Back to Journals » Integrated Blood Pressure Control » Volume 13
Admission and Inpatient Mortality of Hypertension Complications in Addis Ababa
Authors Zeru AB Snr , Muluneh MA
Received 17 June 2020
Accepted for publication 2 September 2020
Published 16 September 2020 Volume 2020:13 Pages 103—110
DOI https://doi.org/10.2147/IBPC.S268184
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Abayneh Birlie Zeru,1 Mikyas Arega Muluneh2
1Department of Public Health, College of Health Science, Debre Berhan University, Debre Berhan, Amhara Regional State, Ethiopia; 2Department of Midwifery, College of Health Science, Debre Berhan University, Debre Berhan, Amhara Regional State, Ethiopia
Correspondence: Abayneh Birlie Zeru
Department of Public Health, College of Health Science, Debre Berhan University, Po. Box: 445, Debre Berhan, Amhara Regional State, Ethiopia
Tel +251919134994
Email [email protected]
Background: The number of people with undiagnosed, untreated, and uncontrolled hypertension is higher in Ethiopia. This in turn increases the risk of developing complications and hospitalization. This study aimed to assess the prevalence of hypertension complication hospitalization among medical admissions and admission outcomes of hypertension complication patients in the medical ward of Saint Peter Specialized Hospital, Addis Ababa.
Methods: We used a hospital-based cross-sectional study. Data were collected by reviewing all medical ward admission logbook records from January 1st, 2018 to December 30th, 2019. An individual patient folder of 308 patients admitted due to hypertension complications was selected for further detailed investigation and then entered into Epi Data version 3.1 and exported to SPSS version 24 statistical software for analysis.
Results: Of the total 2728 medical admissions, 308 (11.3%) were patients with hypertension complications. Hypertension complications account for 308 (11.3%) of all medical admissions. Their mean age and length of hospital stay were 59.85 (± 16.36) years and 11.45 (± 11.48) days, respectively. Near to two-third of 196 (63.6%) of them were stroke patients followed by 76 (24.7%) heart disease. Fifty-two (16.9%) hypertension complication patients died at admission which accounts for 52 (14.6%) of all medical ward deaths. As age increases, the risk of death at admission increases by 6.5%. Similarly, the risk of death increased by three-fold for a month increase in the duration of anti-hypertensive drug discontinuation. Rural residents had a 3.5% lesser risk of death than urban patients.
Conclusion: Hypertension complications had a significant share of the medical ward mortality rate. Cerebrovascular and cardiovascular complications were common causes of hospitalization and inpatient death. Old age, urban residence, and prolonged duration of anti-hypertensive drug discontinuation increased the risk of death at admission.
Keywords: hypertension complication, hypertension-related admission, inpatient mortality
Introduction
The burden of non-communicable diseases (NCDs), mainly cardiovascular diseases (CVDs), cancers, chronic respiratory diseases, and diabetes are major public health challenges worldwide. Currently, most 63% of global deaths are related to NCDs and by 2030 about three-fourth global deaths are estimated to be due to NCDs. CVDs are responsible for 48% of NCDs related deaths.1 According to the 2016 World Health Organization (WHO) global health estimate, CVDs such as ischemic heart disease (16.6%) and stroke (10.2%) are the top leading cause of global deaths.2 Hypertension is known to be the major modifiable risk factor for CVD morbidity and mortality, it is estimated more than half of CVD deaths are attributed to hypertension.3
Hypertension is defined as a persistent elevation of systolic blood pressure (BP) of 140 mmHg or greater and/or diastolic BP of 90 mmHg or greater, taken at least twice on two separate occasions. The higher the pressure in blood vessels the harder the heart has to work to pump blood. If left uncontrolled, hypertension can lead to a heart attack, an enlargement of the heart, and eventually heart failure. Blood vessels may develop bulges (aneurysms) and weak spots due to high pressure, making them more likely to clog and burst. The pressure in the blood vessels can also cause blood to leak out into the brain causing stroke. Hypertension can also lead to kidney failure, blindness, rupture of blood vessels, and cognitive impairment.4–6
Hypertension is one of the most important preventable causes of CVDs and premature mortalities. Hypertension is responsible for 45% and 51% of deaths due to heart disease and stroke, respectively.7,8 The prevalence of hypertension is increasing mainly in middle- and low-income countries (MLICs). Its global prevalence was estimated to be 972 million (26.4% of world adult population) in 2000 and rose to 1.3 billion in 2015, and in 2025 around 1.56 billion (29.2% of world adult population) were predicted to have hypertension. In developing countries, hypertension was estimated to increase by 80% from 639 million in 2000 to 1.15 billion in 2025.9 The increment in population growth, aging, and behavioral risk factors, such as unhealthy diet, harmful use of alcohol, sedentary life, and overweight are responsible for increased hypertension burden in developing countries. The prevalence of hypertension is highest in the African with 46% among adults aged 25 and above, while the lowest prevalence at 35% is found in America.
In Ethiopia, earlier studies have shown the prevalence of hypertension estimated to be somewhere between 12% and 30%.10–13 According to a community-based study in Jigjiga10 and Dire Dawa12 of eastern Ethiopia 63.8% and 51.4%, hypertensive subjects did not know they have had hypertension, respectively. From those who are on antihypertension medication only less than 40% can control their BP.10,13,14 This reflects that people with undiagnosed and untreated hypertension, and uncontrolled hypertension for therapy are high in the country which increases the risk of developing complication and related hospitalization.
Thought the increment in the prevalence of hypertension was evidenced in Ethiopia, there is no clear understanding on the level of hypertension-related hospitalization and admission outcomes because of a lack of sufficient local studies. Therefore, this study was aimed to assess the prevalence of hypertension complications among medical admissions. We also tried to determine the magnitude of admission outcomes of hypertension complications patients and factors associated with death outcomes in Saint Peter Specialized Hospital.
Methods and Materials
Study Design, Period and Setting
This is a hospital-based cross-sectional study conducted to investigate the prevalence and admission outcomes of hypertension complication in the medical ward of Saint Peter Specialized Hospital, Addis Ababa from January 25th to 30th, 2020. The hospital is one of the oldest public hospitals in Addis Ababa, the capital city of Ethiopia, which was established in 1948. The hospital had been a national tuberculosis diagnosis and treatment center until 2005. Currently, the hospital is providing comprehensive health care services at outpatient and inpatient levels. The hospital has a total of 280 beds and 70 beds are assigned to the medical ward for medical cases admission.
Patients admitted with any hypertension-related health disorders were considered as hospital admission due to hypertension complications. All patients admitted to the medical ward of the hospital from January 1st, 2018 to December 30th, 2019, because of hypertension-related health disorders such as stroke, cardiovascular, renal or peripheral vascular diseases, and hypertensive emergencies were included. However, patients with those health conditions and additional comorbidities such as diabetes mellitus, and patients with <140/90mmHg BP at admission or with no documented anti-hypertensive medication history were excluded from the study.
Data Sources and Collection Procedures
Hypertension was defined as admission blood pressure of ≥140 mmHg systolic and/or ≥90 mmHg diastolic or previously on antihypertension medication. Blood pressure was measured by the physician or nurse at the emergency department using a standard mercury sphygmomanometer. Patients were allowed to sit for 5 minutes before measurement than at least two BP measurements; spaced 1–2 minutes apart were taken. This was repeated every 30 minutes until the patient gets stable per the national guideline.6 We took the average of the first two consecutive records as patient’s BP at admission. We considered the type of hypertension complication recorded on the patient discharge notes as the final diagnosis of hypertension complication.
Data were collected through reviewing medical records; admission logbooks and patient folders by the investigation team using data extraction sheet. First, we reviewed medical admission logbooks to tally the sex and admission outs of all medically admitted patients, and to identify and prepare the list of Unique Medical Record Number (UMRN) of 315 patients admitted due to hypertension complications. Then, using patients UMRN those patient folders were drawn from the medical record room and reviewed for data collection. Due to incomplete recording of important variables like admission BP, type of hypertension complication, and outcome of admission, seven patient folders were excluded and we were able to extract data from 308 patient folders.
Data retrieved from patient folders were: age, sex, ethnicity; residence, occupation, alcohol consumption, cigarette smoking, salt restriction, known hypertensive or not, duration of hypertension, antihypertensive medication, type of anti-hypertensive drug, history of drug discontinuation and its duration, type of hypertension complication, admission BP, admission pulse rate, admission respiration rate, duration of hospital stay and admission outcome.
Statistical Analysis
The collected data were checked for completeness and consistency daily by principal investigators. Then entered into Epi Data version 3.1 and exported to SPSS version 24 statistical software for analysis. Categorical variables were summarized as frequency and percentages, whereas continuous variables were summarized using mean and standard deviations. Binary logistics regression was applied to identify variables associated with death admission outcomes. Those variables with p-value ≤0.2 on bi-variable analysis were included in the multivariable analysis. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were used to measure the magnitude of association p-values of <0.05 to declare the statistical significance of the association between the covariates and the dependent variable.
Ethical clearance was obtained from the medical college of Debre Berhan University and Saint Peter’s Specialized Hospital ethical review committees. Permission to proceed was granted Saint Peter’s Specialized Hospital administrative. For confidentiality purpose, information related to personal identification was not included in the data extraction format.
Result
Description of Medically Admitted Patients
A total of 2728 patients were admitted, consisting of 1468 (53.8%) females and 1260 (46.2%) males, at the medical wards of Saint Peter Specialized Hospital from 2018 to 2019. Three hundred and fifty-six deaths were recorded, giving an overall mortality rate of 13.05% among medical admissions. Even though there was no statistically significant difference in mortality rate among female and male patients, higher deaths were observed among females (13.6%) than male (12.4%) medically admitted patients (Table 1).
 |
Table 1 Description of Medical Ward Admitted Patients by Sex, Cause of Admission, and Survival Status at the Medical Ward of Saint Peter Specialized Hospital from Jan. 2018 to Dec. 2019 |
Of the total 2728 medical admissions, hypertension complications account for 308 (11.3%). It also accounts for 52 (14.6%) of all deaths in the medical ward (among males 22/156 (14.1%) and females 30/200 (15.0%)). There was a statistically significant difference in mortality rate between patients admitted due to hypertension complications and those admitted due to other medical reasons (Table 1).
Socio-Demographic, Behavioral and Clinical Characteristics
As shown in Table 2, the majority of 178 (57.8%) hypertension complication admissions were females and 130 (42.2%) males. Their mean age at admission was 59.85 (± 16.36) years. Two-fifth 126 (40.9%) of patients were found in the age range of 61–80 years. Similarly, the majority of 30/52 (57.7%) deaths occurred on 61–80 years old patients. Most hypertension complication-related admissions and deaths were from urban residents. Concerning occupation, 66 (21.4%) were government employees, 58 (18.8%) private business, 56 (18.2%) housewives, and 56 (18.2%) were farmers.
 |
Table 2 Socio-Demographic and Admission Outcome of Hypertension Complication at the Medical Ward of Saint Peter Specialized Hospital |
From 308 patients admitted due to hypertension complications, 54 (17.5%) did not know they were hypertensive before. Of 254 known hypertensive patients 26 (10.2%) were not taking any form of anti-hypertensive medications before. Two hundred twenty-eight (89.8%) were on anti-hypertensive medication and the majority 98 (43.0%) of them were taking Enalapril followed by 60 (26.3%) combined drug and 38 (16.7%) Nifedipine. The prevalence of anti-hypertensive drug discontinuation history was 124 (54.4%). Regarding substance use, 138 (44.8%) and 88 (28.6%) hypertension complication admitted patients had alcohol drinking and smoking habit, respectively. Most 250 (81.2%) patients were not on salt restriction before admission (Table 2).
The mean duration of hypertension was 6.68 (± 4.85) years. Those who were on anti-hypertensive medication took the drug for an average of 5.41 (± 3.44) years. The mean duration of anti-hypertensive drug discontinuation was 4.57 (± 2.57) months. It was higher among the dead (7.14 months) than alive (3.20 months) patients. The mean systolic and diastolic blood pressure at admission was 156.88 (± 15.42) mmHg and 95.82 (± 7.96) mmHg, respectively. The average length of hospital stay of patients with hypertension complications was 11.45 (± 11.48) days ranging from 1 day to 84 days (Table 3).
 |
Table 3 Clinical Characteristics of Patients with Hypertension Complication at the Medical Ward of Saint Peter Specialized Hospital |
Type of Hypertension Complications and Admission Outcomes
Regarding the type of complication, near to two-third of 196 (63.6%) hypertension complication admissions were due to stroke followed by 76 (24.7%) heart disease, 16 (5.2%) renal disease and 16 (5.2%) hypertensive emergency (Figure 1).
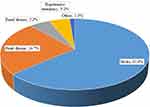 |
Figure 1 Type of hypertension complications admitted in medical ward of Saint Peter Specialized Hospital. |
As shown in Figure 2, the majority 224 (72.7%) hypertension complication admissions were discharged with improvement, 52 (16.9%) dead, 12 (3.9%) referred to another hospital and 20 (6.5%) left the hospital against medical advice (Figure 2).
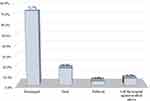 |
Figure 2 Admission outcomes of hypertension complication patients in medical ward of Saint Peter Specialized Hospital. |
Factors Associated with Death Admission Outcome
Variables found to have a p-value of ≤0.2 on the bi-variable analysis were candidates for multi-variable analysis. These variables were age, residence, alcohol drinking habit, cigarette smoking, duration of hypertension, duration on anti-hypertensive medication, duration of anti-hypertensive drug discontinuation, type of complication, and length of hospital stay.
Age, residence, and length of anti-hypertensive drug discontinuation were independently associated with death admission outcomes. As the age of the patient increases by one year, the risk of death increased by 6.5% (AOR = 1.065, 95% CI [1.004–1.129]). Rural residents had 3.5% lesser risk of death than urban patients (AOR = 0.035, 95% CI [0.004–0.289]). For every one month increase in anti-hypertensive drug discontinuation, the risk of death increased by three-fold (AOR = 3.062, 95% CI [2.007–4.673]) (Table 4).
 |
Table 4 Bi-Variable and Multivariable Analysis to Identify Factors Associated with Death of Hypertension Complication Admissions at the Medical Ward of Saint Peter Specialized Hospital |
Discussion
In this study, hypertension complications accounted for 11.3% of adult medical admissions in SPSH. At least one in every ten medical admissions was hypertension complications which are comparable to 12.1% report of Saint-Paul Hospital in Addis Ababa.15 This finding is lower than 23.7% and 20.2% report in tertiary hospitals in Southeast Nigeria16 and the University of Benin Teaching Hospital17 respectively. Study setting differences like the type of hospitals in the study might be the reason why this study had lower hypertension complication admission rates. Because most diseases related to hypertension complications are serious and life-threatening, patients require referral to advanced hospitals for further investigation and better management. This makes higher hypertension complications admissions rate in tertiary and referral hospitals.
According to this study, hypertension complications had a significant contribution to the mortality rate of medically admitted patients in Saint Peter Specialized Hospital. A higher mortality rate was observed among hypertension complication admissions than other medical admissions. The mortality rate of 16.9% among hypertension complication admission was significantly higher than 13.05% overall mortality rate at the medical ward. Likewise, hypertension complication accounts for 11.3% of medical admissions nevertheless it accounts for 14.6% of medical deaths. Studies in Nigeria reported mortality rate among hypertension complication admissions vs overall medical mortality rate of 22.1% vs 16.1%17 in the University of Benin Teaching Hospital and 42.9% vs 23.7%16 in Southeast Nigeria, respectively. This study finding of 16.9% mortality rate among hypertension complication admissions was lower than 22.2% report in Mbuji Mayi, Congo,18 and 42.9% in the University of Nigeria Teaching Hospital, Enugu.19
Hypertension is the most significant risk factor for cardiovascular diseases,5,8,20,21 about 86% of CVD admissions were complications of hypertension.22 A study in the south-west of Nigeria showed that over 90% of hypertension complications were cardiovascular diseases.23 Stroke was the more prevalent complication of hypertension in Brazil.24 Similarly, in this study 63.6% were stroke and 24.7% were hypertensive heart diseases which together accounts for 88% all hypertension complication admissions. This is in line with study reports in the Midwest region of Brazil24 and Indonesia.25,26 Similarly, stroke (44.4%) and hypertensive heart failure (27.8%) were the commonest types of hypertension complications in Northeast Nigeria.16
In this study, most 80.8% of deaths in hypertension complication admitted patients occurred on stroke patients. Similarly, higher (74%) of hypertension deaths were among stroke patients in Black lion hospital, Addis Ababa.27 Most hypertension-related deaths are due to heart diseases and stroke.8,21,24,28
Aged patients admitted with hypertension complications are more likely to end up with death. For a year increase in age, there is a 6.5% increased risk of death by hypertension complication at admission. This is congruent with 2.4% and 4.0% increased probability of death reported in Nigeria16 and Ghana.29
A systematic review in developing countries revealed that around half (47.34%) of hypertensive patients were non-adherent to their medication.30 Poor adherence to antihypertensive medication, commonly caused by drug discontinuation or suboptimal use of the prescribed drugs, is the main cause for uncontrolled BP and less than 50% hypertensive patients with treatment controlled their BP.21,31,32 Poor adherence to antihypertensive medication correlates with a higher risk of complications. Poor adherence is commonly caused by drug discontinuation or suboptimal use of the prescribed drugs. According to the present study, the duration of drug discontinuation was associated with an increased risk of inpatient death of patients with hypertension complication, for every 30-day increase of the duration of drug discontinuation the risk of death in hypertension complication increased by three-fold.
The cross-sectional nature of this study limits in establishing causality based on the observed association between the covariates and the dependent variable.
Conclusions
Hypertension-related complications were responsible for 11.3% of medical admissions and 14.6% of medical ward deaths in Saint Peter Specialized Hospital. Cerebrovascular and cardiovascular complications were common causes for admission and inpatient death of patients with hypertension complications. Stroke and hypertensive heart diseases account for 63.6% and 24.7% admissions of hypertension complications. Most 80.8% of deaths occurred among stroke patients. Old age, urban residence, and prolonged duration of anti-hypertensive drug discontinuation were associated with increased risk of death admission outcome.
Acknowledgments
The authors thank Saint Peter Specialized Hospital administration office for their permission to conduct the study. We acknowledge the assistance of medical ward and medical record room staffs in the data collection process of identifying medical logbooks and drawing patient folders.
Disclosure
The authors received no specific funding for this work. The authors report no conflicts of interest for this work.
References
1. WHO. The global burden of disease: 2004 update. Geneva, Switzerland: World Health Organization; 2008.
2. Global health estimates 2016. Deaths by cause, age, sex, by country and by region, 2000–2016. Geneva: World Health Organization; 2018.
3. He FJ, MacGregor GA. Blood pressure is the most important cause of death and disability in the world. Eur Heart J Suppl. 2007;9:B23–B8.
4. WHO. Hypertension 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.
5. A global brief on hypertension. Geneva, Switzerland: World Health Organization; 2013.
6. MOH. Guidelines on clinical and programmatic management of major non communicable diseases. Addis Ababa: Ethiopian Ministry of Health; 2016.
7. Franklin SS, Thijs L, Hansen TW, et al. International database on ambulatory blood pressure in relation to cardiovascular outcomes investigators. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the international database on ambulatory blood pressure monitoring in relation to cardiovascular outcomes population. Hypertension. 2012;59:564–571.
8. Arima H, Barzi F, Chalmers J. Mortality patterns in hypertension. J Hypertens. 2011;29(suppl 1):S3–S7. doi:10.1097/01.hjh.0000410246.59221.b1
9. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi:10.1016/S0140-6736(05)17741-1
10. Asresahegn H, Tadesse F, Beyene E. Prevalence and associated factors of hypertension among adults in Ethiopia: a community based cross-sectional study. BMC Res Notes. 2017;10:629. doi:10.1186/s13104-017-2966-1
11. Kiber M, Wube M, Temesgen H, Woyraw W, Belay YA. Prevalence of hypertension and its associated factors among adults in Debre Markos Town, Northwest Ethiopia: community based cross-sectional study. BMC Res Notes. 2019;12:406. doi:10.1186/s13104-019-4431-9
12. Roba HS, Beyene AS, Mengesha MM, Ayele BH. Prevalence of hypertension and associated factors in Dire Dawa City, Eastern Ethiopia: a community-based cross-sectional study. Int J Hypertens. 2019;2019:9. doi:10.1155/2019/9878437
13. Bayray A, Meles KG, Sibhatu Y. Magnitude and risk factors for hypertension among public servants in Tigray, Ethiopia: a cross-sectional study. PLoS One. 2018;13(10):e0204879. doi:10.1371/journal.pone.0204879
14. Berhe DF, Taxis K, Haaijer-Ruskamp FM, Mulugeta A, Mengistu YT, Mol PGM. Hypertension treatment practices and its determinants among ambulatory patients: retrospective cohort study in Ethiopia. BMJ Open. 2017;7:e015743. doi:10.1136/bmjopen-2016-015743
15. Bane A, Bayisa T, Adamu F, Abdissa SG. Medical admissions and outcomes at Saint Paul’s Hospital, Addis Ababa, Ethiopia: a retrospective study. Ethiop J Health Dev. 2016;30(1):50–56.
16. Kolo PM, Jibrin YB, Sanya EO, Alkali M, PeterKio IB, Moronkola RK. Hypertension-related admissions and outcome in a Tertiary Hospital in Northeast Nigeria. Int J Hypertens. 2012;2012:6. doi:10.1155/2012/960546
17. Ukoh UA. Admission of hypertensive patients at the University of Benin Teaching Hospital, Nigeria. East Afr Med J. 2007;84(7):329–335.
18. M’Buyamba-Kabangu J-R, Biswika RT, Thijs L, et al. In-hospital mortality among black patients admitted for hypertension-related disorders in Mbuji Mayi, Congo. Am J Hypertens. 2009;22(6):643–648. doi:10.1038/ajh.2009.47
19. EBArodiwe IS, Nwokediuko S. Case fatality among hypertension-related admissions in Enugu, Nigeria. Niger J Clin Pract. 2009;12(2):153–156.
20. Jagadeesh G, Balakumar P, Maung-U K. Pathophysiology and Pharmacotherapy of Cardiovascular Disease: Hypertension: Introduction, Types, Causes, and Complications. Switzerland: Springer International Publishing; 2015.
21. Williams B, Mancia G, Spiering W, et al. 2018ESC/ESH guidelines for the management of arterial hypertension. J Hypertens. 2018;36:1953–2041. doi:10.1097/HJH.0000000000001940
22. Oguanobi NI, Ejim EC, Onwubere BJ, et al. Pattern of cardiovascular disease amongst medical admissions in a regional teaching hospital in Southeastern Nigeria. Niger J Cardiol. 2013;10(2):77–80. doi:10.4103/0189-7969.127005
23. Adedapo AD. Rising trend of cardiovascular diseases among South-Western Nigerian female patients. Nig J Cardiol. 2017;14:71–74. doi:10.4103/njc.njc_23_17
24. Filho GCG, Sousa ALL, TdSV J, Souza WSB, Jardim PCBV. Progression of blood pressure and cardiovascular outcomes in hypertensive patients in a reference center. Arq Bras Cardiol. 2015;104(4):292–298.
25. Fihaya FY, Sofiatin Y, Ong PA, Sukandar H, Roesli RM. Prevalence of hypertension and its complication in Jatinangor 2014. J Hypertens. 2015;33:e35. doi:10.1097/01.hjh.0000469851.39188.36
26. Suling FRW, Agustian Z, Enggar D. 18 Prevalence of hypertension and its complication in emergency room Christian University of Indonesia Hospital in 2017. J Hypertens. 2018;36:e5. doi:10.1097/01.hjh.0000544383.36453.a9
27. Worku T, Tadesse Y, Hughes P, Lemessa T. Patters of complications seen in patients with hypertension admitted to Tikur Anbessa Hospital: a retrospective analysis. Ethiop Med J. 2015;51–56.
28. IFPMA. Hypertension: putting the pressure on the silent killer. 2016.
29. Nuamah K, Bonful HA, Yeboah JD, et al. Characteristics of inpatient hypertension cases and factors associated with admission outcomes in Ashanti Region, Ghana: an analytic cross-sectional study. Int J Hypertens. 2017;2017:11. doi:10.1155/2017/6537956
30. Dhar L, Dantas J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol. 2017;7:211–250. doi:10.4236/ojepi.2017.73018
31. Krousel-Wood M, Joyce C, Holt E, et al. Predictors of decline in medication adherence: results from the cohort study of medication adherence among older adults. Hypertension. 2011;58:804–810. doi:10.1161/HYPERTENSIONAHA.111.176859
32. Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125:882–887. doi:10.1016/j.amjmed.2011.12.013
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
