Eastern Hepatobiliary Surgery Hospital, First Hospital of Jilin University, Zhejiang Sian International Hospital and Fujian Cancer Hospital were retrospectively analyzed. The survival outcomes in the 2 groups were compared.
Results: From May 2014 to July 2020, 66 patients were suitable to enter into this study. The median survival (14.0 vs 8.0 months, p=0.012), and the median time to progression in the ATRA plus FOLFOX4 group were both significantly longer than those in the FOLFOX4 group (8.7 vs 3.2 months, p=0.002). The 6 month-, 1 year- and 2 year- overall survival rates were also significantly better in the ATRA plus FOLFOX4 group (100.0%, 64.7% and 20.5%; respectively) than the FOLFOX4 group (59.4%, 21.9%, and 12.5%, respectively; p< 0.001). Leukocytopenia, fatigue, anorexia, nausea, were the most common acute toxicities, but these were mostly NCI CTCAE Grade 1 or 2. There was no significant difference in adverse events between the two groups.
Conclusion: ATRA plus FOLFOX4 significantly improved the survival outcomes in patients with advanced HCC with pulmonary metastasis.
Keywords: hepatocellular carcinoma, pulmonary metastasis, chemotherapy, ATRA
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common neoplasm and the third most common cause of cancer-related deaths worldwide.1 The morbidity and mortality rates of HCC ranked fourth and third, respectively, among all malignant tumors reported in China.2 Due to the unsatisfactory progress in effective strategies for early diagnosis and treatments, 70% to 80% of patients are diagnosed at an advanced stage, which includes extrahepatic metastasis (EHM) according to the Barcelona Clinic Liver Cancer (BCLC) staging system. The presence of EHM is a major cause of the death of HCC patients, and the expected median survival time is only 6 to 10 months.3,4 The lung is considered the most favorable organ for HCC metastatic colonization, accounting for 51% of all EHMs (followed by lymph nodes, bones, and adrenal glands).5–7 The results from a large-scale population study showed that the 1-year overall survival (OS) was 12.8% in patients diagnosed with HCC pulmonary metastasis (PM).8
There are limited data for subgroup analysis in HCC patients with PM; thus, the efficacy of systemic agents is still unknown. Therefore, there are no specific treatment options for PM other than the recommendations under the guidelines for advanced HCC. Moreover, it has been reported9,10 that HCC patients with PM could not benefit from sorafenib due to the high drug resistance rate. Immune-based therapy might be one of the possible ways in the future but lack of enough evidences.11–13 Further investigation of systemic agents for PM is still urgently needed.
In contrast to the results in other solid cancers, systemic chemotherapy has widely been regarded as ineffective in HCC. A recent study, known as the EACH Study,14 showed that FOLFOX4 (oxaliplatin plus fluorouracil/leucovorin) had some effect on selected patients with advanced HCC, although the partial response (PR) rate was only 8.15%. Chemotherapy combined with other treatments may be one of the ways to solve chemotherapy resistance of HCC.15,17,18 All-trans retinoic acid (ATRA), a key metabolite of vitamin A, is regarded as the first effective targeted therapy for acute promyelocytic leukemia (APL), and its effects have rarely been reported in solid cancers.16 Our previously reported study17,18 showed that all-trans retinoic acid (ATRA) significantly improved the treatment efficacy of cisplatin on HCC in vivo and in vitro, which could at least partially be attributed to the effect of ATRA-induced differentiation of HCC tumor-initiating cells with a resultant decrease in the chemo-resistant subpopulation.
Therefore, our study aimed to determine the efficacy and safety of ATRA plus FOLFOX4 compared to FOLOFX4 monotherapy in HCC patients with PM.
Materials and Methods
Patients
Patients with histologically, cytologically, or clinically diagnosed unresectable HCC treated at the Eastern Hepatobiliary Surgery Hospital (Shanghai, China), First Hospital of Jilin University (Changchun, China), Fujian Cancer Hospital (Fuzhou, China) and Zhejiang Sian International Hospital (Jiaxing, China) from May 2014 to July 2020 were enrolled in this study. The inclusion criteria were as follows: patients diagnosed with HCC based on histopathological findings or from noninvasive assessment according to the American Association for the Study of Liver Diseases criteria for patients with confirmed cirrhosis and classified as Barcelona Clinic Liver Cancer (BCLC) stage C with pulmonary metastasis that had at least one measurable lesion; liver functional status of Child–Pugh Grade A; WBC count ≥3.5 ˟109 cells/L, hemoglobin ≥ 90 g/L, platelet count ≥70 ˟109 cells/L; and life expectancy of ≥12 weeks. The exclusion criteria were hemorrhagic disorders or active bleeding; sepsis; CHF NYHA class > 2; active CAD or cardiac ischemia; uncontrolled cardiac arrhythmias even with anti-arrhythmic therapy; and patients who had undergone any anti-HCC therapy within 4 weeks. This study was approved by the Ethics Committee of Eastern Hepatobiliary Surgery Hospital.
Systemic Chemotherapy
In the control group, only FOLFOX4 (oxaliplatin or OXA at 85 mg/m2 intravenously [IV] on Day 1, leucovorin (LV) at 200 mg/m2 IV from hour 0 to 4 on Day 1, and 5-fluorouracil (5-FU) at 400 mg/m2 IV bolus at hour 4, followed by 600 mg/m2 over 40 hours on Days 1 and 2, once every two weeks) was given. In the ATRA plus FOLFOX4 (ATFOX) group, the treatment regimen consisted of oral administration of 20 mg ATRA 3 times/day for 3 days prior to initiation of FOLFOX4. ATRA was discontinued at the end of FOLFOX4. All doses of the medications were calculated in milligrams of each drug per square meter of body surface area (BSA) as measured at baseline (mg/m2). BSA was recalculated when the body weight changed by 5%.
Evaluation and Follow-Up
All patients were evaluated after chemotherapy and then followed-up. Abdominal ultrasound (USG), chest X-ray, liver function tests, and analysis of alpha fetoprotein (AFP) levels were carried out at each of the follow-up visits and every month thereafter. Chest computed tomography (CT) was carried out once every 2 months. If the diseases progressed, any available effective treatment was administered, and if liver failure or massive ascites occurred, the best supportive care was given. Overall survival (OS) was defined as the interval between the date of start of chemotherapy and the date of death. Time to progression (TTP) was defined as the interval between the date of start of chemotherapy and the date of tumor progression. The response was determined by an independent radiologist using modified RECIST (mRECIST).
Drug toxicities were assessed by vital signs, physical examination, electrocardiogram, echo, clinical laboratory tests and special medical imaging (chest X-ray, CT, MRI, bone scan). All adverse events were evaluated according to the NCI CTCAE (Version 4.0).
Statistical Analysis
Continuous variables are expressed as medians (range) and were compared using the unpaired t test. The v2 test was used for categorical data, including treatment-related morbidity. The survival curves for the two groups were generated by the Kaplan–Meier method and calculated by the log rank test. A p value<0.05 was considered to be statistically significant. Statistical analyses were performed using SPSS 16.0 software.
Results
Patient Characteristics
From May 2014 to July 2020, 66 HCC patients with PM were enrolled in this study. All patients had Child-Pugh A liver function and an Eastern Cooperative Oncology Group performance status of 0 or 1. There were 54 males and 12 females. The median age was 51.5 years (range 25–71 years). Chronic hepatitis B virus infection was the predominant cause of underlying liver diseases (n =58, 87.9%). The median cycle of chemotherapy was 4.5 (range 1–12 cycles). There were 34 patients who received ATRA plus FOLFOX4 and 32 with FOLFOX4 only. Their baseline characteristics are summarized in Table 1. The median follow-up was 24 months (range 6–74 months).
 |
Table 1 The Clinicopathological Features of All Patients (n =66) |
Survival
The median OS was 8.0 months and 14.0 months for the FOLFOX4 group and the ATRA+ FOLFOX4 group, respectively (p<0.001). The corresponding 6-month, 1-year, 2-year and 3-year survival rates were 59.40%, 21.90%, 12.50%, and 9.4% and 100%, 64.7%, 20.5%, and 14.7%, respectively (Figure 1). The median TTP was 3.2 months and 8.7 months for the FOLFOX4 group and the ATRA+ FOLFOX4 group, respectively (p<0.001). The corresponding 6-month, 1-year, 2-year and 3-year TTP rates were 15.6%, 9.4%, 0.0%, and 0.0% and 44.1%, 26.5%, 8.8%, and 8.8%, respectively (Figure 2).
 |
Figure 1 Kaplan–Meier curve of overall survival in the two groups. |
 |
Figure 2 Kaplan–Meier curve of disease-free survival in the two groups. |
Univariate analysis showed that ATRA (p = 0.018), CLIP score (p=0.029), total bilirubin (p=0.019) and HBV-DNA level (p = 0.009) were independent prognostic factors of OS, whereas multivariate analysis showed that only ATRA (p = 0.020) was an independent prognostic factor of OS.
The response rate (RR) of the ATRA+ FOLFOX4 group was 29.4%, including 3 patients with complete remission (CR), and the disease control rate (DCR) was 58.8%. The RR of the FOLFOX4 group was 9.4%, including no patients with CR, and the DCR was 25.0% (Table 2).
 |
Table 2 Disease Response of the Two Groups of Patients |
Adverse Events
Table 3 summarizes the toxicities of NCI CTCAE grades 3–4 for the two groups of patients. Headache occurred in 4 patients in the combined group (NCI CTCAE Grade 1/2), and NSAIDs were effective. Leukocytopenia, anorexia, nausea/vomiting and fatigue were the most common acute toxicities in both groups, but these were mostly NCI CTCAE grade 1 or 2. Nine patients (26.5%) in the FOLFOX4 group and 9 patients (28.1%) in the FOLFOX4 group developed NCI CTCAE grade 3–4 leukocytopenia. All the patients suffering leukocytopenia recovered after chemotherapy. One patient in the FOLFOX4 group suffered NCI CTCAE grade 3 ALT elevation. No treatment-related deaths were observed in this study.
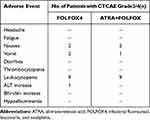 |
Table 3 Adverse Events of Patients with Advanced HCC Who Underwent Chemotherapy |
Discussion
In HCC patients with PM, ATRA plus FOLFOX4 showed more benefits than FOLFOX4 alone, resulting in significantly longer OS and ORR. There were 3 cases with CR (8.8%) in the combined treatment group but none in the control group. The combined therapy did not cause more adverse events than FOLFOX4 alone.
Successful treatment of pulmonary metastases is beneficial to HCC patients with PM,19 but there are no standard treatments for these patients. According to the BCLC staging system, HCC with PM is classified as an advanced stage (BCLC C), and sorafenib/lenvatinib is recommended as the first-line treatment. However, several studies9,10 have revealed that PM could not benefit from sorafenib due to the high rate of drug resistance. A recent single-arm study20 reported the effects of apatinib on HCC patients with PM. For the 41 patients with lung metastasis, the median mPFS was 5 months, with an mOR rate (mORR) of 22.0% (9/41). Local control of PM, such as pulmonary metastasectomy (PMT), might result in better survival, but it is not suitable for multifocal lesions (>3), which account for the majority of PMs.21 Additionally, patients who receive PMT are at high risk of recurrence. Therefore, the development of systemic therapy for this subgroup of patients is urgently needed.
Chemotherapy for HCC is considered ineffective. With constant progress in chemotherapeutic drugs, this treatment can now be used for advanced HCC. FOLFOX4 has been approved by the National Medical Products Administration (NMPA) for the treatment of advanced HCC,22 although the effect is not satisfactory. In the EACH study,14 the PR rate of FOLFOX4 was only 8.15%, and there were no patients with CR. Chemoresistance is still the leading cause of treatment failure and the most urgent problem to be solved to improve the efficacy of systemic chemotherapy in HCC.
Increasing evidence has shown that liver cancer stem cells (LCSCs) to be responsible for the failure of chemotherapy.23 Although systemic chemotherapy can kill a majority of HCC cells, it may ultimately fail because it does not eliminate LCSCs, which survive to regenerate new HCCs. Many LCSC phenotypes24–29 have been reported to be related to chemoresistance in HCC, including CD133+, ALDH, CD13, EPCAM, OV6 and ICAM-1. Thus, specific therapies targeting LCSCs might enhance the effect of chemotherapy.
ATRA is an active natural metabolite of vitamin A that regulates various biological processes. This metabolite has also been shown to exert antitumor properties. ATRA could simultaneously block multiple Pin1-regulated cancer-driving pathways in acute promyelocytic leukemia (APL), breast cancer and melanoma,16,30 which is an attractive property for treating aggressive and drug-resistant tumors. In addition, a series of previous studies17,18 by our research group revealed that ATRA therapy promoted the effect of chemotherapy by inducing the differentiation of LCSCs via the TSC2/AKT pathway. Hence, ATRA and chemotherapy have different mechanisms of action, supporting their augmented activity when administered together. In this study, the response rate of 29.4% for this combination in patients with PM was very encouraging and was higher than that reported in previous literature. Drug resistance is also an important reason for the failure of targeted therapy and immunotherapy, our study might offer a possible solution for such situations. In the case of combination therapy has become the trend now as the effectiveness of mono-therapy has reached a bottleneck. The combination of ATRA with targeted therapy or immunotherapy is our next research focus.
After comparing the incidence of adverse events (AEs) between the two groups, we found that ATRA did not significantly increase the incidence of AEs. Headache is a specific side effect of ATRA, but there were no grade 3/4 patients, and no patients required a dose reduction in the combined group. Leukocytopenia and gastrointestinal AEs were the most common AEs in the two groups and could recover without treatment after chemotherapy.
This study also has some limitations. Firstly, the sample size of our study was small due to difficulties in enrollment. But the study contains patients from 4 different centers and the results are somewhat representative. Secondly, the retrospective design determines that the study might have some bias, but we have balanced the baseline of the two groups as much as possible. Moreover, we cannot assess the impact of chemotherapy on the quality of life (QOL) of these patients. Thirdly, concomitant therapies were inevitable for the retrospective study. Further studies with larger sample sizes and randomized control groups are required to validate the efficacy and safety of ATRA plus FOLFOX4 in the treatment of HCC patients with PM.
In conclusion, combined therapy with ATRA/FOLFOX4 was more effective than FOLFOX4 alone in the treatment of HCC patients with PM. Combined treatment could be given without severe adverse side effects.
Data Sharing Statement
Research data are not shared, owing to the privacy or ethical restrictions.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki and the Eastern Hepatobiliary Surgery Hospital (EHBH) Clinical Research Ethics Committee approved this retrospective study. The requirement for informed consent was waived due to the retrospective nature of the study, and no personal information was disclosed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is supported by the National Natural Science Foundation of China (No.82073293); Clinical Science and Technology Innovation Project of Shanghai Shenkang Hospital Development Center (Joint Project of Emerging Frontier Technology) (No.82073293); the Key Project of Natural Science Foundation of China (No: 81730097).
Disclosure
The authors have no conflicts of interest to declare. Ju-Xian Sun, Chang Liu, and Nanya Wang are co-first authors for this study.
References
1. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. doi:10.1016/S0140-6736(18)30010-2
2. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
3. Guo X, Xu Y, Wang X, et al. Advanced hepatocellular carcinoma with bone metastases: prevalence, associated factors, and survival estimation. Med Sci Monit. 2019;25:1105–1112. doi:10.12659/MSM.913470
4. Kanda M, Tateishi R, Yoshida H, et al. Extrahepatic metastasis of hepatocellular carcinoma: incidence and risk factors. Liver Int. 2008;28(9):1256–1263. doi:10.1111/j.1478-3231.2008.01864.x
5. Uka K, Aikata H, Takaki S, et al. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma. World J Gastroenterol. 2007;13(3):414–420. doi:10.3748/wjg.v13.i3.414
6. Villanueva A, Hernandez-Gea V, Llovet JM. Medical therapies for hepatocellular carcinoma: a critical view of the evidence. Nat Rev Gastroenterol Hepatol. 2013;10(1):34–42. doi:10.1038/nrgastro.2012.199
7. Katyal S, Oliver JH, Peterson MS, et al. Extrahepatic metastases of hepatocellular carcinoma. Radiology. 2000;216(3):698–703. doi:10.1148/radiology.216.3.r00se24698
8. Wu C, Ren X, Zhang Q. Incidence, risk factors, and prognosis in patients with primary hepatocellular carcinoma and lung metastasis: a population-based study. Cancer Manag Res. 2019;11:2759–2768. doi:10.2147/CMAR.S192896
9. Yau T, Chan P, Ng KK, et al. Phase 2 open-label study of single-agent sorafenib in treating advanced hepatocellular carcinoma in a hepatitis B-endemic Asian population: presence of lung metastasis predicts poor response. Cancer. 2009;115(2):428–436. doi:10.1002/cncr.24029
10. Yang T, Lu JH, Lin C, et al. Concomitant lung metastasis in patients with advanced hepatocellular carcinoma. World J Gastroenterol. 2012;18(20):2533–2539. doi:10.3748/wjg.v18.i20.2533
11. Rizzo A, Dadduzio V, Ricci AD, et al. Lenvatinib plus pembrolizumab: the next frontier for the treatment of hepatocellular carcinoma? Expert Opin Investig Drugs. 2021:1–8. doi:10.1080/13543784.2021.1948532
12. Rizzo A, Ricci AD, Brandi G. Atezolizumab in advanced hepatocellular carcinoma: good things come to those who wait. Immunotherapy. 2021;13(8):637–644. doi:10.2217/imt-2021-0026
13. Rizzo A, Ricci AD, Brandi G. Immune-based combinations for advanced hepatocellular carcinoma: shaping the direction of first-line therapy. Future Oncol. 2021;17(7):755–757. doi:10.2217/fon-2020-0986
14. Qin S, Bai Y, Lim HY, et al. Randomized, multicenter, open-label study of oxaliplatin plus fluorouracil/leucovorin versus doxorubicin as palliative chemotherapy in patients with advanced hepatocellular carcinoma from Asia. J Clin Oncol. 2013;31(28):3501–3508. doi:10.1200/JCO.2012.44.5643
15. Guo J, Yu Z, Sun D, et al. Two nanoformulations induce reactive oxygen species and immunogenetic cell death for synergistic chemo-immunotherapy eradicating colorectal cancer and hepatocellular carcinoma. Mol Cancer. 2021;20(1):10. doi:10.1186/s12943-020-01297-0
16. Wei S, Kozono S, Kats L, et al. Active Pin1 is a key target of all-trans retinoic acid in acute promyelocytic leukemia and breast cancer. Nat Med. 2015;21(5):457–466. doi:10.1038/nm.3839
17. Zhang Y, Guan DX, Shi J, et al. All-trans retinoic acid potentiates the chemotherapeutic effect of cisplatin by inducing differentiation of tumor initiating cells in liver cancer. J Hepatol. 2013;59(6):1255–1263. doi:10.1016/j.jhep.2013.07.009
18. Guan DX, Shi J, Zhang Y, et al. Sorafenib enriches epithelial cell adhesion molecule-positive tumor initiating cells and exacerbates a subtype of hepatocellular carcinoma through TSC2-AKT cascade. Hepatology. 2015;62(6):1791–1803. doi:10.1002/hep.28117
19. Cruz RJ Jr, Ranganathan S, Mazariegos G, et al. Analysis of national and single-center incidence and survival after liver transplantation for hepatoblastoma: new trends and future opportunities. Surgery. 2013;153(2):150–159. doi:10.1016/j.surg.2012.11.006
20. Du X, Chen D, Lin Z, et al. Efficacy of apatinib in advanced hepatocellular carcinoma with lung metastasis: a retrospective, multicenter study. J BUON. 2019;24(5):1956–1963.
21. Hu Z, Li W, Huang P, et al. Therapeutic significance and indications of pulmonary metastasectomy for hepatocellular carcinoma following liver resection. Int J Surg. 2017;48:23–31. doi:10.1016/j.ijsu.2017.09.075
22. Zhou J, Sun H, Wang Z, et al. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 edition). Liver Cancer. 2020;9(6):682–720. doi:10.1159/000509424
23. Walcher L, Kistenmacher AK, Suo H, et al. Cancer stem cells-origins and biomarkers: perspectives for targeted personalized therapies. Front Immunol. 2020;11:1280. doi:10.3389/fimmu.2020.01280
24. Sun J, Luo Q, Liu L, et al. Biomechanical profile of cancer stem-like cells derived from MHCC97H cell lines. J Biomech. 2016;49(1):45–52. doi:10.1016/j.jbiomech.2015.11.007
25. Qin Q, Sun Y, Fei M, et al. Expression of putative stem marker nestin and CD133 in advanced serous ovarian cancer. Neoplasma. 2012;59(3):310–315. doi:10.4149/neo_2012_040
26. Yang E, Shim JS, Woo HJ, et al. Aminopeptidase N/CD13 induces angiogenesis through interaction with a pro-angiogenic protein, galectin-3. Biochem Biophys Res Commun. 2007;363(2):336–341. doi:10.1016/j.bbrc.2007.08.179
27. Nio K, Yamashita T, Okada H, et al. Defeating EpCAM(+) liver cancer stem cells by targeting chromatin remodeling enzyme CHD4 in human hepatocellular carcinoma. J Hepatol. 2015;63(5):1164–1172. doi:10.1016/j.jhep.2015.06.009
28. Yang W, Yan HX, Chen L, et al. Wnt/beta-catenin signaling contributes to activation of normal and tumorigenic liver progenitor cells. Cancer Res. 2008;68(11):4287–4295. doi:10.1158/0008-5472.CAN-07-6691
29. Oikawa T, Kamiya A, Zeniya M, et al. Sal-like protein 4 (SALL4), a stem cell biomarker in liver cancers. Hepatology. 2013;57(4):1469–1483. doi:10.1002/hep.26159
30. Kim G, Bhattarai PY, Oh CH, Choi HS. All-trans retinoic acid overcomes acquired resistance to PLX4032 Inhibition of PIN1 in melanoma cells. Anticancer Res. 2019;39(12):6537–6546. doi:10.21873/anticanres.13869
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
