Back to Journals » Patient Preference and Adherence » Volume 14
Adherence with Medical Therapy for Primary Open-Angle Glaucoma in Kenya – A Pilot Study
Authors Murdoch I , Nyakundi D , Baker H , Dulku S, Kiage D
Received 29 October 2019
Accepted for publication 18 December 2019
Published 10 February 2020 Volume 2020:14 Pages 221—225
DOI https://doi.org/10.2147/PPA.S236468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ian Murdoch, 1 David Nyakundi, 2 Helen Baker, 1 Simon Dulku, 3 Daniel Kiage 2
1Institute of Ophthalmology, London EC1V 9EL, UK; 2Innovation Eye Centre Ltd, Kisii, Kenya; 3University Hospitals Birmingham NHS Foundation Trust, Birmingham B15 2WB, UK
Correspondence: Ian Murdoch
Institute of Ophthalmology, Bath Street, London EC1V 9EL, UK
Email [email protected]
Background/Objectives: Adherence is a major challenge in topical glaucoma therapy, particularly in an African context. We report a pilot study assessing adherence independently for the first time in an African context.
Subjects/Methods: Participants with newly diagnosed open-angle glaucoma received a weighed bottle of Lumigan 0.01% with counselling on therapy. The bottles were returned monthly for renewal and weighed on return to estimate drops taken during the period. Data collection was for one year with a short compliance questionnaire.
Results: 11 patients participated. 5 (45%) failed to complete one full year of topical therapy. The overall mean number of drops per eye per day was 1.74 (SD 0.69) for the 6 with one year of monthly returned bottles and controlled IOPs at each visit. Self-perception of compliance in these patients was good.
Conclusion: The signs of poor adherence based on both self-report (previous literature), and in this small-scale study of an objective measure suggest medication may not be the first-line treatment of choice in this environment. Our report does, however, raise the possibility that those patients who return for repeat prescriptions and review are indeed adhering to their treatment regimens.
Keywords: adherence, glaucoma, Africa, medical treatment
Introduction
Glaucoma is the world’s second most prevalent blinding condition causing irreversible visual loss.1 The prevalence of primary open-angle glaucoma (POAG) is often higher in individuals of African descent than in Caucasians2,3. There is now clear evidence that lowering intraocular pressure (IOP) reduces the rate of progression.4–6
Pressure may be lowered by medical therapy, laser therapy or surgical intervention. The most common first-line therapy is medical therapy.7 In high-income countries, there are well-recognised problems with medical therapy. Firstly adherence is a major challenge.8 Secondly, there are adverse effects, both systemic and topical.9 In an African context, we have identified 8 published studies investigating adherence shown in Table 1.
 |
Table 1 Published Studies Reporting Adherence with Medical Therapy for Glaucoma in Sub-Saharan Africa |
Two studies looked at the opinions of ophthalmologists, three studies involved questionnaire to patients who had been on medical therapy for over 6 months. Two studies were medical record reviews and the final study involved focus groups with patients. Poor adherence was consistently reported. No study had investigated the validity of the finding using an alternative assessment we, therefore, designed the pilot study presented here. We reduced the impact of cost by supplying the drops for free and undertaking the work in a local hospital setting to minimise the challenges of travel to receive therapeutic supplies.
Methods
This study was undertaken in Innovation Eye Clinic, Kisii, Kenya. Ethical permission for the trial, of which this is a component, was given by the Aga Khan University Faculty of Health Sciences Research Ethics Committee. This study was conducted in accordance with the Declaration of Helsinki. The trial was a randomised controlled trial of selective laser trabeculoplasty compared to medical therapy. It had to be abandoned due to recurrent challenges maintaining a functional laser machine.
Following written, informed consent to participation in the study, patients received counselling in glaucoma, the aims of therapy and drop technique. They were supplied with a bottle of topical bimatoprost 0.01% to use once a day in the affected eye(s) and informed that the next bottle would be supplied free of charge in one months’ time upon return of the current bottle. All bottles were weighed prior to being given to patients and weighed again upon return; the underlying assumption being that the difference in weights represented the quantity of drug used in therapy. A short questionnaire on adherence was completed.
Primary Outcome Measure
Three bottles of lumigan 0.01% were weighed and 6.99, 6.99 and 7.00 g. A large sample was not taken since the weight was taken at point of delivery. Two bottles were weighed 5 times each with an average variation of 0.003 g showing the accuracy of the scales. Two bottles had their plastic covers removed. These weighed 0.155 and 0.15 g. In view of the potential for variation in this weight, it was decided to remove the plastic seals prior to weighing and release of bottles to patients.
One bottle was weighed after each drop, it contained 76 drops. The total weight of drug in the bottle was 2.85g. Each drop amounted to an average weight of 0.0375 g (SD 0.010).
Questionnaire
Guided by social science expertise (HB) and following discussion with patients and staff, a simple questionnaire was developed translated into Kiswahili and back translated to ensure consistency. This was then administered to 5 clinic patients taking medical therapy for feedback. The first two questions were retained unaltered in the final version; however, a third open-ended question was added inviting their view as to why they were not adhering. This questionnaire was aimed at gaining a basic measure of self-perceived compliance. The final questionnaire in both English and Kiswahili is shown in Figure 1.
 |
Figure 1 Questionnaire on drug adherence administered to patients. |
Results
A total of 11 patients participated in the study. Of these 5 (45%) failed to complete one full year of topical therapy for a variety of reasons. One came back for one further bottle then said he was “otherwise engaged” and could not come. One came for bottles for four months then stopped attending and was seen at 6 months at which stage his non-adherence was discussed and he was listed for surgery. One developed itchy red eyes after 6 months on therapy and defaulted further drops and follow-up from that report. One returned the first bottle and did not attend following this, it turned out her son had taken her to another hospital; we do not know the outcome following this. One patient had no reduction in IOP from the drops and was listed for trabeculectomy surgery.
From the above, the topical drug failed to lower pressure in 1 (9%) and adverse effects were a component of non-adherence in 4 (36%).
A total of 6 (55%) completed one year of monthly follow-up with returned bottles and controlled IOPs at each visit. The baseline study showed each drop amounted to an average weight of 0.0375 g (SD 0.010) for Lumigan 0.01%. Using this and the weight of drug removed from the returned bottles all patients showed consistent adherence. The overall mean number of drops per eye per day was 1.74 (SD 0.69). Over the eleven months of follow-up, there was a suggestion of slight tail off in frequency of drop use in the last two months only (Table 2).
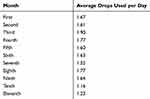 |
Table 2 Average Number of Drops Used per Day by 6 Patients on Topical Glaucoma Therapy Returning Weighed Bottles Monthly |
Of importance is that every adherent patient had a comment in the notes that they were experiencing itching, fullness or redness of the eyes on the drops. Thus, adherence was strong despite topical side effects. Following the study 4 remained on topical therapy 2 on Lumigan and two on t-bet [travoprost 0.004% and Timolol 0.5%] since that is a cheaper drug for them. One patient was lost to follow-up and the final patient had a pressure of 26 on final return and was listed for trabeculectomy.
Of the five who failed to complete a year on lumigan therapy, adherence data existed for four. The mean number of drops per day per eye was 1.69 (SD 0.90). As noted above, two were listed for surgery because of non-adherence.
Seven patients completed the questionnaire concerning compliance. All reported good compliance and found the drugs easy to use as advised. Two patients reported missing no drops and the remainder reported missing 1–3 doses per week.
Discussion
We recognise that this pilot study is small and thus prone to potential bias. None-the-less the findings do present some interesting insights. Our finding of 1/11 (9% (95% CI 1–40%)) with poor response to bimatoprost is in keeping with Sherwood et al who reported 25% (95% CI 21–29%) failing to have a pressure drop to 18mmHg or lower.18 The finding of non-adherence in 4/11 (36% (95% CI 14–65%)) is lower than several of the previous reports (Table 1). There are some factors that may explain the improved adherence in our study. Firstly the patients had consented to participate in a study hence were a selected population. Secondly, there was no charge for the therapy. Thirdly there was monthly contact with the patients which may contribute to adherence by reinforcement of the therapeutic message. Reports of non-adherence are hugely variable not least because of very different methods of assessing adherence.20 In high-income settings, comparable measures generally suggest levels of non-adherence between 10% and 20%.8
To our knowledge, this is the first report in a sub-Saharan population attempting to validate attendance and reported adherence by an alternative assessment of drop use. Our findings suggest that those who attend and receive regular bottles, take the drops as prescribed. The use of an unobtrusive medication monitor is regarded as the “gold standard” in measuring adherence. Such a device was not available to us hence we used the bottle weight before and after use. Male gender, poor knowledge of the disease and complex dose frequencies are definite risk factors of poor compliance.20 Our patients had received counselling in the disease and the once daily dosage regimen is the least complex possible. These may have contributed to the high adherence we found.
Establishing the use of drops does not, of course, mean the drops are entering the eye. Davis et al reviewed the literature on drop instillation and found reports suggest 6.8–37.3% of patients miss the eye with the drop.21 None-the-less our patients had a reduction in pressure implying the active ingredient was reaching their eye; at least on the days they were assessed.
All of our patients mentioned redness or irritation in the eyes at some stage during the study (recoded in the notes). This is recognised as a common topical side effect of bimatoprost, Parish et al reporting 35% with this symptom after 12 weeks therapy.19 It is of note that, despite these symptoms, our adherent patients persisted with their medication. We believe this may reflect the counselling they received in the disease and its treatment.
The questionnaire was informative in illustrating that patient-reported compliance is in agreement with the weight results of drops taken.
The signs of poor adherence based on both self-report (previous literature Table 1), and in this small-scale study of an objective measure, suggest medication may not be the first-line treatment of choice in this environment. Our report does, however, raise the possibility that those patients who return for repeat prescriptions and review are indeed adhering to their treatment regimens.
Abbreviations
IGA, international glaucoma association; IOP, intraocular pressure; POAG, primary open-angle glaucoma.
Declarations
Ethical permission for the study was given by the Aga Khan University Faculty of Health Sciences Research Ethics Committee (Ref: 2012/24).
Acknowledgment
We are grateful for an unrestricted grant from L’Occitane foundation and the International Glaucoma association for supporting this work ID 520440 F89 IGA Murdoch.
Author Contributions
Ian Murdoch undertook the analysis of the data. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Available from: https://www.iapb.org/wp-content/uploads/world-vision-report-accessible1.pdf.
2. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–2090. doi:10.1016/j.ophtha.2014.05.013
3. Kyari F, Abdull MM, Bastawrous A, Gilbert CE, Faal H. Epidemiology of glaucoma in sub-Saharan Africa: prevalence, incidence and risk factors. Middle East Afr J Ophthalmol. 2013;20:111–125. doi:10.4103/0974-9233.110605
4. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS investigators. Am J Ophthalmol. 2000;130:429–440. doi:10.1016/S0002-9394(00)00538-9
5. Heijl A, Leske MC, Bengtsson B, Hyman L, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120:1268–1279. doi:10.1001/archopht.120.10.1268
6. Kass MA, Heuer DK, Higginbotham EJ, et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:
7. Available from: https://cks.nice.org.uk/glaucoma#!scenariorecommendation:1.
8. Vélez-Gómez MC
9. Detry-Morel M. Side effects of glaucoma medications. Bull Soc Belge Ophtalmol. 2006;299:27–40.
10. Adekoya BJ, Adepoju FG, Moshood KF, Balarabe AH. Challenges in the management of glaucoma in a developing country; a qualitative study of providers’ perspectives. Niger J Med. 2015;24(4):315–322.
11. Santos MA, Ayena DK, Kuaovi KR, Vonor K, Djagnikpo A, Balo KP. Adherence with medical treatment in primary open-angle glaucoma in Lomé. J Fr Ophtalmol. 2016;39(5):459–466. doi:10.1016/j.jfo.2015.10.013
12. Tchabi S, Abouki C, Sounouvou I, Yèhouessi L, Doutetien C, Bassabi SK. Observance au traitement médical dans le glaucome primitif à angle ouvert. [Survey of medical treatment in primary open-angle glaucoma]. J Fr Ophtalmol. 2011;34(9):624–628. doi:10.1016/j.jfo.2011.07.009
13. Kyari F, Nolan W, Gilbert C. Ophthalmologists’ practice patterns and challenges in achieving optimal management for glaucoma in Nigeria: results from a nationwide survey. BMJ Open. 2016;6(10). doi:10.1136/bmjopen-2016-012230
14. Tamrat L, Gessesse GW. Gelaw Y Adherence to topical glaucoma medications in Ethiopian patients. Middle East Afr J Ophthalmol. 2015;22(1):59–63. doi:10.4103/0974-9233.148350
15. Abdull MM, Chandler C, Gilbert C. Glaucoma,“the silent thief of sight”: patients’ perspectives and health seeking behaviour in Bauchi, northern Nigeria. BMC Ophthalmol. 2016;21(16):44. doi:10.1186/s12886-016-0220-6
16. Ocansey S, Kyei S, Diafo A, Darfor KN, Boadi-Kusi SB, Aglobitse PB. Cost of the medical management and prescription pattern for primary open angle glaucoma (POAG) in Ghana-a retrospective cross-sectional study from three referral facilities. BMC Health Serv Res. 2016;19(16):282. doi:10.1186/s12913-016-1528-x
17. Mehari T, Giorgis AT, Shibeshi W. Level of adherence to ocular hypotensive agents and its determinant factors among glaucoma patients in Menelik II Referral Hospital, Ethiopia. BMC Ophthalmol. 2016;2(16):131. doi:10.1186/s12886-016-0316-z
18. Sherwood M, Brandt J, for the Bimatoprost Study Groups 1 and 2. Six-month comparison of bimatoprost once-daily and twice-daily with timolol twice-daily in patients with elevated intraocular pressure. Surv Ophthalmol. 2001;45(S4):S361–S368. doi:10.1016/S0039-6257(01)00219-3
19. Parrish RK, Palmberg P, Sheu WP, XLT Study Group. A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: a 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmol. 2003;135:688–703. doi:10.1016/S0002-9394(03)00098-9
20. Olthoff C, Schouten J, van de Borne B, Webers C. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension- an evidence based review. Ophthalmology. 2005;112:953–961. doi:10.1016/j.ophtha.2004.12.035
21. Davis S, Sleath B, Carpenter D, Blalock S, Muir K, Budenz D. Drop instillation and glaucoma. Curr.Opin.Ophthalmol. 2018;29:171–177. doi:10.1097/ICU.0000000000000451
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
