Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Age-Related Macular Degeneration in Primary Osteoarthritis Egyptian Patients
Authors Mahgoub MY , Abou Ghanima AT, Elmohamady MN , Abdul Basset S
Received 5 January 2020
Accepted for publication 20 March 2020
Published 30 March 2020 Volume 2020:12 Pages 35—40
DOI https://doi.org/10.2147/OARRR.S244838
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Chuan-Ju Liu
Marwa Yahia Mahgoub,1 Ahmed Taha Abou Ghanima,1 Mohamed Nagy Elmohamady,2 Shaza Abdul Basset1
1Department of Rheumatology, Rehabilitation and Physical Medicine, Faculty of Medicine, Benha University, Benha, Egypt; 2Department of Ophthalmology, Faculty of Medicine, Benha University, Benha, Egypt
Correspondence: Marwa Yahia Mahgoub
Department of Rheumatology, Rehabilitation and Physical Medicine, Faculty of Medicine, Benha University, Benha, Egypt
Tel +20 1005530882
Email [email protected]
Introduction: Both primary osteoarthritis (OA) and age-related macular degeneration (AMD) cause disability in old people. This study aimed to detect the relation between primary osteoarthritis and age-related macular degeneration in a sample of geriatric Egyptian population.
Methods: This cross-sectional study included 222 primary OA patients. Medical history, musculoskeletal examination, body mass index (BMI) calculation, and ophthalmological examination, radiographs of anteroposterior view and weight-bearing position for both hips and both knees and posteroanterior view for hands, Kellgren and Lawrence grading score for radiological severity of OA, optical coherence tomography (OCT), and fundus fluorescence angiography FFA for evaluation of the macula were done. AMD was classified into early, intermediate, and late. The collected data were analyzed using SPSS version 25.0.
Results: Forty-six OA patients had AMD [19 cases had early, 15 cases had intermediate and 12 cases with late (7 neovascular (NV) and 5 geographic atrophy (GA))]. There was a significant correlation between AMD stages and OA grading score. There were significant differences between OA patient with AMD and those without AMD regarding age, disease duration, disease severity, family history of OA, daily mild exercise and calcium, and vitamin D intake. Multivariable analysis revealed that older age, more severe OA, low exercise and less calcium and vitamin D intake were considered independent risk factors for AMD development in primary OA.
Conclusion: Primary OA patients are more liable to AMD due to common risk factors and related pathogenesis. Ophthalmological follow up of those patients is recommended.
Keywords: primary osteoarthritis, age-related macular degeneration, age-related diseases
Introduction
Ageing is a process of molecular, cellular, and organ damage that increase the susceptibility to morbidity and mortality.1 Although there is a controversy about considering ageing as a risk factor in age-related diseases, but there is an evident consensus that ageing and age-related diseases share the same basic molecular and cellular mechanisms.2 Inflammaging, chronic sterile low-grade inflammation during ageing, contributes to the pathogenesis of age-related diseases.3
Primary osteoarthritis (OA) is one of the age-related diseases that causes disability in people aged >65 years. OA is not considered an inflammatory form of arthritis, but subclinical low-grade inflammation plays a key role in the disease pathogenesis.3 Alterations in cell signaling promote a pro-inflammatory, catabolic state with augmented cell death that lead to increased joint tissue destruction and defective repair of damaged matrix.4
Age-related macular degeneration (AMD) is a multifactorial retinal degenerative disease and one of the leading causes of visual impairment and even blindness. An estimated prevalence of 196 million people worldwide who suffer from AMD. Inflammation and immune system have a prevailing role in AMD pathogenesis.5
Inflammaging was proposed to give a crucial contribution in the onset of AMD and OA that may give the clue of their relationship.6 Recent researches approved the coincidence of AMD and inflammatory diseases like gout7 and OA.8 We aimed to detect this relation in a sample of geriatric Egyptian population. Furthermore, we aimed to correlate their disease grading and severity. This may affect our policy for screening of AMD in Egyptian OA patients leading to early diagnosis.
Patients and Methods
This study was conducted from June 2018 to October 2019 as a collaborative study between the Rheumatology, Rehabilitation & Physical Medicine and the Ophthalmology Departments, Faculty of Medicine, in Benha University, Egypt.
The patients were collected from the outpatients’ clinic of the Rheumatology, Rehabilitation & Physical Medicine Department, Benha University. All ophthalmological examination and imaging were done in Ophthalmology Department, Benha University. The study was approved by local Research Ethics Committee at Benha University (20-02-18) and was done in accordance with the ethical standards laid down in an appropriate version of the 1964 Declaration of Helsinki and its revisions. A written informed consent in Arabic language was obtained from every participant before being enrolled in the study.
Patients diagnosed as primary OA according to American College of Rheumatology Subcommittee on Osteoarthritis Guidelines8 and aged ≥45 years old (45–80) were included in this study. Risk factors of AMD other than OA were excluded by a face to face questionnaire. Patients with history of alcohol consumption, smoking, hypertension, diabetes, 2ry OA, arthritis of diseases other than OA, chronic inflammatory diseases, chronic infection as tuberculosis were excluded.
Two hundred and twenty-two [222] patients were involved in this study and asked about medical history, family history of OA, exercise type and duration/week, calcium intake and vitamin D supplement intake. They were subjected to clinical examination especially Musculoskeletal examination, body mass index (BMI) calculation, and Ophthalmological examination (fundus examination, slit lamp examination, intraocular pressure (IOP) measurement and visual acuity). Patients demographic details are presented in Table 1.
 |
Table 1 The Characteristics of the Patients |
Radiographs of anteroposterior view and weight-bearing position for both hips and both knees and posteroanterior view for hands were done for all subjects. Kellgren and Lawrence grading score9 was used to evaluate the radiological severity of OA.
Optical Coherence Tomography (OCT), Fundus Fluorescein Angiography (FFA) were used for evaluation of the macula. AMD was classified as: -
Early AMD
Cases with drusen from 63 to 124 um with no pigmentary changes
Intermediate
Cases with drusen 125 um or larger and cases with drusen from 63 to 124 um with pigmentary changes
Late AMD
Neovascular AMD (NV) or geographic atrophy (GA)
NV is serous/hemorrhagic retinal pigment epithelial detachment and/or subretinal neovascular membrane and/or subretinal fibrosis with no retinal vasculopathy.
GA is retinal pigment epithelium depigmentation in area of 175 um or larger.10,11
Statistical Methods
The collected data were revised, coded, tabulated and introduced to a PC using Statistical package for Social Science (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Data were presented and suitable analysis was done according to the type of data obtained for each parameter. Kolmogorov–Smirnov test was done to test the normality of data distribution. Significant data were nonparametric. Mean, Standard deviation (±SD) were used to describe parametric numerical data, while Median and range were used for non-parametric numerical data. Frequency and percentage were used for non-numerical data. Student’s T-test was used to assess the statistical significance of the difference between two study group means. Mann Whitney Test (U-test) was used to assess the statistical significance of the difference of a non-parametric variable between two study groups. Correlation analysis was used to assess the strength of association between two quantitative variables. The correlation coefficient defines the strength and direction of the linear relationship between two variables. Logistic regression analysis was used for prediction of risk factors, using generalized linear models. N.B: p is significant if <0.05 at confidence interval 95%.
Results
Our study included 222 OA patients (58 males (26.1%) and 164 females (73.9%)), 18% of them (40 patients) were asymptomatic and diagnosed radiologically as primary OA and 82% of them (182 patients) were symptomatic. There was overlapping in the affected joints with knee OA was detected in 206 persons, hip OA in 45 and hand OA in 26 persons.
AMD was detected in 46 OA patients (10 males (21.7%), 36 females (78.3%)), 19 cases (41.3%) had early AMD (6 males, 13 females), 15 cases (32.6%) had intermediate AMD (3 males, 12 females) and 12 cases (26.1%) with late AMD (1 male, 11 females). Cases with late AMD were seven cases of NV and 5 cases with GA. (Figure 1)
|
Figure 1 OCT images of some AMD cases: (A) Early AMD (white arrow: drusen, (B) Intermediate AMD (white arrow: pigmentary changes, (C) Late AMD with geographic atrophy (white arrow: macular atrophy), (D) Late AMD with CNV (white arrow: CNV). |
There were significant differences between OA patient with AMD and those without AMD regarding age, disease duration, disease severity, family history of OA, daily mild exercise, and calcium and vitamin D intake. (Table 1)
Regression analysis was conducted for prediction of AMD using age, gender, duration, BMI, family history, symptoms, severity, exercise, calcium and vitamin D intake as covariates. (Table 2)
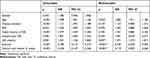 |
Table 2 Regression Analysis for Prediction of AMD in Primary OA Patients |
In univariable analysis older age, longer disease duration, higher BMI, positive family history, symptomatic OA, more severe OA, low exercise and less calcium and vitamin D intake were significantly associated with AMD occurrence in Primary OA patients.
Taking significant covariates in univariable into multivariable analysis revealed that only older age, more severe OA, low exercise and less calcium and vitamin D intake were considered independent risk factors for AMD development in Primary OA patients.
There was a significant correlation between AMD severity stages and OA severity grading score (r = 0.876, p<0.001) (Figure 2). The distribution of AMD stages in different OA grades is shown in Table 3.
 |
Table 3 AMD in Different OA Grades |
|
Figure 2 Correlation between OA severity grading and AMD stages (r = 0.876, p<0.001). |
Discussion
Both AMD and OA are degenerative diseases linked to aging and, in both diseases, the extracellular matrix is involved in pathogenesis.8 The two diseases share some disease mechanisms, like implication of the complement pathway of the innate immune system.9 Reliable biochemical and genetic evidences have verified that complement dysregulation is a mark of AMD vulnerability.12,13 Also, evidence from biochemical studies and animal models has recommended a share for complement activation in OA.14
AMD is a degenerative disease of the photoreceptors and retinal pigment epithelium of the macula. Early detection is valued as it is the third worldwide cause of blindness in old age.12 Previous studies pointed to the coincidence of AMD and inflammatory diseases as gout and OA.7,8 We designed this study to assess the prevalence of AMD in a sample of Egyptian OA patient to highlight the association between the two diseases that may help in early detection of AMD.
We screened 222 Egyptian primary OA patients for presence of AMD. AMD was detected in 46 OA patients (20.7%). There was a significant correlation between the stage of AMD and the severity of OA. Our data pointed to older age, more severe OA, low exercise and less calcium and vitamin D intake as risk factors for AMD development in Primary OA patients.
In the current study, we founded that AMD in primary OA patients (20.7%) is significantly higher than in healthy population. Development of AMD in apparently healthy populations was previously reported in several studies. An Egyptian study screened 532 individuals and reported only 6.6% having AMD.11 Also, in a metanalysis study, AMD was reported in 12.3% in Europeans, 7.4% in Asians and 7.5% in Africans of healthy populations.16
The results from former studies have reported little differing results for any possible association between AMD and OA. Zlateva et al, concluded that patients neovascular AMD patients were more liable to develop arthritis than controls; though, this finding related specifically to RA, and not OA.17 The Age-Related Eye Disease Study (AREDS) detected a tendency toward increased prevalence of arthritis in individuals with neovascular AMD but this was insignificant; moreover, this category was described as “arthritis” and made no discrepancy between OA and RA.18
Regarding stages of AMD in our study, 41.3% of OA patients with AMD had early AMD and 26% had late AMD. That is clearly higher than reported ratios of both AMD stages in apparently healthy individuals (Europeans early: 11.2% and late: 0·5%, Asians early: 6.8% and late: 7.4%, Africans early: 7.1% and late: 0·3%16 Egyptians early: 5.3% and late: 2.4%).11
This emphasizes the suggestion of the co-pathogenesis of both diseases. Inflammaging,6,8 the complement activation,19,20 and the involvement of the extracellular matrix are degenerative pathogenesis implicated in both. However, some previous researches reported the co-incidence of AMD in arthritis-suffering patients but not vice versa.15 Treatments of OA21,22 or/and profoundly systemic inflammatory process23 may be of risk in developing AMD. Moreover, we found that older age, more severe OA, low exercise and less calcium and vitamin D intake were associated with higher incidence of AMD in OA patients.
The strength of this study is AMD screening in all OA stages even the asymptomatic stage that was provided by collecting the patients from outpatients’ clinic in addition to the Elderly Care. Noting that the previous reports were based on hospital admissions and day specialist care representing the more severe end of OA.15 On the other hand, our limitations were the relatively small sample number and neglecting the implications of the treatment lines.
We concluded that primary OA patients are more liable to develop AMD and early detection may be of great benefit in treatable stages that devoid these patients the blindness. Also, we found that less exercise, low calcium and vitamin D intake, older age, and more severe OA stage are risk factors of Primary OA patients to develop AMD.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Valdes AM, Stocks J. Osteoarthritis and ageing. EMJ. 2018;3(1):116–123.
2. Franceschi C, Garagnani P, Morsiani C, et al. The continuum of aging and age-related diseases: common mechanisms but different rates. Front Med (Lausanne). 2018;12(5):61. doi:10.3389/fmed.2018.00061
3. Bortoluzzi A, Furini F, Scirè CA. Osteoarthritis and its management - epidemiology, nutritional aspects and environmental factors. Autoimmun Rev. 2018;17(11):1097–1104. doi:10.1016/j.autrev.2018.06.002
4. Loeser RF, Collins JA, Diekman BO. Ageing and the pathogenesis of osteoarthritis. Nat Rev Rheumatol. 2016;12(7):412–420. doi:10.1038/nrrheum.2016.65
5. Gehrs KM, Jackson JR, Brown EN, Allikmets R, Hageman GS. Complement, age-related macular degeneration and a vision of the future. Arch Ophthalmol. 2010;128(3):349–358. doi:10.1001/archophthalmol.2010.18
6. Chen M, Xu H. Para inflammation, chronic inflammation, and age-related macular degeneration. J Leukoc Biol. 2015;98(5):713–725. doi:10.1189/jlb.3RI0615-239R
7. Singh JA, Cleveland JD, Tsai D-C. Gout and the risk of age-related macular degeneration in the elderly. PLoS One. 2018;13(7):e0199562. doi:10.1371/journal.pone.0199562
8. Rezuș E, Cardoneanu A, Burlui A, et al. The link between inflammaging and degenerative joint diseases. Int J Mol Sci. 2019;20(3):614. doi:10.3390/ijms20030614
9. Altman RD, Hochberg MC, Moskowitz RW, Schnitzer TJ. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43(9):1905–1915.
10. Ferris FL, Davis MD, Clemons TE. A simplified severity scale for age-related macular degeneration: AREDS Report No. 18. Arch Ophthalmol. 2005;123(11):1570–1574. doi:10.1001/archopht.123.11.1570
11. Fadel AM, El Hennawi HM, Bayoumi NH, Elweshahi HMT, Zaki MM. Prevalence of age-related macular degeneration among elderly patients attending Alexandria Main University Hospital. Delta J Ophthalmol. 2016;17:91–96. doi:10.4103/1110-9173.189075
12. Kellgren JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi:10.1136/ard.16.4.494
13. Ardeljan D, Chan CC. Aging is not a disease: distinguishing age-related macular degeneration from aging. Prog Retin Eye Res. 2013;37:68–89. doi:10.1016/j.preteyeres.2013.07.003
14. Urano T, Narusawa K, Kobayashi S. Association of HTRA1 promoter polymorphism with spinal disc degeneration in Japanese women. J Bone Miner Metab. 2010;28:220–226. doi:10.1007/s00774-009-0124-0
15. Keenan TD, Goldacre R, Goldacre MJ. Associations between age-related macular degeneration, osteoarthritis and rheumatoid arthritis: record linkage study. Retina. 2015;35(12):2613–2618. doi:10.1097/IAE.0000000000000651
16. Wong WL, Su X, Li X, et al. prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–e116. doi:10.1016/S2214-109X(13)70145-1
17. Zlateva GP, Javitt JC, Shah SN, et al. Comparison of comorbid conditions between neovascular age-related macular degeneration patients and a control cohort in the medicare population. Retina. 2007;27(9):1292–1299. doi:10.1097/01.iae.0000300915.81866.b8
18. Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: age-related Eye Disease Study Report Number 3. Ophthalmology. 2000;107(12):2224–2232. doi:10.1016/s0161-6420(00)00409-7
19. Wang Q, Rozelle AL, Lepus CM. Identification of a central role for complement in osteoarthritis. Nat Med. 2011;17(12):1674–1679. doi:10.1038/nm.2543
20. Anderson DH, Radeke MJ, Gallo NB. The pivotal role of the complement system in aging and age-related macular degeneration: hypothesis re-visited. Prog Retin Eye Res. 2010;29(2):95–112. doi:10.1016/j.preteyeres.2009.11.003
21. Li L, Li W, Chen CZ, Yi ZHZ, Zhou YY. Is aspirin use associated with age related macular degeneration? A meta-analysis. J Clin Pharm Ther. 2015;40(2):144–154. doi:10.1111/jcpt.12241
22. Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther. 2013;15(S3):S2. doi:10.1186/ar4174
23. Molins B, Romero-Vázquez S, Fuentes-Prior P, Adan A, Dick AD. C-Reactive protein as a therapeutic target in age-related macular degeneration. Front Immunol. 2018;9:808. doi:10.3389/fimmu.2018.00808
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
